Abstract
Background
The relationship between insight and internalized stigma in patients with schizophrenia is important both for theoretical and practical reasons because of its close association with patients' willingness to seek (or accept) care for their mental illness.
Objective
To investigate the relationship between insight and internalized stigma in patients with schizophrenia in mainland China.
Methods
65 inpatients and 27 outpatients with schizophrenia who had a median duration of four years of illness completed Chinese versions of two self-report questionnaires—the Internalized Stigma of Mental Illness (ISMI) scale and the Modified Consumer Experiences of Stigma Questionnaire (MCESQ). The patients were also assessed by senior psychiatrists using the Scale for Assessment of Positive Symptoms (SAPS) and the Scale for Assessment of Negative Symptoms (SANS). Patients were divided into those with and without insight into their illness based on the score of the insight item on the Chinese version of the Brief Psychiatric Rating Scale.
Results
49 patients were classified as having insight and 43 classified as lacking insight. Compared to patients with insight, those without insight had a significantly shorter duration of illness, were more likely to be inpatients, and (at trend level only) had more prominent positive and negative symptoms. The ‘alienation’ subscale score of the ISMI was significantly higher in patients with insight but none of the remaining six subscales in the two instruments were different between the two groups and only 4 of the 48 separate items in the two scales were significantly different between the groups. Logistic regression analysis found no relationship between lack of insight and the scores of the two self-completion stigma scales or the scores of the two clinician-administered symptom scales.
Conclusion
This study among inpatients and outpatients with schizophrenia in China does not support findings of previous studies that report increased experience of stigma among patients who have better insight. The measures of stigma used in the study need further revision and validation for use in China and studies with a wider spectrum of patients that make more detailed assessments of insight and that follow fluctuations in insight and experiences of stigma over time are needed to clarify the complex relationship between these two phenomena in patients with schizophrenia.
Abstract
背景
精神分裂症患者自知力和内在耻感的关系具有理论和实践上的重要性,因为这和患者寻找或接受治疗的意愿密切相关。
目的
研究中国大陆精神分裂症患者自知力和内在耻感的关系。
方法
共有65例住院治疗的精神分裂症患者和27例门诊治疗的精神分裂症患者(病程的中位数为4年)完成了两个中文版自评量表-精神疾病内在耻感量表(Internalized Stigma of Mental Illness,ISMI)和修订版病耻感经历问卷 (Modified Consumer Experiences of Stigma Questionnaire,MCESQ)的测评。由高年资精神科医生采用阳性症状量表(Scale for Assessment of Positive Symptoms,SAPS)和阴性症状量表(Scale for Assessment of Negative Symptoms,SANS)评定了患者的精神病理症状。由两位高年资精神科医生采用简明精神病学量表中文版的自知力条目评定患者对自身精神疾病的认知,依据分数将患者分为有自知力组和无自知力组。
结果
有自知力组有49例患者,无自知力组为43例。无自知力患者的病程显著短于有自知力组,更可能为住院治疗者,并且具有更明显的阴性和阳性症状(仅仅表现在趋势上)。有自知力组患者在精神疾病内在耻感量表疏离分量表得分上显著高于无自知力组的患者,但是两个量表的其他分量表得分组间无统计学差异。两个量表48个条目中仅有4个条目得分存在组间差异。Logistic回归没有发现无自知力和两个耻感量表分数或症状量表得分之间存在相关性。
结论
中国大陆精神分裂症门诊与住院患者中进行的本研究不支持以前的研究发现:即有自知力的精神分裂症患者会报告更多的耻感经历。本研究使用的耻感量表在中国地区的应用还需要进一步的修订和证实;未来需要对下列问题进行研究:选择不同诊断的患者、对自知力进行更精细的评估以及随时间推移自知力及病耻感经历的波动等等,进一步澄清精神分裂症患者中这两个现象间的复杂关系。
1. Introduction
The concept of stigma, initially proposed by Goffman in 1963, refers to an attribute that is deeply discrediting.[1] Stigma initially meant a brand, the mark that identifies persons with immoral character. Since the 1990s, stigma related to mental disorders has been extensively studied in Western countries. The stigmatization of mental illness is common among the general population, psychiatric patients, and their families. These negative attitudes are primarily based on the belief that psychiatric patients are prone to impulsive acts of violence and are incompetent because of their decreased capabilities.[2],[3] Such negative attitudes label psychiatric patients and isolate them from society. Because of the existence of stigma, patients often decrease their expectations about their potential achievements and regard themselves as losers.[4] Stigma delays care-seeking for psychological problems and increases the difficulties patients with mental illnesses face when trying to re-integrate into society after an acute episode of illness.
