Abstract
Background
The aim of the present meta-analysis of cohort studies was to focus on monounsaturated fat (MUFA) and cardiovascular disease, cardiovascular mortality as well as all-cause mortality, and to distinguish between the different dietary sources of MUFA.
Methods
Literature search was performed using the electronic databases PUBMED, and EMBASE until June 2nd, 2014. Study specific risk ratios and hazard ratios were pooled using a inverse variance random effect model.
Results
Thirty-two cohort studies (42 reports) including 841,211 subjects met the objectives and were included. The comparison of the top versus bottom third of the distribution of a combination of MUFA (of both plant and animal origin), olive oil, oleic acid, and MUFA:SFA ratio in each study resulted in a significant risk reduction for: all-cause mortality (RR: 0.89, 95% CI 0.83, 0.96, p = 0.001; I2 = 64%), cardiovascular mortality (RR: 0.88, 95% CI 0.80, 0.96, p = 0.004; I2 = 50%), cardiovascular events (RR: 0.91, 95% CI 0.86, 0.96, p = 0.001; I2 = 58%), and stroke (RR: 0.83, 95% CI 0.71, 0.97, p = 0.02; I2 = 70%). Following subgroup analyses, significant associations could only be found between higher intakes of olive oil and reduced risk of all-cause mortality, cardiovascular events, and stroke, respectively. The MUFA subgroup analyses did not reveal any significant risk reduction.
Conclusion
The results indicate an overall risk reduction of all-cause mortality (11%), cardiovascular mortality (12%), cardiovascular events (9%), and stroke (17%) when comparing the top versus bottom third of MUFA, olive oil, oleic acid, and MUFA:SFA ratio. MUFA of mixed animal and vegetable sources per se did not yield any significant effects on these outcome parameters. However, only olive oil seems to be associated with reduced risk. Further research is necessary to evaluate specific sources of MUFA (i.e. plant vs. animal) and cardiovascular risk.
Electronic supplementary material
The online version of this article (doi:10.1186/1476-511X-13-154) contains supplementary material, which is available to authorized users.
Keywords: Monounsaturated fatty acids, Olive oil, Cohort studies, Meta-analysis, Cardiovascular disease
Background
The most common monounsaturated fatty acids (MUFA) in daily nutrition is oleic acid, followed by palmitoleic acid, and vaccenic acid. Moreover, oleic acid represents the topmost MUFA provided in the diet (~90% of all MUFA). No dietary recommendations for MUFA are given by the National Institute of Medicine, the United States Department of Agriculture, the European Food and Safety Authority and the American Diabetes Association. In contrast, the Academy of Nutrition and Dietetics as well as the Canadian Dietetic Association both promote <20% MUFA of daily total energy consumption, while the American Heart Association sets a limit of 20% MUFA in their respective guidelines [1–3]. One reason for specific MUFA recommendations might be their potential benefit in the primary and secondary prevention of cardiovascular diseases. However, previous meta-analyses of cohort studies reported inconsistent results of MUFA on coronary heart disease (CHD). Jakobsen et al. [4] observed that replacement of SFA by MUFA marginally increased the risk of coronary events, whereas no significant effects on coronary death could be observed. These results are in strong discrepancy with another meta-analysis of cohort studies, were Mente et al. [5] reported a significant correlation between MUFA intake and a decrease in the relative risk for CHD. Skeaff and Miller [6] did not observe any effects of MUFA-rich diets on relative risks of CHD events and CHD death. Likewise, the most recent meta-analysis by Chowdhury et al. including nine cohort studies found no significant associations between MUFA intake, circulating MUFA and risk of CHD [7].
One explanation for these inconclusive data might be that different sources of MUFA were not taken into account. Adopting a western diet means that MUFA is predominantly supplied by foods of animal origin, while in south European countries, extra virgin olive oil is the most dominant source of this type of fatty acid [8]. Results of the recently published PREDIMED trial demonstrated major cardiovascular benefits of olive oil and nuts when compared to a low-fat diet [9]. As a major outcome parameter, the risk of stroke was reduced, an event which has not been included in the meta-analyses mentioned above. In addition, a recent cohort study observed a significant association between dietary olive oil, higher plasma oleic acid and reduced risk of stroke [10]. Extra virgin olive oil is regarded to be the genuine driver of the Mediterranean diet and was found to be associated with a 26% reduced risk of all-cause mortality in the Spanish branch of the EPIC study [11]. The aim of the present meta-analysis of cohort studies was to focus on MUFA and CVD (combining CHD and stroke), cardiovascular mortality, and all-cause mortality, and to distinguish between the different dietary sources of MUFA (e.g. olive oil).
Materials and methods
Literature search
Queries of literature were performed using the electronic databases PUBMED, and EMBASE (until 2nd June 2014, respectively) with no restrictions to language, and calendar date using the following search terms: (“dietary fat” OR “fatty acids” OR “monounsaturated fat” OR “mufa” OR “olive oil” OR “oleic acid” OR “mediterranean diet”) AND (“cardiovascular disease” OR “myocardial infarction” OR “coronary heart disease” OR “stroke” OR “mortality”) AND (“incidence” OR “cohort” OR “follow-up” OR “prospective” OR “risk ratio” OR “hazard ratio” OR “rate ratio”). Moreover, the reference lists from retrieved articles, systematic reviews, and meta-analyses were checked to search for further relevant studies. This systematic review was planned, conducted, and reported in adherence to standards of quality for reporting meta-analyses [12]. Literature search was conducted independently by both authors, with disagreements resolved by consensus.
Eligibility criteria
Studies were included in the meta-analysis if they met all of the following criteria: (i) cohort study design; (ii) data related to dietary consumption of MUFA, MUFA:SFA ratio, olive oil, and oleic acid; (iii) the primary outcomes were: all-cause mortality, CVD mortality, combined CVD events (cardiovascular mortality, cardiovascular morbidity (non-fatal myocardial infarction, angina, stroke, heart failure, peripheral vascular events)); the secondary outcomes were: coronary heart disease, and stroke; (iv) adjusted relative risks (RRs), and hazard ratios (HRs) with corresponding 95% confidence intervals (95% CIs) or the data necessary to calculate these; (v) when a study appeared to have been published in duplicate, the version containing the most comprehensive information was selected.
Data extraction and quality assessment
The following data were extracted from each study: the first author’s last name, year of publication, study origin, outcome parameter, sample size, study length, age at entry, sex, specification of MUFA, adjustment factors, quality score, and risk estimates (HR, RR; highest vs. lowest category) with their corresponding 95% CIs. If separate risk estimates for males and females or separate risk estimates for ages were available in one study, the data were pooled and treated as one study. When a study provided several risk estimates, the maximally adjusted model was chosen. To assess the study quality, a 9-point scoring system according to the Newcastle-Ottawa Scale (NOS) was used. Hence, the full score was 9, and a high-quality study in the present analysis was defined by a threshold of ≥ 7 points [13]. Data extraction and quality assessment were performed by one author (L.S).
Statistical analysis
The meta-analysis was performed by combining the multivariable adjusted RR or HR of the highest compared with the lowest MUFA, MUFA:SFA ratio, oleic acid, or olive oil category based on random effects model using DerSimonian-Laird method, which incorporated both within and between study variability [14]. To ensure a transparent approach to meta-analysis and interpretation of findings in this review, RR/HR estimates for association of fatty acids and primary/secondary outcomes that were often differently reported by each study (such as per-unit or per-1-SD change or comparing quintiles, quartiles, thirds, and other groupings) were transformed, using methods previously described [7]. These transformed estimates consistently corresponded to the comparison of the top versus bottom third of MUFA, MUFA:SFA ratio, olive oil, and oleic acid distribution in each study. To evaluate the weighting of each study, the standard error for the logarithm HR/RR of each study was calculated and regarded as the estimated variance of the logarithm HR/RR using an inverse variance method [14]. Studies were grouped according to the different clinical outcomes (all-cause mortality, cardiovascular mortality, combined cardiovascular events, coronary heart disease, and stroke). Subgroup analysis was performed for total MUFA, MUFA:SFA ratio, oleic acid, and olive oil. Heterogeneity was estimated by the Cochrane Q test together with the I2 statistic. An I2 value >50% indicates substantial heterogeneity across studies [15]. The heterogi command in STATA was used to calculate the confidence intervals for the heterogeneity estimates. Funnel plots were used to assess potential publication bias. To determine the presence of publication bias, we assessed the symmetry of the funnel plots in which mean differences were plotted against their corresponding standard errors. In addition, Egger test was performed to test for potential publication bias [16]. Sensitivity analyses were performed assuming statistical heterogeneity with the metaan command in STATA [17]. All analyses were conducted using the Review Manager by the Cochrane Collaboration (version 5.2) and STATA 13.0 (Stata-Corp, College Station, TX).
