Abstract
Background. After 2 decades of focused efforts to eradicate polio, the impact of eradication activities on health systems continues to be controversial. This study evaluated the impact of polio eradication activities on routine immunization (RI) and primary healthcare (PHC).
Methods. Quantitative analysis assessed the effects of polio eradication campaigns on RI and maternal healthcare coverage. A systematic qualitative analysis in 7 countries in South Asia and sub-Saharan Africa assessed impacts of polio eradication activities on key health system functions, using data from interviews, participant observation, and document review.
Results. Our quantitative analysis did not find compelling evidence of widespread and significant effects of polio eradication campaigns, either positive or negative, on measures of RI and maternal healthcare. Our qualitative analysis revealed context-specific positive impacts of polio eradication activities in many of our case studies, particularly disease surveillance and cold chain strengthening. These impacts were dependent on the initiative of policy makers. Negative impacts, including service interruption and public dissatisfaction, were observed primarily in districts with many campaigns per year.
Conclusions. Polio eradication activities can provide support for RI and PHC, but many opportunities to do so remain missed. Increased commitment to scaling up best practices could lead to significant positive impacts.
Keywords: poliomyelitis, eradication, routine immunization, health systems
The goal of polio eradication has mobilized an extensive effort involving most of the world's countries: over the last 20 years, mass polio vaccination campaigns have delivered around 20 billion doses of polio vaccine to children across the globe and have succeeded in interrupting transmission in all but 3 countries. Polio eradication gained international support in the late 1980s in part because of the argument that eradication activities could mobilize support and resources for routine immunization (RI) and primary healthcare (PHC) [1–5]. But whether the effects of polio eradication campaigns—and their attendant planning, monitoring, and surveillance activities—on health systems have proved positive or negative has been debated ever since [6–8].
Small-scale studies of the effect of polio eradication activities on RI and PHC have provided equivocal or mixed results [9–12]. A large-scale study in the 1980s found a positive effect of polio eradication activities on health systems in the Americas, but health infrastructure in most of these countries was already strong relative to that in developing countries in Asia and Africa [13]. Studies in Egypt, the Philippines, and the World Health Organization's (WHO's) Western Pacific Region in the mid-1990s showed that the initial implementation of polio eradication activities had positive effects on immunization more generally [14–16].
A study in Tanzania, Nepal, and the Lao People's Democratic Republic (PDR) performed in the late 1990s showed that polio eradication activities had a mix of effects that varied depending on context, with the most short-term benefits occurring in countries such as Lao PDR, where existing health services were at the time extremely limited [17–19]. Another study, in India, found positive effects in a number of arenas but noted some negative impacts due to disruption of normal activities caused by the campaigns [17, 19]. These studies showed that the relationship between polio eradication activities and other health services was highly context dependent. A systematic analysis to determine where and when polio eradication activities have positively and negatively impacted RI and PHC was needed.
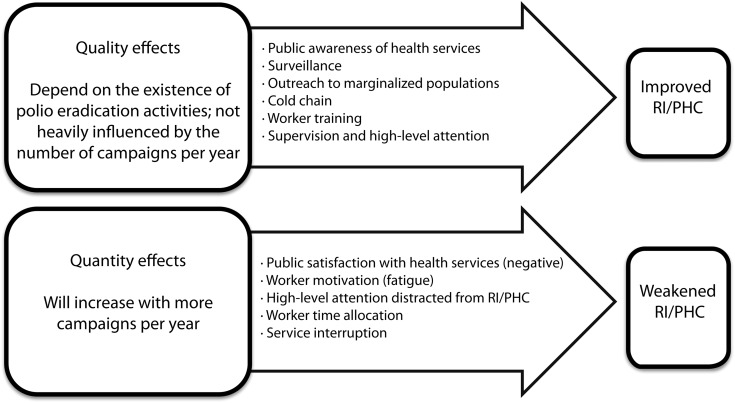
This study quantitatively evaluated the effects of (1) the initial scale-up of polio eradication activities and (2) the number of polio vaccination campaigns per year on measures of RI and PHC. The study also qualitatively examined potential mediators of these relationships in 8 district-level case studies in 7 countries in Africa and South Asia. Our hypotheses are summarized in Figure 1.
Figure 1.
Study hypotheses. Abbreviations: PHC, primary healthcare; RI, routine immunization.
METHODS
We used a combination of qualitative and quantitative methods to examine the relationship between polio eradication activities, RI, and PHC. This research was approved by the Middlebury College Institutional Review Board. Informed consent was obtained from all participants. A detailed description of our methods is available in an open-access article [20], and the full qualitative protocol is accessible online (available at: http://sites.middlebury.edu/polio_eradication_impacts_study/qualitative-research-guide/).
