Abstract
We examined the factor structure of borderline personality disorder (BPD) symptoms by using a multi-method, multi-sample approach. The factorial structure of BPD has previously been examined through the lens of broad retrospective reports of symptoms without directly contrasting results from different samples of participants, with studies producing inconsistent patterns of results. We go beyond previous work by examining symptoms from multiple timeframes and by examining results across and within two diagnostic groups – individuals with and without BPD. Participants (N = 281) completed a structured clinical interview for personality disorders, two weekly reports of BPD symptoms, and two weeks of in-the-moment “immediate” symptom reports, assessed five times daily. Across all participants, results revealed a robust one-factor structure that replicated across all assessment methods. Moreover, these results replicated within each diagnostic group, with the lone exception of an unclear structure in interview assessment among participants who had a BPD diagnosis. Results have implications regarding the nature, assessment, and treatment of BPD.
Keywords: Borderline Personality Disorder, Heterogeneity, Factor Structure, Experience Sampling Methods
The purpose of this research is to reveal the structure of borderline personality disorder (BPD) symptoms across different timeframes and methods of assessment. Establishing the structure of BPD is important for several reasons. First, it is fundamental to understanding the nature of BPD as a coherent – or perhaps incoherent – psychological concept. The Diagnostic and Statistical Manuals (DSMs) have treated BPD as a unitary disorder, without clinically-relevant differences in facets or subtypes. However, the validity of this perspective hinges on the implicit assumption that BPD symptoms have a unidimensional structure. Second, clarifying the structure of BPD symptoms can affect the study of BPD’s etiology. It is possible that different facets or subtypes of BPD arise from different biological pathways and/or from different environmental mechanisms. Third, it can facilitate the development and evaluation of novel assessment, diagnosis, and treatment programs that might be appropriate for different facets or subtypes of the disorder (Bornovalova, Levy, Gratz, & Lejuez, 2010; Bradley, Conklin, Westen, 2005; Clifton & Pilkonis, 2007; Leihener, Wagner, Haaf, Schmidt, Lieb, Stieglitz, & Bohus, 2003; Lenzenweger, Clarkin, Yeomans, Kernberg, & Levy, 2008; Sanislow, Grilo, Morey, Bender, Skodol, Gunderson et al., 2002).
The DSM-5 (APA, 2013) defines BPD in terms of nine symptoms that span affective, interpersonal, and intrapersonal disturbances. A diagnosis requires the presence of any five symptoms, which allows for 256 combinations by which an individual could receive a BPD diagnosis. This variety of potential combinations raises the possibility that there are different dimensions or forms of BPD, which might have different etiologies, follow different paths of change, and respond to different treatments.
To evaluate the existence and nature of such potential heterogeneity in BPD, researchers have attempted to identify clusters or factors of BPD symptoms that tend to co-occur. Most of this work has been conducted via factor analysis, and results have provided mixed evidence of symptom heterogeneity1. Examining DSM-based criteria, some studies have identified a unitary construct (Clifton & Pilkonis, 2007; Fossati et al., 1999; Johansen et al., 2004; Sanislow et al., 2002), while others have identified two (Benazzi, 2006; Rosenberger & Miller, 1989; Whewell, Ryman, Bonanno, & Heather, 2000), three (Blais et al., 1997; Clarkin, Hull, & Hurt, 1993; Lewis, Caputi, & Grenyer, 2012; Sanislow, Grilo, & McGlashan, 2000; Sanislow et al., 2002; Taylor & Reeves, 2007), and four (Becker, McGlashan, & Grilo, 2006) factors of borderline symptoms. Among studies reporting multiple dimensions, there is some convergence in the nature of those dimensions (e.g., “affective regulation” or “identity disturbance”); however, there is also a great degree of divergence. Such divergence creates ambiguity both in the number and nature of BPD symptom factors. Perhaps contributing to this ambiguity, the studies differ dramatically in terms of their samples, their general analytic approaches, their specific statistical procedures, and to some degree, their assessment techniques.
One commonality among previous studies is their reliance on broad retrospective assessment tools – primarily in terms of clinician administered diagnostic interviews, self-report personality measures, or chart reviews. Although such tools are useful and necessary for traditional diagnostic procedures, they reflect only one temporal perspective on symptom experiences. As a broad summary of experiences, such assessments are based upon the assumption that symptoms are relatively stable across time and thus differentiate between people in terms of longstanding patterns, tendencies, and experiences. In terms of factorial structure, this perspective reveals whether people who generally experience one symptom also generally experience other specific symptoms (or perhaps all other symptoms, in the case of unidimensional structure).
However, symptoms can also be viewed through a narrower experiential timeframe. Given the ebb and flow of pathology across time, assessments based on broad summaries might not reflect a person’s experiences at any particular point in time – e.g., a given hour, day, or week. In terms of factorial structure, narrower timeframes reveal whether people who experience a symptom at one point in time also experience other specific symptoms at the same time. Thus, narrower timeframes provide sharp insight into patterns of symptom co-occurrence in real time, and thus provide a novel perspective on the potential existence of subtypes of borderline pathology.
Moreover, the difference between broad and narrow assessment timeframes can have important implications for the accuracy with which people report clinical events and symptoms. On one hand, broad retrospective assessments may be subject to a variety of recall-based biases and distortions (Ebner-Premier & Trull, 2009). Although BPD is defined as a chronic and longstanding pattern of behavior, cognition, and affect (APA, 2013), assessments that are relatively immediate and proximal to important psychosocial events might reflect even longstanding patterns more accurately than methods that require one to recall and summarize events over a broad temporal range (e.g., several years). In fact, some biases might be particularly pronounced among people with BPD. For example, people with BPD may overestimate earlier occurrences of negative emotions and underestimate occurrences of positive emotions (Ebner-Priemer, Kuo, Welch, Thielgen, Witte, Bohus, & Linehan, 2006). Thus, previous structural examinations of BPD symptoms may suffer from biases introduced by reliance on broad retrospective reports. On the other hand, despite important advantages of “narrow timeframe” assessments, there are also some potential disadvantages in narrow-timeframe assessments of BPD symptoms. Some symptoms are likely to be rather infrequent (e.g., self-harm, suicidal behavior), and the full extent of some symptoms might be experienced only occasionally. Such experiences might not be “caught” via assessments based on narrow timeframes, but they might well be recalled and reported through a broader assessment method.
Thus, it is quite conceivable that the apparent nature and factorial structure of BPD differs when assessed via broad versus narrower timeframes, as they reflect potentially different perspectives on the experience of BPD symptoms. Such findings would expand our understanding of BPD and the temporality of its symptoms. However, it is also conceivable that the factorial structure of BPD is consistent across timeframes. The emergence of a single coherent factorial structure that is consistent across timeframes would provide powerful convergent evidence on the general validity of that structure.
