Abstract
Objectives
To determine if clavicle fracture displacement and shortening are different between upright and supine radiographic examinations.
Design
Combined retrospective and prospective comparative study.
Setting
Level I Trauma Center
Patients
Forty-six patients (mean age 49 years, range 24–89 years) with an acute clavicle fracture were evaluated.
Intervention
Standardized clavicle radiographs were obtained in both supine and upright positions for each patient. Displacement and shortening were measured and compared between the two positions.
Main Outcomes Measurements
One resident and three traumatologists classified the fractures and measured displacement and shortening. Data was aggregated and compared to ensure reliability with a two-way mixed intraclass correlation (ICC).
Results
Fracture displacement was significantly greater when measured from upright radiographs (15.9±8.9mm) than from supine radiographs (8.4±6.6mm, p<0.001), representing an 89% increase in displacement with upright positioning. Forty-one percent of patients had greater than 100% displacement on upright, but not on supine radiographs. Compared to the uninjured side, 3.0±10.7mm of shortening was noted on upright radiographs and 1.3±9.5mm of lengthening on supine radiographs (p<0.001). The ICC was 0.82 (95% CI: 0.73–0.89) for OTA fracture classification, 0.81 (95% CI: 0.75–0.87) for vertical displacement, and 0.92 (95% CI: 0.88–0.95) for injured clavicle length, demonstrating very high agreement among evaluators.
Conclusions
Increased fracture displacement and shortening was observed on upright compared to supine radiographs. This suggests that upright radiographs may better demonstrate clavicle displacement and predict the position at healing if nonoperative treatment is selected.
Keywords: Clavicle Fractures, Midshaft clavicle fractures, Displacement, Shortening, radiographs, nonunion
Introduction
Clavicle fractures are a common injury treated by orthopaedic surgeons representing 2.6–10% of all fractures and typically occur in the midshaft.1–3 Nonoperative treatment of these injuries has been the leading treatment method for the latter half of the 20th century; however, recent evidence has led to increased support for operative fixation, especially for displaced midshaft clavicle fractures.4–11 A 2005 systematic review found nonunion rates after non-operative treatment to be 5.9% for all clavicle fractures and 15.1% for displaced midshaft clavicle fractures.5 Moreover, a recent report suggests that fracture displacement and comminution are independent radiographic risk factors for predicting nonunion.11 Several studies have showed improved functional outcomes and decreased nonunion rates with either intramedullary nailing9, 12 or plate and screw fixation8; yet operative management still remains highly controversial.10, 13
The indications for open reduction and internal fixation are evolving. Traditional absolute operative indications include open fractures, neurovascular embarrassment, and threatened skin. Based on current literature, relative indications for fixation also include fractures with greater than 2cm shortening6, vertical displacement greater than 100% of the injured clavicular shaft diameter, severe comminution, young or athletic patients, significant cosmetic deformity, and multi-limb injuries.4 To this end, operative decisions are largely based on radiographic appearance; however, a standardized radiographic protocol has not been established. This is especially pertinent when considering the degree that gravity affects the fracture alignment at the time of radiographic evaluation. Radiographs taken with the patient upright may show greater fracture displacement and better assess trauma energy and soft tissue injury than x-rays taken with the patient supine. If this is true, the patient position at the time of x-ray may affect recommendations regarding the indications for surgery. To our knowledge the effect of patient positioning on clavicle length and fracture fragment displacement has not been studied. We hypothesized that clavicle fracture displacement and shortening measured on upright radiographs would be greater when compared to supine radiographs.