Most studies on stigma among psychiatric patients have been conducted in Western countries. The results have often been used by governments and civil society organizations in carrying out activities or interventions to reduce stigma. In China, more than half of the subjects included in the limited number of studies about stigma in the mentally ill report various forms of discrimination.[5],[6] Some authors have described possible reasons for mental disorder-related stigma and possible countermeasures.[7],[8] However, few Chinese researchers have separately studied stigma among schizophrenic patients using standardized stigma evaluation tools.
Insight in mental illness refers to a patient's understanding and judgment of his disorder. It is an important marker of recovery from some mental disorders, including schizophrenia. Some authors believe patients with insight tend to have higher self-stigma,[9] while other authors do not support this conclusion.[10] In this study we administer standardized stigma evaluation tools to patients with schizophrenia to explore the association between insight and internalized stigma.
2. Methods
2.1. Subjects
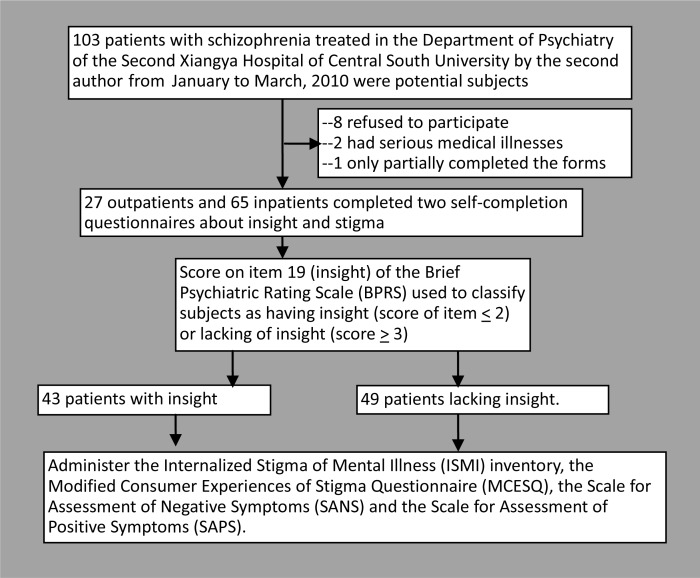
The enrollment of subjects in the study is shown in Figure 1. Outpatients and inpatients 17-60 years of age with a DSM-IV diagnosis of schizophrenia who were in an active course of treatment (i.e., not in the residual phase of illness) at the Department of Psychiatry at the Second Xiangya Hospital from January 2010 to March 2010 were potential subjects for the study. Patients with co-morbid mental or physical disorders or who were unable to understand the self-completion questionnaires employed in the study were excluded. Of 103 identified subjects, 8 refused to participate, 2 had co-morbid serious physical illnesses, and 1 only completed part of the self-completion instruments; most patients who refused did so because of concerns regarding confidentiality of the information obtained. Thus 92 subjects (30 outpatients and 62 inpatients) were included in the analysis. There were no significant differences in the age, gender, duration or illness or status (inpatient v. outpatient) between those who did and did not complete the questionnaires.
Figure 1. Enrollment and follow-up of subjects.
All subjects and their guardians provided written consent to participate in the study. The study was approved by the ethics review committee of the Second Xiangya Hospital of Central South University.
2.2. Instruments
2.2.1. Demographic data
A questionnaire designed by the authors was used to collect basic demographic data and information about the course of illness: age of the first onset, frequency of hospitalizations, family history, and current status of the disease.
2.2.2. Evaluation of insight
Insight was evaluated using item 19 of the Chinese version of the Brief Psychiatric Rating Scale (BPRS)[11] which reads ‘Disorder of insight involving failure to recognize one's own mental illness, psychological symptoms or abnormal words and deeds’. Patients who scored ‘0’ (not present) or ‘1’ (very mild) on the item were classified as having insight into their illness while those scoring ‘2’ (‘mild’) or higher on the item were classified as lacking insight. The reported inter-rater reliability of item 19 is excellent (ICC=0.913).[11]
2.2.3. Assessment of stigma
Two self-completion instruments for assessing stigma were translated by the second author. The reliability and validity of the Chinese versions of these instruments have not yet been fully assessed.