The current study examines the structure of BPD symptoms with both a traditional retrospective diagnostic interview as well as two novel methods with more focused and immediate timeframes. In the first novel method, participants reported symptoms on a weekly basis for two weeks, describing symptoms as they occurred during each week. This “weekly” method represents a much narrower temporal window, as compared to the traditional diagnostic interview. However, as it requires participants to reflect back over an entire week, it represents a somewhat more distal reporting perspective as compared to the second novel method. In that second novel method, participants reported BPD symptoms as they occurred within the preceding hour, doing this several times a day for 14 consecutive days. Such Experience Sampling Methods (ESM, or Ecological Momentary Assessment, EMA) have emerged as important and highly informative complements to broad retrospective reports, providing a much more “immediate” temporal perspective that reduces recall biases that affect broader retrospective reports (Conner, Tennen, Fleeson, & Barrett, 2009; Furr, 2009; Ebner-Priemer & Trull, 2009; Myin-Germeys, Oorschot, Collip, Lataster, Delespaul, & van Os, 2009). No previous research has examined the factorial structure of BPD symptoms from the perspectives represented by these novel methods.
We also examine the structure of BPD symptoms within and across different samples of participants. Previous research has primarily focused on clinical samples, with a number of studies focusing specifically on individuals diagnosed with BPD (e.g., Bradley et al., 2005; Lewis et al., 2012; Whewell et al., 2002). However, other research is based solely on non-clinical participants, while still other research includes both clinical and non-clinical participants. Such inconsistency in sample composition might well contribute to the inconsistency in findings across studies. Unfortunately, to our knowledge, there has been no systematic comparison of factorial structure across diagnostic samples. Thus, it is not clear whether, for example, the structure of BPD symptoms among people diagnosed with BPD is similar or meaningfully different from the structure of BPD symptoms among people representing a wide spectrum of pathology or among people without BPD. Systematic comparisons could not only clarify previous inconsistencies in examinations of the structure of BPD, but also have implications for a wide range of issues. For example, structural comparisons across clinical and non-clinical samples can inform debate about the diagnostic continuity or discontinuity of BPD (Krueger, Skodol, Livesley, Shrout, Huang, 2007; Widiger, Livesley, & Clark, 2009). For example, if clearly-different structures emerge across different types of samples, then this indicates a form of discontinuity in the elements of BPD (i.e., by suggesting that the fundamental facets of BPD function differently within the different samples). However, if a similar structure emerges across samples, then this would indicate an important form of continuity.
Method
Participants
As part of a larger longitudinal study, participants were recruited through two methods to ensure that a wide range of borderline pathology was represented. Some participants, including many recruited through a university psychiatric clinic, responded to flyers describing problems associated with BPD (e.g., “Are you extremely moody? Do you often feel distrustful of others?”; Zanarini, Vujanovic, Parachini, Boulanger, Frankenburg, & Hennen, 2003). Potential participants recruited via this method completed a screening that included the 10-item McLean Screening Instrument for BPD (MSI-BPD, Zanarini et al., 2003) and were invited to take part in the study if they endorsed at least seven items. Other participants responded to flyers advertising a general personality study. Participants recruited via this second method completed the same screening, but were included regardless of MSI-BPD responses. Exclusion criteria for all participants included being less than 18 years old, being greater than 65 years old, living more than 50 miles from the university, limited English language comprehension, having a court-appointed guardian, history of a violent crime arrest, current alcohol or substance dependency with use in the last 30 days, diagnosis of a current psychotic disorder, or actively suicidal. Participants were compensated with up to $170 in gift cards.
Across both recruitment methods, a total of 438 participants were screened. All participants who met inclusion and exclusion criteria (N=281) completed a diagnostic interview (the SIDP-IV, see below), with 86 meeting criteria for BPD (79 recruited via the psychiatric clinic and fliers referencing BPD-related problems, 7 recruited via fliers for a general personality study) and 195 not meeting criteria. Diagnostic groups did not differ on sex (NFemale=191, NMale=90) or race (NBlack=101, NWhite=164, NOther=16), but the BPD group had significantly lower age (MNonBPD=45, MBPD=41, p=.01, d=.36) and education levels (MNonBPD=14.9, MBPD=13.8, p=.004, d=.41). All subsequent analyses of diagnostic groups (BPD and Non-BPD) are based on actual SIDP-IV diagnosis, regardless of recruitment origin or MSI-BPD score.
Procedure and Materials
Diagnostic Interview (SIDP-IV)
The SIDP-IV is a semi-structured interview guiding diagnosis of psychiatric disorders, and it assesses global retrospective symptom experiences over the past five years. Participants completed the interview at their first visit after study enrollment. One score was derived for each BPD symptom, representing the degree to which a participant experienced each symptom as his or her “usual self.” For each symptom, interviewers (staff members with either a Ph.D. in Clinical Psychology or M.S.W.) implemented the scoring guidelines provided by Pfhol et al. (1995) on the following scale (0–3): not present (absent or rare and limited examples), subthreshold (some evidence but not to the point of considering a symptom present), present (symptom present most of the time) and strongly present (symptom is clearly associated with distress or impairment of functioning and/or relationships). All interviews were audio-taped, and 20 were later reviewed by a second rater for purposes of reliability estimation. For those 20 interviews, across the nine symptoms, inter-rater reliability ranged from.79 to .92, mean = .88.
Weekly Assessments
At the end of each of two successive weeks, participants reported symptom experienced during the previous week. This two-week period began the day after the diagnostic interview. Reports included, among other items, 19 items reflecting the nine symptoms of BPD, with 2 or 3 items per symptom (e.g., “An interpersonal relationship of mine was unstable and intense in the last 7 days,” and “I thought that people close to me were worthless in the last 7 days, although recently I have thought they were wonderful”). Items were rated on a 6-point scale (0=Never, 1=Once or twice, 2=3–5 times, 3=6–20 times, 4=21–50 times, and 5=50+ times). To parallel the SIDP’s symptom-level scoring and for convergence with previous examinations (e.g., Becker et al., 2010; Hallquist & Pilnkonis 2012; Lewis et al., 2012; Sansislow, 2002), we focused on symptom scores. Ratings were averaged across the two weekly reports and across items to produce one score per symptom, with scores representing the average degree to which each participant experienced each symptom in the two week period. Participants were given the choice of completing reports either online (n = 83) or on paper returned via standard mail (n = 137), and reports were excluded if completed more than three days after the scheduled response date. Weekly ratings were available for 220 participants (62 with BPD, 158 without BPD). Across the nine symptoms, internal consistency reliability ranged from.60 to .96, mean = .81.