Methods
Patients and Fractures
After obtaining IRB approval, patients treated for clavicle fractures from January 2010 to January 2012 were identified (n=19) from hospital and department records. After January 2012, patients with clavicle fractures were enrolled prospectively (n=27). Forty-six patients age 18 years or greater (average age 49, range 24 – 89) with an acute unilateral clavicle fracture and adequate radiographs that would allow measurement of supine and upright displacement and clavicle length were included for study. At our institution, all patients with acute clavicle injuries are evaluated with a standardized protocol that includes upright and supine anteroposterior (AP) and 30° cephalic tilt radiographs of both clavicles. This protocol was established because it was anecdotally noted that fracture displacement was greater in upright radiographs. Excluded were patients with ipsilateral scapular fractures, patients unable to be positioned upright at the time of initial radiographs, patients who had their injured arm supported on upright images, and patients with insufficient radiographic exams from the time of injury.
All fractures were closed. Twenty-eight fractures were left sided and 18 were right sided. Demographics, including gender and mechanism of injury, of the included patients are further described in Table #1. Twenty-five patients underwent open reduction and internal fixation and the remaining 21 patients were treated non-operatively with sling immobilization followed by early range of motion exercises. Neither analysis of fracture treatment nor patient outcomes were part of the study design.
Table 1.
Patient Demographics
| Number | 46 |
|
| |
| Age (mean, range) | 49 years (24–89 years) |
|
| |
| Gender | 38 Male, 8 female |
|
| |
| Side | 28 Left, 18 Right |
|
| |
| OTA fracture classification | 39 B-type, 7 C-type |
|
| |
| MOI: Number (% of patients) | |
| Bicycle accident or MCC- | 24 (52.2%) |
| MVC- | 10 (21.7%) |
| ATV accident- | 8 (17.4%) |
| Fall*- | 2 (4.3%) |
| Other**- | 2 (4.3%) |
MCC=Motorcycle Collision, MVC=Motor vehicle collision, ATV=All-terrain vehicle.
Four patients sustained a same level fall, 4 patients fell from greater than 4 feet
One patient was assaulted; the other had an I-beam fall on him from 30 feet high
Radiographic Evaluation
Clavicle length and fracture fragment displacement were measured using a picture archiving and communicating system (PACS, EVMS - Emageon Inc., Birmingham, AL). Clavicle length was assessed by measuring the distance between the center of the medial edge at the sternoclavicular joint to the most lateral edge (Figure 1a). When available on the same radiograph (n=24), the contralateral clavicle length was also measured in a similar fashion. In these patients, the injured clavicle length was compared to the contralateral length to determine relative shortening or lengthening. Vertical fracture displacement was measured from the vertical distance between lines drawn co-linear with the long axis of the main medial and lateral fragments (Figure 1b). Both length and vertical displacement measurements were obtained from upright and supine radiographs for each patient. These measurements were taken from either the upright and supine AP view or the upright and supine 30° cephalic tilt view depending on which radiograph showed the greatest displacement. The upright and supine 30° cephalic tilt radiographs were used in 40 of the 46 patients. The Fractures were classified based on the OTA classification system.14 All radiographs were independently evaluated by one resident and three fellowship-trained traumatologists.
Figure 1. Measuring Displacement and Length.


In the top image, displacement is determined by the distance between lines drawn co-linear with the long axis of the medial and lateral fragments. In the bottom image, length is determined by the distance between the medial aspect of the clavicle at the sternoclavicular joint to the most lateral edge
Statistical Analyses
Measurements and fracture classification data was aggregated and compared. Intraclass correlation (ICC) was estimated amongst the four observers for measures of displacement, length, and OTA classification using a two-way, mixed effects model and an absolute agreement definition. The ICC is a common descriptive statistic used to assess the reproducibility of quantitative measurements made by different observers. According to guidelines proposed by Landis and Koch15, an ICC value of less than 0 indicates no agreement, 0–0.20 indicates slight agreement, 0.21–0.40 indicates fair agreement, 0.41–0.60 indicates moderate agreement, 0.61–0.80 indicates substantial agreement, and 0.81–1 indicates almost perfect agreement. Length and displacement values were averaged for each patient. Two-tailed paired samples t-tests were used to compare mean measurements of displacement and length between supine and upright clavicle radiographs. This same analysis was also performed in OTA B-type and C-type clavicle fractures separately. All statistical analyses were performed using a standard software package (IBM SPSS Statistics for Windows, Version 21.0, Armonk, NY).
