Dear Editor:
A 30-year-old woman developed pemphigoid gestationis (PG) after 20 weeks of gestation during her first pregnancy. Initially, she was treated with prednisone (10~30 mg/d), but she had a miscarriage in the 26th week of pregnancy. After the miscarriage, she was treated with prednisone (30~40 mg/d) and azathioprine (100 mg/d). However, her PG did not show clinical remission and new blisters continued to develop until the 12th post-partum week. Therefore, she was referred to our clinic for further treatment.
She had erythematous patches, plaques and tense bullae on both the upper extremities and trunk (Fig. 1A). Histopathological examination of the skin samples showed the presence of subepidermal vesicles with perivascular lymphocytes and eosinophils (Fig. 2A, B). Direct immunofluorescence examination revealed positive, linear deposition of IgG and C3 in the basement membrane zone (Fig. 2C, D). Therefore, we confirmed the diagnosis of PG and started her on high-dose systemic corticosteroids; however, after receiving the treatment, she rapidly gained weight and developed moon face. Therefore, we performed a rapid adrenocorticotropic hormone stimulation test and measured her 24-hour urine cortisol level; on the basis of the test results, she was diagnosed with iatrogenic Cushing's syndrome. Therefore, she was started on prednisone (40~60 mg/d) and azathiprine (100 mg/d), but the symptoms persisted. After considering further treatment options, we decided to administer intravenous immunoglobulin (IVIG) therapy at a dose of 0.5 g kg-1 day-1 for 2 consecutive days.
Fig. 1.
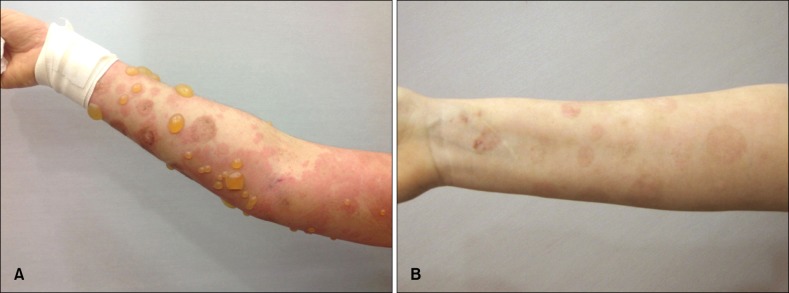
(A) Large tense bullae and erythematous pruritic plaques on the arm. (B) Improved skin lesions with postinflammatory hyperpigmentation after intravenous immunoglobulin combination treatment.
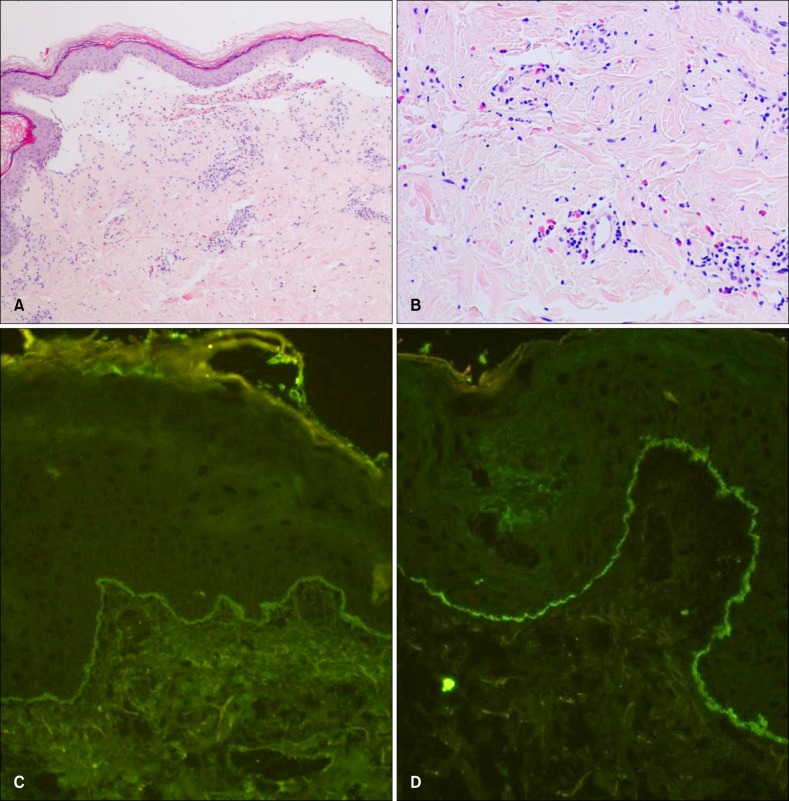
Fig. 2.