Immediate Assessments
For the most immediate measure of symptoms, participants completed ESM reports five times daily for 14 days (the same two weeks during which participants provided weekly assessments). Participants carried personal digital assistants which presented symptom questions at pre-set times, 10 AM, 1 PM, 4 PM, 7 PM, and 10 PM. Items inquired about recent (last 60 minutes) BPD symptom experiences, strictly paralleling the weekly-report items (e.g., “An interpersonal relationship of mine was unstable or intense in the last 60 minutes”)2. Items were rated on a 6-point scale, from 0=does not describe me at all to 5=describes me very well. Similar to the weekly reports, symptoms assessed by two items were averaged for a symptom score and all symptom scores were averaged across all 14 days. The final averaged scores reflected the average degree to which the participant experienced each symptom during the two week period. Stringent inclusion criteria were used for ESM reports, with reports and individual items excluded from analyses for the following reasons: completed too quickly (i.e., 500 ms or faster), completed more than three hours after a designated start time or five minutes prior to a designated start time, or if there was an insufficient number of reports (i.e., less than 14 valid reports). In total, 207 participants had valid immediate data (58 with BPD, 149 without BPD). Across the 14 days, participants completed a mean of 43.4 valid ESM reports (Min = 13, Max = 68), with the modal number of reports being 56. Across the nine symptoms, internal consistency reliability ranged from .94 to .98, mean = .97.
Results
Analyses were conducted in two phases. The primary phase examined the factor structure of symptoms in each assessment method, across all participants. Secondarily, we explored whether the factor structures differed by BPD diagnosis, by examining the factor structure separately for participants with and without a diagnosis of BPD.
We conducted principal axis factor analyses, as recommended for this type of research questions (Fabrigar, Wegener, MacCallum, & Strahan, 1999; Floyd & Widaman, 1995). To determine the number of factors, we examined scree plots and parallel analysis (Fabrigar et al., 1999; Floyd & Widaman, 1995; Hayton, Allen, & Scarpello, 2004). To compare structural qualities across assessment methods and groups, we examined congruence coefficients (Tucker, 1951) and, where possible, inter-factor correlations. Congruence coefficients range from −1 to +1 and reflect similarity between factors. Coefficients higher than .95 indicate that factors are roughly equivalent, coefficients between .85 and .94 indicate “fair” similarity, and coefficients below .85 indicate dissimilar factors (Lorenzo-Seva & ten Berge, 2006).
Primary Analyses: Factor Structure for Different Measures
Table 1 presents descriptive statistics for BPD symptoms as measured by each method. Within each assessment method, symptoms had roughly similar means and variabilities, with the notable exception of suicide and self-harm in the weekly and immediate reports. Symptoms were generally strongly inter-correlated within each assessment method, with mean correlations of .60, .44, and .39 for the immediate assessments, weekly, and clinical interview (retrospective), respectively. Minimum correlations were, .44, .17, and .26, and the corresponding maximums were .80, .75, and .58. Thus, people who tended to experience any symptom of BPD also tended to experience the other symptoms, regardless of measurement method. Moreover, symptoms were significantly correlated across assessment methods. Across the 27 same-symptom/cross-method correlations (e.g., between Anger assessed via the clinical interview and Anger assessed via the immediate assessments), all were significant at p < .05, with r̄ = .46 (range = .18 to .81).
Table 1.
Descriptive Statistics for All Participants
| Assessment Method | Correlations
|
Structure Coefficient | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
| Immediate (N = 207) | ||||||||||
| 1. Unstable Relationships | .45 (.66) | - | - | - | - | - | - | - | - | .87 |
| 2. Abandonment | .36 (.74) | .67 | - | - | - | - | - | - | - | .73 |
| 3. Unstable Affect | .78 (.90) | .73 | .53 | - | - | - | - | - | - | .81 |
| 4. Emptiness/Hollow | .60 (.87) | .59 | .47 | .63 | - | - | - | - | - | .73 |
| 5. Unstable Identity | .37 (.65) | .66 | .63 | .66 | .78 | - | - | - | - | .85 |
| 6. Uncontrollable Anger | .39 (.59) | .73 | .47 | .80 | .52 | .59 | - | - | - | .76 |
| 7. Paranoid Ideation | .35 (.60) | .74 | .75 | .65 | .63 | .77 | .62 | - | - | .88 |
| 8. Suicide/Self-Harm | .06 (.15) | .63 | .46 | .44 | .44 | .52 | .51 | .58 | - | .64 |
| 9. Impulsivity | .40 (.61) | .58 | .60 | .55 | .50 | .60 | .51 | .64 | .50 | .71 |
| Weekly (N=220) | ||||||||||
| 1. Unstable Relationships | .79 (1.03) | - | - | - | - | - | - | - | - | .83 |
| 2. Abandonment | .71 (1.12) | .59 | - | - | - | - | - | - | - | .67 |