Missing data
Dr. Goldbourt (personal communication) provided the 23 year follow-up all-cause mortality and cardiovascular mortality data of the Israeli civil cohort for the highest vs. lowest quintile MUFA: SFA ratio [18].
Results
Literature search and study characteristics
A total of 32 cohort studies (42 reports) met the inclusion criteria and were included in the meta-analysis [10, 11, 18–57]. Full search strategy for PUBMED is given in the Additional file 1. General study characteristics are given in Table 1. Sample size varied between 161 and 161,808 with a follow-up time ranging from 3.7 to 30 years. The total number of subjects in the included studies was 841,211.
Table 1.
General study characteristics of the included cohort studies
| Author, year | Cohort name country | Outcomes | Population | Follow-up (years) | Age at entry (years) | Sex | MUFA source | Adjustment | Multivariate adjusted | Study quality |
|---|---|---|---|---|---|---|---|---|---|---|
| (Newcastle-Ottawa scale) | ||||||||||
| Atkins et al. 2014 [34] | British Regional Heart Study GBR | All-cause mortality CVD mortality CVD events CHD events | 3,328 | 11.3 | 60-79 | M | Olive oil | Age, energy intake, smoking, alcohol, PA, social class, BMI, and a modified version of the HDI/EDI score not containing the individual component of interest | Fourth vs. first quartile | 8 |
| Barzi et al. 2003 [50] | Studio della Sopravvivenza nell’Infarto Miocardico ITA | All-cause mortality | 11,323 with myocardial infarction | 6.5 | 59 | M/F | Olive oil | Age, sex, hypertension, HDL-cholesterol, diabetes, smoking, claudication, electrical instability, left ventricular dysfunction, residual myocardial ischaemia, dietary supplementation, pharmacological therapies | Third vs. first tertile | 7 |
| Bendinelli et al. 2011 [49] | European Prospective Into Cancer and Nutrition ITA | CHD | 29,689 | 7.85 | 35-74 | F | MUFA MUFA:SFA | Energy intake, educational level, smoking status, alcohol consumption, body height, body weight, waist circumference daily non-alcohol caloric intake, hypertension, menopausal status, PA, total meat consumption | Fourth vs. first quartile | 8 |
| Buckland et al. 2012 [11] | European Prospective Into Cancer and Nutrition SPA | All-cause mortality CVD mortality Cancer mortality | 41,078 | 10.4 | 29-69 | M/F | Olive oil | Centre, sex, age, energy intake, BMI, waist circumference, educational status, smoking status, PA, and alcohol intake, intake of fruit, vegetables, meat, and dairy | Fourth vs. first quartile | 8 |
| Buckland et al. 2012 [56] | European Prospective Into Cancer and Nutrition SPA | CHD | 40,142 | 10.4 | 29-69 | M/F | Olive oil | Educational level, BMI, waist circumference, PA, smoking status, alcohol consumption, energy intake excluding alcohol, hyperlipidaemia, hypertension and diabetes, Mediterranean diet score (excluding olive oil and alcohol) | Fourth vs. first quartile | 8 |
| Chiuve et al. 2012 [32] | Nurses’ Health Study USA | Sudden death | 91,981 | 30 | 34-59 | F | MUFA | Total calories, smoking, BMI, family history of myocardial infarction, menopausal status, hormone therapy, exercise, aspirin use, use of multivitamins, use of vitamin E supplements, alcohol use, and history of diabetes, hypertension, hypercholesterolemia, coronary heart disease, and cancer at baseline, percentage of energy from total fat | Fifth vs. first quintile | 8 |
| Dilis et al. 2012 [19] | European Prospective Into Cancer and Nutrition GRE | CHD mortality CHD incidence | 23,929 | 10 | 20-86 | M/F | MUFA Olive Oil MUFA:SFA | Age, BMI, height, PA, years of schooling and energy intake entered, alcohol consumption, smoking status and arterial blood pressure | 1 SD increment | 9 |
| Esrey et al. 1996 [42] | Lipid Research Clinics Prevalence Study USA | CVD mortality | 4,546 | 12.4 | ≥30 | M/F | MUFA | Age, sex, energy intake, serum lipids, systolic blood pressure, cigarette smoking, BMI, glucose intolerance | 1 unit increase | 9 |
| Gardener et al. 2011 [43] | Northern Manhattan Study USA | Ischemic stroke Myocardial infarction Vascular death | 2,568 | 9 | >40 | M/F | MUFA:SFA | Age, sex, race ethnicity, completion of high school education, moderate-to-heavy PA, energy intake, and cigarette smoking | ≥ median vs. < median | 7 |
| Gillman et al. 1997 [40] | Framingham Heart Study USA | Stroke | 832 | 20 | 45-65 | M | MUFA | Age, energy, systolic blood pressure, cigarette smoking, glucose intolerance, BMI, PA, left ventricular hypertrophy, alcohol, fruit and vegetables | 1% increase MUFA | 9 |
| Goldbourt et al. 1993 [18] | Israeli Ischemic Heart Disease Study ISR | CHD All-cause mortality | 10,059 | 23 | >40 | M | MUFA:SFA | Age | Fifth vs. first quintile | 7 |
| Guasch-Ferre et al. 2014 [54] | PREvención con DIeta MEDiterránea SPA | All-cause mortality CVD mortality CVD events | 7216 | 4.8 | 55-80 | M/W | Olive oil | Age, sex, BMI, smoking status, alcohol intake, education level, PA, prevalence of diabetes, prevalence of hypertension, prevalence of hypercholesterolemia, use of antihypertensive, use of statins, Mediterranean diet adherence | Third vs. first tertile | 8 |
| He et al. 2003 [47] | Health professional study USA | Stroke | 43,732 | 14 | 40-75 | M | MUFA | BMI, PA, history of hypertension, smoking status, aspirin use, multivitamin use, and consumption of alcohol, potassium, fibre, and vitamin E, total servings of fruit and vegetables, total energy intake, and hypercholesterolemia at baseline | Fifth vs. first quintile | 7 |
| Houston et al. 2011 [38] | Health ABC study USA | CVD events | 1,941 | 9 | 70-79 | M/F | MUFA | Age, gender, race, education, field centre, smoking, alcohol use, PA, BMI, total energy intake, protein intake, fibre intake, multivitamin use, supplemental vitamin E use, statin use, aspirin use, oral estrogen use, and prevalent diabetes or hypertension, fat, PUFA, trans fat, and cholesterol | Third vs. first tertile | 8 |
| Iso et al. 2001 [37] | Nurses’ Health Study USA | Stroke | 85,764 | 14 | 30-59 | F | MUFA | Age, smoking status, time interval, BMI, alcohol intake, menopausal status and postmenopausal hormone use, vigorous exercise, usual aspirin use, multivitamin use, vitamin E use, n-3 fatty acid intake, calcium intake, and histories of hypertension, diabetes, high cholesterol levels, and total energy intake | Fifth vs. first quintile | 7 |
| Iso et al. 2003 [36] | JAP | Stroke | 4,775 | 14 | 40-69 | M/F | MUFA | Age, sex, quartiles of total energy intake and BMI, hypertension category, diabetes, serum total cholesterol, smoking status, ethanol intake, and menopausal status | Fourth vs. first quartile | 8 |
| Jakobsen et al. 2004 [4] | Multinational MONItoring of trends and determinants in CArdiovascular disease I, II EU | CHD | 3,686 | 16 | 30-71 | M/F | MUFA | Total energy intake, energy from protein, energy from fat, energy from carbohydrates, non-dietary and dietary coronary heart disease risk factors | 5% increase | 8 |
| Kouris-Blazos et al. 1999 [55] | AUS | All-cause mortality | 330 | 4-6 | >70 | M/F | MUFA:SFA | Age, sex and smoking status but not ethnic origin | MUFA:SFA (1 unit) | 6 |
| Larsson et al. 2012 [48] | Swedish Mammography Cohort SWE | Stroke | 34,670 | 10.4 | 49-83 | F | MUFA | Age, smoking status and pack-years of smoking, education, BMI, PA, history of hypertension, history of diabetes, aspirin use, family history of myocardial infarction, intakes of alcohol, protein, and dietary fibre, cholesterol | Fifth vs. first quintile | 8 |
| Lasheras et al. 2000 [26] | SPA | All-cause mortality | 161 | 9 | 65-95 | M/F | MUFA:SFA | Age, sex, BMI, albumin concentration, PA, self-assessment of health, and dieting for chronic conditions | MUFA:SFA (1 unit) | 6 |
