Abstract
Background and Purpose
Process improvement (PI) is an approach for enhancing the existing quality improvement process by making changes while keeping the existing process. We have shown that implementation of a stroke code program using a computerized physician order entry system is effective in reducing the in-hospital time delay to thrombolysis in acute stroke patients. We investigated whether implementation of this PI could further reduce the time delays by continuous improvement of the existing process.
Methods
After determining a key indicator [time interval from emergency department (ED) arrival to intravenous (IV) thrombolysis] and conducting data analysis, the target time from ED arrival to IV thrombolysis in acute stroke patients was set at 40 min. The key indicator was monitored continuously at a weekly stroke conference. The possible reasons for the delay were determined in cases for which IV thrombolysis was not administered within the target time and, where possible, the problems were corrected. The time intervals from ED arrival to the various evaluation steps and treatment before and after implementation of the PI were compared.
Results
The median time interval from ED arrival to IV thrombolysis in acute stroke patients was significantly reduced after implementation of the PI (from 63.5 to 45 min, p=0.001). The variation in the time interval was also reduced. A reduction in the evaluation time intervals was achieved after the PI [from 23 to 17 min for computed tomography scanning (p=0.003) and from 35 to 29 min for complete blood counts (p=0.006)].
Conclusions
PI is effective for continuous improvement of the existing process by reducing the time delays between ED arrival and IV thrombolysis in acute stroke patients.
Keywords: stroke, thrombolysis, quality improvement, emergency medical services, stroke teams, code stroke
Introduction
Thrombolytic therapy with intravenous (IV) recombinant tissue plasminogen activator (rt-PA) is effective if started within 4.5 hours after symptom onset in ischemic stroke patients.1 An earlier administration of rt-PA is associated with a greater benefit of thrombolytic treatment,2 highlighting the need for rapid assessment in the treatment of stroke patients. However, only a small proportion of stroke patients actually receive thrombolytic therapy within the therapeutic window.3 Previous studies have shown that many of the patients who were eligible for thrombolysis did not receive thrombolytic treatment due to in-hospital delays, despite their arrival at the hospital emergency department (ED) within the therapeutic time window.4,5,6,7
One of the important elements associated with an increased use of thrombolytics for ischemic stroke is reducing the time interval from ED arrival to initiation of rt-PA. Previous studies have indicated that several types of intervention might be effective for shortening that time interval.8,9,10,11 We developed a stroke code program based on the computerized physician order entry (CPOE) system using a quality improvement approach. We have demonstrated previously that this system can reduce the time interval from hospital arrival to thrombolysis and increases the number of patients treated with thrombolysis.12 We have also shown that this program can be successfully implemented in various hospital settings.13
The time interval from hospital arrival to the thrombolytic treatment in acute stroke patients may be further reduced by a series of actions designed to improve the existing process. Process improvement (PI) is an approach for improving existing quality improvement processes by making changes while keeping the existing process. The PI approach is different from the quality improvement approach in that it involves regular and continuous monitoring of key indicators over time, while quality improvement is stopped after completing the improvement steps.
The purpose of this study was to determine the effect of the PI approach on the time from the arrival at the ED to the initiation of IV thrombolytic treatment in acute stroke patients.