| 3. Unstable Affect | .34 (.68) | .24 | .19 | - | - | - | - | - | - | .32 |
| 4. Emptiness/Hollow | 1.23 (1.39) | .71 | .53 | .18 | - | - | - | - | - | .82 |
| 5. Unstable Identity | .63 (.99) | .63 | .60 | .23 | .66 | - | - | - | - | .82 |
| 6. Uncontrollable Anger | .85 (1.24) | .53 | .48 | .19 | .59 | .71 | - | - | - | .71 |
| 7. Paranoid Ideation | .83 (1.11) | .72 | .45 | .20 | .75 | .60 | .53 | - | - | .79 |
| 8. Suicide/Self-Harm | .07 (.33) | .28 | .22 | .41 | .17 | .35 | .30 | .24 | - | .37 |
| 9. Impulsivity | .83 (1.08) | .52 | .46 | .37 | .53 | .45 | .38 | .53 | .30 | .64 |
| Retrospective (N = 281) | ||||||||||
| 1. Unstable Relationships | 1.05 (1.14) | - | - | - | - | - | - | - | - | .67 |
| 2. Abandonment | .81 (1.11) | .41 | - | - | - | - | - | - | - | .59 |
| 3. Unstable Affect | 1.31 (1.18) | .55 | .35 | - | - | - | - | - | - | .74 |
| 4. Emptiness/Hollow | .83 (1.05) | .35 | .33 | .43 | - | - | - | - | - | .59 |
| 5. Unstable Identity | .57 (1.04) | .44 | .44 | .49 | .47 | - | - | - | - | .67 |
| 6. Uncontrollable Anger | 1.54 (1.08) | .54 | .33 | .58 | .33 | .39 | - | - | - | .65 |
| 7. Paranoid Ideation | .99 (1.34) | .27 | .38 | .33 | .35 | .36 | .26 | - | - | .51 |
| 8. Suicide/Self-Harm | .93 (1.21) | .35 | .40 | .47 | .48 | .45 | .34 | .38 | - | .65 |
| 9. Impulsivity | 1.54 (1.20) | .38 | .36 | .36 | .26 | .26 | .41 | .28 | .37 | .53 |
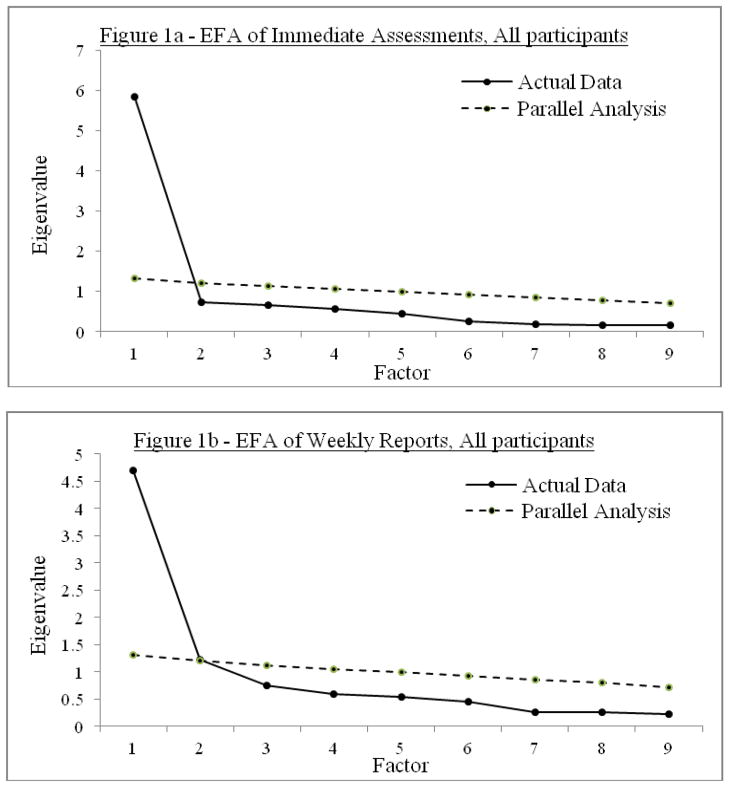
As shown in Figure 1, factor analyses clearly indicated a unidimensional structure that replicated across all three assessment methods. Scree plots show one robust first eigenvalue, a clear drop, and “leveling-off” beginning at the second eigenvalue. Moreover, parallel analyses show that only the first eigenvalue in each analysis is greater than the estimated random-data eigenvalues; all other eigenvalues are at or below the random-data eigenvalues3.
Figure 1.
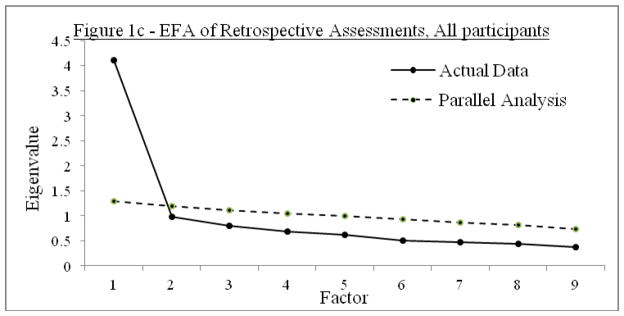
Exploratory Factor Analysis of BPD Symptoms
To clarify the nature of each factor, we extracted a single factor for each assessment method and examined factor loadings. The last column of Table 1 presents the loadings, all with generally strong positive values (min = .32, max = .88, mean = .69). Unstable relationships and unstable identity were among the three highest loading symptoms for all three assessments, potentially indicating that they are the most fundamental symptoms of BPD. In contrast, impulsivity was among the three lowest loading symptoms for every assessment, and suicide/self-harm was among the lowest for the weekly and immediate reports.
Although some differences occurred across assessment methods (e.g., unstable affect was among the highest loading symptoms in the clinical interview but the lowest among weekly reports), evidence indicates generally high levels of similarity in the factor structure. Indeed, as shown in the “All Participants” rows in Table 2, congruence coefficients revealed extremely high similarity across assessments (φ values ranging from .95 to.99). In addition, we computed factor scores for each participant via each assessment method, and examined correlations between factors. Again as shown in Table 2, results demonstrate strong correlations between all three methods (r’s ranging from .64 to .78, all p < .001).
Table 2.
Convergence of Factor Structure Across Methods of Assessment
| Assessment Method
|
|||
|---|---|---|---|
| Assessment Method | I | W | R |
| All participants | |||
| Immediate | .78*** | .67*** | |
| Weekly | .97 | .64*** | |
| Retrospective | .99 | .95 | |
| BPD participants | |||
| Immediate | .61** | .34* | |
| Weekly | .95 | .38** | |
| Retrospective | .77 | .62 | |
| Non-BPD participants | |||
| Immediate | .75*** | .52*** | |
| Weekly | .96 | .50*** | |
| Retrospective | .96 | .90 | |
Note. Congruence coefficients are below the diagonals, inter-factor correlations are above the diagonals.
p < .05;
p < .01;
p < .001.
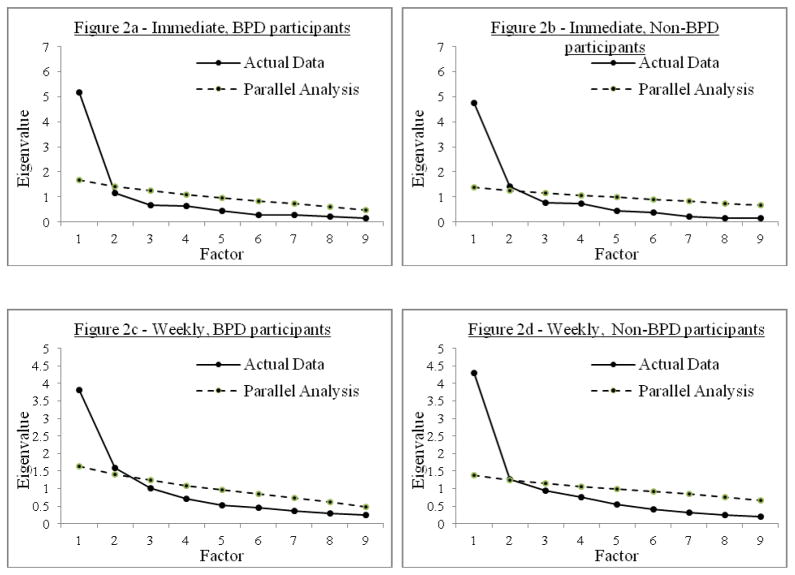
Secondary Analyses: Comparisons Across Diagnostic Groups
Factor analyses using the same guidelines as the primary analyses were run separately for participants diagnosed with and without BPD (see Table 3 for descriptive statistics by diagnostic group). Presented in Figure 2, scree plots again reveal clear one-factor structures replicated across four of the six factor analyses; both diagnostic groups had unidimensional structures for weekly and immediate reports (Figures 2a–2d)4. Within each diagnostic group, the factors from the weekly and immediate reports converged robustly (see Table 2 for cross-method congruence coefficients and inter-factor correlations). Moreover, the factors were highly similar across groups (φ for weekly = .98; φ for immediate = .98). For example, unstable affect and suicide/self-harm were the lowest loading symptoms in both groups’ weekly reports, and paranoid ideation and unstable relationships were among the highest loading symptoms for both groups’ immediate reports.