Results
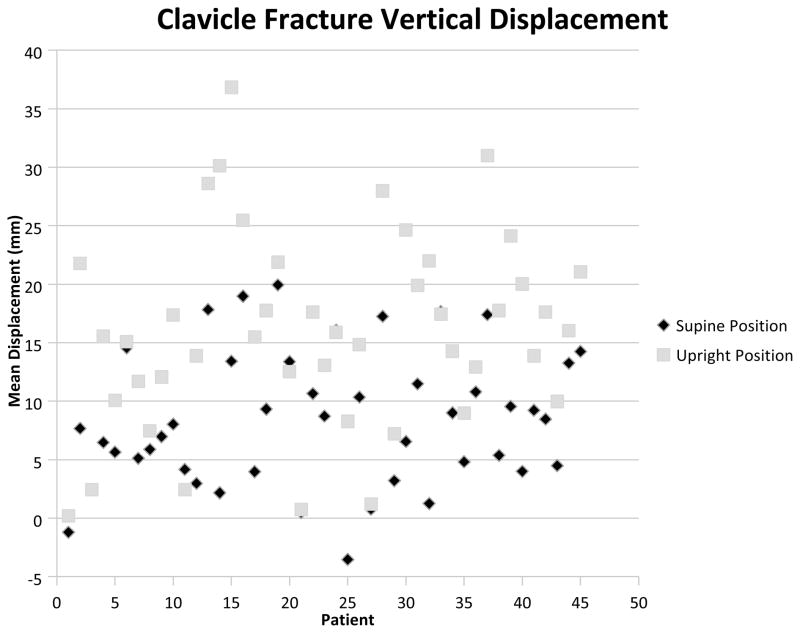
Vertical displacement was significantly greater in upright versus supine films (p<0.001). Supine radiographs had a mean displacement of 8.4±6.6mm and upright radiographs had a mean displacement of 15.9±8.9mm. Displacement increased by an average 7.5mm (89%) in upright films when compared to supine radiographs (figure 2). Furthermore, 44% (20/46) of patients had greater than 100% displacement on upright, but not on supine, radiographs (Figure 3). When displacement was compared among only midshaft clavicle fractures (OTA B-type) an average of (17.1±7.9 mm) displacement was measured on upright radiographs versus 9.0±6.0 mm on supine radiographs (p<0.001). When lateral clavicle fractures (OTA C-type) were evaluated independently, there was an insignificant trend to increased displacement in upright films (9.7±8.6mm upright vs. 5.2±3.2 mm supine; p=0.13); however, this analysis is likely underpowered to determine any real difference. The ICC for vertical fracture displacement among evaluators was 0.81 (95% CI: 0.75–0.87) indicating almost perfect agreement.
Figure 2. Upright vs. supine vertical displacement measurements per patient.
Graphical representation of average vertical displacement in upright and supine radiographs for each patient. A trend line demonstrates that upright radiographs show significantly greater displacement than supine radiographs
Figure 3. Vertical Displacement is increased in upright films.


3A shows an upangle clavicle radiograph with the patient in the upright position. 3B shows a similar upangle clavicle radiograph on the same patient in the supine position.
