Abstract
Objective:
While 90% of suicide victims have suffered from mental health disorders, less than one-half are in contact with a mental health professional in the year preceding their death. Service use in the last year of life of young suicide victims and control subjects was studied in Quebec. We wanted to determine what kinds of health care services were needed and if they were actually received by suicide victims.
Method:
We recruited 67 consecutive suicide victims and 56 matched living control subjects (aged 25 years and younger). We evaluated subjects’ psychopathological profile and determined which services would have been indicated by conducting a needs assessment. We then compared this with what services were actually received.
Results:
Suicide victims were more likely than living control subjects to have a psychiatric diagnosis. They were most in need of services to address substance use disorder, depression, interpersonal distress, and suicide-related problems. There were significant deficits in the domains of coordination and continuity of care, mental health promotion and training, and governance.
Conclusions:
Our results show that we need to urgently take action to address these identified deficits to prevent further loss of life in our young people.
Keywords: suicide, public health, mental health services, substance-related disorders, youth, prevention
Abstract
Objectif :
Bien que 90 % des victimes de suicide aient souffert de troubles de santé mentale, moins de la moitié ont été en contact avec un professionnel de la santé mentale dans l’année précédant leur décès. L’utilisation des services dans la dernière année de vie des jeunes victimes de suicide et de sujets témoins a été étudiée au Québec. Nous avons voulu déterminer quels genres de services de soins de santé étaient nécessaires et s’ils ont été reçus en réalité par les victimes de suicide.
Méthode :
Nous avons recruté 67 victimes consécutives de suicide et 56 sujets témoins appariés et vivants (âgés de 25 ans et moins). Nous avons évalué le profil psychopathologique des sujets et déterminé quels services auraient été indiqués par une évaluation des besoins. Nous avons ensuite comparé ceci avec les services réels qui ont été reçus.
Résultats :
Les victimes de suicide étaient plus susceptibles que les sujets témoins vivants d’avoir un diagnostic psychiatrique. Elles avaient surtout besoin des services pour traiter un trouble lié à l’utilisation de substances, à la dépression, à la détresse interpersonnelle, et à des problèmes liés au suicide. Il y avait des déficits significatifs dans les domaines de la coordination et de la continuité des soins, de la promotion et de la formation en santé mentale, et de la gouvernance.
Conclusions :
Nos résultats indiquent qu’il est urgent d’agir pour régler ces déficits identifiés afin de prévenir d’autres pertes de vie chez nos jeunes gens.
In 2009, suicide was the second leading cause of death of Canadians aged 15 to 34 years old. In that year, out of the 3890 suicides in Canada, 1060 were by young people under the age of 34.1 Within Quebec, 2% of all deaths occur by suicide. This percentage is higher for men and male youth (3%) than for women and female youth (0.9%), and the rates vary by geographical area.2
It is known that 90% of people who have died by suicide suffered from a mental disorder.3 Despite this, people who have died by suicide have low rates of contact with health care providers. In a study of Quebec adolescent suicide victims, while two-thirds did see a GP in their last year of life, less than one-fifth saw one within their last month.4 Only 13% had seen a psychiatrist in their last month of life. Perhaps even more seriously, among those who have died by suicide who sought professional help, less than one-half were properly diagnosed.4 Other studies have also found low use of second-line specialized mental health services by youth and young adult who have died by suicide, ranging between 15% to 50% within the year preceding death.5–7
Many studies have looked at suicide risk factors; however, with the exception of audit and coroner’s reports or media scandals following a lawsuit, little research or documentation exists on the adequacy of services. Consequently, in our study, we report on the health service use of young suicide victims in their last year of life. By conducting psychological autopsies, we identified the psychopathological profile of each person and had an expert panel of psychiatrists determine which health services were indicated. The deficits in services were determined and the deficiencies are described by organizational level (that is, individual, local, regional, and provincial). Finally, we present organized recommendations for suicide prevention.