Methods
Preexisting CPOE-based stroke code program
Beginning in June 2004, a quality improvement approach was used to develop a stroke code program based on the CPOE system, called Brain salvage through Emergent Stroke Therapy (BEST), to reduce the in-hospital time delays from ED arrival to thrombolytic treatment in acute ischemic stroke. The CPOE system is a hospital information technology system that improves the operation of a stroke team by facilitating rapid communication among team members and providing immediate access to information. Briefly, the BEST program uses a CPOE system for activation, communication, notification, entering of predetermined order sets, providing protocols, deactivation, and obtaining time data for various evaluation steps. The features of the BEST program have been described in detail previously.12,13
The PI approach
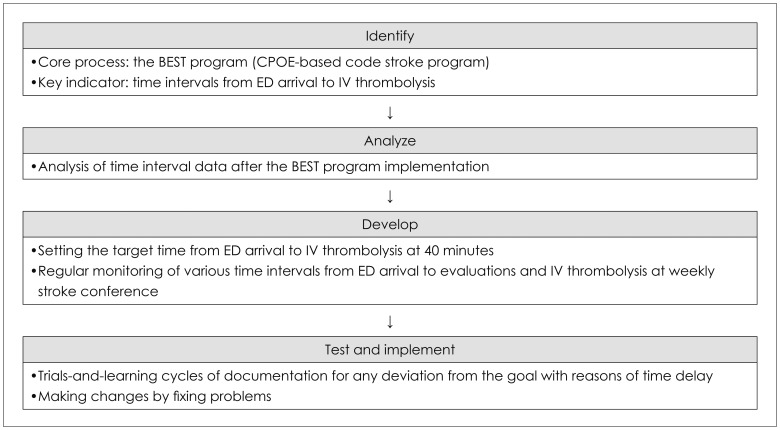
The PI activity was implemented from January 2007, and included four steps: identify, analyze, develop, and test and implement. The aim of the 'identify' step is to identify the core process that will be the focus and to determine the associated indicators. In the 'analyze' step, the data are analyzed to determine where the problems exist within the identified process, and the 'develop' step involves developing solutions that make changes while not extensively altering the existing process. The 'test and implement' step uses tools such as Plan-Do-Study-Act cycles, six-sigma, or lean strategies, which involve a 'trials-and-learning' approach.14
The PI steps used in this study are shown in Fig. 1. The key indicator of our PI approach was the time from ED arrival to IV thrombolysis. The data regarding the time intervals from ED arrival to various evaluations and IV thrombolysis in acute stroke patients between June 2004 and December 2006 were analyzed after implementation of the BEST program. The median time interval from ED arrival to IV thrombolysis was about 63 min. We developed two processes to improve the existing process and reduce the time from ED arrival to IV thrombolysis. First, the target time from ED arrival to IV thrombolysis was set at 40 min based on analyses of median time intervals from hospital arrival to completion of computed tomography (CT) scanning (22 min) and complete blood count (34 min), which are essential steps before rt-PA treatment. Second, the performance of the stroke team was monitored regularly at a weekly stroke conference by reviewing the time intervals between ED arrival and notification to a neurologist, CT scanning, receipt of complete blood count or prothrombin time/activated partial thromboplastin time results, and the administration of IV rt-PA. The CPOE system was used for acquiring time data for activation of the BEST program, receipt of blood samples in the laboratory, reporting of blood tests, and initiation of a brain CT scan. The 'test and implement' step of the PI was achieved by identifying the possible reasons for the delay in those cases for which the time interval from ED arrival to IV thrombolysis was longer than the target time of 40 min, determining whether the reasons/problems were correctable at the weekly stroke conference, and by attempting (where possible) to correct those problems.
Fig. 1.
The process improvement step designed to reduce the time delay from arrival at the emergency department (ED) to intravenous (IV) thrombolysis. BEST: Brain salvage through Emergent Stroke Therapy, CPOE: computerized physician order entry.
Efficacy of the PI approach
The patients who visited the ED and were treated with IV thrombolysis within the 3-hour time window were eligible for this study. Patients who developed ischemic stroke during hospitalization and those who were transferred with the results of imaging studies from other hospitals were excluded.
The effect of the PI was assessed by comparing time intervals from the ED arrival to various steps in the evaluation and treatment of patients who received IV thrombolysis during the 1.5 years before implementation of the PI (pre-PI group) and 1.5 years after implementation of the PI (post-PI group). The steps in the evaluation and treatment of the patients included the notification to a neurologist, CT scan, complete blood count or prothrombin time/activated partial thromboplastin results, and the initiation of IV rt-PA injection.
The prospectively collected reasons for time delays in the post-PI group were summarized in order to identify the potential barriers that contribute to a time interval of longer than 40 min from the ED arrival of a patient with acute stroke to IV thrombolysis. This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System.