The Internalized Stigma of Mental Illness (ISMI) inventory, developed by Ritsher and colleagues in 2003[12] contains 29 items scored on a 4-point Likert scales (1=‘strongly disagree’ to 4=‘strongly agree’) that are assorted into five subscales: alienation (six items reflecting the respondent's feeling of participation in the society; alpha in current study=0.70), stereotype endorsement (seven items reflecting the respondent's tendency to endorse stereotyped impressions of psychiatric patients, alpha=0.67), discrimination experience (five items reflecting the respondent's experiences of unfair treatment due to other people's discrimination, alpha=0.63), social withdrawal (six items reflecting the respondent's experience of frequent refusal by others due to his mental disorder, alpha=0.73), and stigma resistance (five items reflecting respondent's perceived ability to deflect stigma, alpha=0.01). Based on previous studies, four subscales (excluding stigma resistance) are used to calculate the adjusted total score of stigma; in the current study this adjusted total score had good internal consistency (alpha=0.85).
The Modified Consumer Experiences of Stigma Questionnaire (MCESQ), compiled by Wahl and colleagues[13]–[14] is mainly used to assess respondents' expected sense of mental disorder-related stigma as well as their actual experience of stigma and discrimination. It contains 19 items scored on five point Likert scales (1=never to 5=always) and is divided into two subscales: the Stigma Experiences Scale (with nine items, alpha in current study=0.70) and the Discrimination Experiences Scale (with ten items, alpha in current study=0.50). In the current study the internal consistency of the total 19-item scale is poor (ICC=0.67).
2.2.4. Assessment of psychotic symptoms
Chinese versions of the Scale for the Assessment of Negative Symptoms (SANS) and the Scale for the Assessment of Positive Symptoms (SAPS), developed by Andreasen in 1982,[11] were used for the assessment of negative symptoms and positive symptoms in the participants. The SANS contains 24 items and the SAPS contains 34 items scored on six-point Likert scales (0=not present to 5=severe). The SANS is divided into five subscales: affective blunting; alogia (impoverished thinking); avolition/apathy; anhedonia/asociality; and disturbance of attention. The SAPS is divided into four subscales: hallucinations, delusions, bizarre behavior, and positive formal thought disorder. A high score is interpreted as having prominent negative or positive symptoms. The Chinese versions of the scales have good reliability and validity.[11]
2.3. Research process
SANS, SAPS, BPRS, and insight were assessed simultaneously. The assessments were conducted by two trained doctoral candidates who had good test-retest reliability (ICC=0.80-0.95 for SAPS items and 0.80-0.88 for SANS items). The two self-rated scales about stigma were completed by patients immediately after the clinician-conducted evaluations (in the presence of the researcher). After the researchers read the instructions, subjects completed the forms on their own but were free to ask questions if they did not understand specific items. Researchers read the entire questionnaire to six subjects who were unable to understand the instrument because they were semiliterate. On average it took patients 30-40 minutes to complete the two self-completion instruments.
2.4. Statistical methods
All the data were processed using SPSS 17.0 software. Statistical analyses included descriptive statistics, t-tests, chi-square tests, and Mann-Whitney U tests.
3. Results
3.1. Characteristics of the sample
A total of 92 patients completed valid forms. There were 43 patients with a score of two or more on the BPRS insight item and, thus, classified as ‘lacking insight’; the remaining 49 subjects were classified as having insight into their illness. The demographic characteristics of the two groups are shown in Table 1. Compared to patients with insight, those lacking insight had a significantly shorter duration of illness, were more likely to be inpatients, and (at trend level only) had more prominent positive and negative symptoms.
Table 1. Comparison of demographic and clinical data characteristics of patients with schizophrenia with and without insight into their illness.