Method
Recruitment
Details of the recruitment procedures for this group have been previously published.8 In collaboration with the Quebec Coroner’s Office and the Montreal Central Morgue from September 2002 to December 2005, families of suicide victims aged 25 and younger were contacted by mail and invited to participate in our study. A total of 67 consecutive suicide victims were recruited with a participation acceptance rate of 75%. Fifty-six living control subjects with no suicidal ideation within the last year were also recruited and matched for age, sex, and local health services region. They were not matched for educational level, but a posteriori were found to be not significantly different from the suicide group. Control subjects were recruited by school principals, members of the health and social services community, and through posters placed on the walls of our research partners. Our study was approved by our local institutional review boards, the Douglas Mental Health University Institute, the Centre Hospitalier Universitaire Sainte-Justine, and the Université du Québec en Outaouais. Families of the suicide victims, control subjects, and informants signed written informed consent.
Clinical Implications
Better training, coordination, and continuity of care are strategies to prevent suicide in young people.
Government-supported protocols are potential strategies to optimize service delivery.
Limitations
Psychological autopsy is subject to selection and recall bias.
As the sample studied is almost entirely Caucasian, it does not reflect the First Nations in northern Quebec who may be subject to different barriers of care.
Data Gathering
Suicides were assessed by psychological autopsy, a validated method9,10 where a key informant best acquainted with the subject in question was interviewed. Interviews were usually completed with a parent, sibling, or spouse. To ensure comparability of the 2 groups, all comparison subjects were also diagnosed through interviews carried out with an appropriate informant. For both suicide and control subjects, demographic and clinical data, as well as detailed accounts, of their requests and usage of health care services were gathered. Through semi-structured interviews, families provided information on life trajectory, events, circumstances, psychological symptoms and disorders, and types of received health services. Axis I and II diagnoses were determined with the administration of the SCID.11,12 Several studies have established that DSM diagnoses generated by informant-report are of good to excellent reliability.7,10,13,14 Coroner’s reports and hospital files were also examined. We also considered any other relevant personal documents (for example, letters). This procedure was previously described by our group.15–17
Data were collected according to the needs assessment procedures as initially developed for people with severe mental illness,18 and subsequently for people with common mental disorders coming from the community.19 In the course of the latter study, interrater reliability of the methods was assessed, comparing assessment by 2 independent panels, and found satisfactory for most areas (for example, care for addiction disorders problems).20 A schedule for service needs had also been developed21 and adapted for our study.
Information Processing
After data were collected, the coding procedure was done quantitatively and qualitatively, as described previously in Séguin et al.8 A narrative case vignette of 3 to 7 pages was produced for each subject. Information identifying whether the patient was deceased or living was carefully removed. The vignettes were then presented to a panel composed of 1 adult psychiatrist and 2 child and adolescent psychiatrists. All panellists were experienced, having worked in EDs, outpatient clinics, inpatient services, and as consultants for youth protection services. The panel independently reviewed each vignette. For each subject, the panel determined the DSM-IV diagnoses by consensus.
Needs Assessment Evaluation
Using a validated and reliable needs assessment procedure20,22 the panel determined, from the vignettes, what services were indicated for each subject. Subsequently, they considered whether these needs had in fact been met. This needs analysis was done in 4 steps:
For each person, a list of received services was generated and divided into 4 time frames (last month, last year excluding last month, lifetime excluding last year, and lifetime). The services were also classified into types of service delivery: front-line medical services, front-line health and social services, second-line specialized mental health private or public services, and volunteer or non-profit services (Table 1).
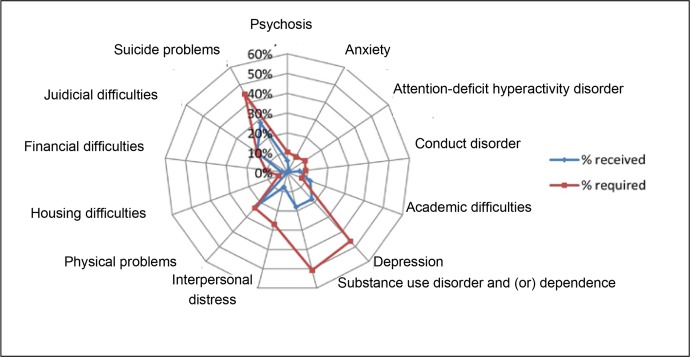
For each person, problem areas were identified (psychiatric, interpersonal, physical, financial, judicial, academic, or housing). The received interventions were classified by problem area and are represented in Figure 1.