Statistical analysis
Categorical variables were compared between the pre-PI and post-PI groups using Pearson's χ2 test. Continuous variables including the time intervals were compared using the Mann-Whitney U test and are expressed as median [interquartile range (IQR)] values. The cutoff for statistical significance was set at p<0.05. SPSS for Windows (version 18.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
Results
Baseline characteristics
Totals of 888 and 799 patients with cerebral infarction were admitted to the Neurology Department via the ED during the 1.5 years pre-PI and 1.5 years post-PI, respectively, of which 39 (4.4%) and 63 (7.9%) received IV rt-PA (p=0.003). In the pre-PI group, 28 (71.8%) of the 39 patients were men and the median age was 68 years (IQR, 56-75 years). In the post-PI group, 41 patients (65.1%) were men and the median age was 69 years (IQR, 57-77 years). The interval between onset to door time did not differ significantly between the two groups [44 min (IQR, 30-80 min) in the pre-PI group vs. 56 min (IQR, 30-90 min) in the post-PI group, p=0.310]. The initial stroke severity, which was determined using the National Institutes of Health Stroke Scale (NIHSS) score, also did not differ between the groups. The median NIHSS scores in the pre-PI and post-PI groups were 13 (IQR, 9-19) and 16 (IQR, 12.25-20), respectively (p=0.125).
Efficacy of the PI approach on reducing the time intervals
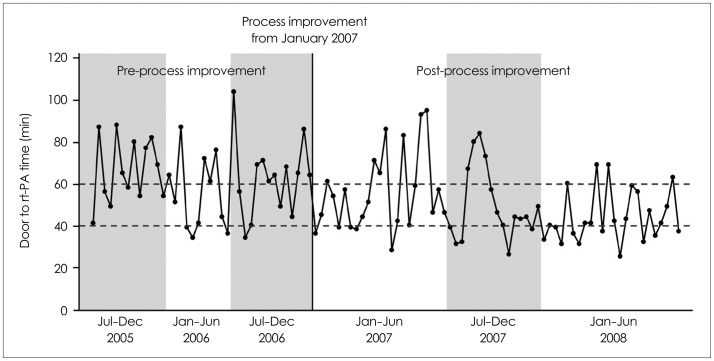
The median time from ED arrival to IV thrombolysis was significantly shorter in the post-PI group (45 min) than the pre-PI group (63.5 min, p=0.001). We further analyzed the time intervals at 6-month intervals. The median values of time intervals from ED arrival to IV thrombolysis divided into 6-month periods of July to December 2005, January to June 2006, July to December 2006, January to June 2007, July to December 2007, and January to June 2008 were 66, 52, 65, 52, 45, and 42 min, respectively. A run chart showed that the variation in time from ED arrival to IV thrombolysis was not reduced immediately after implementation of the PI, but that after the trials-and-learning period, the variation was substantially reduced (Fig. 2). The time intervals from ED arrival to the various evaluation steps were significantly shortened in the post-PI group. The median time intervals to the notification to a neurologist, the CT scan, the complete blood count results, and the prothrombin time/activated partial thromboplastin time results were reduced from 12 to 7 min (p=0.001), from 23 to 17 min (p=0.003), from 35 to 29 min (p=0.006), and from 51 to 45 min (p=0.004), respectively (Table 1).
Fig. 2.
A run chart showing time interval from arrival at the emergency department to intravenous thrombolysis in each acute stroke patient over time. rt-PA: recombinant tissue plasminogen activator.
Table 1.
