Abstract
Eosinophils are granulocytes integral to allergic inflammation and parasitic responses and comprise 1–4% of the circulating leukocytes in human beings under normal conditions. Isolation of human eosinophils allows for ex vivo and in vitro experimentation, providing a valuable tool for the study of allergic mechanisms. Here, we describe a technique for the isolation of human eosinophils by negative selection from whole blood obtained by venipuncture.
Keywords: Eosinophils, Cell separation/instrumentation, Cell separation/methods, Granulocytes, Humans
1 Introduction
Negative selection methods have allowed investigators to obtain purified populations of eosinophils from both normal and eosinophilic human donors [2–4]. The resulting availability of human eosinophils has directly led to a wide range of ex vivo and in vitro studies that have greatly enhanced understanding of human eosinophil immunobiology [1, 5].
In this protocol, we describe the use of a commercially available negative selection system from StemCell Technologies. Prior to employing magnetic negative selection, an enriched granulocyte population is obtained from whole blood obtained by venipuncture through a series of steps. Red blood cells are first depleted by dextran sedimentation. After depletion of red blood cells, an enriched granulocyte population is then obtained by density gradient separation. Granulocytes are then incubated with an antibody cocktail against multiple surface antigens found on specific non-eosinophil blood components, including neutrophils (CD16), monocytes (CD14), lymphocytes (CD2), natural killer cells (CD56), and red blood cells (glycophorin A), allowing for efficient negative selection. These antibodies also specifically bind to the dextran-based magnetic colloid with which the granulocyte suspension is subsequently incubated [6]. When the cell suspension is passed through a magnetized steel mesh column, the antibody- bound non-eosinophil blood cells are trapped in the column. The purified eosinophil population flows through unhindered and is collected.
Of note, other commercially available negative selection products are available, including products from Miltenyi Biotec and R&D Systems. We have chosen to describe eosinophil isolation using the column-based StemCell system based on the routine use of this product in our laboratory. Non-column-based negative selection systems are also available.
2 Materials
All reagents and equipment coming into contact with live cells must be sterile, and proper sterile technique should be followed accordingly.
2.1 Blood Donation
Human blood donor (see Note 1).
Butterfly needle (with Luer-lock compatibility) for venipuncture, 19-gauge.
Sterile Luer-lock syringes, 60 ml (1–8 syringes depending on volume of blood drawn, see Note 2).
Alcohol wipe.
Gauze.
Rubber tourniquet.
Adhesive bandage.
Sodium citrate: 3.2 % (w/v) solution in water (see Note 3).
2.2 Eosinophil Purification
Dextran 70 (Pharmacosmos, Denmark): 6 % (w/v) solution in 0.9 % sodium chloride (see Note 4).
Ficoll-Paque Premium.
Hanks’ Buffer Salt Solution, without calcium or magnesium (HBSS).
Ovalbumin for Separation Medium (see Note 5).
Parafilm.
Conical polypropylene centrifuge tubes, 50 ml.
Sterile disposable transfer pipets.
Turk Blood Diluting Fluid (Ricca Chemical Company).
Hemocytometer for cell counting.
Magnet for cell separation (see Note 6).
Cell separation magnetic column (StemCell Technologies, size will depend size of granulocyte input).
Three-way Luer-lock stopcock.
Sterile Luer-lock syringe, 10 ml.
Negative selection antibody cocktail (StemCell Technologies).
Magnetic colloid (StemCell Technologies).
Hema 3 Staining Kit (Fisher Scientific).
3 Methods
3.1 Blood Draw
Bring sodium citrate solution, dextran, and Ficoll-Paque to room temperature.
Fill 60 ml syringes each with 10 ml of sodium citrate solution in a tissue culture hood. One syringe should be used for each 40 ml of blood drawn (up to 320 ml, see Note 2).
Apply tourniquet to the arm of the donor and wipe the antecubital fossa with an alcohol pad. Allow alcohol to dry prior to venipuncture.
Attach 60 ml syringe to a 19-gauge butterfly needle and draw blood from an antecubital vein by venipuncture.