(A) Subepidermal blister with superficial inflammatory infiltrate. (B) Superficial perivascular lymphohistiocytic infiltration, with moderate infiltration of eosinophils. Linear staining for (C) IgG, (D) C3 at the basement membrane zone. (A) H&E, ×40; (B) H&E, ×100; (C) direct immunofluorescence (DIF), ×100; (D) DIF, ×100.
After receiving the IVIG therapy, her skin lesions quickly subsided (Fig. 1B), so prednisone was tapered down to 10 mg/day. She was also administered a steroid at a low dose for 8 weeks for treating her Cushing's syndrome. At the follow-up after 3 months, no lesions were found on the patient.
PG is a rare autoimmune-mediated blistering disease, usually occurring in the late pregnancy and immediate postpartum period. Many patients experience spontaneous resolution during the latter part of gestation only to experience a flare at the time of delivery. However, the persistence of disease activity for many years postpartum has been reported. Numerous immunosuppressive treatments have been reported for PG1. If the disease persists, treatment options are limited because they have potential side-effects, e.g. development of Cushing's syndrome, as seen in our patient.
IVIG has been used to treat various autoimmune blistering diseases2. Many authors reported the use of IVIG for treating PG. The immunomodulatory actions of IVIG are mediated via several immune-mediated mechanisms, such as complement blockade and degradation, Fc receptor blockade and induction of immunomodulatory Fc receptors, inhibition of B cells, and alteration of T-cell function, cytokine modulation, and cellular migration3. IVIG therapy is relatively safe, and severe adverse events associated with the use of IVIG are rare. Headache and acute cutaneous reactions are the most common adverse effects of the therapy, while renal failure, thromboembolic events, and anaphylaxis have rarely been reported in association with IVIG therapy3.
It is difficult to differentiate refractory PG from epidermolysis bullosa acquisita using only clinical, histological and direct immunofluorescence findings. Therefore, the findings of enzyme-linked immunosorbent assay and indirect immunofluorescence performed on sodium chloride-split skin are helpful in the differentiation4. We confirmed the diagnosis of PG in the case of our patient, as PG manifests itself during pregnancy, moreover, the patient achieved remission after one-cycle treatment2,3.
PG is a rare disease and only 4 cases of PG treated with IVIG have been reported to date. We presented a case of persistent PG treated with IVIG combination therapy. IVIG should be considered as a therapeutic option in patients that fail to respond to conventional immunosuppressive treatment.
ACKNOWLEDGMENT
This work was supported in part by the Soonchunhyang University Research fund.
References
- 1.Castro LA, Lundell RB, Krause PK, Gibson LE. Clinical experience in pemphigoid gestationis: report of 10 cases. J Am Acad Dermatol. 2006;55:823–828. doi: 10.1016/j.jaad.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Harman KE, Black MM. High-dose intravenous immune globulin for the treatment of autoimmune blistering diseases: an evaluation of its use in 14 cases. Br J Dermatol. 1999;140:865–874. doi: 10.1046/j.1365-2133.1999.02817.x. [DOI] [PubMed] [Google Scholar]
- 3.Czernik A, Toosi S, Bystryn JC, Grando SA. Intravenous immunoglobulin in the treatment of autoimmune bullous dermatoses: an update. Autoimmunity. 2012;45:111–118. doi: 10.3109/08916934.2011.606452. [DOI] [PubMed] [Google Scholar]
- 4.Yang B, Wang C, Chen S, Chen X, Zhou G, Tian H, et al. Accuracy of indirect immunofluorescence on sodium chloride-split skin in the differential diagnosis of bullous pemphigoid and epidermolysis bullosa acquisita. Indian J Dermatol Venereol Leprol. 2011;77:677–682. doi: 10.4103/0378-6323.86479. [DOI] [PubMed] [Google Scholar]