Comparison of the time intervals from arrival at the emergency department to various evaluation steps and thrombolytic treatment among acute stroke patients
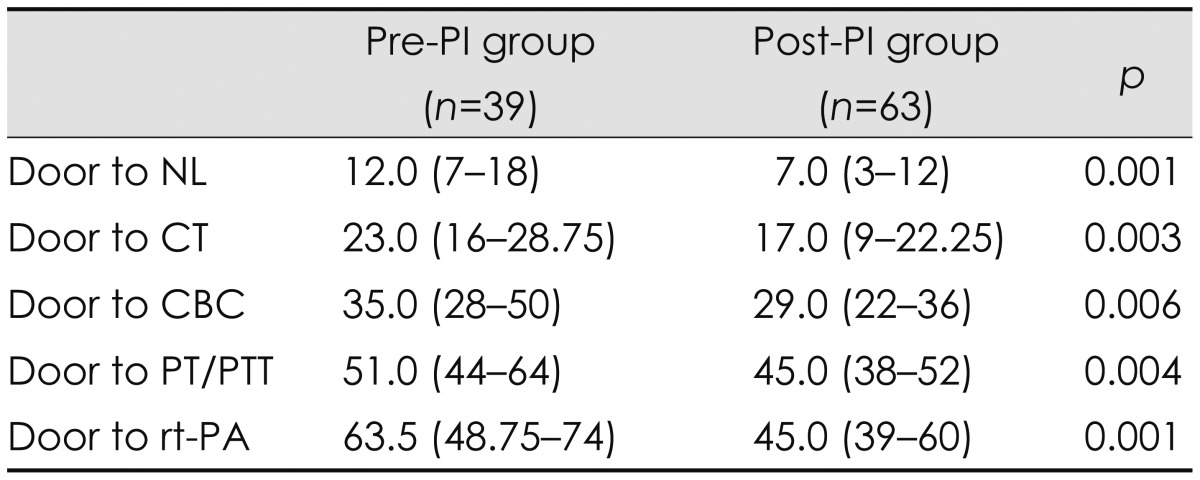
Data are median (interquartile range) times, in minutes.
CBC: complete blood count, CT: computed tomography, NL: notification to a neurologist, PI: process improvement, PT: prothrombin time, PTT: partial thromboplastin time, rt-PA: recombinant tissue plasminogen activator.
The proportion of patients who underwent thrombolytic treatment within 40 min was higher in the post-PI group (20/63 patients, 31.7%) than in the pre-PI group (5/39 patients, 12.8%) (p=0.031). The number of patients who underwent IV thrombolysis within 60 min was also higher in the post-PI group (48/63 patients, 76.2%) than in the pre-PI group (18/39 patients, 46.2%) (p=0.002).
Reasons for in-hospital delays
Ten reasons were identified for a delay longer than 40 min from ED arrival to IV thrombolysis in 43 acute stroke patients (Table 2), including indecision of family members, the need to confirm the prothrombin time results due to a previous history of anticoagulation, a prolonged CT scanning time due to poor patient cooperation, unavailability of the CT room due to ongoing scanning of another patient, a new CT technician with insufficient knowledge of the stroke code program, delayed notification to a neurologist due to misdiagnosis of the thrombolysis candidates at triage, the need to control high blood pressure, and delayed laboratory tests due to the technician's lack of awareness of the stroke code program. In eight cases we were unable to determine specific reasons why IV thrombolysis was started later than 40 min after their ED arrival.
Table 2.