Fill each syringe with 40 ml of blood by applying gentle negative pressure with the plunger of the syringe. (This will bring the total volume in each syringe to 50 ml). Pinch off the butterfly when switching to subsequent Luer-lock syringes to avoid blood spillage.
Remove tourniquet after filling final syringe.
Remove butterfly needle and apply pressure with gauze to achieve hemostasis.
Apply adhesive bandage to venipuncture site.
3.2 Eosinophil Purification
Move syringes to a tissue culture hood and add 10 ml of dextran solution to each syringe. Dextran can be drawn into the syringes using a fresh Luer-lock butterfly needle, taking care to maintain sterility of the needle tip and the dextran solution. Introduction of any air bubbles into the syringes should also be avoided to the greatest extent possible as well.
Gently mix syringes by holding a piece of Parafilm over the open Luer-lock end and inverting ten times.
Place syringes standing upright in the hood in a compatible rack and allow red blood cells to settle for approximately 40 min. Approximately 20–25 ml of red blood cell-depleted straw-colored fluid will form as the upper layer (see Note 7).
Remove the needle from a new butterfly infusion set and attach to the first syringe. Keeping the syringe upright and taking care not to disturb the interface between the two layers, collect the straw-colored layer by pushing through the tubing and into a 50 ml conical tube. Take care to not collect any material from the red cell layer to minimize red cell contamination. Discard red cell layer in an appropriate biohazard container. Repeat for each syringe (Fractions from separate syringes may be combined in the collection process in order to minimize the number of conical tubes needed at this step).
Fill fresh 50 ml conical tubes each with 23 ml of Ficoll-Paque Premium. The number of tubes used will depend on the amount of straw-colored layer collected. Using a serological pipette, carefully layer the straw-colored fluid over the Ficoll-Paque in an approximately 1:1 ratio (about 20–25 ml per conical tube). Take care to minimize any disturbance in the interface between the two layers when pipetting.
Carefully transfer the conical tubes to the centrifuge and centrifuge for 20 min at 300 × g at room temperature. Use the lowest acceleration and deceleration setting (no brake) available on the centrifuge (For subsequent centrifugation steps, mid-range acceleration and deceleration settings may be used).
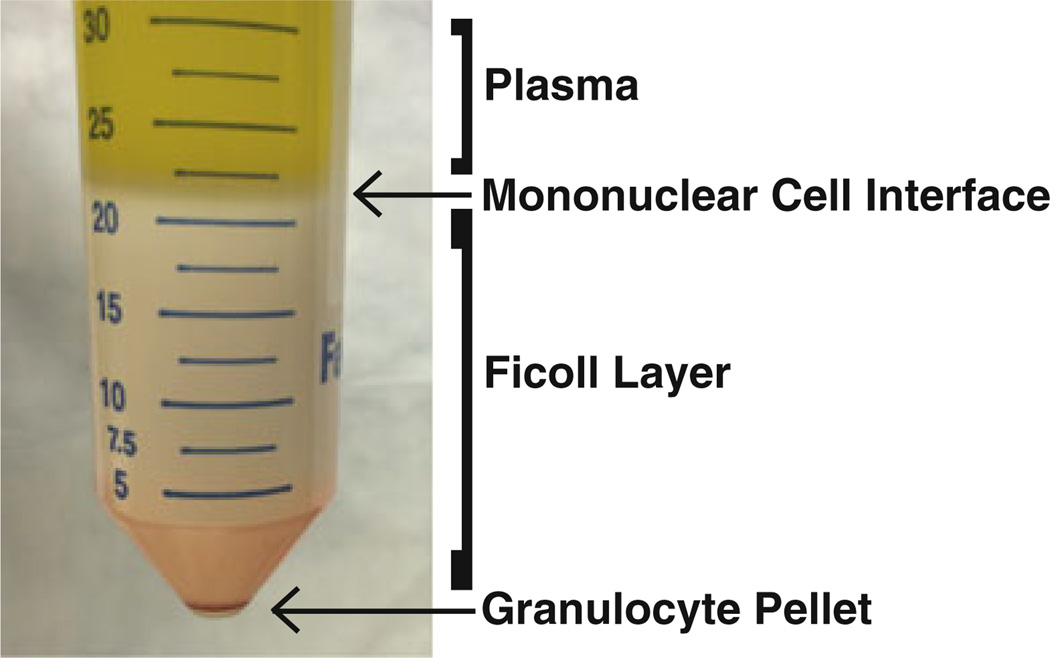
Granulocytes, consisting of eosinophils and neutrophils, will be pelleted at the bottom of the conical tube at the bottom of the Ficoll-Paque layer. Immediately above the Ficoll-Paque layer will be a pale whitish interface consisting of mononuclear cells, with a true plasma layer formed above the monocyte layer (Fig. 1).