Quantitative Analysis
In a global cross-national time series analysis, we evaluated (1) a hypothesized “scale-up” effect of polio immunization campaigns involving an initial benefit to RI and PHC and (2) the impact of campaign intensity, or number of campaigns. The Supplementary Materials contain further technical details about the global analysis and information on 4 country-specific analyses.
Our analyses used multiple regression to examine the degree to which polio eradication campaigns explain observed rates of change in diphtheria-tetanus-pertussis (DTP3) vaccination and attended birth coverage. The 3 dependent variables were DTP3 vaccine coverage estimates from the WHO and UNICEF (United Nations Children's Fund), from 1990–2010; DTP3 vaccine coverage estimates from the Institute for Health Metrics and Evaluation (IHME), from 1995–2006 [21–24]; and attended birth coverage from the World Bank's World Development Indicators, from 1996–2010 [25]. We operationalized campaign intensity, our independent variable, in 2 ways: the number of polio eradication campaigns per year, and the cumulative percentage of the under-five population targeted by polio eradication campaigns in a given year. The regressions controlled for (1) the initial levels of the dependent variable; (2) political instability, regime type, and wealth and education levels [26–28]; (3) other health financing [29, 30]; and (4) the number of nonpolio health campaigns.
By use of R [31], models were fit with each of the 3 different dependent variables to examine the effect of each of the 2 different measures of campaign intensity. For each of these models, we proceeded by first fitting a parsimonious baseline model, using step-down regression, to explain country-wise variability in the dependent variable in terms of the control variables. Then, the resulting baseline model was augmented with one of the measures of campaign intensity to evaluate its additional explanatory power. We used the resulting full model to evaluate the magnitude and direction of the partial effect of polio eradication activities.
Qualitative Case Studies
Our qualitative work was performed in 8 districts evenly divided between South Asia and sub-Saharan Africa (Figure 2). Six-week case studies provided an in-depth understanding of the relationship between polio eradication, RI, and PHC within the focal district, not the entire country. Case study districts were purposively selected on the basis of specific guidelines described in our published protocol. Our case studies are drawn from regions with ongoing polio eradication activities and do not represent the current or historical experience of regions of the world (such as the Americas or Southeast Asia) where polio was eliminated relatively quickly.
Figure 2.
Qualitative case studies.
To ensure that we collected comparable information in each site, we followed a standardized protocol involving a comprehensive document review; semistructured interviews with approximately 50 respondents, including community members, ground-level staff, and district and national leadership; and participant observation in polio eradication, RI, and PHC activities. While the protocol included national-level interviews and document review, we focused on evaluating impacts at the district level. The Qualitative Research Guide contains a full description of our qualitative methods [29]. We coded all documents, interview transcripts, and field notes, using the qualitative analysis program NVivo [32], and compared key variables across the case studies.
A Note on PHC
While we endorse the broad definition of PHC framed at Alma-Ata, we used maternal health indicators as a proxy for PHC in our quantitative work because there exist few other reasonably reliable and comparable indicators of PHC across time and space. In qualitative work, we defined PHC as the provision of healthcare at the basic health unit level and below, including services provided by community health workers. We also considered health education, nutrition, and water and sanitation. We did not evaluate the impacts of polio eradication on other vertical programs, such as measles campaigns.
RESULTS
Quantitative Findings
Impact of the Initiation of Polio Eradication Activities
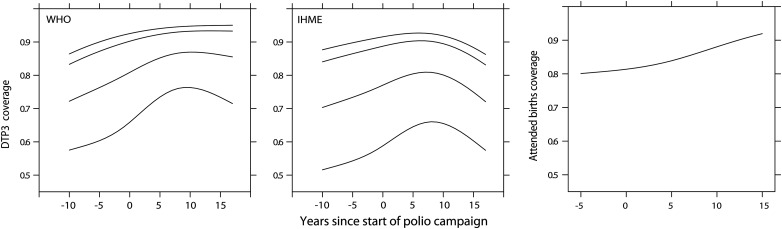
The start of polio eradication efforts was associated with an increase in DTP3 vaccine coverage, especially for countries that had low initial values of DTP3 vaccine coverage. Similarly, there was an increase in attended birth coverage (Figure 3).
Figure 3.