Reasons for delays longer than 40 min from hospital arrival to thrombolytic therapy during the period after implementation of the process improvement
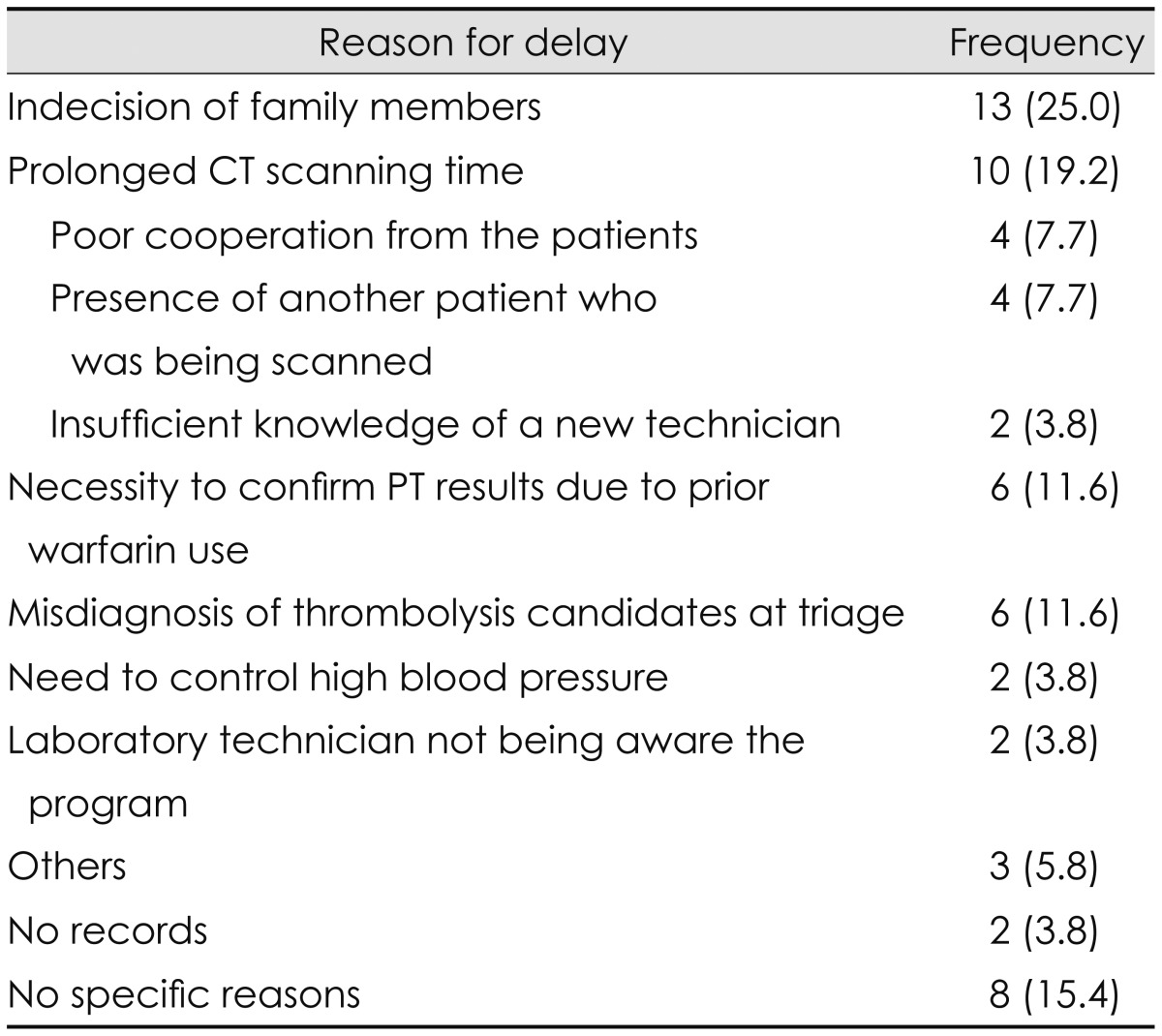
Data are n (%) values.
CT: computed tomography, PT: prothrombin time.
Discussion
The findings of this study demonstrate the efficacy of the PI approach for continuous improvement of an existing process. The PI reduced the time interval to IV thrombolysis and increased the number of patients treated with thrombolysis even after the successful implementation of a stroke code program. After successful implementation of the CPOE-based BEST program in our institute, the quality improvement team was disbanded, and the stroke team was encouraged to reduce as far as possible the time interval from ED arrival to thrombolysis during routine clinical practice. However, there was no further reduction of the time interval from ED arrival to thrombolysis, indeed, it tended to be slightly prolonged. Thus, it became clear that continuous quality improvement approaches were necessary. The PI approach usually begins after implementation of a quality improvement process and is applied over a long time period. It can achieve long-term improvements by continuous monitoring of the process and fixing problems as they arise. Our findings clearly demonstrate the necessity of the PI approach to make long-term improvement after successful implementation of a quality improvement process.