Statistically significant shortening was noted for upright compared to supine films (p<0.001). The average length of the injured clavicle in upright films was 16.2±1.7 cm compared with 16.8±1.6 cm in supine films. This only represents 6mm (4%) of increased shortening for the injured clavicle seen with upright films and is unlikely to be clinically significant. In the 24 patients where injured clavicle length could be compared to the contralateral side, an average of 3.0±10.7mm of shortening was noted on upright radiographs and 1.3±9.5mm of lengthening on supine radiographs (p<0.001). Although statistically significant, it is still difficult to determine if this 4.3mm difference is clinically significant. When injured clavicle length was compared among only OTA B-type fractures, upright films still showed significant shortening (p<0.01). Mean length was 16.1±1.7 cm for upright radiographs and 16.8±1.6 cm for supine radiographs. Orthopaedic Trauma Association C-type clavicle fractures had essentially no change in length between upright and supine films (17.1±1.4 cm upright vs. 17.2±1.7 cm supine; p=0.82); yet, this analysis is also underpowered. The ICC for clavicle length among evaluators was 0.92 (95% CI: 0.88–0.95) indicating very good agreement.
The ICC for OTA fracture classification identified to the first decimal (eg, 15B-2.2) was 0.78 (95% CI: 0.67–0.86) indicating substantial agreement among evaluators. When the OTA classification is abbreviated to exclude numbers after the decimal point (eg, 15B-2), the ICC increased to 0.82 (95% CI: 0.73–0.89) indicating almost perfect agreement. The majority (n=39) of the fractures were B-type (midshaft) clavicle fractures, with many (31%) being classified as comminuted spiral wedge fractures (15B2.3). There were 7 C-type (lateral) fractures, and no A-type (medial) fractures. Fifty percent (23/46) of fractures were comminuted.
Discussion
The advocation for nonoperative treatment of clavicle fractures was based largely on publications from the 1960’s that reported nonunion rates of less than 1%, and a three-fold higher nonunion rate with operative intervention.16, 17 Patient populations for these studies were ill-defined and may have included both pediatric and adult patients. Recent studies with only adult patients suggest that the nonunion rates of nonoperative treatment are actually much higher than previously reported.4–11 These contemporary studies suggest that operative treatment should be considered for patients, particularly those with displaced midshaft clavicle fractures. The precise indications for operative management are still being debated; but, a standardized imaging protocol would be useful to accurately and reproducibly predict the risk of nonunion and malunion as well as determine the need for operative intervention.
Traditionally, a clavicle series includes a standard AP radiograph and a 30° cephalic tilt view;18 yet, it is unclear if these views taken with the patient supine or upright would yield similar information. It has been suggested previously by Plocher et al19 that fracture displacement may change with patient positioning during radiographic evaluation; however, this question was not directly addressed in this study. The data presented here confirms this assertion and suggests that upright clavicle radiographs better assess maximal fracture displacement when compared to supine films. Average vertical displacement on upright radiographs was 15.9±8.9mm, representing an 89% increase when compared to displacement measured on supine radiographs. Positioning during radiographic examination is therefore important, as many studies have reported an association between initial displacement and increased nonunion rates.4, 16, 20–24 Robinson et al.4 reported an 18.5 fold increase in nonunion likelihood for displaced fractures when compared to non-displaced fractures. Furthermore, a direct relationship has also been established between increased vertical displacement and poor functional outcomes.8 It should be noted that neither of these studies report patient positioning during radiographic analysis; yet, it is clear that accurately determining initial fracture displacement is essential in guiding patient care.
A recent study by Murray et al.11 found fracture displacement to be an independent risk factor in predicting clavicle nonunion when evaluating 941 patients (odds ratio, 1.17). They also created a prognostic “ready reckoner” tool to help estimate the risk fracture nonunion. According to this instrument, a patient with 15mm of fracture displacement has a 3–19% risk of nonunion depending on their smoking status and fracture comminution, whereas a patient with 10mm of fracture displacement had a 2–10% risk of nonunion depending on the same concurrent risk factors. In this study, they determined overall displacement by combining both vertical displacement and shortening; however, the patient positioning was not reported. While it is difficult to use their instrument to analyze our absolute vertical displacement data, it suggests that there is likely a significant difference in predicted nonunion risk between upright and supine films. Furthermore, it is possible that many of the films in their study were taken supine, and therefore underestimated the importance of fracture displacement in predicting nonunion.