Association between the onset of polio eradication campaigns and diphtheria-tetanus-pertussis (DTP3) vaccine coverage from 2 different sources, the World Health Organization (WHO; left side) and the Institute for Health Metrics and Evaluation (IHME; middle), and attended birth coverage, from the World Bank's World Development Indicators (right side). Each line depicts the predicted values from regression models fit to restricted cubic splines in the presence of covariates. All additional covariates were set at median values. Lines indicate quintiles of initial values of coverage (at time 0), showing that the change in coverage over time depends on the initial coverage.
However, these increases began prior to the onset of polio eradication campaigns and were sustained for ∼10 years following the onset of campaigns. This suggests that other factors, unaccounted for in our suite of contextual variables, were also driving DTP3 and attended birth coverage during this time. Most countries in our analysis initiated polio eradication campaigns around the same time (in approximately 1996). Thus, any effects of widespread temporal trends, such as decentralization initiatives or global policy shifts regarding RI, will also be correlated with initiation of campaigns. We therefore cannot attribute the changes shown here to initiation of polio eradication campaigns.
Impact of Number of Campaigns Per Year
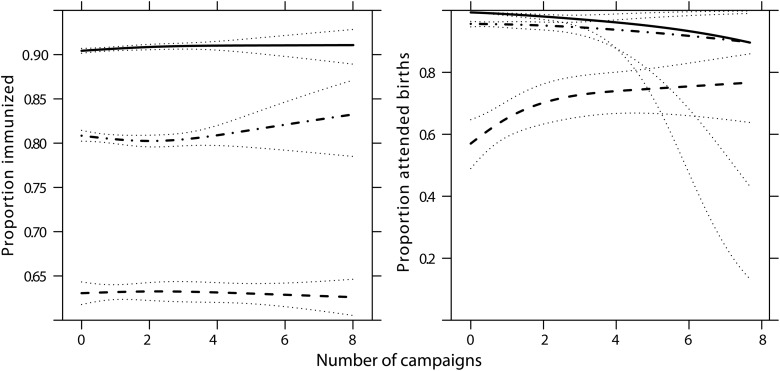
For models explaining DTP3 vaccine coverage as estimated by the IHME and attended births (but not for DTP3 vaccine coverage as estimated by the WHO), the best fitting models included a measure of campaign intensity. However, while statistically significant, campaign intensity explained a very small proportion of the total variation in coverage. Most of the variation (as measured by r2) was explained by the lagged dependent variable alone.
Campaign intensity was associated with changes in DTP3 vaccine coverage (using the IHME but not the WHO/UNICEF coverage estimates), but these changes were so small that they are unlikely to be meaningful (Figure 4). While larger effects were seen for attended births, they were still almost entirely within the range of the 95% confidence interval. A lack of observations at high levels of campaign intensity (as illustrated by the very wide confidence intervals in the right panel) complicates interpretation of this analysis. Notably, polio campaign intensity tends to be highest in areas with low levels of coverage of RI and attended births, creating a persistent selection bias.
Figure 4.
Association between polio eradication campaign intensity and diphtheria-tetanus-pertussis vaccine coverage (data are from the Institute for Health Metrics and Evaluation, IHME; left side) and on attended birth coverage (right side). Thick lines indicate different levels of initial coverage (first quartile, median, and third quartile). Dotted lines represent 95% confidence intervals. Partial effects for both dependent variables were very similar for an alternate measure of campaign intensity, percentage of population targeted (not shown). The very wide confidence intervals in the right panel for higher initial values of coverage (dot-dash and solid lines) indicate a lack of observations at high levels of campaign intensity for countries. This selection bias complicates interpretation of this analysis.
Overall, we consider the results of our quantitative analysis inconclusive. To the degree that polio eradication campaigns have an effect on outcomes in RI and maternal healthcare, these effects are small relative to other factors and are inconsistent from place to place.
Positive Impacts on RI and PHC in the Qualitative Case Studies
Across our case studies, polio eradication built impressive global systems for service delivery and monitoring. With the exception of supports to the cold chain, these systems were usually parallel to RI and PHC delivery and monitoring systems.
Although we observed positive impacts across our case studies, polio eradication had the most beneficial effects overall in case studies with health systems that were relatively strong. The effects we observed in our study districts are highly context specific and cannot be assumed to be the same dynamics at play in a given country as a whole. The information presented here is a highly condensed and simplified description of a set of complex processes, and we urge readers to consult the Supplementary Materials for more-detailed information. In the following sections, we address each column of Figure 5 in turn.
Figure 5.