Table 3.
Descriptive Statistics by Diagnostic Subgroup
| Assessment Method | BPD Participants
|
Non-BPD Participants
|
|---|---|---|
| Symptom | Mean (SD) | Mean (SD) |
| Immediate (N = 58 & 149) | ||
| 1. Unstable Relationships | 1.02 (.80) | .23(.42) |
| 2. Abandonment | .88 (1.05) | .16(.44) |
| 3. Unstable Affect | 1.57 (1.03) | .48(.63) |
| 4. Emptiness/Hollow | 1.34 (.97) | .32(.63) |
| 5. Unstable Identity | .87 (.82) | .18(.44) |
| 6. Uncontrollable Anger | .81 (.79) | .23(.39) |
| 7. Paranoid Ideation | .76 (.84) | .18(.36) |
| 8. Suicide/Self-Harm | .15 (.23) | .02(.09) |
| 9. Impulsivity | .82 (.78) | .24(.43) |
| Weekly (N=62 & 158) | ||
| 1. Unstable Relationships | 1.50 (1.19) | .51(.81) |
| 2. Abandonment | 1.47 (1.36) | .41(.82) |
| 3. Unstable Affect | .66 (.88) | .22(.54) |
| 4. Emptiness/Hollow | 2.32 (1.43) | .84(1.13) |
| 5. Unstable Identity | 1.37 (1.25) | .34(.67) |
| 6. Uncontrollable Anger | 1.75 (1.49) | .49(.91) |
| 7. Paranoid Ideation | 1.50 (1.39) | .57(.86) |
| 8. Suicide/Self-Harm | .20 (.56) | .02(.15) |
| 9. Impulsivity | 1.31 (1.22) | .64(.96) |
| Retrospective (N = 86 & 195) | ||
| 1. Unstable Relationships | 2.09 (1.01) | .59(.85) |
| 2. Abandonment | 1.65 (1.25) | .45(.79) |
| 3. Unstable Affect | 2.44 (.74) | .81(.97) |
| 4. Emptiness/Hollow | 1.71 (1.16) | .44(.72) |
| 5. Unstable Identity | 1.56 (1.29) | .14(.46) |
| 6. Uncontrollable Anger | 2.38 (.722) | 1.17(1.00) |
| 7. Paranoid Ideation | 1.94 (1.37) | .58(1.10) |
| 8. Suicide/Self-Harm | 2.01 (1.18) | .45(.86) |
| 9. Impulsivity | 2.30 (.98) | 1.2(1.13) |
Figure 2.
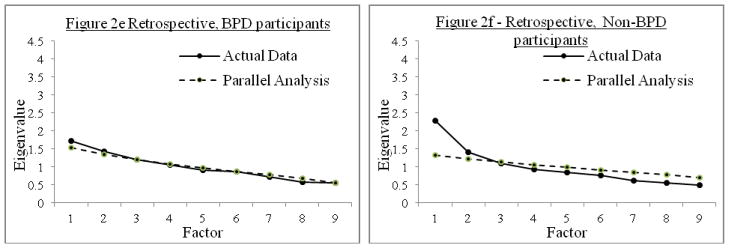
EFA of BPD Symptoms Within Diagnostic Groups
Results within diagnostic groups were less clear for the clinical interview. The BPD group seemed to have no clear factor structure for the SIDP-IV, as shown by the screen plot in Figure 2e and by the fact that all actual eigenvalues were nearly identical to corresponding random-data eigenvalues. This lack of clear factorial structure reflects a general lack of correlation among the SIDP-IV symptoms in the BPD group – the mean symptom inter-correlation was only r̄ = .07. We examined whether this lack of inter-correlation reflected restricted ranges, with mixed results. On one hand, standard deviations of symptoms within the BPD group (average SD = 1.07) were close to those in the entire sample (average SD = 1.15), suggesting no restriction of range. On the other hand, the standard deviation of the sum of raw symptom scores (each on a 0–3 scale) was somewhat lower in the BPD group (SD = 4.09) than in the entire sample (SD = 6.95). Similarly, the standard deviation of the total number of symptoms (0–9) was noticeably lower in the BPD (SD = 1.38) than in the entire sample (SD = 2.60). The latter two findings do suggest some restriction of range in the BPD group SIDP scores. A similar pattern of standard deviations was identified in the non-BPD group. Despite this, and in contrast to the lack of structure in the BPD subgroup, the non-BPD subgroup’s results (Figure 2f) somewhat suggest a one factor solution, though not as robustly as for other analyses. Again, the first eigenvalue differed from its corresponding random-data eigenvalue, though the difference was less than in other analyses, while the second eigenvalue was very close to its corresponding random-data value. Examining the non-BPD group’s potential one-factor solution further, congruence coefficients suggest fair (φ = .90) to strong (φ = .96) similarity between the SIDP-IV factor and the group’s weekly and immediate factors, respectively (See Table 2).
Discussion
In three very different methods of assessment and across diagnostic groups, this research identified a one-factor structure for BPD symptoms. Moreover, the nature of these factors was similar across assessment methods. Results replicated across broad and narrow timeframes, across distal and proximal reporting perspectives, and across clinician-administered and self-report measures. Thus, diverse methods converged on essentially the same single dimension of BPD symptoms. Results also revealed similar one-factor structures within diagnostic groups, for at least two assessment methods. Overall, the current results correspond strongly with previous studies identifying a unidimensional structure of BPD symptoms (Clifton & Pilkonis, 2007; Fossati et al., 1999; Johansen et al., 2004; Sanislow et al., 2002).