| Characteristic | Total (n=92) |
With insight (n=49) |
Lacking insight (n=43) |
statistic | p-value | |||
| Male (n, %) | 54 | (58.7) | 30 | (61.2) | 24 | (55.8) | χ2=0.28 | 0.599 |
| Age (n, mean, sd) | 92 | 26.1 (7.5) | 49 | 26.6 (7.2) | 43 | 25.4 (7.9) | t=-0.76 | 0.450 |
| Currently employed (n, %) | 58 | (63.0) | 31 | (63.3) | 27 | (62.8) | χ2<0.01 | 0.962 |
| Marital status (n, %) | χ2=3.41 | 0.224 | ||||||
| unmarried | 62 | (67.4) | 37 | (75.5) | 25 | (58.1) | ||
| married | 26 | (28.3) | 10 | (20.4) | 16 | (37.2) | ||
| divorced | 4 | (4.3) | 2 | (4.1) | 2 | (4.7) | ||
| Under 9 years of schooling (n, %) | 31 | (33.7) | 16 | (32.7) | 15 | (34.9) | χ2=0.05 | 0.821 |
| Age of onset (n, mean, sd) | 92 | 21.6 (6.3) | 49 | 21.5 (6.3) | 43 | 21.7 (6.3) | t=0.16 | 0.874 |
| Years of illness (n, median, IQR) | 92 | 4.0 (1.5–6.0) | 49 | 5.0 (3.3–6.0) | 43 | 3.0 (1.0–5.0) | U=-2.67a | 0.008 |
| Family history (n, %) | Fisher | |||||||
| yes | 16 | (17.4) | 7 | (14.3) | 9 | (20.9) | exact test | 0.709 |
| no | 74 | (80.4) | 41 | (83.7) | 33 | (76.7) | ||
| unknown | 2 | (2.2) | 1 | (2.0) | 1 | (2.4) | ||
| Current inpatient (n, %) | 65 | (70.7) | 28 | (57.1) | 37 | (86.0) | χ2=3.02 | 0.003 |
| Hospitalizations (n, %) | Fisher | |||||||
| 0 times | 7 | (7.6) | 5 | (10.2) | 2 | (4.7) | exact test | 0.664 |
| <3 times | 61 | (66.3) | 32 | (65.3) | 29 | (67.4) | ||
| >3 times | 24 | (26.1) | 12 | (24.5) | 12 | (27.9) | ||
| Total SAPS score (n, mean, sd) | 89 | 25.4 (15.3) | 46 | 22.5(14.8) | 43 | 28.6 (15.3) | t=1.92 | 0.058 |
| Total SANS score (n, mean, sd) | 89 | 41.0 (19.7) | 46 | 37.1 (21.2) | 43 | 45.1 (17.2) | t=1.96 | 0.053 |
IQR=inter-quartile range; SAPS=Scale for Assessment of Positive Symptoms; SANS=Scale for Assessment of Negative Symptoms
a Mann-Whitney U test
3.2. Comparison of stigma in those with and without insight
Comparison of the mean total scores and mean subscale scores of the two self-completion assessments of stigma (Table 2) between patients with and without insight found that only the alienation subscale score of the ISMI was significantly different; patients with insight reported a greater feeling of alienation than those without insight. There was also a trend finding (p=0.068) of higher internalized stigma on the MCSQ in patients with insight. None of the other subscale scores of the ISMI or MCESQ were significantly different between patients with and without insight; but the power of these assessments was under 80% for all except one of the comparisons.
Table 2. Mean (sd) total scores and subscale scores on the Internalized Stigma of Mental Illness (ISMI) inventory and the Modified Consumer Experiences of Stigma Questionnaire (MCESQ) for patients with schizophrenia who do and do not have insight into their illne.
| Scale/subscale | Total |
With insight |
Lacking insight |
t-value | p-value | Power | |||
| n | mean (sd) | n | mean (sd) | n | mean (sd) | ||||
| ISMI inventory | |||||||||
| Alienation | 92 | 2.29 (0.50) | 49 | 2.42 (0.45) | 43 | 2.16 (0.52) | 6.62 | 0.012 | -- |
| Stereotype endorsement | 91 | 2.09 (0.41) | 49 | 2.12 (0.42) | 42 | 2.06 (0.40) | 0.57 | 0.453 | 55.2% |
| Discrimination experience | 91 | 2.17 (0.44) | 49 | 2.22 (0.42) | 42 | 2.10 (0.47) | 1.66 | 0.202 | 51.1% |
| Social withdrawal | 89 | 2.20 (0.45) | 48 | 2.26 (0.42) | 41 | 2.1 4(0.48) | 1.55 | 0.217 | 51.2% |
| Stigma resistance | 92 | 2.43 (0.34) | 49 | 2.40 (0.28) | 43 | 2.47 (0.39) | 0.86 | 0.356 | 55.2% |
| Total scorea | 88 | 2.18 (0.38) | 48 | 2.25 (0.35) | 40 | 2.10 (0.40) | 3.42 | 0.068 | 63.9% |
| MCESQ | |||||||||
| Experiences of stigma | 91 | 2.54 (0.60) | 48 | 2.58 (0.57) | 43 | 2.48 (0.64) | 0.62 | 0.433 | 55.6% |
| Experiences of discrimination | 90 | 1.70 (0.40) | 47 | 1.70 (0.45) | 43 | 1.70 (0.35) | <0.01 | 0.960 | 96.0% |
| Total score | 89 | 2.08 (0.39) | 46 | 2.10 (0.39) | 43 | 2.07 (0.39) | 0.10 | 0.751 | 76.6% |
a Total score for the ISMI inventory excludes the stigma resistance items.