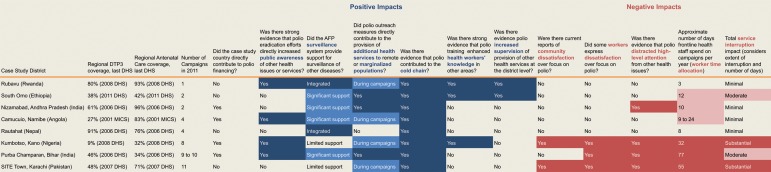
Results of qualitative analysis. Please refer to the end of the Supplementary Materials for definitions of the categories used in the figure.
Public Awareness of Health Services
Public awareness of vaccination and health services had increased markedly in the past 15 years in many of our case studies. Polio eradication activities made some contributions to this increase in awareness but were not the only or primary contributing factor in any case study.
In most case studies, polio's social mobilization materials focused solely on polio vaccination. Notable exceptions were social mobilization surrounding Immunization Plus Days in Kumbotso, Nigeria, and the integrated communication provided under India's 107 Block Plan (see Case 1). In Camucuio, Angola, and Rubavu, Rwanda, respondents noted that polio campaigns provided an opportunity for face-to-face communication about RI and other health services.
Surveillance
The acute flaccid paralysis (AFP) surveillance systems in each case study save Rwanda were largely managed by WHO staff at the national level. Each of our case study countries also had a government surveillance system (or >1, in most cases), which ranged widely in quality.
When viewed across the case studies, the AFP surveillance system was high quality. In Angola, Ethiopia, India, and Nepal, the AFP system provided a base for additional disease surveillance. However, despite some system overlap, many of the surveillance protocols for AFP, including monitoring and reporting forms, remained separate. The Nepal system was unusual in using a single form for surveillance of AFP along with other diseases or conditions (see Case 2).
Outreach to Marginalized Populations
In most of our case studies, people working on polio eradication found, mapped, and repeatedly visited populations that were previously unreached by other health services. The maps and information created by polio eradication teams in the districts we studied represent a likely unprecedented collection of information on populations—including urban slum populations, pastoralists, and socially marginalized groups—most marginalized from health services.
The extent to which this often detailed information was used to provide other health services to these populations varied widely across case studies. In Purba Champaran, Bihar, India, residents of “high-risk” blocks were provided with a wide range of health education and services in addition to polio vaccination (see Case 1). In the case of Kumbotso, Nigeria, integrated campaigns provided additional health services to these populations, and in some other case studies, these populations received vitamin A or other interventions during polio vaccination campaigns. Polio eradication's extensive information on and outreach to the world's most underserved populations were not routinely used to reach those populations outside of campaigns in the majority of case studies.
Cold Chain
The cold chain was the only example of a system essential to polio eradication that was truly integrated with other health services. The same freezers were used for polio and other vaccines in all case studies, and portable vaccine carriers were shared in many case studies, including Rautahat, Nepal, and Camucuio, Angola.
Polio eradication funds provided key improvements to the cold chain system. When polio eradication campaigns started in the mid-1990s, they substantially strengthened the cold chain in many areas. Polio funds have since been used for significant cold chain upgrades, as well as ongoing repair and maintenance, in many case studies. In all cases, these cold chain improvements also benefited RI. Also in all cases, polio was not the sole contributor to cold chain creation or maintenance.
Worker Training
In all of our case studies, staff working on polio campaigns were trained prior to each campaign. In part because polio campaigns in Kumbotso, Nigeria, and Rubavu, Rwanda, also provide other services to the public, training materials in these case studies laid out clear plans to transfer additional knowledge and skills to workers. Also, trainings for surveillance-related activities were sometimes integrated with other trainings. However, in the majority of case studies, campaign trainings focused only on polio-related information, missing opportunities to broaden worker knowledge—and in some cases contributing to worker fatigue through repetition.
Supervision
Across our case studies, polio received as much or more attention than any other health issue from high-level officials, including visits to the district from health and political leaders at national and regional levels. In some case studies, these officials used this opportunity to bring attention to and to supervise other health services. In most cases, however, these campaign-related visits focused only on polio.
Intensity-Related Effects in Our Case Studies
There were several observable effects of the number of campaigns per year, and most negative effects were seen in case studies with frequent campaigns. Because all case studies with a high number of campaigns had relatively weak provision of other health services, the effects we describe here are the result of a high intensity of campaigns interacting with weak health systems.
Community Satisfaction
Overall satisfaction with health services across our case studies was, perhaps not surprisingly, linked primarily to the quality of those services, not to polio activities. In 4 case studies (Purba Champaran, Bihar; SITE Town, Pakistan; Kumbotso, Nigeria; and Camucuio, Angola), community members raised questions about why polio campaigns were so frequent. In 2, SITE Town and Kumbotso, there was evidence that a perceived focus on polio over other health services led to public dissatisfaction.