Considered alongside previous evidence of a unidimensional structure, current results have several implications. First, they suggest that BPD is not heterogeneous, in terms of the nine definitional criteria in the DSM – people who tend to experience relatively high levels of one symptom tend to experience relatively high levels of all other symptoms. These results argue against the existence of separate facets of BPD symptoms and against subtypes of BPD with differing symptom configurations. Second, a single factor suggests that assessment and treatment focus on a single, coherent form of borderline pathology. The findings argue against the need to create new multidimensional diagnostic tools or to develop new treatments tailored for different “types” of BPD. Third, researchers and clinicians interested in different timeframes of symptom experiences can proceed knowing that BPD pathology is structured similarly regardless of the timeframe. This argues against a frequency-based bias in broad or narrow methods of assessment, at least in terms of reflecting individual differences in BPD. It suggests, for example, that BPD symptoms assessed at different timeframes will likely be comparable in terms of their dimensionality, having similar meaning, despite potential variability in symptom frequency. Indeed, the cross-method correlations between symptoms and between factor scores indicate substantial convergence among the three methods of assessment. Fourth, convergence across diagnostic subgroups suggests a form of continuity in BPD. The similar structures of BPD symptoms across the BPD group and the Non-BPD group indicate that the elements of the disorder themselves operate similarly (in the sense of their internal structure) at both clinical and non-clinical levels, rather than reflecting categorically-different constructs.
The primary exception to unidimensionality occurred with the BPD group’s scores on the SIDP, with no coherent factor structure emerging. This finding might reflect a psychometric issue with the groups or analysis (e.g., restriction of range, relatively small sample size), or a quality of the SIDP-IV, with broad summary measures more generally, or with retrospective reporting biases. To evaluate this in further depth, we examined an additional summary/retrospective measure – an 18-month retrospective measure of BPD symptoms – that participants completed at the beginning of the study (immediately prior to completing the clinical interview, weekly assessments, or immediate assessments). This assessment included the same symptom descriptions as the weekly and immediate assessments and was based on the same 6-point scale (0=Never, 1=Once or twice, etc.), with ratings made in terms of the previous 18 months (e.g., “An interpersonal relationship of mine was unstable and intense in the last 18 months”). Factor analyses of these 18-month retrospective assessments revealed robust unidimensionality for the entire sample (first 3 eigenvalues = 5.556, .597, .527), as well as for the BPD group (first 3 eigenvalues = 4.359, .944, .657) and the non-BPD group (first 3 eigenvalues = 5.194, .715, .641).
Thus, the lack of unidimensionality among subgroups’ SIDP scores may not reflect a general lack of unidimensionality in retrospective or broad summary methods of assessment. More likely, the current SIDP findings within subgroups are at least partially driven by some restriction of range. Moreover, there is some robust evidence of unidimensionality in past studies that have examined broad retrospective assessments. However, if some retrospectively-oriented assessments do have structures that are ambiguous within diagnostic groups, then a study focused on only one diagnostic group might well produce an ambiguous factor structure (as in the current study) or would identify a particular structure based on idiosyncracies of those data. Clarification of this issue requires further examination, potentially clarifying the divergent findings across previous studies.
Our results differ from several previous studies reporting multidimensional structures (Becker et al., 2006; Benazzi, 2006; Blais et al., 1997; Bradley et al., 2005; Clarkin et al., 1993; Hallquist & Pilkonis, 2012; Lewis et al., 2012; Rosenberger & Miller, 1989; Sanislow et al., 2000; Sanislow et al., 2002; Taylor & Reeves, 2007; Whewell et al., 2000; Wright et al., 2013). Unfortunately, there is ambiguity in interpreting some of these previous findings. For example, not all studies provided enough information to evaluate the clarity of particular structure (e.g., scree plots and/or eigenvalues were not always presented). In addition, some studies did not examine or report correlations among the various factors. Some studies, for example, imposed orthogonal rotations which resulted in substantial cross-loadings of symptoms. This creates ambiguity in the meaning and distinction between factors. Other studies used oblique rotations, but did not report inter-factor correlations. Such information is crucial when evaluating the overall factor structure, because substantial inter-factor correlations would indicate that the factors are not very different from each other, potentially indicating that those apparently different factors truly represent a single fundamental factor. Indeed, some research finds extremely large inter-factor correlations in a multidimensional structure. For example, Sanislow et al. (2002) report a three-factor structure among the symptoms, but the inter-factor correlations were extremely high, at .90, .94, and .99. Such results might well be better evidence of unidimensionality than of multidimensionality. Perhaps not surprisingly, considering the extremely large inter-factor correlations, Sanislow et al. (2002) also reported compelling evidence for a one-factor structure.
Although there is ambiguity regarding some of these previous studies, the multidimensionality observed in other studies is likely linked to the range of variables examined. For example, in examinations of all DSM-based personality disorder symptoms (i.e., going beyond those specifically linked to BPD), some research indicates five (Nestadt et al., 2006), seven (Trull, Vergés, Wood, Jahng, & Sher, 2012), eight (Blais & Malone, 2013), or even ten factors (Huprich, Schmitt, Richard, Chelminski, & Zimmerman, 2010), with BPD symptoms often cross-loading with other PD symptoms and/or loading mostly on different factors. Similarly, in other examinations of clinically-relevant criteria beyond BPD, some studies have identified BPD subtypes. For example, Wright and colleagues identified six subtypes of BPD, Hallquist and Pilkonis identified four subtypes, and Bradley et al. identified four subtypes, based on a variety of different measures related to personality pathology. Thus, going beyond the DSM criteria for BPD seems to provide a different perspective on the structure of BPD symptoms and the heterogeneity of people with BPD, as compared to focusing squarely on BPD criteria. This warrants further research and conceptual integration with the clear unidimensionality observed when focusing solely on the DSM’s criteria for BPD.
Although we view our results as generally robust evidence of unidimensionality, we take previous findings of multidimensionality seriously. Therefore, we explored more deeply the possibility of multidimensionality in our data. In cases where more than one dimension was even partially suggested, we examined additional factors (see footnote 4), but results reinforced unidimensionality. Specifically, the multidimensional solutions produced correlated factors that were inconsistent across subsamples and that were not highly consistent with previous multidimensional findings. These findings, along with the scree plots and parallel analyses, therefore, suggested that a one-factor structure was the clearest and most appropriate solution.
There are at least two limitations or caveats that merit attention in future research. First, although this was a secondary issue, this study was the first to systematically compare the symptom structure among participants diagnosed with and without BPD; however, subgroup sample size (N=84 for the BPD subgroup) imply that these comparisons should be examined further. Although our BPD subgroup was similar in size to some previous factor analytic examinations of individuals with BPD (Lewis et al., 2012; N = 95) and, in fact, larger than other such examinations (Bradley et al., 2005; N = 55), larger sample sizes would provide greater precision in estimating and comparing subgroup factor structures.