| Leosdottir et al. 2007 [28], Wallström et al. 2012 [29] | Malmö Diet and cancer Study SWE | CVD events Stroke CHD | 28,098 | 13.5 | 44-73 | M/F | MUFA MUFA:SFA | Age, smoking habits, alcohol consumption, socioeconomic status, marital status, PA, BMI, fibre intake, and blood pressure, total fat intake for the ratio between unsaturated and saturated fats | Fifth vs. first quintile Fourth vs. first quartile | 9 |
| Levitan et al. 2013 [57] | Women’s Health Initiative trial and observational study USA | Heart Failure | 68,132 (WHI) 93,676 (WHI-OS) | 4.6 | 50-79 | F | MUFA:SFA | Age at heart failure hospitalization, total energy intake, race/ethnicity, education, income, married, current smoking, total exercise, physical function, use of off-study postmenopausal hormone therapy, Women’s Health Initiative (WHI) study arm, systolic blood pressure, diastolic blood pressure, use of diuretics, β-blockers, and angiotensin converting enzyme inhibitors or angiotensin receptor blockers, BMI, and history of high cholesterol, high blood pressure, diabetes mellitus, myocardial infarction, coronary revascularization, and atrial fibrillation | Fourth vs. first quartile | 8 |
| Martinez-Gonzalez et al. 2011 [45] | Seguimiento University of Navarra SPA | All-cause mortality | 15,535 | 6.8 | University graduates (mean: 38) | M/F | MUFA:SFA | Age, years of university of education, BMI, smoking, PA, hours per day spent watching television, history of depression, baseline hypertension, baseline hypercholesterolemia, total energy intake, egg consumption, potato consumption, and adoption of special diets | ≥ median vs. < median | 8 |
| Martinez-Gonzalez et al. 2009 | Seguimiento University of Navarra SPA | CVD CHD | 13,609 | 4.9 | University graduates (mean: 38) | M/F | MUFA:SFA | Age, sex, family history of coronary heart disease, total energy intake, PA, smoking, BMI, diabetes at baseline, use of aspirin, history of hypertension and history of hypercholesterolemia | ≥ median (W: ≥1.24, M: ≥1.19) vs. < median | 8 |
| Misirli et al. 2012 [52] | European Prospective Into Cancer and Nutrition GRE | Stroke Incidence Stroke Mortality | 23,601 | 10.6 | 20-87 | M/F | MUFA Olive Oil | Age, sex, education, smoking status, BMI, PA, hypertension, diabetes, and total energy intake. | Olive oil (23 g/d) MUFA (18 g/d) | 9 |
| Nagata et al. 2012 [31] | Takayama study JAP | All-cause mortality CVD mortality Cancer mortality | 28,356 | 16 | ≥35 | M/F | MUFA | Age, non-alcohol energy, and protein expressed as percentage of non-alcohol energy and was additionally adjusted for fat subtypes expressed as percentage of non-alcohol energy as appropriate, height, BMI, PA, smoking status, alcohol intake, education, marital status, menopausal status, histories of diabetes and hypertension, and intakes of fruits, vegetables, and dietary fibre | Fifth vs. first quintile | 8 |
| Oh et al. 2005 [33] | Nurses’ Health Study USA | CHD | 78,778 | 20 | 30-55 | F | MUFA | Age, BMI, smoking, alcohol intake, parental history of myocardial infarction, history of hypertension, menopausal status and hormone use, aspirin use, multivitamin use, vitamin E supplement use, PA, energy, protein, cholesterol intake, saturated, polyunsaturated, and trans-fat; a-linolenic acid; marine n-3 fatty acids; cereal fiber; and fruits and vegetables | Fifth vs. first quintile | 7 |
| Pietinen et al. 1997 [53] | Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study USA | CVD events CVD mortality | 21,930 | 6.1 | 50-69 | M | MUFA Oleic acid | Age, smoking, BMI, blood pressure, energy intake, alcohol, education, PA | Fifth vs. first quintile | 7 |
| Posner et al. 1991 [46] | Framingham Study USA | CHD | 813 | 16 | 45-65 | M | MUFA | Energy, serum cholesterol levels, PA, systolic blood pressure, left ventricular hypertrophy, cigarette smoking, glucose intolerance, and metropolitan relative weight | For recommended vs. actual intake | 9 |
| Sauvaget et al. 2004 [35] | JAP | Stroke | 3,731 | 14 | 35-89 | M/F | MUFA | Age, sex, adjusted for radiation dose, city, BMI, smoking status, alcohol habits, and medical history of hypertension and diabetes | Third vs. first tertile | 8 |
| Samieri et al. 2011 [10] | Three city study FRA | Stroke | 7,625 | 5.25 | ≥65 | M/F | Olive oil | Age, sex, education, smoking status, BMI, PA, hypertension, diabetes, and total energy intake | Third vs. first tertile | 8 |
| Solfrizzi et al. 2005 [51] | Italian Longitudinal Study on Aging ITA | All-cause mortality | 278 | 8.5 | 65-84 | F | MUFA MUFA:SFA | Age, sex, waist-hip ratio, smoking status, Charlson co-morbidity index, and total energy intake | Fourth vs. first quartile | 7 |
| Tognon et al. 2011 [24] | DEN | All-cause mortality | 1,037 | 8.5 | 70 | M/F | MUFA:SFA | Gender, BMI, waist circumference, PA, smoking status, marital status and education | ≥ median vs. < median | 7 |
| Trichopoulou et al. 2005 [23] | European Prospective Into Cancer and Nutrition Elderly EU | All-cause mortality | 74,607 | 7.4 | >60 | M/F | MUFA MUFA:SFA | Age, sex, diabetes mellitus at baseline, waist to hip ratio, BMI, educational achievement, smoking status, PA at occupation, PA score at leisure, alcohol intake, and total energy intake | MUFA (12 g) MUFA:SFA (0.4) | 8 |
| Trichopoulou et al. 2009 [20] | European Prospective Into Cancer and Nutrition GRE | All-cause mortality | 23,349 | 8.5 | 20-86 | M/F | MUFA:SFA | Age, sex, education, smoking status, waist-to-hip ratio, BMI, MET score, and total energy intake | ≥ median vs. < median | 9 |
| Trichopoulou et al. 1995 [22] | GRE | All-cause mortality | 182 | 4-5 | >70 | M/F | MUFA:SFA | Age, sex, and smoking status | MUFA:SFA (1 unit) | 7 |
| Trichopoulou et al. 2003 [21] | European Prospective Into Cancer and Nutrition GRE | All-cause mortality | 22,043 | 3.7 | 20-86 | M/F | MUFA Olive oil MUFA:SFA | Age, sex, waist-to-hip ratio, energy-expenditure score, years of education, smoking status, BMI, and total energy intake | MUFA (15 g/d) Increment olive oil (20 g) MUFA:SFA (0.5) | 9 |
| Van den Brandt et al. 2011 [27] | Netherlands cohort study NED | All-cause mortality | 120,852 | 10 | 55-69 | M/F | MUFA:SFA | Age, cigarette smoking status, number of cigarettes smoked per day, years of smoking, BMI, non-occupational PA, history of hypertension, highest level of education, and energy intake | Fourth vs. first quartile | 9 |
| Yaemsiri et al. 2012 [39] | Women’s Health initiative observational study USA | Stroke | 87,025 | 7.6 | 50-79 | F | MUFA | Age, race, education, family income, total metabolic equivalent task hours per week, alcohol intake, history of CHD, history of atrial fibrillation, history of diabetes, aspirin use, use of antihypertensive medication, use of cholesterol-lowering medication, BMI, systolic blood pressure, and total energy intake, dietary vitamin E, fruits and vegetable intake, fibre | Fifth vs. first quintile | 8 |
| Xu et al. 2006 [41] | Strong Heart Study USA | CHD CHD mortality | 2,938 | 7.2 | 47-79 | M/F | MUFA | Age, sex, energy, study centre, diabetes status, BMI, HDL, LDL, triacylglycerol, smoking, alcohol consumption, hypertension, percentage of energy from protein, and total energy intake | Fourth vs. first quartile | 9 |
| Wakai et al. 2014 [30] | Japan Collaborative Cohort Study JAP | All-cause mortality CVD mortality | 58,672 | 19.3 | 40-79 | M/F | MUFA | Age, area, education, smoking, alcohol consumption, BMI, sleep duration, walking, consumption of vegetables and fruit, and total energy intake | Fifth vs. first quintile | 8 |
BMI Body Mass Index, CHD coronary heart disease, CVD cardiovascular disease, DEN Denmark, EDI Elderly Diet Index, EU European Union, FRA France, GBR Great Britain, HDI Healthy Diet Index, ISR Israel, ITA Italy, JAP Japan, MET metabolic equivalent of task, MUFA monounsaturated fatty acids, NED The Netherlands, PA physical activity, SFA saturated fatty acids, SPA Spain, SWE Sweden, WHI Women’s Health Initiative, USA United States of America.