For each person, the panel generated, by consensus, a list of health services that were indicated within the last year. The interventions received by the suicide group, compared with interventions required, are illustrated by problem area and by type of intervention (for example, assessment, psychotherapy, and psychiatric medications) (Table 2).
For each person, the panel compared required interventions with those actually received and considered possible reasons for any deficit in services. The panel then generated a list of recommendations directed at different levels of the health care system (individual, local, regional, and provincial) that, if implemented, could have helped ensure that a person obtain the needed intervention(s). These recommendations were divided into 5 categories: mental health promotion and training, treatment, funding, continuity of care, and governance.
Table 1.
Service use of people in the suicide group over time (n = 67)
| Service provider | Last month | Last year (excludes last month) | Lifetime (excludes last year) | Lifetime | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| n | % | n | % | n | % | n | % | |
| Front-line medical services (family doctors and other physicians) | 2 | 3.0 | 12 | 17.9 | 25 | 37.3 | 28 | 41.8 |
| Allied health, social service, and community professionals (nurses, social workers, school professionals, and police) | 6 | 9.0 | 12 | 17.9 | 15 | 22.4 | 24 | 35.8 |
| Second-line specialized mental health services (psychiatrists, psychologists, nurses, social workers, youth and crisis centre workers, addiction treatment centres, and hospital emergency departments) | 5 | 7.5 | 13 | 19.4 | 15 | 22.4 | 24 | 35.8 |
| Volunteer or non-profit services (hotlines and support lines, clergy, Alcoholic Anonymous, and Narcotics Anonymous) | 3 | 4.5 | 3 | 4.5 | 3 | 4.5 | 7 | 10.4 |
| At least 1 of the above | 14 | 20.9 | 28 | 41.8 | 35 | 52.2 | 63 | 94.0 |
Figure 1.
Summary of interventions received, compared with required, in percentages, classified by problem, in the suicide group (n = 67)
Table 2.
The number of people in the suicide group who received each specific intervention, compared with the number of people who required each intervention, with the percentage deficit also shown (n = 67)
| Interventions | Received | Required | Percentage deficita |
|---|---|---|---|
| School setting follow-up | 5 | 5 | 0 |
| Medication follow-up for a medical condition | 8 | 12 | 33 |
| Psychiatric medication | 17 | 26 | 35 |
| Residential setting, hospitalization, and addiction treatment centre | 10 | 16 | 38 |
| Case follow-up | 8 | 16 | 50 |
| Assessment | 23 | 59 | 61 |
| Psychotherapy | 8 | 21 | 62 |
| Counselling | 13 | 39 | 67 |
Results
Sociodemographic Profile
About 80% of both the suicide and control group were men or male youth. There was no significant difference in age between groups. People in the suicide group ranged between the ages of 13 to 25 years old (mean 20.43, SD 3.2), while people in the control group were between the ages of 14 and 25 (mean 20.22, SD 3.14) (Table 3).
Table 3.
Sociodemographic profile of people in the suicide and control groups
| Sociodemographic variable | Suicide group, % n = 67 | Control group, % n = 56 |
|---|---|---|
| Sex | ||
| Male | 80.6 | 76.8 |
| Female | 19.4 | 23.2 |
| Age, years | ||
| Mean age (SD) | 20.4 (3.2) | 20.2 (3.1) |
| <15 | 6.0 | 5.4 |
| 15–19 | 30.0 | 35.7 |
| 20–24 | 59.5 | 50.0 |
| 25 | 4.5 | 9.0 |
| Ethnicity | ||
| Caucasian | 94.0 | 96.0 |
| Means of suicide | ||
| Strangulation | 73.1 | n/a |
| Firearms | 10.4 | n/a |
| Carbon monoxide | 4.5 | n/a |
| Medication overdose | 3.0 | n/a |
| Collision (train or subway) | 3.0 | n/a |
| Jumping from a height | 3.0 | n/a |
| Stabbing | 1.5 | n/a |
| Drowning | 1.5 | n/a |
n/a = not applicable
Psychopathology of the Suicide Group, Compared With the Control Group
During the last year of life, mood disorders were much more common in the suicide group, compared with the control group (70%, compared with 4%), but there were also important differences in the rates of SUDs (45%, compared with 5%) and anxiety disorders (13%, compared with 2%). Overall, it was 8 to 63 times more likely for a person afflicted by 1 of these conditions to be in the suicide group, rather than the control group.