Second, our general evidence of unidimensionality hinges, in part, on the congruence of factor structures across methods and diagnostic samples. Some readers might note that, though the congruence coefficients are themselves generally quite high, the patterns of factor loadings differ between somewhat the methods. For example, as shown in Table 1, the symptoms loading most strongly on the clinical interview’s factor are not necessarily those loading most strongly on the immediate assessment’s factor (i.e., the correlation between clinical interview and immediate assessment factor loadings from Table 1 is only r = .11). This apparent disconnect between congruence coefficients and “pattern similarity correlations” arises because congruence coefficients reflect three values: a) average magnitudes of loadings, b) variability among loadings, and c) the similarity in the “pattern” of loadings. Table 1 shows that all symptoms load robustly on the factors (mean = .69, min = .32, max = .88) and that there is relatively little variability in the loadings within a factor (Mean Absolute Deviations are .06, .15, and .07 for clinical interviews, weeklies, and immediate assessments, respectively). In computing congruence coefficients, these two facts (i.e., large magnitudes and limited variability in loadings) outweigh the fact that symptoms do not load in the identical pattern. Conceptually, given that all symptoms load strongly and to fairly similar levels, the precise order in which they load has little practical psychological or psychometric implication. This is underscored by the fact that, when factor scores are computed and correlated, the inter-factor correlations are generally quite robust (Table 2).
In sum, the current study provides evidence of unidimensionality among the DSM-defined symptoms of BPD, with results replicated across three methods and (generally) across levels of borderline severity. These results converge with similar previous findings suggesting that BPD is a coherent, unitary disorder, with no robust facet or subtypes defined by unique combinations or configurations of DSM symptoms.
Acknowledgments
This work was supported by the National Institute of Mental Health Grant R01 MH70571. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Jennifer L. Wages and Michelle Anderson for their valuable assistance.
Footnotes
Some researchers have alternatively used latent class analysis (Bornovalova at al., 2010; Shevlin, Dorahy, Adamson, & Murphy, 2007), factor mixture modeling (Hallquist & Pilkonis, 2012) or cluster analysis – (Grinker, Werble, & Drye, 1968) to examine heterogeneity of BPD DSM-based criteria. However, such approaches differentiate people from each other, rather than symptoms. Moreover, latent class analyses have tended to identify groups of people having different degrees of BPD symptomatology, without strong differentiation between “types” or “classes” of BPD.
For other purposes, half of the participants did not complete ESM reports of suicide-related items (leaving 17 items related to BPD symptoms for these participants). To account for this, subsequent factor analyses used pairwise deletion to allow all available data to be included in analyses.
We examined SIDP’s symptom structure in two additional ways, using Mplus 7. First, we examined raw symptom scores as ordinal variables, using polychoric correlations. Second, we examined symptoms in terms of the SIDP-IV’s dichotomous scoring guidelines, where symptoms’ original values of 0 and 1 are treated as “symptom absent” and values of 2 and 3 are treated as “symptom present.” Based on the recommended robust weighted least squares estimators for both analyses (Muthen & Muthen, 1998–2012), results were consistent with those reported in the text, for both the entire sample and the subgroup analyses.
Although the 2nd-factor eigenvalues were slightly larger than their corresponding random-data eigenvalues in Figure 2c and 2f, these differences are so small as to provide very weak evidence of a meaningful second factor in either case. Given the weakness of any such second factor and a preference for parsimony, we believe that a one-factor solution is the superior structure. However, for exploratory purposes, we examined 2-factor solutions in both cases. For weekly reports in the BPD subgroup, Factor 1 partially reflected interpersonal difficulties and identity disturbance, while Factor 2 partially reflected dysregulation (interfactor r = .29). For ESM reports in the non-BPD subgroup, Factor 1 primarily reflected identity disturbance and paranoia, while Factor 2 primarily reflected anger and emotionality (interfactor r = .51).
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. (DSM-5) [Google Scholar]
- Becker DF, McGlashan TH, Grilo CM. Exploratory factor analysis of borderline personality disorder criteria in hospitalized adolescents. Comprehensive Psychiatry. 2006;47:99–105. doi: 10.1016/j.comppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Benazzi F. Borderline personality-bipolar spectrum relationship. Progress in Neuro Psychopharmacology & Biological Psychiatry. 2006;30:68–74. doi: 10.1016/j.pnpbp.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Blais MA, Hilsenroth MJ, Castlebury FD. Content validity of the DSM IV borderline and narcissistic personality disorder criteria sets. Comprehensive Psychiatry. 1997;38:31–37. doi: 10.1016/s0010-440x(97)90050-x. [DOI] [PubMed] [Google Scholar]
- Blais MA, Malone JC. Structure of the DSM-IV personality disorders as revealed in clinician ratings. Comprehensive Psychiatry. 2013;54:326–333. doi: 10.1016/j.comppsych.2012.10.014. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Levy R, Gratz KL, Lejuez CW. Understanding the heterogeneity of BPD symptoms through latent class analysis: Initial results and clinical correlates among inner city substance users. Psychological Assessment. 2010;22:233–245. doi: 10.1037/a0018493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R, Conklin CZ, Westen D. The borderline personality diagnosis in adolescents: Gender differences and subtypes. Journal of Child Psychology and Psychiatry. 2005;46:1006–1019. doi: 10.1111/j.1469-7610.2004.00401.x. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Hull JW, Hurt SW. Factor structure of borderline personality disorder criteria. Journal of Personality Disorders. 1993;7:137–143. [Google Scholar]
- Clifton A, Pilkonis PA. Evidence for a single latent class of Diagnostic and Statistical Manual of Mental Disorders borderline personality pathology. Comprehensive Psychiatry. 2007;48:70–78. doi: 10.1016/j.comppsych.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Conner TS, Tennen H, Fleeson W, Barrett LF. Experience sampling methods: A modern idiographic approach to personality research. Social and Personality Psychology Compass. 2009;3:292–313. doi: 10.1111/j.1751-9004.2009.00170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Kuo J, Welch SS, Thielgen T, Witte S, Bohus M, Linehan MM. A valence-dependent group-specific recall bias of retrospective self-reports: A study of borderline personality disorder in everyday life. Journal of Nervous and Mental Disease. 2006;194:774–779. doi: 10.1097/01.nmd.0000239900.46595.72. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Trull TJ. Ambulatory assessment: An innovative and promising approach for clinical psychology. European Psychologist. 2009;14:109–119. [Google Scholar]
- Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4:272–299. [Google Scholar]
- Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995;7:286–299. [Google Scholar]
- Fossati A, Maffei C, Bagnato M, Donati D, Namia C, Novella L. Latent structure analysis of DSM-IV borderline personality disorder criteria. Comprehensive Psychiatry. 1999;40:72–79. doi: 10.1016/s0010-440x(99)90080-9. [DOI] [PubMed] [Google Scholar]
- Furr RM. Personality psychology as a truly behavioural science. European Journal of Personality. 2009;23:369–401. [Google Scholar]
- Hallquist MN, Pilkonis PA. Refining the phenotype of borderline personality disorder: Diagnostic criteria and beyond. Personality Disorders: Theory, Research, and Treatment. 2012;3:228–246. doi: 10.1037/a0027953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayton JC, Allen DG, Scarpello V. Factor retention decisions in exploratory factor analysis: A tutorial on parallel analysis. Organizational Research Methods. 2004;7:191–205. [Google Scholar]
- Huprich SK, Schmitt TA, Richard DCS, Chelminski I, Zimmerman MA. Comparing factor analytic models of the DSM-IV personality disorders. Personality Disorders: Theory, Research, and Treatment. 2010;1:22–37. doi: 10.1037/a0018245. [DOI] [PubMed] [Google Scholar]
- Grinker RR, Werble B, Drye RC. The borderline syndrome: A behavioral study of ego-functions. New York: Basic Books; 1968. [Google Scholar]
- Johansen MM, Karterud SS, Pedersen GG, Gude TT, Falkum EE. An investigation of the prototype validity of the borderline DSM-IV construct. Acta Psychiatrica Scandinavica. 2004;109:289–298. doi: 10.1046/j.1600-0447.2003.00268.x. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Skodol AE, Livesley WJ, Shrout PE, Huang Y. Synthesizing dimensional and categorical approaches to personality disorders: Refining the research agenda for DSM-V Axis II. International Journal of Methods in Psychiatric Research. 2007;16(Suppl 1):S65–73. doi: 10.1002/mpr.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leihener F, Wagner A, Haaf B, Schmidt C, Lieb K, Stieglitz R, Bohus M. Subtype differentiation of patients with borderline personality disorder using a circumplex model of interpersonal behavior. Journal of Nervous and Mental Disease. 2003;191:248–254. doi: 10.1097/01.NMD.0000061150.38924.2A. [DOI] [PubMed] [Google Scholar]
- Lenzenweger MF, Clarkin JF, Yeomans FE, Kernberg OF, Levy KN. Refining the borderline personality disorder phenotype through finite mixture modeling: Implications for classification. Journal of Personality Disorders. 2008;22:313–331. doi: 10.1521/pedi.2008.22.4.313. [DOI] [PubMed] [Google Scholar]
- Lewis K, Caputi P, Grenyer FS. Borderline personality disorder subtypes: A factor analysis of the DSM-IV criteria. Personality and Mental Health. 2012 doi:10.1002.pmh.1183. [Google Scholar]
- Lorenzo-Seva U, ten Berge JF. Tucker’s congruence coefficient as a meaningful index of factor similarity. Methodology: European Journal of Research Methods For The Behavioral And Social Sciences. 2006;2:57–64. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, van Os J. Experience sampling research in psychopathology: Opening the black box of daily life. Psychological Medicine. 2009;39:1533–1547. doi: 10.1017/S0033291708004947. [DOI] [PubMed] [Google Scholar]
- Nestadt G, Hsu FC, Samuels J, Bienvenu OJ, Reti I, Costa PT, Eaton WW. Latent structure of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition personality disorder criteria. Comprehensive Psychiatry. 2006;47:54–62. doi: 10.1016/j.comppsych.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured Interview for DSM-IV Personality Disorders (SIDP-IV) Washington, DC: American Psychiatric Association; 1995. [Google Scholar]
- Rosenberger PH, Miller GA. Comparing borderline definitions: DSM-III borderline and schizotypal personality disorders. Journal of Abnormal Psychology. 1989;98:161–169. doi: 10.1037//0021-843x.98.2.161. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Grilo CM, McGlashan TH. Factor analysis of the DSM III-R borderline personality disorder criteria in psychiatric inpatients. The American Journal of Psychiatry. 2000;157:1629–1633. doi: 10.1176/appi.ajp.157.10.1629. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, et al. Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: Findings from the Collaborative Longitudinal Personality Disorders Study. The American Journal of Psychiatry. 2002;159:284–290. doi: 10.1176/appi.ajp.159.2.284. [DOI] [PubMed] [Google Scholar]
- Shevlin M, Dorahy M, Adamson G, Murphy J. Subtypes of borderline personality disorder, associated clinical disorders and stressful life-events: A latent class analysis based on the British Psychiatric Morbidity Survey. British Journal of Clinical Psychology. 2007;46:273–281. doi: 10.1348/014466506x150291. [DOI] [PubMed] [Google Scholar]
- Taylor J, Reeves M. Structure of borderline personality disorder symptoms in a nonclinical sample. Journal of Clinical Psychology. 2007;63:805–816. doi: 10.1002/jclp.20398. [DOI] [PubMed] [Google Scholar]
- Trull T, Vergés A, Wood PK, Jahng S, Sher KJ. The structure of diagnostic and statistical manual of mental disorders (4th edition, text revision) personality disorder symptoms in a large national sample. Personality Disorders: Theory, Research, and Treatment. 2012;3:355–369. doi: 10.1037/a0027766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker LR. A method for the synthesis of factor analysis studies. Washington: Department of the Army; 1951. Personnel Research Section Report No. 984. [Google Scholar]
- Whewell P, Ryman AA, Bonanno DD, Heather NN. Does the ICD 10 classification accurately describe subtypes of borderline personality disorder? British Journal of Medical Psychology. 2000;73:483–494. doi: 10.1348/000711200160679. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Livesley WJ, Clark LA. An integrative dimensional classification of personality disorder. Psychological Assessment. 2009;21:243–55. doi: 10.1037/a0016606. [DOI] [PubMed] [Google Scholar]
- Wright AGC, Hallquist MN, Morse JQ, Scott LN, Stepp SD, Nolf KA, Pilkonis PA. Clarifying the interpersonal heterogeneity in borderline personality disorder using latent mixture modeling. Journal of Personality Disorders. 2013;27:125–142. doi: 10.1521/pedi.2013.27.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Vujanovic A, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J. A screening measure for BPD: The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) Journal of Personality Disorders. 2003;17:568–573. doi: 10.1521/pedi.17.6.568.25355. [DOI] [PubMed] [Google Scholar]