Main outcomes
According to the different clinical outcomes, overall risk of all-cause mortality was evaluated in seventeen cohorts, cardiovascular mortality in fourteen cohorts, combined cardiovascular events in twenty-eight cohort studies, coronary heart disease in fifteen cohorts, and stroke in eleven cohorts, respectively.
Random effects model data (as summarized in Table 2) revealed that top versus bottom third combined MUFA, olive oil, oleic acid, and MUFA:SFA ratio was significantly associated with a reduced risk of: all-cause mortality (relative risk, RR: 0.89, 95% confidence interval 0.83 to 0.96; p = 0.001, I2 = 64%) (Figure 1), cardiovascular mortality (RR: 0.88, 95% CI 0.80 to 0.96, p = 0.004, I2 = 50%) (Figure 2), combined cardiovascular events (RR: 0.91, 95% CI 0.86 to 0.96, p = 0.001, I2 = 58%) (Figure 3), and stroke (RR: 0.83, 95% CI 0.71 to 0.97, p = 0.02, I2 = 70%). In contrast, no significant changes could be observed for coronary heart disease (RR: 0.96, 95% CI 0.90 to 1.01, p = 0.13, I2 = 41%).
Table 2.
Relative risk for all-cause mortality, cardiovascular mortality, combined cardiovascular events, stroke, and coronary heart disease (with 95% confidence intervals) comparing the top versus bottom third of MUFA, MUFA:SFA ratio, olive oil, and oleic acid
| Outcome | No studies | MUFA source | Relative risk | 95% CI | p-value | I 2 (%) a 95% CI |
|---|---|---|---|---|---|---|
| All-cause mortality | 17 | All MUFA combined | 0.89 | 0.83 to 0.96 | 0.001 | 64 |
| 42 to 78 | ||||||
| 5 | MUFA | 1.00 | 0.93 to 1.08 | 0.93 | 23 | |
| 10 | MUFA:SFA | 0.90 | 0.82 to 1.00 | 0.04 | 59 | |
| 5 | Olive oil | 0.77 | 0.71 to 0.84 | <0.00001 | 0 | |
| Cardiovascular mortality | 14 | All MUFA combined | 0.88 | 0.80 to 0.96 | 0.004 | 50 |
| 15 to 71 | ||||||
| 8 | MUFA | 0.96 | 0.89 to 1.04 | 0.36 | 7 | |
| 4 | MUFA:SFA | 0.91 | 0.83 to 0.99 | 0.04 | 0 | |
| 5 | Olive oil | 0.70 | 0.48 to 1.03 | 0.07 | 71 | |
| 1 | Oleic acid | 0.81 | 0.66 to 0.99 | 0.04 | n.a. | |
| Combined cardiovascular events | 30 | All MUFA combined | 0.91 | 0.86 to 0.96 | 0.001 | 58 |
| 38 to 71 | ||||||
| 20 | MUFA | 0.95 | 0.89 to 1.02 | 0.14 | 52 | |
| 6 | MUFA:SFA | 0.93 | 0.86 to 1.01 | 0.07 | 0 | |
| 7 | Olive oil | 0.72 | 0.57 to 0.91 | 0.007 | 75 | |
| 1 | Oleic acid | 0.87 | 0.76 to 1.00 | 0.04 | n.a. | |
| Stroke | 11 | All MUFA combined | 0.83 | 0.71 to 0.97 | 0.02 | 70 |
| 46 to 84 | ||||||
| 9 | MUFA | 0.85 | 0.72 to 1.01 | 0.07 | 65 | |
| 1 | MUFA:SFA | 1.18 | 0.91 to 1.53 | 0.21 | n.a. | |
| 2 | Olive oil | 0.60 | 0.47 to 0.77 | <0.0001 | 0 | |
| Coronary heart disease | 15 | All MUFA combined | 0.96 | 0.90 to 1.01 | 0.13 | 41 |
| 0 to 66 | ||||||
| 9 | MUFA | 0.99 | 0.93 to 1.06 | 0.76 | 29 | |
| 4 | MUFA:SFA | 0.94 | 0.86 to 1.02 | 0.14 | 0 | |
| 4 | Olive oil | 0.80 | 0.57 to 1.14 | 0.22 | 77 | |
| 1 | Oleic acid | 0.87 | 0.76 to 1.00 | 0.04 | n.a. |
a I 2 inconsistency, percentage of variation across studies due to heterogeneity.
MUFA monounsaturated fatty acids, n.a. not applicable, SFA saturated fatty acids.
Figure 1.
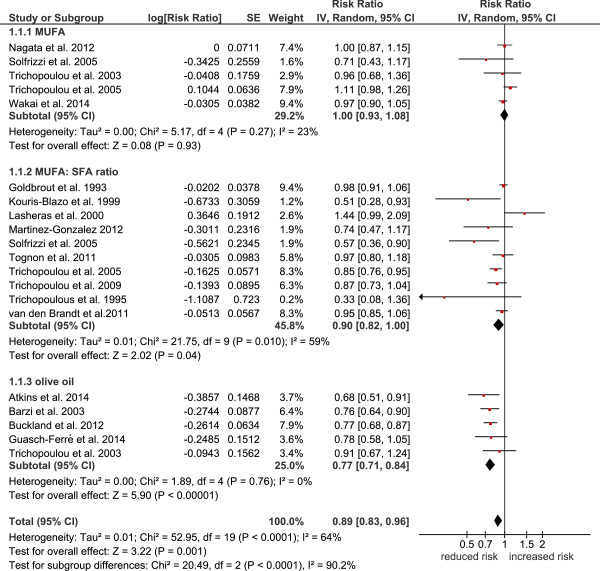
Forest plot showing pooled relative risks (RRs) with 95% CI for all-cause mortality comparing the top versus bottom third of the distribution of MUFA, MUFA:SFA ratio, olive oil, and oleic acid. I2: Inconsistency; MUFA: monounsaturated fatty acids; SE: standard error; SFA: saturated fatty acids.
Figure 2.
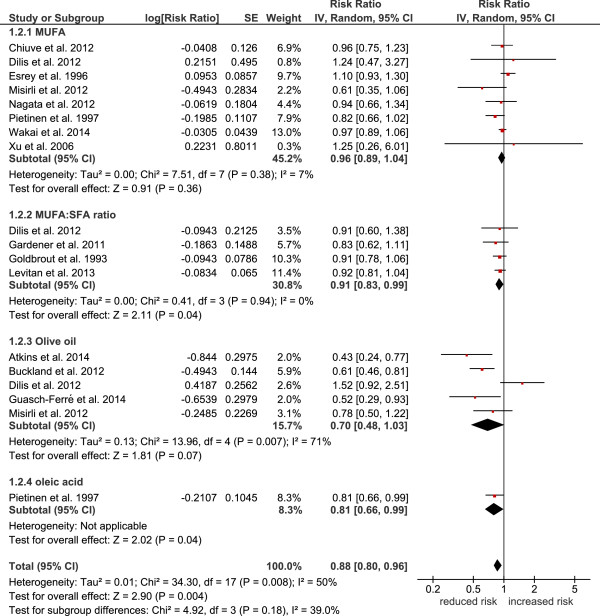
Forest plot showing pooled relative risks (RRs) with 95% CI for cardiovascular mortality comparing the top versus bottom third of the distribution of MUFA, MUFA:SFA ratio, olive oil, and oleic acid. I2: Inconsistency; MUFA: monounsaturated fatty acids; SE: standard error; SFA: saturated fatty acids.
Figure 3.