Mental health problems were also commonly present prior to the last 12 months of life, most notably affective disorders (40.3%), SUDs (44.8%), attention-deficit hyperactivity disorders (22.4%), and anxiety disorders (14.9%). Results indicate that 87.5% of participants in the suicide group had at least 1 lifetime diagnosis, compared with 9.6% in the control group.
In terms of DSM-IV Axis II personality disorders, 47.8% of participants from the suicide group had 1 or more diagnosis, particularly in clusters B (23.9%) and C (22.4%). In comparison, personality disorders were found in only 5.4% of the control group. As for the number of suicide attempts reported by the informant, 34.4% of the suicide group had previously made at least 1 attempt and none of the control group participants were reported to have ever made an attempt.
A detailed table of Axis I and II disorders identified within the suicide and control groups is presented in Séguin et al.8
Services Received by the Suicide Group
Only about 40% of people used any type of health service within the last year preceding their death; however, the use of specialized mental health services was particularly uncommon. More than 35% of people had used these specialized services in their lifetime, and only 20.9% of them had used any type within the last year of life. In the month preceding death, only 7.5% received second-line specialized mental health services (Table 1).
Health Service Needs, Classified By Service
Following the panel’s recommendations, their list of necessary services was compared with those actually received. It was found that 52 of the 67 suicide victims did not obtain all the services they needed. By comparison, among the 56 control subjects, 12 required services. Among these 12 control subjects, 5 received the services they needed and 7 were found with unmet needs.
The most commonly required need in the suicide group was for assessment or referral to another level of services. Among the 52 suicide victims with unmet needs, there were 59 episodes (some had more than 1 episode) for which a need for referral or assessment was identified. Counselling, psychotherapy, psychiatric medication, and medical follow-up for a physical condition were very often needed as well. Admission to an addiction treatment centre, to a residential setting, or to an inpatient hospital ward was also often indicated. Many subjects required regular follow-up, including surveillance and supervision from family members (not shown in Table 2).
Unmet Health Service Needs of the Suicide Group, Classified by Problem
The most frequently unmet needs were in the domains of SUD and depression, where in both, roughly 50% of those who should have received services did not receive them. Other common areas of unmet needs included situations of interpersonal distress, suicide-related problems, and legal problems. Other clinical and psychosocial problems (for example, anxiety, disruptive disorders, school, or residential) were considered to represent a deficit of 10.0% or less in terms of needs (Figure 1).
Shortfalls in the Health Care System
Table 4 outlines possible interventions to address the problem of unmet health needs. The panel considered ways that these shortfalls could have been averted or minimized. It became clearly apparent that in many subjects (39 of 67 of the suicide group) there were problems in the coordination of services and continuity of care. Our results showed that this could be manifested as poor communication of the patient’s suicide risk factors and urgency in which joint action needed to be taken, or a failure to designate a fixed point of responsibility within the health care team or between service levels. In other cases, there was a tendency for health care providers to wait for the patient to be motivated rather than to be more proactive. We recommend stricter protocol application and monitoring, follow-up with the development and application of treatment plans, and individual and (or) group case management. This could involve specialized mental health services, addiction treatment centres, youth protection, police, and school services, GPs, hospital, and ED staff.
Table 4.