SITE Town and Kumbotso are in regions that harbor polio transmission and have weak provision of other health services (the regional DTP3 vaccine coverage was <50% in the last Demographic and Health Survey). The high level of commitment, funding, and service provision in the case of polio, when compared with poor provision of other services, was cause for public complaint. Specifically, lack of medications at basic health posts and lack of basic sanitation services were repeatedly contrasted with door-to-door administration of polio vaccine. This dynamic also contributed to public distrust of polio vaccination in these case studies.
Such sentiments were not observed in districts with 2 campaigns per year, even in cases where provision of other services was weak. While people might be dissatisfied with health services in these areas, they did not link this dissatisfaction to polio campaigns.
Worker Satisfaction and Motivation
In case studies with ≤4 campaigns per year, the effects of the polio program on worker motivation were generally neutral or slightly positive. In areas with many campaigns per year, polio eradication had more complex and sometimes detrimental effects on worker motivation. Fatigue due to repeated campaigns was mentioned in all case studies with >4 campaigns per year.
National Focus on Polio
International attention has focused on countries that still harbor polio transmission. In India, Pakistan, and Nigeria, there was evidence that this focus on polio diverted attention from other health issues. In SITE Town and Kumbutso, prioritizing polio eradication was largely driven by international pressure, rather than by the desires of communities, local health staff, or district health leadership.
Worker Time Allocation
Government RI and PHC staff worked in all case studies as vaccinators and/or supervisors on polio campaigns. In addition, across all case studies, the polio program has trained large groups of staff from outside the health department, commonly referred to as volunteers. The extent of time health and other staff devoted to polio eradication, however, varied widely. In some case studies, it consumed a significant amount of worker time, as in Purba Champaran, Bihar, India, where many frontline health workers devoted >70 days per year to polio campaigns.
In all case studies, the WHO and UNICEF provided polio-funded staff whose primary goal was to focus on polio eradication; these workers spent significant time outside of campaigns on RI and PHC work. For example, in Nepal, 60 WHO staff and 14 UNICEF staff (many of whom are funded by the polio program) provide some support for RI and PHC activities. However, this is far outweighed by the time spent by government health workers on polio campaigns in our case studies. In Nepal, >92 000 government workers contribute time to polio eradication. Thus, we conclude that, across our case studies, polio eradication reduced overall worker time available for RI and PHC activities.
Service Interruption
Our 2 case studies in cities with consistent and ongoing polio transmission—SITE Town, Pakistan, and Kumbotso, Nigeria—showed evidence of the most significant campaign-related service interruption. In these locations, services at some (although not all) health posts were not provided during campaigns.
DISCUSSION
Polio eradication's surveillance, communications, and service delivery systems were unmatched in terms of combining quality with reach. In areas with few campaigns per year and with dedicated national governments to build on these systems—as in Rubavu, Rwanda, and South Omo, Ethiopia—polio eradication delivered its most unambiguously positive impacts. Our qualitative work did not examine impacts in parts of the world, such as the Americas, where high levels of RI coverage are the norm and polio campaigns are few. Others have found that polio eradication activities in these areas had broadly positive impacts [13, 14], findings consistent with the patterns we observed.
Not coincidentally, SITE Town, Pakistan, and Kumbotso, Nigeria, the case study districts with ongoing polio transmission, were also home to violent unrest, high levels of poverty, tensions between minority populations and governments, and underresourced health systems. Polio eradication did not create the poor health services in these areas, and we found no compelling evidence that polio eradication activities had widespread negative effects on RI. However, it also did little to change the situation. Community members and health staff were involved in increasingly heavily supervised, well-funded, and repeated polio eradication campaigns, even as basic services remained underfunded and sometimes unprovided. The focus on polio led to public and worker dissatisfaction, and RI remained weak.
In polio's final strongholds—Afghanistan, Pakistan, and Nigeria—community support, worker motivation, and high levels of baseline RI coverage will be critical to secure eradication. It is in these places where polio eradication's infrastructure could most immediately and dramatically benefit RI and PHC. In areas where few other health services are fully functioning, polio eradication has built robust and impressive systems for surveillance, communications, and outreach.
These systems, built and maintained through often heroic effort by individuals involved in polio eradication, could provide strong support for other critical health services. Inspiring best practices observed in our case studies—including the examples in Cases 1 and 2 show that polio eradication can make substantial contributions to health systems. AFP surveillance can be expanded to include robust surveillance for other diseases. Outreach to marginalized populations can provide bed nets and oral rehydration solution. Communications materials can educate about vaccines and breast-feeding. Applying the resolve and dedication that characterizes polio eradication to a wider suite of services could provide communities with the services they are demanding, give workers a fresh reason for enthusiasm, and increase baseline RI coverage. The eradication of polio would probably not be far behind.