Others have suggested that greater than 100% clavicle fracture displacement is also a risk factor for nonunion, and this parameter has subsequently been one factor in determining whether a patient is indicated for operative fixation.4 In our study, 39% of patients had greater than 100% fracture fragment displacement on supine radiographs versus 80% of patients with upright radiographs. Nearly forty-four percent of patients had greater than 100% displacement noted on upright radiographs that was not appreciated on supine films. This further supports the need for this imaging modality.
In the present study, upright clavicle length was 16.2±1.7cm compared with 16.8±1.6 cm in supine films (p<0.001). This represents a 4% increase in clavicle shortening in upright when compared to supine films. Although this was statistically significant, it is unlikely that it has any clinical significance. In an effort to better estimate shortening, difference in length was calculated between injured and contralateral clavicles in 24 patients. This analysis found an average of 3.0±10.7mm of shortening with upright radiographs and 1.3±9.5mm of lengthening on supine radiographs (p<0.001). Again, although this difference was statistically significant, it is difficult to extrapolate the clinical significance of such a small change in clavicle length. In the literature, a significant correlation between shortening at the time of initial evaluation and the development of nonunion has been reported.6 In a study by Hill et al.6, 52 clavicle fractures were followed for an average of 38 months. All patients with greater than 20mm of shortening had a nonunion and these patients reported an unsatisfactory result. Murray et al.11 also found shortening (overlap) to have a significant association with nonunion on bivariate analysis. As mentioned earlier, this measurement was combined with vertical displacement (translation) in their final multivariate analysis.
Two-way mixed Intraclass-correlation found very high agreement among evaluators for OTA fracture classification, vertical displacement measurement, and clavicle length. This supports the assertion that the measuring methods described here are reproducible by orthopaedic surgeons of various levels of experience and training.
There are several limitations in the current study. Determining clavicle length is difficult with plain radiographs. The film exposure and patient positioning affect the ability to obtain accurate measurements. These factors are challenging in an emergency room setting with patients of various body habitus. Larger patients often have soft tissue shadows that conceal the exact location of the medial end of the clavicle and it is difficult to optimize thorax rotation in a patient with a painful shoulder girdle. Anecdotally, we believe these factors led to a wide variation in measured clavicle lengths. Although we report a statistically significant decrease in injured clavicle length, there were many patients who had an increased length on upright films when compared to the contralateral side. These difficulties in obtaining accurate clavicle length likely underestimated the amount shortening that occurs with a clavicle fracture.
Another potential limitation of this study is the lack of radiographic markers to define absolute displacement. We believe this limitation is mitigated due to the focus on relative displacement between views rather than absolute displacement and the ability to use the clavicle diameter as an internal control for vertical displacement.
Additionally, the configuration of many clavicle fractures is difficult to appreciate on two-dimensional radiographs. Three-dimensional computed tomography would provide a more accurate representation of clavicle fractures; however, there is a significant increase in patient radiation exposure and cost associated with this exam. And finally, patients were not evaluated consecutively and therefore a selection bias may exist. Unfortunately, a handful of patients were excluded because they did not receive adequate initial films secondary to the reasons listed above.
We believe that a radiographic protocol that includes upright views better estimates the energy and severity of clavicle fractures and more accurately demonstrates maximal displacement. In upright radiographs, the weight of the shoulder girdle and upper extremity essentially stresses the clavicle fracture and may demonstrate the true extent of soft tissue injury that accompanied the fracture. These views may aid in predicting nonunion for patients by better representing actual displacement at the time of injury. This study also indicates that patient positioning may influence operative indications. Larger case series and longer patient follow-up are needed to determine if nonunion rates and fracture displacement at union for non-operatively treated clavicle fractures are better predicted with upright or supine imaging. We recommend obtaining upright films during the initial evaluation for clavicle fractures.