Identified needs in suicide (n = 67) and control (n = 56) groups, and recommendations
| Needs to be addressed | Level of responsibility | Affected cases | |||
|---|---|---|---|---|---|
|
|
|
||||
| SG (n = 67) | CG (n = 56) | Recommendations | Stakeholders involved | ||
| Coordination and continuity of care | Regions | 39 | 0 | Protocol application and monitoring Follow-up Development and application of treatment plans Case management |
Specialized mental health services ATCs Youth centres Police services GPs School services Psychosocial services Hospital and ED staff |
| Mental health promotion and training | Provinces Professional organizations |
35 | 5 | Develop strategies to bring people with mental health and substance use disorder to medical attention Training in suicidal crises management |
Patients and families Primary health providers Specialized mental health providers Social services Judicial services School services |
| Governance | Provincial health and social department and justice department | 17 | 1 | Development and implementation systematic protocols in each region Outreach protocols |
Specialized mental health services ATCs Justice department GPs School services Psychosocial services Hospital and EDs |
| Treatment | Provinces | 1 | 1 | Shorten waiting lists | Psychosocial services |
| Regions | Improve access | ||||
| Funding | Provinces | 1 | 0 | School counsellors | School professionals |
| Regions | Psychologists | ||||
ATC = addiction treatment centre; CG = control group; ED = emergency department; GP = general practitioner; SG = suicide group
In many cases, there needed to be better identification of mental health problems in people (35 of 67 of the suicide group). Most often, family members and the general population recognized signs of distress but were unsure how to go about directing the person toward services. Mental health promotion and training are the purviews of the province and the professional organizations, such as the associations of psychiatrists, physicians, nurses, and psychologists. We recommend the development of strategies to help patients, families, and other interested parties ensure that people suffering from mental health problems come to the attention of the health care system.
Once the families, school services, or the patient present problems to the health care system’s basic services, the intervention of GPs trained in the identification and treatment of mental disorders is required. This is especially important for more complex cases, such as depression or SUD, depression or behavioural problems, or a combination of all of these. Basic health care providers must know when to refer a patient to mental health services for refinement of diagnoses and for further referral to more specialized services, if indicated. We also recommend training of social, judicial, and school services in patient referrals and in the possibility of shared care within front-line psychosocial services, specialized mental health services, and addiction, and crisis systems for continuity of care. Further, more education is needed in the proper assessment of suicide risk.
In a considerable number of subjects (17 of 67 of the suicide group), the person may have benefited from a systematic pathway to care, had it been established by the provincial Departments of Health, Social Services, and Justice. Our recommendation is the development and implementation of systematic protocols in each health administrative region in the province, as well as outreach programs. For example, a person who is having suicidal thoughts coming to the ED with an SUD and driving a car would have to be assessed in the ED, then referred to mental health services in conjunction with addiction services and police services, to better intervene in this high-risk situation. Systematic government-supported protocols would ensure equivalent quality of care across the province. Protocols usually identify specific key professionals and timely interventions, under a regional administrative infrastructure that allow more rapid, coordinated, and effective interventions.
In conclusion, the last needs to be addressed are regarding treatment and funding categories, both the purview of the province and its regional authorities. These were not found in many cases; however, our recommendations for treatment are shortened waiting lists and improved access to services, both of which would mainly involve psychosocial services. Finally, school services were broadly in place; however, full-time availability and sustainability of this type of services should be supported by recurrent budget.
Limitations
There are limitations to our study design at various steps. There is a risk of selection bias as we relied on volunteers when we recruited live control subjects. However, we did find that 12% of our control group had major mental health difficulties over the course of the last 12 months prior to the study, which is consistent with Canadian epidemiologic studies.23 Additionally, one of our inclusion criteria was the absence of suicidal ideation within the last year. One way to limit the bias would have been to use a control group consisting of deceased victims, for instance from traffic accidents.
The psychological autopsy method is also subject to recall bias as the information is obtained from an informant who may not have been aware of all the care received. Therefore, we included other sources (medical records and coroner reports). Past studies7,13,14 have shown that DSM diagnoses derived from the proxy-based psychological autopsy do not significantly differ from those found in medical records. We also could not take into account what services may have been offered and turned down by the person.