CASE 1: THE 107 BLOCK PLAN
India's 107 Block Plan began in 2009 from the observation that polio transmission in India was primarily focused in just 107 blocks or subdistricts. In these “high-risk” blocks, the program focused on improving RI, increasing rates of breast-feeding, lowering rates of diarrhea, and improving sanitation practices. The 107 Block Plan included a wide variety of activities, from filling vacant medical officer positions to improving polio campaigns. In this section, we focus on one piece of the 107 Block Plan: its extensive communications strategy.
As part of the 107 Block Plan, polio eradication's communications increased attention to issues beyond polio vaccination—in the words of one interviewee, it was “polio plus plus plus plus.” Targeted messages included information about the benefits, common side effects, and local availability of RI; the importance of oral rehydration solution in cases of diarrhea; instructions to exclusively breast-feed for 6 months; and to wash hands with soap at specific times throughout the day.
Additional staff were hired to disseminate these messages: up to 1500 community mobilizers were deployed in Bihar alone. As a UNICEF official explained, the mobilizers “embraced” this work, owing to excitement that, after years of the same polio messaging, they could do more.
The potential to roll out programs similar to the 107 Block Plan in other polio-endemic areas should be given serious consideration. Still, those familiar with the program caution that its success was dependent on a “very robust” polio program, as well as on government support for programs like RI. For example, in Bihar, the 107 Block Plan coincided with the Muskaan program, which renewed interest in RI at the state level. The 107 Block Plan did not increase RI coverage alone, but rather, in the words of another interviewee, “amplified and supported” other programs.
Still, it is probably not a coincidence that India saw its last polio case within a few years of the inception of the 107 Block Plan. Overall, it is an inspiring example of how polio eradication can spearhead a project that improves RI and PHC, with positive impacts on the polio program, as well.
CASE 2: INTEGRATED DISEASE SURVEILLANCE IN NEPAL
In 2003 and 2004, Nepal integrated measles, neonatal tetanus, and Japanese encephalitis surveillance into the WHO-supported AFP surveillance system designed to detect cases of polio. Surveillance of these diseases, which prior to integration had suffered from a lack of funding and poor reporting compliance, improved markedly. Satisfaction with the system is now high at national, regional, and local levels, and integration of vaccine-preventable disease surveillance is seen as successful—one national official described it as “the only surveillance working.”
The high quality of the surveillance program was attributed to WHO support and oversight. A network of 15 WHO surveillance medical officers, trained in RI management, as well as in surveillance, support the program. In our study district, government health workers reported a good relationship with the WHO officers and satisfaction with the system.
The vaccine-preventable disease surveillance system in Nepal was the most broad and integrated AFP-based surveillance system in our case studies. It uses integrated reporting forms and the same staff for surveillance of 4 diseases or conditions. This streamlined process avoids the duplication of effort that characterized less integrated surveillance systems in our case studies. It demonstrates that commitment to building a strong surveillance system on the polio framework can yield powerful results.
Despite the desires of many in the government and the WHO, the Nepal government had not yet assumed full responsibility for the integrated surveillance system. Many respondents viewed the system as a WHO responsibility and expected that the program would be terminated if and when WHO funding and support end. Thus, the sustainability of the surveillance system is at risk. One national-level respondent said, “There is a good chance when polio funds stop, the surveillance system won't go on any longer.”