Aspirate the plasma layer using a vacuum apparatus with a clean pipette tip (The same tip may be used for the plasma layer for all tubes if care is made maintain sterility between tubes). Using a fresh pipette tip, then aspirate the mononuclear cell layer. Again using a fresh pipette tip, aspirate the Ficoll layer down to the granulocyte pellet, taking care to not contact the pellet with the pipette tip.
Using a transfer pipette, resuspend the granulocyte pellet with 1 ml of ice-cold sterile HBSS. Minimize contact of the transfer pipette with the walls of the conical tube in the interest of avoiding contamination with mononuclear cells that may be adherent to the wall of the tube. From this point forward, all steps will be done on ice.
Transfer and combine the resuspended pellets to a new 50 ml conical tube containing 30 ml of ice-cold sterile HBSS. In order to maximize cell recovery, the bottom of the tubes containing granulocyte pellets may be washed with an additional 1 ml HBSS which is then transferred to the new conical tube. Bring the total volume of the new conical tube up to 50 ml with ice-cold sterile HBSS after granulocyte transfer.
Centrifuge at 300 × g for 5 min at 4 °C. Remove supernatant and discard, resuspend pellet, and refill tube to 50 ml with ice-cold HBSS (see Note 8).
Count granulocytes using a hemocytometer. Dilute the aliquot of granulocyte suspension used for counting 1:1 in Turk Blood Diluting Fluid prior to counting in order to lyse red blood cells (see Note 9).
Centrifuge at 300 × g for 5 min at 4 °C. Remove supernatant and discard.
Resuspend granulocyte pellet in 1 ml of separation medium per 50 × 106 granulocytes (from count obtained in step 20).
Add 100 µl of negative selection antibody cocktail per ml of cell suspension in separation medium. Incubate for 20 min on ice.
Add 60 µl of magnetic colloid per ml of cell suspension. Incubate for 20 min on ice with periodic manual gentle agitation to prevent settling of the magnetic colloid.
During the incubation with magnetic colloid, set up the negative selection column. Attach a three-way Luer lock stopcock to the end of the column, and prime the column with about 12 ml of separation medium through the side port of the three-way stopcock using a 10 ml Luer lock syringe. Attach a 21-guage needle to unoccupied end of the stopcock. Open the stopcock to the needle and allow the liquid level to drop to just above the level of the metallic mesh and close stopcock. Insert column into the magnet, which should be located in either a cold room or a refrigerated cabinet.
Load the top of the column with the cell suspension and open the stopcock, collecting the effluent in a 50 ml conical tube. Continue to add cell suspension followed by 20 ml of separation medium to the top of the column without allowing any of the metal mesh to run dry until all the liquid has passed through the column (see Note 10). The effluent will contain the purified eosinophil population.
Count eosinophils in the effluent using a hemocytometer (see Note 11).
Centrifuge eosinophils at 300 × g for 5 min at 4 °C. Discard supernatant and resuspend in desired volume of HBSS. Purified eosinophils are ready for experimental use.
Fig. 1.