Our study was based in Quebec and may not be fully generalizable to other systems, even in Canada where health care falls under provincial jurisdiction. Quebec residents also have the benefit of a public medication insurance policy. As the groups studied were almost entirely Caucasians, it does not reflect the First Nations in northern Quebec who may be subject to different barriers of care.
Finally, the needs, as determined by the needs assessment, reflect the opinions of the panel. Given that the panel was comprised of an experienced team of 3 psychiatrists, it is most likely that their opinions reflect general psychiatric practice in Quebec and the rest of Canada.
Discussion
As expected, we found a much higher rate of psychopathology in the suicide group, compared with the control group. The most common mental illnesses identified in the suicide group were SUDs (45%) and affective disorders (40%). Axis II disorders were also detectable in a large number of suicide victims (48%), compared with the control group (5%). Despite the high level of psychopathology, there was relatively little use of health services. Within their last year of life, less than one-half of suicide victims (41.8%) received any services at all, while about 20% received specialized mental health services. The people in the suicide group had particularly needed interventions to address suicide-related problems, depression, and SUD. Less than one-half of people who needed assessment, counselling, or psychotherapy received such services. When the subjects were individually considered, it became clear that the unmet service needs of suicide victims were, in large part, due to weaknesses in coordination and continuity of care, and insufficient mental health promotion and training. We also found that strategies needed to be implemented at the government level.
One way to look at our findings is to use the model of Andersen and Laake24 related to 3 main determinants involved in the use of health services: societal, system, and individual. One societal determinant is mental health stigma. According to a Canadian Medical Association study,25 only 58% of people said they would feel comfortable talking with an immediate family member if they suspected having a mental illness, and 40% would try to deal with it themselves without speaking to anyone about it. Young people were less comfortable speaking to their family doctor about mental illness, compared with older adults (36% of 18- to 34-year-olds, compared with 60% of people aged 55 years or older).
Second, there may be several systemic determinants affecting health services use. In a 2011 survey of Canadian family physicians, psychiatry was among the specialties identified as the most difficult to access.26 Long wait times were the most commonly identified reason. As it is more common for people to be seen in primary care, it is critical that these front-line workers have sufficient training to be able to identify those who suffer from mental illness. As mentioned in a previous study,4 less than one-half of suicide victims had been properly diagnosed by the time of death. If the health system is too strained, it is easy for well-intentioned professionals to miss a diagnosis that is not spontaneously presented by the patient, to lose a patient during follow-up when they are not coming to appointments, or to not spend the time trying to contact colleagues to ensure better continuity of care.
Finally, individual determinants may be of great importance. People in our suicide group had many factors working against them receiving care: Axis II personality disorders impairing their ability to form stable relationships (friends, family, and health professionals); or their impulsively missing appointments. Many people in the suicide group had alcohol problems and may not have had the insight to accept help. If they suffer from comorbid mental disorders, they may have been untreated and without follow-up, as health professionals may ask that they seek help for the SUD first. Another possible explanation to further explore is that some youth may also have avoided consulting available services. This should challenge mental health services to think about more creative, innovative health care services that would better fit their needs.
The recommendations in our report were mainly based on expert opinion, using information obtained mainly from the subjects’ relatives. Recommendations are based on the assumption that if people with mental health problems receive adequate services they are less likely to die as a result of suicide. A study by Desai et al27 showed an increase risk of suicide with decreased continuity of care, and another study28 suggests that access to care is negatively correlated with suicide rates.
Specific, evidence-based strategies are needed to reduce the rate of suicide. In line with our results, a recent study29 looked at the effect of the Safety First mental health recommendations in the United Kingdom. The study compared suicide rates of patients followed in mental health services before and after the implementation of specific recommendations: the availability of 24-hour crisis care, local policies on dual diagnosis, and multidisciplinary review after a suicide. Notably, places that did not implement the recommendations saw little reduction in suicide. This supports our views of implementing best practices based on our research findings. It also highlights how a governmental investment implementing evidence-based mental health policy on a national scale can lead to positive change and the development of knowledge that can be easily translated into clinical practice.
Conclusions
Needs assessment procedures aimed at formulating the best intervention, timely offered services, and even system recommendations, involve comprehensive data collection and clinical service judgments, which we sought to systematize. Based on our findings, important clinical, research, and public health actions are urgently needed.