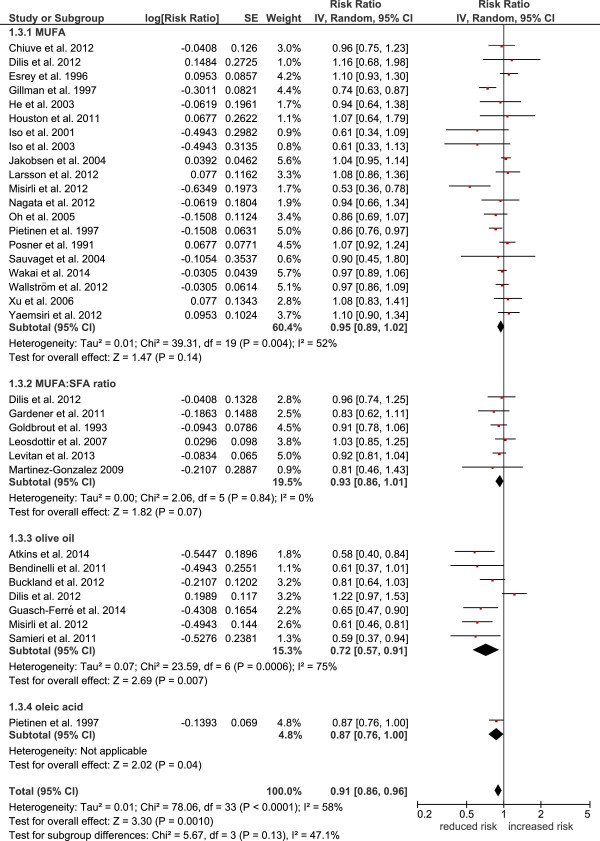
Forest plot showing pooled relative risks (RRs) with 95% CI for combined cardiovascular events comparing the top versus bottom third of the distribution of MUFA, MUFA:SFA ratio, olive oil, and oleic acid. I2: Inconsistency; MUFA: monounsaturated fatty acids; SE: standard error; SFA: saturated fatty acids.
Subgroup/sensitivity analyses
Following subgroup analyses, olive oil most likely turned out to be crucial for the results of the primary analysis, since significant associations could only be found between higher intakes of olive oil and reduced risk of all-cause mortality (RR: 0.77, 95% CI 0.71 to 0.84, p < 0.00001, I2 = 0%), cardiovascular events (RR: 0.72, 95% CI 0.57 to 0.91, p = 0.007, I2 = 77%), and stroke (RR: 0.60, 95% CI 0.47 to 0.77, p < 0.0001, I2 = 0%), respectively. Subgroup analysis for MUFA (of mixed animal and plant origin) did not reveal any significant risk reduction for all-cause mortality (RR: 1.00, 95% CI 0.93 to 1.08, p = 0.93, I2 = 23%), cardiovascular mortality (RR: 0.95, 95% CI 0.89 to 1.02, p = 0.14, I2 = 52%), cardiovascular events (RR: 0.96, 95% CI 0.89 to 1.04, p = 0.36, I2 = 7%), coronary heart disease (RR: 0.99, 95% CI 0.93 to 1.06, p = 0.76, I2 = 29%), and stroke (RR: 0.85, 95% CI 0.72 to 1.01, p = 0.07, I2 = 65%). To investigate statistical heterogeneity, sensitivity analyses were performed with the metaan command in STATA. Heterogeneity of the main analysis could be confirmed in the sensitivity analyses. Differentiating between studies performed in Europe vs. non-European investigations resulted in significant differences as compared to the main analysis. Pooling European based cohorts resulted in a significant risk reduction for all-cause mortality (RR: 0.87, 95% CI 0.79 to 0.95) as well as for cardiovascular mortality (RR: 0.76, 95% CI 0.64 to 0.91) and cardiovascular events (RR: 0.86, 95% CI 0.78, 0.95). In contrast, no significant reduction in all-cause mortality risk (RR: 0.97, 95% CI 0.91 to 1.04) could be observed for non-European cohorts (the respective data for cardiovascular mortality being RR: 0.94, 95% CI 0.89 to 0.99 and for cardiovascular events being RR: 0.93, 95% CI 0.87 to 0.98). With respect to study length, studies with a follow-up ≥ 10 years resulted in similar results as compared to short-term studies (<10 years follow up). Likewise, high quality studies could confirm the results of the primary analysis.
Publication bias
The Egger’s linear regression tests provided evidence for a potential publication bias for combined cardiovascular events (p = 0.018), all-cause mortality (p = 0.041), and cardiovascular mortality (p = 0.12) following comparison of the top versus bottom third combined MUFA, olive oil, oleic acid, and MUFA:SFA ratio. No evidence of publication bias could be detected for risk of CHD (p = 0.28) and stroke (p = 0.28). All funnel plots indicate little to moderate asymmetry, suggesting that publication bias cannot be completely excluded as a factor of influence on the present meta-analysis (Additional file 1: Figures S1, S2, S3, S4 and S5). It remains possible that small studies with inconclusive results have not been published or failed to do so.
Discussion
In the present meta-analysis, comparison of the top versus the bottom third of combined MUFA subgroups (MUFA, olive oil, oleic acid, and MUFA:SFA) was associated with reduced risk of all-cause mortality (11%), cardiovascular mortality (12%), combined cardiovascular events (9%), and stroke (17%). In the ensuing subgroup analyses, this significant correlation could only be observed between higher intakes of olive oil and reduced risk of all-cause mortality, cardiovascular events, and stroke, respectively. In contrast, monounsaturated fatty acids of mixed animal and plant origin did not result in any significant effects with respect to these outcome parameters. Thus, it seems possible that olive oil represents the crucial factor of influence for the protective health effects observed in the primary analysis. However, one has to keep in mind the limitations of the present systematic review and meta-analysis summarized at the end of this section, especially the fact that the specific sources of MUFA have not been indicated in every study.
In order to properly evaluate the potential beneficial or detrimental effects of MUFA with respect to cardiovascular diseases, it seems of importance to consider the source of food providing these fatty acids. In the Nurses’ Health Study, MUFA intake was highly correlated with SFA intake (correlation coefficient of 0.81) but only moderately correlated with intakes of PUFA (correlation coefficient of 0.30), suggesting that fat was primarily of animal origin [58]. In the different EPIC cohorts, MUFA intakes ranged between approximately 10% of daily total energy consumption (TEC) in The Netherlands and ~ 20% of TEC in Greece. In general, intake of MUFA was higher in southern European countries as compared central or northern cohorts. However, another distinguishing feature seems to be the predominant source of MUFA in the respective cohorts. In Greece, Spain, and Italy, fat of plant origin (mainly olive oil) provided up to 64% of MUFA intake, whereas in most other EPIC centers, the main contributors to total MUFA intake were meat and meat products, added fats, and dairy products [8]. This might also provide an explanation for the somewhat mixed results provided by systematic reviews and meta-analyses in the past. Thus, a diet rich in MUFA was found to have beneficial effects on a broad range of CVD risk factors, not only in the primary prevention of CVD [1, 59–61]. On the other hand, no association between total and individual MUFA and CHD was reported in a meta-analysis of studies assessing both dietary intake and circulating fatty acid composition, [7] while a meta-analysis of observational studies suggested that replacing SFAs with PUFAs might have a greater benefit than replacement of SFAs by MUFA [4]. There is some evidence drawn from prospective studies of an adverse association between MUFA and coronary events, but this correlation might be influenced by high amounts of MUFA of animal origin [4].
A number of in-vivo and in-vitro studies examined the health effects of extra virgin olive oil, the potential “Unique Selling Proposition” of a genuine Mediterranean diet. Thus, the Di@bet.es study demonstrated that individuals who consumed olive oil had a significantly lower risk of developing obesity, impaired glucose metabolism, hypertriglyceridemia, and lower HDL cholesterol levels as compared to a group consuming sunflower oil [62]. In addition, results from experimental studies provide evidence that olive oil consumption improves several CHD risk factors [63, 64]. The PREDIMED dietary intervention trial aimed a intake of 50 g/d or more of extra virgin olive oil observed a significant risk reduction of both combined cardiovascular events as well as primary stroke, but not of CHD, indicating a consistency with the results of the present meta-analyses of cohort studies [9]. In a long-term intervention trial by Esposito et al., a higher regression in as well as a lower rate of progression of the intima–media thickness of the carotid artery was found in the group adopting a Mediterranean diet as compared to a low-fat diet reference arm [65].
Apart from oleic acid, olive oil contains a number of bioactive compounds such as polyphenols which are especially prominent in virgin and extra-virgin olive oil, but not in refined olive oil [64, 66]. A key olive oil polyphenol is oleuropein (a compound that generates tyrosol and hydroxytyrosol), which accounts for approximately 80% of olive oil phenolic content and is a potent scavenger of superoxide radicals and inhibits LDL oxidation [67, 68]. There is a causal link between oxidative stress, inflammation, endothelial dysfunction, and CVD/CHD [69]. A meta-analysis of intervention trials provide evidence that an MD decreases inflammation and improves endothelial function [70]. When focusing on virgin olive oil consumption, the inverse correlation between olive oil and CHD risk found in the present meta-analysis is consistent with the fact that olive oil is not just a supplier of MUFA but of other biologically active components as well.