We set the target time after we had identified the key indicator and analyzed the data. The setting of a target time may encourage team members to act more quickly to achieve the goal. The National Institute of Neurological Disorders and Stroke (NINDS) recommended 60 min as the target time from hospital arrival to drug administration. However, we set the much faster target time of 40 min. The target time may be set according to the situation and the needs of each institute. The behavior of physicians is often a major factor controlling the time limit for administering thrombolysis. The time to treatment tends to be longer when patients arrive at the ED earlier after onset of symptoms,15,16 and hence setting a target time to be the shortest possible may be helpful for improving the behavior of physicians.
The key activity of the PI approach is a continuous monitoring of the process, detecting and fixing problems, and making changes. This process should be continued over a long time period. These features are different from a typical quality improvement approach. We monitored the recorded time intervals at a weekly stroke conference and identified the possible reasons for delays. The weekly stroke conference is a routine clinical activity at our institute, and this makes it possible to easily and consistently monitor the data and detect problems. This study found that the main causes of in-hospital delays exceeding 40 min were delays in obtaining informed consent for thrombolysis due to the indecision of family members, prolonged CT scanning time, failed triage of thrombolysis candidates, and waiting for prothrombin time results in patients with previous use of anticoagulants; together these causes accounted for 67.4% of delays. Although similar reasons for a delay have been found in previous studies,6,7,17,18 most of those studies only assessed reasons for delays, and not ways of reducing them. The PI approach might be helpful for detecting and correcting possible problems in a timely manner. For instance, at our institute there is a relatively high turnover of radiology and laboratory technicians, and this can cause delays in performing tests due to a lack of awareness of the stroke code program. Re-educating new technicians in a timely manner to increase awareness of the stroke code program would ameliorate this problem. Re-education of the triage nurses and the ED staff could also be useful, since misdiagnosis of stroke at triage was one of the common reasons for the delay to treatment in our study.
This study was subject to several limitations. First, a 1.5-year period may not be long enough to demonstrate the efficacy of the PI program. However, the time intervals were reduced consistently from the first 6 months after implementation of the PI program, although it took time to achieve remarkable changes in the variation of time intervals. Second, we could neither compare the reasons for delay before and after the PI program nor provide the changes or improvements in the specific reasons for delay after implementation of the PI program because those reasons were documented only after the implementation of the PI program.
Our findings suggest that simply setting the target time from ED arrival to IV thrombolysis and encouraging a stroke team to act fast may not be sufficient to induce changes in that team's behavior. The NINDS recommended a target time of 60 min between hospital arrival and drug administration for stroke patients. However, in data from the Get With the Guidelines-Stroke Program from April 2003 to September 2009, which included 25,504 patients treated with rt-PA, only 26.6% of patients received thrombolysis within 60 min after arrival at the hospital,3 which also suggests that stroke team activities are necessary to make changes.
In conclusion, our findings suggest that setting a shorter target time from hospital arrival to commencement of thrombolytic treatment for acute stroke patients and implementing continuous monitoring and identifying and fixing problems via the PI approach can improve the activities of the stroke team and thereby reduce the treatment-time delays.
Acknowledgements
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (HI10C2020).