Nepal's integrated surveillance system demonstrates that, with committed leadership, polio surveillance can create health system benefits. It is a model worth replicating in areas where other disease surveillance remains weak and the AFP surveillance system is strong. Nevertheless, the purview of Nepal's integrated surveillance system is limited, and its sustainability is in question. There is a need for international institutional support for consolidating and expanding AFP surveillance systems to provide long-term health system gains—and for continued collaboration with governments to transition these systems into capable local hands.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Notes
Acknowledgments. We are grateful to the following individuals for their support of the study: Molly Abbruzzese, Ni'ma Abid, Amina Mohammad Adamu, Samesh Adhikari, Mercy Ahun, Aminu Ali, Aline Bahati, Kate Bass, David Bishai, Altaf Bosan, Logan Brenzel, Hannah Burnett, Marcolino Cambumba, Anna Clements, Bala Danyaro, V. Renuka Devi, Elias Durry, Donatha Dushimimana, Jessie Ebersole, Lisa Emmer, Michal Fishman, Marta Gacic-Dobo, Maurice Gatera, Lenette Golding, Nicole Grohoski, John Grove, Suraj Gurau, Melkam Hailom, Robel Hailom, Karin Hanta, Obaid ul Islam, Aline Ikirezi, Radha Jayannagari, Sarwat Jehan, Hannah Judge, Innocent Kabayiza, Farhat Khan, Alyssa Lowe, Meghan Lynch, Anil Menon, Zubair Mufti, Clotilde Muhimpundu, Maikano Madaki, Assumpta Mukabutera, Agnes Mukamana, Marie Jeanne Mukarwego, Joseph Murwanyi, Angèle Musabyimana, Eularie Mutamuliza, Aminu Ahmed Musa, Wadood Myireh, Grace Natson, Fidele Ngabo, Joseph Ngamije, Aftab Pasha, Muhammad Pate, Quan Pham, Allison Prather, K. Srinivas Rao, Marty Roper, Joel Rugomboka, William Schluter, Benjamin Schwartz, Isabel Shaw, Simarjit Singh, Ali Sohail, Jessica Stevens, Shiva Prasad Subedi, Marie Claire Umuhoza, Béata Umutesi, Shyam Raj Upreti, Théophila Uwanyiligira, Linda Venczel, Lucio Verani, Dora Ward, Chris Wolff, Naziru Mohammed Zakari, and Rahel Zewengel.
Financial support. This work was supported by the Bill and Melinda Gates Foundation (contract 20333).
Supplement sponsorship. This article is part of a supplement entitled “The Final Phase of Polio Eradication and Endgame Strategies for the Post-Eradication Era,” which was sponsored by the Centers for Disease Control and Prevention.
Potential conflicts of interest. S. C. received travel funding or held consultancies with the Independent Monitoring Board for polio eradication and with UNICEF. A. K. worked as a consultant for a separate division of the WHO in 2012. R. G. provided technical assistance to the government of Andhra Pradesh, India. P. T. held a Rotary Ambassadorial Scholarship. N. T. received travel funding from the GAVI Secretariat. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.De Quadros C. Onward towards victory. In: Daniel TM, Robbins FC, editors. Polio. Rochester: University of Rochester Press; 1997. pp. 181–98. [Google Scholar]
- 2.Hampton L. Albert Sabin and the Coalition to Eliminate Polio from the Americas. Am J Public Health. 2009;99:34–44. doi: 10.2105/AJPH.2007.117952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Risi JB. Poliomyelitis in Brazil. In: Daniel TM, Robbins FC, editors. Polio. Rochester: Rochester University Press; 1997. pp. 159–80. [Google Scholar]
- 4.Aylward RB, Acharya A, England S. Global health goals: lessons from the worldwide effort to eradicate poliomyelitis. Lancet. 2003;364:909–14. doi: 10.1016/S0140-6736(03)14337-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Assembly. Global eradication of poliomyelitis by the year 2000. Geneva: Forty-First World Health Assembly; 1988. [Google Scholar]
- 6.Sutter RW, Cochi SL. Ethical dilemmas in worldwide polio eradication programs. Am J Public Health. 1997;87:913–6. doi: 10.2105/ajph.87.6.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JW, Melgaard B, Hull HF, Barakamfitiye D, Okwo-Bele JM. On the other hand: ethical dilemmas in polio eradication. Am J Public Health. 1998;88:130–1. doi: 10.2105/ajph.88.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor CE, Cutts F, Taylor ME. Ethical dilemmas in current planning for polio eradication. Am J Public Health. 1997;87:922–5. doi: 10.2105/ajph.87.6.922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dietz V, Cutts F. The use of mass campaigns in the expanded program on immunization: a review of reported advantages and disadvantages. Int J Health Serv. 1997;27:767–90. doi: 10.2190/QPCQ-FBF8-6ABX-2TB5. [DOI] [PubMed] [Google Scholar]
- 10.Levin A, Ram S, Kaddar M. The impact of the global polio eradication initiative on the financing of routine immunization: case studies in Bangladesh, Cote d'Ivoire, and Morocco. Bull World Health Organ. 2002;80:822–8. [PMC free article] [PubMed] [Google Scholar]