Acknowledgments
The authors would like to recognize Angel Brandt for her assistance in creating this manuscript
Footnotes
Presented at the Annual meeting of the Orthopaedic Trauma Association, Phoenix, AZ, October 12, 2013 and as a poster at the Annual Meeting of the American Academy of Orthopaedic Surgeons, Chicago, IL February 2013.
References
- 1.Nordqvist A, Petersson C. The incidence of fractures of the clavicle. Clin Orthop Relat Res. 1994:127–32. [PubMed] [Google Scholar]
- 2.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11:452–6. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 3.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification J Bone Joint Surg Br. 1998;80:476–84. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 4.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86-A:1359–65. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–7. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
- 6.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537–9. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 7.Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: end result study after conservative treatment. J Orthop Trauma. 1998;12:572–6. doi: 10.1097/00005131-199811000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 9.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23:106–12. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 10.McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg Am. 2012;94:675–84. doi: 10.2106/JBJS.J.01364. [DOI] [PubMed] [Google Scholar]
- 11.Murray IR, Foster CJ, Eros A, Robinson CM. Risk factors for nonunion after nonoperative treatment of displaced midshaft fractures of the clavicle. J Bone Joint Surg Am. 2013;95:1153–8. doi: 10.2106/JBJS.K.01275. [DOI] [PubMed] [Google Scholar]
- 12.Witzel K. Intramedullary osteosynthesis in fractures of the mid-third of the clavicle in sports traumatology. Z Orthop Unfall. 2007;145:639–42. doi: 10.1055/s-2007-965616. [DOI] [PubMed] [Google Scholar]
- 13.Daniilidis K, Raschke MJ, Vogt B, et al. Comparison between conservative and surgical treatment of midshaft clavicle fractures: Outcome of 151 cases. Technol Health Care. 2013;21:143–7. doi: 10.3233/THC-130714. [DOI] [PubMed] [Google Scholar]
- 14.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 16.Neer CS., 2nd Nonunion of the clavicle. J Am Med Assoc. 1960;172:1006–11. doi: 10.1001/jama.1960.03020100014003. [DOI] [PubMed] [Google Scholar]
- 17.Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29–42. [PubMed] [Google Scholar]
- 18.Jeray KJ. Acute midshaft clavicular fracture. J Am Acad Orthop Surg. 2007;15:239–48. doi: 10.5435/00124635-200704000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Plocher EK, Anavian J, Vang S, Cole PA. Progressive displacement of clavicular fractures in the early postinjury period. J Trauma. 2011;70:1263–7. doi: 10.1097/TA.0b013e3182166a6f. [DOI] [PubMed] [Google Scholar]
- 20.Kulshrestha V, Roy T, Audige L. Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma. 2011;25:31–8. doi: 10.1097/BOT.0b013e3181d8290e. [DOI] [PubMed] [Google Scholar]
- 21.Eskola A, Vainionpaa S, Myllynen P, Patiala H, Rokkanen P. Outcome of clavicular fracture in 89 patients. Arch Orthop Trauma Surg. 1986;105:337–8. doi: 10.1007/BF00449938. [DOI] [PubMed] [Google Scholar]
- 22.Wilkins RM, Johnston RM. Ununited fractures of the clavicle. J Bone Joint Surg Am. 1983;65:773–8. [PubMed] [Google Scholar]
- 23.Wick M, Muller EJ, Kollig E, Muhr G. Midshaft fractures of the clavicle with a shortening of more than 2 cm predispose to nonunion. Arch Orthop Trauma Surg. 2001;121:207–11. doi: 10.1007/s004020000202. [DOI] [PubMed] [Google Scholar]
- 24.Davids PH, Luitse JS, Strating RP, van der Hart CP. Operative treatment for delayed union and nonunion of midshaft clavicular fractures: AO reconstruction plate fixation and early mobilization. J Trauma. 1996;40:985–6. doi: 10.1097/00005373-199606000-00021. [DOI] [PubMed] [Google Scholar]