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 2.Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010;375:1695–1703. doi: 10.1016/S0140-6736(10)60491-6. [DOI] [PubMed] [Google Scholar]
- 3.Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–758. doi: 10.1161/CIRCULATIONAHA.110.974675. [DOI] [PubMed] [Google Scholar]
- 4.Eissa A, Krass I, Bajorek BV. Barriers to the utilization of thrombolysis for acute ischaemic stroke. J Clin Pharm Ther. 2012;37:399–409. doi: 10.1111/j.1365-2710.2011.01329.x. [DOI] [PubMed] [Google Scholar]
- 5.California Acute Stroke Pilot Registry (CASPR) Investigators. Prioritizing interventions to improve rates of thrombolysis for ischemic stroke. Neurology. 2005;64:654–659. doi: 10.1212/01.WNL.0000151850.39648.51. [DOI] [PubMed] [Google Scholar]
- 6.Qureshi AI, Kirmani JF, Sayed MA, Safdar A, Ahmed S, Ferguson R, et al. Time to hospital arrival, use of thrombolytics, and in-hospital outcomes in ischemic stroke. Neurology. 2005;64:2115–2120. doi: 10.1212/01.WNL.0000165951.03373.25. [DOI] [PubMed] [Google Scholar]
- 7.García-Moncó JC, Pinedo A, Escalza I, Ferreira E, Foncea N, Gómez-Beldarrain M, et al. Analysis of the reasons for exclusion from tPA therapy after early arrival in acute stroke patients. Clin Neurol Neurosurg. 2007;109:50–53. doi: 10.1016/j.clineuro.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 8.Köhrmann M, Schellinger PD, Breuer L, Dohrn M, Kuramatsu JB, Blinzler C, et al. Avoiding in hospital delays and eliminating the three-hour effect in thrombolysis for stroke. Int J Stroke. 2011;6:493–497. doi: 10.1111/j.1747-4949.2011.00585.x. [DOI] [PubMed] [Google Scholar]
- 9.Nolte CH, Malzahn U, Kühnle Y, Ploner CJ, Müller-Nordhorn J, Möckel M. Improvement of door-to-imaging time in acute stroke patients by implementation of an all-points alarm. J Stroke Cerebrovasc Dis. 2013;22:149–153. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 10.Sung SF, Huang YC, Ong CT, Chen YW. A Parallel Thrombolysis Protocol with Nurse Practitioners As Coordinators Minimized Door-to-Needle Time for Acute Ischemic Stroke. Stroke Res Treat. 2011;2011:198518. doi: 10.4061/2011/198518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tai YJ, Weir L, Hand P, Davis S, Yan B. Does a 'code stroke' rapid access protocol decrease door-to-needle time for thrombolysis? Intern Med J. 2012;42:1316–1324. doi: 10.1111/j.1445-5994.2011.02709.x. [DOI] [PubMed] [Google Scholar]
- 12.Nam HS, Han SW, Ahn SH, Lee JY, Choi HY, Park IC, et al. Improved time intervals by implementation of computerized physician order entry-based stroke team approach. Cerebrovasc Dis. 2007;23:289–293. doi: 10.1159/000098329. [DOI] [PubMed] [Google Scholar]
- 13.Heo JH, Kim YD, Nam HS, Hong KS, Ahn SH, Cho HJ, et al. A computerized in-hospital alert system for thrombolysis in acute stroke. Stroke. 2010;41:1978–1983. doi: 10.1161/STROKEAHA.110.583591. [DOI] [PubMed] [Google Scholar]
- 14.Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc. 2007;82:735–739. doi: 10.4065/82.6.735. [DOI] [PubMed] [Google Scholar]
- 15.Strbian D, Michel P, Ringleb P, Numminen H, Breuer L, Bodenant M, et al. Relationship between onset-to-door time and door-to-thrombolysis time: a pooled analysis of 10 dedicated stroke centers. Stroke. 2013;44:2808–2813. doi: 10.1161/STROKEAHA.113.000995. [DOI] [PubMed] [Google Scholar]
- 16.Ferrari J, Knoflach M, Kiechl S, Willeit J, Matosevic B, Seyfang L, et al. Stroke thrombolysis: having more time translates into delayed therapy: data from the Austrian Stroke Unit Registry. Stroke. 2010;41:2001–2004. doi: 10.1161/STROKEAHA.110.590372. [DOI] [PubMed] [Google Scholar]
- 17.Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004;33:116–121. doi: 10.1093/ageing/afh064. [DOI] [PubMed] [Google Scholar]
- 18.Johnson M, Bakas T. A review of barriers to thrombolytic therapy: implications for nursing care in the emergency department. J Neurosci Nurs. 2010;42:88–94. [PubMed] [Google Scholar]