Acknowledgments
The research has been funded by the Canadian Institute of Health Research.
The authors have no financial relations or conflicts of interest to disclose. Dr Renaud has been supported by the National Alliance for Research on Schizophrenia and Depression and Brain and Behaviour Research Foundation Young Investigator Award, and is a Standard Life Senior Fellow in Teen Mental Health. We warmly thank all families for their unique contribution to our study.
Dr Claude Marquette (1940–2014) created the first adolescent unit and department at the Philippe-Pinel Institute, then at the Centre Hospitalier Universitaire Sainte-Justine, (both affiliated with the Université de Montréal), where he was also director of the Department of Psychiatry from 1987 to 2000. He was central in the development, in 2000, of the protocol on suicide assessment in youth centres, created in collaboration with the Quebec College of Physicians and the Association of Quebec Youth Centres. Since then, suicide rates have decreased by 65% among adolescents in Quebec.
Abbreviations
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ED
emergency department
- GP
general practitioner
- SCID
Structured Clinical Interview for DSM-IV
- SUD
substance use disorder
References
- 1.Statistics Canada. Navaneelan T. Suicide rates: an overview. Ottawa (ON): Statistics Canada; 2012. [Google Scholar]
- 2.Institut National de la Statistique du Québec . Le médecin de famille et l’endroit habituel de soins : regard sur l’expérience vécue par les Québécois. Quebec (QC): Institut National de la Statistique du Québec; 2013. Enquête québécoise sur l’expérience de soins 2010–2011. [Google Scholar]
- 3.Cavanagh JT, Carson AJ, Sharpe M, et al. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 4.Renaud J, Berlim M, Séguin M, et al. Recent and lifetime utilization of health care services by children and adolescent suicide victims: a case–control study. J Affect Disord. 2009;117:168–173. doi: 10.1016/j.jad.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 5.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martunnen MJ, Aro HM, Lonngvist JK. Adolescence and suicide: a review of psychological autopsy studies. Eur Child Adolesc Psychiatry. 1993;2(1):10–18. doi: 10.1007/BF02098826. [DOI] [PubMed] [Google Scholar]
- 7.Brent DA, Perper JA, Mortiz G, et al. Psychiatric risk factors for adolescent suicide: a case–control study. J Am Acad Child Adolesc Psychiatry. 1993;32:521–529. doi: 10.1097/00004583-199305000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Séguin M, Renaud J, Lesage AD, et al. Youth and young adult suicide: a study of life trajectory. J Psychiatr Res. 2011;45:863–870. doi: 10.1016/j.jpsychires.2011.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Conner KR, Conwell Y, Duberstein PR. The validity of proxy-based data in suicide research: a study of patients 50 years of age and older who attempted suicide. I. Psychiatric diagnoses. Acta Psychiatr Scand. 2001;104:452–457. doi: 10.1034/j.1600-0447.2001.00405.x. [DOI] [PubMed] [Google Scholar]
- 10.Kelly TM, Mann JJ. Validity of DSM-III-R diagnosis by psychological autopsy: a comparison with clinician ante-mortem diagnosis. Acta Psychiatr Scand. 1996;94:337–343. doi: 10.1111/j.1600-0447.1996.tb09869.x. [DOI] [PubMed] [Google Scholar]
- 11.First MB, Spitzer RL, Robert L, et al. Structured Clinical Interview for DSM-IV-TR Axis I disorders, research version, patient edition (SCID-I/P) New York (NY): Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 12.First MB, Gibbon M, Spitzer RL, et al. Structured clinical interview for DSM-IV Axis II personality disorders (SCID-II) Washington (DC): American Psychiatric Press; 1990. [Google Scholar]