Several limitations should be taken into account when interpreting the results of the present meta-analysis. MUFA coexist with SFA in several food sources. In addition, cis- and trans-isomers of MUFAs were sometimes categorized together in cohort studies. Furthermore, moderate to substantial heterogeneity could be observed in the present meta-analysis. Potential sources of heterogeneity include combining MUFA/olive oil/oleic acid/MUFA:SFA ratio in the same analysis, heterogeneous risk estimates, heterogeneous populations/ages/gender, sample sizes as well as follow-up periods of the included studies. No unpublished data were considered for the present meta-analysis, and it cannot be excluded that these results may influence the effect size estimates. Examination of funnel plots showed little to moderate asymmetry suggesting that publication bias cannot be completely excluded as a confounder of the present meta-analysis (e.g. it remains possible that small studies yielding inconclusive data have not been published). In addition, the specific food sources of MUFA could not always identified, limiting the validity of any general recommendation towards MUFAs of plant origin (it is most likely olive oil, but it might be other types of food as well, e.g. nuts, canola oil or a specific variety of sunflower oil). Conversely, it might be that results from studies using mixed sources of MUFA might be biased by non-identified olive oil, making MUFA appear to be beneficial in general when some sources are not. Furthermore, observational studies including cohort studies assessing outcome events affected by nutrition should be interpreted with caution, since reliance on nutritional assessment methods with validity and reliability is lower when compared to randomized controlled trials.
However, the present study has some complementary strengths as well. Compared to cohort studies, dietary intervention trials are often limited by lack of double blinding, non-compliance, cross-over, and high drop-out rates. Therefore, well-designed analyses in prospective cohort studies could also provide important evidence with respect to long-term clinical outcomes. Another strength of this work is the inclusion of an overall population >800,000 subjects. To the best of our knowledge, this represents the most comprehensive summary of the evidence on MUFA, olive oil, MUFA:SFA on hard clinical outcome parameters.
Conclusion
The results of the present meta-analysis indicate an overall risk reduction of all-cause mortality (11%), cardiovascular mortality (12%), cardiovascular events (9%), and stroke (17%) when comparing the top vs. bottom thirds of a combination of MUFA, olive oil, oleic acid, and MUFA:SFA ratio. Monounsaturated fat of mixed animal and vegetable sources per se did not yield any significant effects on these outcome parameters. Subgroup analysis indicated that only olive oil (the primary monounsaturated fat source in south European countries) is was associated with a significant risk reduction for several outcomes. These data provide evidence that the source and origin of MUFA within a specific diet should be taken into account in order to evaluate the potential benefits of this type of fatty acids. Further studies are required evaluating specific food sources of MUFA and risk of all-cause mortality and CVD events.
Electronic supplementary material
Additional file 1: Detailed search strategy; Figure S1-S5: Funnel Plots. (DOCX 44 KB)
Footnotes
Competing interests
Both authors declare that they have no competing interest.
Authors’ contributions
LS and GH conducted the data analysis, interpretation of results, manuscript drafting, and finalizing manuscript. Both authors read and approved the final manuscript.
Contributor Information
Lukas Schwingshackl, Email: lukas.schwingshackl@univie.ac.at.
Georg Hoffmann, Email: georg.hoffmann@univie.ac.at.
References
- 1.Schwingshackl L, Hoffmann G. Monounsaturated fatty acids and risk of cardiovascular disease: synopsis of the evidence available from systematic reviews and meta-analyses. Nutr. 2012;4(12):1989–2007. doi: 10.3390/nu4121989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vannice G, Rasmussen H. Position of the academy of nutrition and dietetics: dietary fatty acids for healthy adults. J Acad Nutr Diet. 2014;114(1):136–153. doi: 10.1016/j.jand.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Kris-Etherton PM. AHA science advisory. Monounsaturated fatty acids and risk of cardiovascular disease. American heart association. Nutrition committee. Circulation. 1999;100(11):1253–1258. doi: 10.1161/01.CIR.100.11.1253. [DOI] [PubMed] [Google Scholar]
- 4.Jakobsen MU, O’Reilly EJ, Heitmann BL, Pereira MA, Balter K, Fraser GE, Goldbourt U, Hallmans G, Knekt P, Liu S, Pietinen P, Spiegelman D, Stevens J, Virtamo J, Willett WC, Ascherio A. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. Am J Clin Nutr. 2009;89(5):1425–1432. doi: 10.3945/ajcn.2008.27124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 6.Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55(1–3):173–201. doi: 10.1159/000229002. [DOI] [PubMed] [Google Scholar]
- 7.Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, Franco OH, Butterworth AS, Forouhi NG, Thompson SG, Khaw KT, Mozaffarian D, Danesh J, Di Angelantonio E. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160(6):398–406. doi: 10.7326/M13-1788. [DOI] [PubMed] [Google Scholar]
- 8.Linseisen J, Welch AA, Ocke M, Amiano P, Agnoli C, Ferrari P, Sonestedt E, Chajes V, Bueno-de-Mesquita HB, Kaaks R, Weikert C, Dorronsoro M, Rodríguez L, Ermini I, Mattiello A, van der Schouw YT, Manjer J, Nilsson S, Jenab M, Lund E, Brustad M, Halkjaer J, Jakobsen MU, Khaw KT, Crowe F, Georgila C, Misirli G, Niravong M, Touvier M, Bingham S, et al. Dietary fat intake in the european prospective investigation into cancer and nutrition: results from the 24-h dietary recalls. Eur J Clin Nutr. 2009;63(Suppl 4):S61–S80. doi: 10.1038/ejcn.2009.75. [DOI] [PubMed] [Google Scholar]
- 9.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Martínez-González MA. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 10.Samieri C, Feart C, Proust-Lima C, Peuchant E, Tzourio C, Stapf C, Berr C, Barberger-Gateau P. Olive oil consumption, plasma oleic acid, and stroke incidence the three-city study. Neurology. 2011;77(5):418–425. doi: 10.1212/WNL.0b013e318220abeb. [DOI] [PubMed] [Google Scholar]
- 11.Buckland G, Mayen AL, Agudo A, Travier N, Navarro C, Huerta JM, Chirlaque MD, Barricarte A, Ardanaz E, Moreno-Iribas C, Marin P, Quirós JR, Redondo ML, Amiano P, Dorronsoro M, Arriola L, Molina E, Sanchez MJ, Gonzalez CA. Olive oil intake and mortality within the Spanish population (EPIC-Spain) Am J Clin Nutr. 2012;96(1):142–149. doi: 10.3945/ajcn.111.024216. [DOI] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P: The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses.http://www.medicine.mcgill.ca/rtamblyn/Readings%5CThe%20Newcastle%20-%20Scale%20for%20assessing%20the%20quality%20of%20nonrandomised%20studies%20in%20meta-analyses.pdf (08.06.2014)
- 14.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kontopantelis E, Reeves D. Metaan: random-effects meta-analysis. Stata J. 2010;10(3):395–407. [Google Scholar]
- 18.Goldbourt U, Yaari S, Medalie JH. Factors predictive of long-term coronary heart disease mortality among 10,059 male israeli civil servants and municipal employees. A 23-year mortality follow-up in the Israeli ischemic heart disease study. Cardiology. 1993;82(2–3):100–121. doi: 10.1159/000175862. [DOI] [PubMed] [Google Scholar]