- 11.Bonu S, Rani M, Razum O. Global public health mandates in a diverse world: the polio eradication initiative and the expanded programme on immunization in sub-Saharan Africa and South Asia. Health Policy. 2004;70:327–45. doi: 10.1016/j.healthpol.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Bonu S, Rani M, Baker T. The impact of the national polio immunization campaign on levels and equity in immunization coverage: evidence from rural North India. Soc Sci Med. 2003;57:1807–19. doi: 10.1016/s0277-9536(03)00056-x. [DOI] [PubMed] [Google Scholar]
- 13.Pan American Health Organization. Washington, DC: PAHO; 1995. The Impact of the Expanded Program on Immunization and the Polio Eradication Initiative on Health Systems in the Americas: final report of the “Taylor Commission.”. [Google Scholar]
- 14.Aylward B. Strengthening routine immunization services in the Western pacific through the eradication of poliomyelitis. J Infect Dis. 1997;175(suppl 1):S268–71. doi: 10.1093/infdis/175.supplement_1.s268. [DOI] [PubMed] [Google Scholar]
- 15.Tangermann R. Poliomyelitis eradication and its impact on PHC in the Philippines. J Infect Dis. 1997;175(suppl 1):S272–6. doi: 10.1093/infdis/175.supplement_1.s272. [DOI] [PubMed] [Google Scholar]
- 16.Mansour E. Integrated disease control initiatives: polio eradication and neonatal tetanus elimination in Egypt. J Infect Dis. 1997;175(suppl 1):S277–80. doi: 10.1093/infdis/175.supplement_1.s277. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization. Geneva: WHO; 2000. Meeting on the impact of targeted programmes on health systems: a case study of the Polio Eradication Initiative. [Google Scholar]
- 18.Mogedal S, Stenson B. Disease eradication: friend or foe to the health system? Geneva: WHO; 2000. p. 29. [Google Scholar]
- 19.Loevinsohn B, Aylward B, Steinglass R, Ogden E, Goodman T, Melgaard B. Impact of targeted programs on health systems: a case study of the polio eradication initiative. Am J Public Health. 2002;92:19–23. doi: 10.2105/ajph.92.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Closser S, Rosenthal A, Parris T, et al. Methods for evaluating the impact of vertical programs on health systems: protocol for a study on the impact of the global polio eradication initiative on strengthening routine immunization and primary health care. BMC Public Health. 2012;12:728. doi: 10.1186/1471-2458-12-728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Institute for Health Metrics and Evaluation. DTP3 immunization coverage by country 1986–2006. http://www.healthmetricsandevaluation.org/sites/default/files/record-attached-files/IHME_DTP3_IMMUNIZATION_COVERAGE_1986_2006.xls. Accessed 13 March 2012. [Google Scholar]
- 22.World Health Organization, UNICEF. WHO/UNICEF coverage estimates. http://www.who.int/entity/immunization_monitoring/data/coverage_estimates_series.xls. Accessed 13 March 2012. [PMC free article] [PubMed] [Google Scholar]
- 23.Burton A, Monasch R, Lautenbach B, et al. WHO and UNICEF estimates of national infant immunization coverage: methods and processes. Bull World Health Organ. 2009;87:535–41. doi: 10.2471/BLT.08.053819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lim SS, Stein DB, Charrow A, Murray CJ. Tracking progress towards universal childhood immunisation and the impact of global initiatives: a systematic analysis of three-dose diphtheria, tetanus, and pertussis immunisation coverage. Lancet. 2008;372:2031–46. doi: 10.1016/S0140-6736(08)61869-3. [DOI] [PubMed] [Google Scholar]
- 25.World Bank. World development indicators. http://api.worldbank.org/datafiles/SH.STA.BRTC.ZS_Indicator_MetaData_en_EXCEL.xls. Accessed 13 March 2012. [Google Scholar]
- 26.World Bank. World development indicators. http://databank.worldbank.org/databank/download/WDIandGDF_csv.zip. Accessed 5 February 2012. [Google Scholar]
- 27.Political Instability Task Force. Worldwide atrocities dataset. 2011. http://eventdata.psu.edu/data.dir/atrocities.html. Accessed 21 February 2012. [Google Scholar]
- 28.Marshall MG, Jaggers K, Gurr TR. Polity IV project: political regime characteristics and transitions, 1800–2010. Vienna, VA: Center for Systemic Peace; 2011. Dataset user's manual www.systemicpeace.org/polity/polity4.htm . Accessed 21 February 2012. [Google Scholar]
- 29.World Health Organization. Global health observatory data repository. 2011. http://apps.who.int/ghodata. Accessed 7 March 2012. [Google Scholar]
- 30.GAVI Alliance. Disbursements by country. 2012. http://www.gavialliance.org/results/disbursements/ Accessed 15 February 2012. [Google Scholar]
- 31.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. http://www.R-project.org/ . Accessed 4 March 2013. [Google Scholar]
- 32.QSR International. NVivo qualitative data analysis software. 2012. http://www.qsrinternational.com/products_nvivo.aspx . Accessed 4 March 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.