- 13.Zhang J, Conwell Y, Wieczorek WF, et al. Studying Chinese suicide with proxy-based data: reliability and validity of the methodology and instruments in China. J Nerv Ment Dis. 2003;191:450–457. doi: 10.1097/01.NMD.0000081613.03157.D9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schneider B, Maurer K, Sargk D, et al. Concordance of DSM-IV Axis I and II diagnoses by personal and informant’s interview. J Psychiatr Res. 2004;127:121–136. doi: 10.1016/j.psychres.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 15.Lesage AD, Boyer R, Grunberg F, et al. Suicide and mental disorders: a case–control study of young men. Am J Psychiatry. 1994;151:1063–1068. doi: 10.1176/ajp.151.7.1063. [DOI] [PubMed] [Google Scholar]
- 16.Dumais A, Lesage AD, Lalovic A, et al. Is violent method of suicide a behavioral marker of lifetime aggression? Am J Psychiatry. 2005;162:1375–1378. doi: 10.1176/appi.ajp.162.7.1375. [DOI] [PubMed] [Google Scholar]
- 17.Kim C, Lesage A, Séguin M, et al. Patterns of comorbidity in male suicide completers. Psychol Med. 2003;33:1299–1309. doi: 10.1017/s0033291703008146. [DOI] [PubMed] [Google Scholar]
- 18.Brugha TS, Wing JK, Brewin CR, et al. The problems of people in long-term psychiatric day care. An introduction to the Camberwell High Contact Survey. Psychol Med. 1988;18(2):443–456. doi: 10.1017/s0033291700007984. [DOI] [PubMed] [Google Scholar]
- 19.Bebbington PE, Brewin CR, Marsden L, et al. Measuring the need for psychiatric treatment in the general population: the community version of the MRC Needs for Care Assessment. Psychol Med. 1996;47:343–357. doi: 10.1017/s0033291700034620. [DOI] [PubMed] [Google Scholar]
- 20.Lesage AD, Séguin M, Guy A, et al. Systematic services audit of consecutive suicides in New Brunswick: the case for coordinating specialist mental health and addiction services. Can J Psychiatry. 2008;53(10):671–678. doi: 10.1177/070674370805301006. [DOI] [PubMed] [Google Scholar]
- 21.Brewin CR, Wing JK, Mangen S, et al. Needs for care among the long-term mentally ill: a report from the Camberwell High Contact Survey. Psychol Med. 1988;18(2):457–468. doi: 10.1017/s0033291700007996. [DOI] [PubMed] [Google Scholar]
- 22.Van Haaster I, Lesage AD, Cyr M, et al. Further reliability and validity studies of a procedure to assess the needs for care of the chronically mentally ill. Psychol Med. 1994;24:215–222. doi: 10.1017/s0033291700026970. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen CT, Fournier L, Bergeron L, et al. Correlates of depressive and anxiety disorders among young Canadians. Can J Psychiatry. 2005;50(10):620–628. doi: 10.1177/070674370505001008. [DOI] [PubMed] [Google Scholar]
- 24.Andersen AS, Laake P. A causal model for physician utilization: analysis of Norwegian data. Med Care. 1983;21(3):266–278. doi: 10.1097/00005650-198303000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Canadian Medical Association (CMA) 8th annual national report card on health care. Ottawa (ON): CMA; 2008. [Google Scholar]
- 26.Canadian Cancer Survivor Network . Wait Times Alliance report card 2012: shedding light on Canadians’ total wait for care. Ottawa (ON): Canadian Cancer Survivor Network; 2014. [Google Scholar]
- 27.Desai RA, Dausey DJ, Rosenheck RA. Mental health service delivery and suicide risk: the role of individual patient and facility factors. Am J Psychiatry. 2005;162(2):311–318. doi: 10.1176/appi.ajp.162.2.311. [DOI] [PubMed] [Google Scholar]
- 28.Tondo L, Albert MJ, Baldessarini RJ. Suicide rates in relation to health care access in the United States: an ecological study. J Clin Psychiatry. 2006;67(4):517–523. doi: 10.4088/jcp.v67n0402. [DOI] [PubMed] [Google Scholar]
- 29.While P, Roscoe A, Windfuhr K, et al. Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross sectional and before-and-after observational study. Lancet. 2012;379:1005–1012. doi: 10.1016/S0140-6736(11)61712-1. [DOI] [PubMed] [Google Scholar]