- 19.Dilis V, Katsoulis M, Lagiou P, Trichopoulos D, Naska A, Trichopoulou A. Mediterranean diet and CHD: the greek european prospective investigation into cancer and nutrition cohort. Br J Nutr. 2012;108(4):699–709. doi: 10.1017/S0007114512001821. [DOI] [PubMed] [Google Scholar]
- 20.Trichopoulou A, Bamia C, Trichopoulos D. Anatomy of health effects of Mediterranean diet: greek EPIC prospective cohort study. BMJ. 2009;338:b2337. doi: 10.1136/bmj.b2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a greek population. N Engl J Med. 2003;348(26):2599–2608. doi: 10.1056/NEJMoa025039. [DOI] [PubMed] [Google Scholar]
- 22.Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. BMJ. 1995;311(7018):1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trichopoulou A, Orfanos P, Norat T, Bueno-de-Mesquita B, Ocke MC, Peeters PH, van der Schouw YT, Boeing H, Hoffmann K, Boffetta P, Nagel G, Masala G, Krogh V, Panico S, Tumino R, Vineis P, Bamia C, Naska A, Benetou V, Ferrari P, Slimani N, Pera G, Martinez-Garcia C, Navarro C, Rodriguez-Barranco M, Dorronsoro M, Spencer EA, Key TJ, Bingham S, Khaw KT, et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ. 2005;330(7498):991. doi: 10.1136/bmj.38415.644155.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tognon G, Rothenberg E, Eiben G, Sundh V, Winkvist A, Lissner L. Does the Mediterranean diet predict longevity in the elderly? A Swedish perspective. Age (Dordr) 2011;33(3):439–450. doi: 10.1007/s11357-010-9193-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez-Gonzalez MA, Guillen-Grima F, De Irala J, Ruiz-Canela M, Bes-Rastrollo M, Beunza JJ, Lopez Del Burgo C, Toledo E, Carlos S, Sanchez-Villegas A. The Mediterranean diet is associated with a reduction in premature mortality among middle-aged adults. J Nutr. 2012;142(9):1672–1678. doi: 10.3945/jn.112.162891. [DOI] [PubMed] [Google Scholar]
- 26.Lasheras C, Fernandez S, Patterson AM. Mediterranean diet and age with respect to overall survival in institutionalized, nonsmoking elderly people. Am J Clin Nutr. 2000;71(4):987–992. doi: 10.1093/ajcn/71.4.987. [DOI] [PubMed] [Google Scholar]
- 27.van den Brandt PA. The impact of a Mediterranean diet and healthy lifestyle on premature mortality in men and women. Am J Clin Nutr. 2011;94(3):913–920. doi: 10.3945/ajcn.110.008250. [DOI] [PubMed] [Google Scholar]
- 28.Leosdottir M, Nilsson PM, Nilsson JA, Berglund G. Cardiovascular event risk in relation to dietary fat intake in middle-aged individuals: data from the malmo diet and cancer study. Eur J Cardiovasc Prev Rehabil. 2007;14(5):701–706. doi: 10.1097/HJR.0b013e3282a56c45. [DOI] [PubMed] [Google Scholar]
- 29.Wallstrom P, Sonestedt E, Hlebowicz J, Ericson U, Drake I, Persson M, Gullberg B, Hedblad B, Wirfalt E. Dietary fiber and saturated fat intake associations with cardiovascular disease differ by sex in the malmo diet and cancer cohort: a prospective study. PLoS One. 2012;7(2):e31637. doi: 10.1371/journal.pone.0031637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wakai K, Naito M, Date C, Iso H, Tamakoshi A, Group JS. Dietary intakes of fat and total mortality among japanese populations with a low fat intake: the Japan collaborative cohort (JACC) study. Nutri Metabol. 2014;11(1):12. doi: 10.1186/1743-7075-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagata C, Nakamura K, Wada K, Oba S, Tsuji M, Tamai Y, Kawachi T. Total fat intake is associated with decreased mortality in Japanese men but not in women. J Nutri. 2012;142(9):1713–1719. doi: 10.3945/jn.112.161661. [DOI] [PubMed] [Google Scholar]
- 32.Chiuve SE, Rimm EB, Sandhu RK, Bernstein AM, Rexrode KM, Manson JE, Willett WC, Albert CM. Dietary fat quality and risk of sudden cardiac death in women. Am J Clin Nutr. 2012;96(3):498–507. doi: 10.3945/ajcn.112.040287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oh K, Hu FB, Manson JE, Stampfer MJ, Willett WC. Dietary fat intake and risk of coronary heart disease in women: 20 years of follow-up of the nurses’ health study. Am J Epidemiol. 2005;161(7):672–679. doi: 10.1093/aje/kwi085. [DOI] [PubMed] [Google Scholar]
- 34.Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. High diet quality is associated with a lower risk of cardiovascular disease and all-cause mortality in older men. J Nutr. 2014;144(5):673–680. doi: 10.3945/jn.113.186486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sauvaget C, Nagano J, Hayashi M, Yamada M. Animal protein, animal fat, and cholesterol intakes and risk of cerebral infarction mortality in the adult health study. Stroke. 2004;35(7):1531–1537. doi: 10.1161/01.STR.0000130426.52064.09. [DOI] [PubMed] [Google Scholar]
- 36.Iso H, Sato S, Kitamura A, Naito Y, Shimamoto T, Komachi Y. Fat and protein intakes and risk of intraparenchymal hemorrhage among middle-aged Japanese. Am J Epidemiol. 2003;157(1):32–39. doi: 10.1093/aje/kwf166. [DOI] [PubMed] [Google Scholar]
- 37.Iso H, Stampfer MJ, Manson JE, Rexrode K, Hu F, Hennekens CH, Colditz GA, Speizer FE, Willett WC. Prospective study of fat and protein intake and risk of intraparenchymal hemorrhage in women. Circulation. 2001;103(6):856–863. doi: 10.1161/01.CIR.103.6.856. [DOI] [PubMed] [Google Scholar]
- 38.Houston DK, Ding J, Lee JS, Garcia M, Kanaya AM, Tylavsky FA, Newman AB, Visser M, Kritchevsky SB, Health ABCS. Dietary fat and cholesterol and risk of cardiovascular disease in older adults: the health ABC study. Nutr Metab Cardiovasc Dis. 2011;21(6):430–437. doi: 10.1016/j.numecd.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yaemsiri S, Sen S, Tinker L, Rosamond W, Wassertheil-Smoller S, He K. Trans fat, aspirin, and ischemic stroke in postmenopausal women. Ann Neurol. 2012;72(5):704–715. doi: 10.1002/ana.23555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gillman MW, Cupples LA, Millen BE, Ellison RC, Wolf PA. Inverse association of dietary fat with development of ischemic stroke in men. JAMA. 1997;278(24):2145–2150. doi: 10.1001/jama.1997.03550240035030. [DOI] [PubMed] [Google Scholar]
- 41.Xu J, Eilat-Adar S, Loria C, Goldbourt U, Howard BV, Fabsitz RR, Zephier EM, Mattil C, Lee ET. Dietary fat intake and risk of coronary heart disease: the strong heart study. Am J Clin Nutr. 2006;84(4):894–902. doi: 10.1093/ajcn/84.4.894. [DOI] [PubMed] [Google Scholar]
- 42.Esrey KL, Joseph L, Grover SA. Relationship between dietary intake and coronary heart disease mortality: lipid research clinics prevalence follow-up study. J Clin Epidemiol. 1996;49(2):211–216. doi: 10.1016/0895-4356(95)00066-6. [DOI] [PubMed] [Google Scholar]
- 43.Gardener H, Wright CB, Gu Y, Demmer RT, Boden-Albala B, Elkind MS, Sacco RL, Scarmeas N. Mediterranean-style diet and risk of ischemic stroke, myocardial infarction, and vascular death: the Northern Manhattan Study. Am J Clin Nutr. 2011;94(6):1458–1464. doi: 10.3945/ajcn.111.012799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jakobsen MU, Overvad K, Dyerberg J, Schroll M, Heitmann BL. Dietary fat and risk of coronary heart disease: possible effect modification by gender and age. Am J Epidemiol. 2004;160(2):141–149. doi: 10.1093/aje/kwh193. [DOI] [PubMed] [Google Scholar]
- 45.Martinez-Gonzalez MA, Garcia-Lopez M, Bes-Rastrollo M, Toledo E, Martinez-Lapiscina EH, Delgado-Rodriguez M, Vazquez Z, Benito S, Beunza JJ. Mediterranean diet and the incidence of cardiovascular disease: a Spanish cohort. Nutr Metab Cardiovasc Dis. 2011;21(4):237–244. doi: 10.1016/j.numecd.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 46.Posner BM, Cobb JL, Belanger AJ, Cupples LA, D’Agostino RB, Stokes J., 3rd Dietary lipid predictors of coronary heart disease in men. The framingham study. Arch Intern Med. 1991;151(6):1181–1187. doi: 10.1001/archinte.1991.00400060105018. [DOI] [PubMed] [Google Scholar]