Appearance of conical tube after Ficoll-Paque density gradient separation
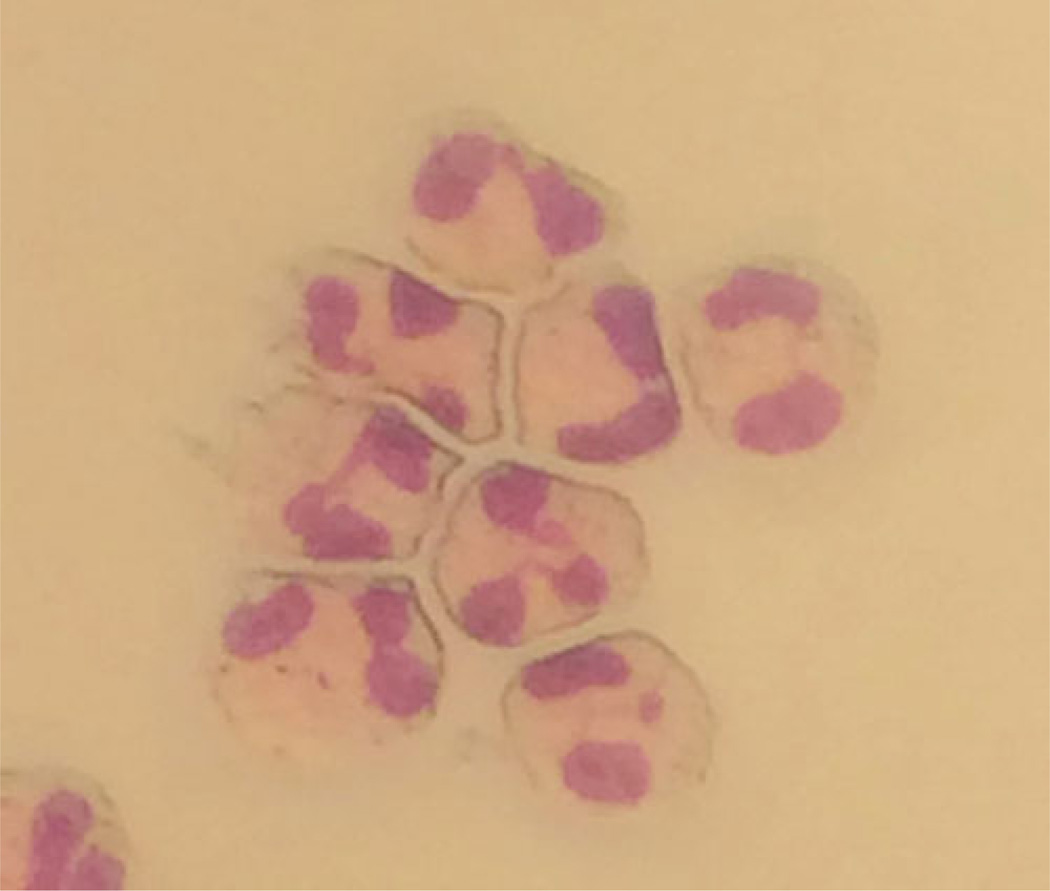
Fig. 2.
Cytocentrifuge slide of purified eosinophils prepared with Hema 3 staining, 40× objective
Acknowledgments
This work was supported by a HOPE Pilot Grant from the American Partnership for Eosinophilic Disorders (to PA) and National Institutes of Health grants R01AI051645 and R37AI020241 (to PFW).
Footnotes
A human blood donor is required for this protocol. Blood must be drawn by trained personnel after informed consent is obtained under the auspices of a study approved by the investigator’s Institutional Review Board (or equivalent).
We recommend that no more than 320 ml of blood is drawn from a human volunteer at a time. Though adjustments may be made depending on the volume of blood drawn, male volunteers should not donate blood more frequently than every 2 months, while female volunteers should not donate blood more frequently than every 3 months. The primary purpose of this restriction is to avoid anemia.
We use commercially available 4 % (w/v) sodium citrate solution (Sigma Aldrich) that is diluted to 3.2 % in sterile water in a tissue culture hood. Sterile water is added to 4 % sodium citrate in a ratio of 1:4 to arrive at the desired concentration. The solution should be stored at 4 °C and brought to room temperature prior to use in this protocol. Alternatively, sodium citrate solution can be made by combining 37.3 g of sodium citrate powder and 8 g of citric acid in 500 ml of distilled water. Adjust pH to 5.2 with sodium hydroxide, filter sterilize (0.22 µm pore size), and store at 4 °C.
The 6 % dextran 70 solution is used for red blood cell sedimentation. Alternatively, 6 % hetastarch may be used in a buffered formulation available from StemCell Technologies. However, the use of hetastarch may affect eosinophil granule morphology [7].
Separation medium consists of 0.5 % (w/v) of Grade V ovalbumin in HBSS without calcium or magnesium. A 5× stock solution of 2.5 % (w/v) ovalbumin in HBSS may be made and stored in aliquots at −20 °C.
Our laboratory uses a magnet from StemCell Technologies that can fit their 0.5-in. or 0.6-in. columns.
This is not truly plasma because it contains cellular components, including eosinophils and other leukocytes.
Because the negative selection protocol efficiently removes red blood cells under most circumstances, we do not recommend routine red blood cell lysis with hypotonic saline. However, if lysis must be performed to ensure an eosinophil population completely devoid of red blood cells, it can occur at this point prior to resuspension of the granulocyte pellet in HBSS. We recommend hypotonic saline lysis and recommend against the use of ammonium chloride, as exposure to ammonium chloride will effect eosinophil functional responses [8, 9]. Resuspend the granulocyte pellet in 20–25 ml of 0.2 % sodium chloride. Within 30 s, add an equal volume of 1.6 % sodium chloride. Centrifuge at 300 × g for 5 min at 4 °C. Discard supernatant and wash pellet in 50 ml of HBSS. Repeat centrifugation and wash before proceeding with the remainder of the protocol.
This dilution must be accounted for in calculating the number total granulocytes. The cell suspension may be made more dilute if necessary to facilitate counting on the hemocytometer.
The size of the column used will depend on the number of granulocytes counted. The 0.5-inch column is designed to process 50–300 × 106 granulocytes; the 0.6-inch column is designed to process 100–1,500 × 106 granulocytes.
We also recommend assessment of eosinophil purity by examination of a cytocentrifuge slide prepared with Hema 3 staining (similar to Wright-Giemsa staining) and assessment of viability by Trypan Blue staining. Eosinophils will demonstrate purple bilobed (or multilobed) nuclei with pink granular cytoplasmic staining with the Hema 3 stain (Fig. 2).
References
- 1.Rosenberg H, Dyer K, Foster P. Eosinophils: changing perspectives in health and disease. Nat Rev Immunol. 2013;13:9–22. doi: 10.1038/nri3341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansel T, Pound J, Thompson R. Isolation of eosinophils from human blood. J Immunol Methods. 1990;127:153–164. doi: 10.1016/0022-1759(90)90064-3. [DOI] [PubMed] [Google Scholar]
- 3.Hansel T, de Vries I, Iff T, et al. An improved immunomagnetic procedure for the isolation of highly purified human blood eosinophils. J Immunol Methods. 1991;145:105–110. doi: 10.1016/0022-1759(91)90315-7. [DOI] [PubMed] [Google Scholar]
- 4.Miltenyi S, Müller W, Weichel W, et al. High gradient magnetic cell separation with MACS. Cytometry. 1990;11:231–238. doi: 10.1002/cyto.990110203. [DOI] [PubMed] [Google Scholar]
- 5.Rothenberg M, Hogan S. The eosinophil. Annu Rev Immunol. 2006;24:147–174. doi: 10.1146/annurev.immunol.24.021605.090720. [DOI] [PubMed] [Google Scholar]
- 6.Lansdorp P, Thomas T. Purification and analysis of bispecific tetrameric antibody complexes. Mol Immunol. 1990;27:659–666. doi: 10.1016/0161-5890(90)90009-o. [DOI] [PubMed] [Google Scholar]
- 7.Jackson M, Millar A, Dawes J, et al. Neutrophil activation during cell separation procedures. Nucl Med Commun. 1989;10:901–904. doi: 10.1097/00006231-198912000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Ide M, Weiler D, Kita H, et al. Ammonium chloride exposure inhibits cytokine-mediated eosinophil survival. J Immunol Methods. 1994;168:187–196. doi: 10.1016/0022-1759(94)90054-x. [DOI] [PubMed] [Google Scholar]
- 9.Wang H, Ghiran I, Matthaei K, et al. Airway eosinophils: allergic inflammation recruited professional antigen-presenting cells. J Immunol. 2007;179:7585–7592. doi: 10.4049/jimmunol.179.11.7585. [DOI] [PMC free article] [PubMed] [Google Scholar]