- 47.He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC, Ascherio A. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ. 2003;327(7418):777–782. doi: 10.1136/bmj.327.7418.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larsson SC, Virtamo J, Wolk A. Dietary fats and dietary cholesterol and risk of stroke in women. Atherosclerosis. 2012;221(1):282–286. doi: 10.1016/j.atherosclerosis.2011.12.043. [DOI] [PubMed] [Google Scholar]
- 49.Bendinelli B, Masala G, Saieva C, Salvini S, Calonico C, Sacerdote C, Agnoli C, Grioni S, Frasca G, Mattiello A, Chiodini P, Tumino R, Vineis P, Palli D, Panico S. Fruit, vegetables, and olive oil and risk of coronary heart disease in italian women: the EPICOR study. Am J Clin Nutr. 2011;93(2):275–283. doi: 10.3945/ajcn.110.000521. [DOI] [PubMed] [Google Scholar]
- 50.Barzi F, Woodward M, Marfisi RM, Tavazzi L, Valagussa F, Marchioli R, Investigators GI-P. Mediterranean diet and all-causes mortality after myocardial infarction: results from the GISSI-prevenzione trial. Eur J Clin Nutr. 2003;57(4):604–611. doi: 10.1038/sj.ejcn.1601575. [DOI] [PubMed] [Google Scholar]
- 51.Solfrizzi V, D’Introno A, Colacicco AM, Capurso C, Palasciano R, Capurso S, Torres F, Capurso A, Panza F. Unsaturated fatty acids intake and all-causes mortality: a 8.5-year follow-up of the Italian longitudinal study on aging. Exp Gerontol. 2005;40(4):335–343. doi: 10.1016/j.exger.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 52.Misirli G, Benetou V, Lagiou P, Bamia C, Trichopoulos D, Trichopoulou A. Relation of the traditional Mediterranean diet to cerebrovascular disease in a Mediterranean population. Am J Epidemiol. 2012;176(12):1185–1192. doi: 10.1093/aje/kws205. [DOI] [PubMed] [Google Scholar]
- 53.Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, Virtamo J. Intake of fatty acids and risk of coronary heart disease in a cohort of finnish men. The alpha-tocopherol, beta-carotene cancer prevention study. Am J Epidemiol. 1997;145(10):876–887. doi: 10.1093/oxfordjournals.aje.a009047. [DOI] [PubMed] [Google Scholar]
- 54.Guasch-Ferre M, Hu FB, Martinez-Gonzalez MA, Fito M, Bullo M, Estruch R, Ros E, Corella D, Recondo J, Gomez-Gracia E, Fiol M, Lapetra J, Serra-Majem L, Muñoz MA, Pintó X, Lamuela-Raventós RM, Basora J, Buil-Cosiales P, Sorlí JV, Ruiz-Gutiérrez V, Martínez JA, Salas-Salvadó J. Olive oil intake and risk of cardiovascular disease and mortality in the PREDIMED study. BMC Med. 2014;12(1):78. doi: 10.1186/1741-7015-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kouris-Blazos A, Gnardellis C, Wahlqvist ML, Trichopoulos D, Lukito W, Trichopoulou A. Are the advantages of the Mediterranean diet transferable to other populations? A cohort study in Melbourne, Australia. Br J Nutr. 1999;82(1):57–61. doi: 10.1017/s0007114599001129. [DOI] [PubMed] [Google Scholar]
- 56.Buckland G, Travier N, Barricarte A, Ardanaz E, Moreno-Iribas C, Sánchez MJ, Molina-Montes E, Chirlaque MD, Huerta JM, Navarro C, Redondo ML, Amiano P, Dorronsoro M, Larrañaga N, Gonzalez CA. Olive oil intake and CHD in the European Prospective Investigation into Cancer and Nutrition Spanish cohort. Br J Nutr. 2012;108(11):2075–2082. doi: 10.1017/S000711451200298X. [DOI] [PubMed] [Google Scholar]
- 57.Levitan EB, Lewis CE, Tinker LF, Eaton CB, Ahmed A, Manson JE, Snetselaar LG, Martin LW, Trevisan M, Howard BV, Shikany JM. Mediterranean and DASH diet scores and mortality in women with heart failure: The Women’s Health Initiative. Circ Heart Fail. 2013;6(6):1116–1123. doi: 10.1161/CIRCHEARTFAILURE.113.000495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hu FB, Stampfer MJ, Manson JE, Rimm E, Colditz GA, Rosner BA, Hennekens CH, Willett WC. Dietary fat intake and the risk of coronary heart disease in women. N Engl J Med. 1997;337(21):1491–1499. doi: 10.1056/NEJM199711203372102. [DOI] [PubMed] [Google Scholar]
- 59.Schwingshackl L, Strasser B. High-MUFA diets reduce fasting glucose in patients with type 2 diabetes. Ann Nutr Metab. 2012;60(1):33–34. doi: 10.1159/000335162. [DOI] [PubMed] [Google Scholar]
- 60.Schwingshackl L, Strasser B, Hoffmann G. Effects of monounsaturated fatty acids on cardiovascular risk factors: a systematic review and meta-analysis. Ann Nutr Metab. 2011;59(2–4):176–186. doi: 10.1159/000334071. [DOI] [PubMed] [Google Scholar]
- 61.Schwingshackl L, Strasser B, Hoffmann G. Effects of monounsaturated fatty acids on glycaemic control in patients with abnormal glucose metabolism: a systematic review and meta-analysis. Ann Nutr Metab. 2011;58(4):290–296. doi: 10.1159/000331214. [DOI] [PubMed] [Google Scholar]
- 62.Soriguer F, Rojo-Martinez G, Goday A, Bosch-Comas A, Bordiu E, Caballero-Diaz F, Calle-Pascual A, Carmena R, Casamitjana R, Castano L, Castell C, Catalá M, Delgado E, Franch J, Gaztambide S, Girbés J, Gomis R, Gutiérrez G, López-Alba A, Teresa Martínez-Larrad M, Menéndez E, Mora-Peces I, Ortega E, Pascual-Manich G, Serrano-Rios M, Urrutia I, Valdés S, Antonio Vázquez J, Vendrell J. Olive oil has a beneficial effect on impaired glucose regulation and other cardiometabolic risk factors. Di@bet.es study. Eur J Clin Nutr. 2013;67(9):911–916. doi: 10.1038/ejcn.2013.130. [DOI] [PubMed] [Google Scholar]
- 63.Covas MI, Konstantinidou V, Fito M. Olive oil and cardiovascular health. J Cardiovasc Pharmacol. 2009;54(6):477–482. doi: 10.1097/FJC.0b013e3181c5e7fd. [DOI] [PubMed] [Google Scholar]
- 64.Lopez-Miranda J, Perez-Jimenez F, Ros E, De Caterina R, Badimon L, Covas MI, Escrich E, Ordovas JM, Soriguer F, Abia R, de la Lastra CA, Battino M, Corella D, Chamorro-Quirós J, Delgado-Lista J, Giugliano D, Esposito K, Estruch R, Fernandez-Real JM, Gaforio JJ, La Vecchia C, Lairon D, López-Segura F, Mata P, Menéndez JA, Muriana FJ, Osada J, Panagiotakos DB, Paniagua JA, Pérez-Martinez P, et al. Olive oil and health: summary of the II international conference on olive oil and health consensus report, Jaen and Cordoba (Spain) 2008. Nutri Metabol Cardiovasc Dis NMCD. 2010;20(4):284–294. doi: 10.1016/j.numecd.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 65.Esposito K, Giugliano D, Nappo F, Marfella R, Campanian Postprandial Hyperglycemia Study G Regression of carotid atherosclerosis by control of postprandial hyperglycemia in type 2 diabetes mellitus. Circulation. 2004;110(2):214–219. doi: 10.1161/01.CIR.0000134501.57864.66. [DOI] [PubMed] [Google Scholar]
- 66.Visioli F, Bernardini E. Extra virgin olive oil’s polyphenols: biological activities. Curr Pharm Des. 2011;17(8):786–804. doi: 10.2174/138161211795428885. [DOI] [PubMed] [Google Scholar]
- 67.Perez-Jimenez F, Ruano J, Perez-Martinez P, Lopez-Segura F, Lopez-Miranda J. The influence of olive oil on human health: not a question of fat alone. Mol Nutr Food Res. 2007;51(10):1199–1208. doi: 10.1002/mnfr.200790023. [DOI] [PubMed] [Google Scholar]
- 68.Visioli F, Bellomo G, Galli C. Free radical-scavenging properties of olive oil polyphenols. Biochem Biophys Res Commun. 1998;247(1):60–64. doi: 10.1006/bbrc.1998.8735. [DOI] [PubMed] [Google Scholar]
- 69.Marin C, Yubero-Serrano EM, Lopez-Miranda J, Perez-Jimenez F. Endothelial aging associated with oxidative stress can be modulated by a healthy mediterranean diet. Int J Mol Sci. 2013;14(5):8869–8889. doi: 10.3390/ijms14058869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schwingshackl L, Hoffmann G. Mediterranean dietary pattern, inflammation and endothelial function: a systematic review and meta-analysis of intervention trials. Nutri Metabol Cardiovasc Dis NMCD. 2014;24(9):929–939. doi: 10.1016/j.numecd.2014.03.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Detailed search strategy; Figure S1-S5: Funnel Plots. (DOCX 44 KB)