Item-level comparisons of the two groups also found few differences. Only 1 of the 19 items on the MCESQ showed a significant difference: patients without insight were more likely to report being refused a driver's license or other document because of prior psychiatric treatment (mean [sd] items score, 1.56 [0.85] v. 1.15 [0.46], t=2.82, p=0.006). And only 4 of the 29 items on the ISMI were significantly different: patients with insight were more likely to report feeling inferior to others (2.14 [0.68] v. 1.79 [0.74], t=2.38, p=0.019), more likely to report feeling hopeless because of having a mental illness in the family (2.37 [0.70] v. 2.05 [0.72], t=2.16, p=0.033), more likely to report needing to have others make their decisions for them (2.41 [0.71] v. 2.09 [0.68], t=2.17, p=0.033), and more likely to report restricting their social activities for fear that they be perceived as being strange (2.42 [0.74] v. 2.12 [0.70], t=1.99, p=0.050).
The ranked correlation of the score of BPRS item 19 (on stigma) with the total score of the ISMI was 0.21 (p=0.053) and the correlation of the item with the total MCESQ score was 0.003 (p=0.977).
3.3. Comparison of stigma in those with and without insight
Table 3 shows the results of a logistic regression analysis using lack of insight as the dependent variable and demographic and clinical variables as independent variables. Only the inpatient versus outpatient status of the patient remained statistically significant when all variables were considered in the logistic model: as expected, inpatients were less likely to have insight into their illness than outpatients. The scores on the self-completion scales (MCESQ and ISMI) and on the clinician-administered clinical scales (SAPS and SANS) were not significantly associated with lack of insight as defined by item 19 of the BPRS. Stepwise logistic regression analysis (not shown) had the same result.
Table 3. Logistic regression of factors associated with having insight into the illness among 92 patients with schizophrenia.
| Factor | Odds ratio | 95% CI of odds ratio | |
| Female | 1.39 | 0.46 | 4.22 |
| Age | 0.97 | 0.90 | 1.05 |
| Years of schooling | 0.97 | 0.54 | 1.75 |
| Years duration of illness | 1.10 | 0.92 | 1.31 |
| Inpatient (v. outpatient) | 0.24 | 0.06 | 0.97 |
| Number of hospitalizations | 1.17 | 0.39 | 3.48 |
| Total ISMI score | 2.11 | 0.45 | 9.98 |
| Total MCESQ score | 1.62 | 0.36 | 7.19 |
| Total SAPS score | 0.97 | 0.93 | 1.01 |
| Total SANS score | 0.99 | 0.97 | 1.02 |
CI, Confidence Interval; ISMI, Internalized Stigma of Mental Illness inventory; MCESQ, Modified Consumer Experiences of Stigma Questionnaire; SAPS, Scale for Assessment of Positive Symptoms; SANS, the Scale for Assessment of Negative Symptoms
4. Discussion
4.1. Main findings
This study among inpatients and outpatients with schizophrenia in China only provided weak support for previous studies that report increased experience of stigma among patients who have better insight.[8] Among the eight subscales of the two self-report instruments used to assess stigma only one (alienation) was significantly more prominent in patients with insight into their illness than in those without insight. And among the 48 individual items in the two scales about stigma considered only five were statistically significant between patients with and without insight into their illness—this is little more than would be expected by chance given the number of items that were being compared. Further studies with a wider spectrum of patients that make more detailed assessments of stigma and insight and that follow fluctuations in insight and experiences of stigma over time are needed to clarify the complex relationship between these two phenomena in patients with schizophrenia.
4.2. Limitations
There are several limitations in this preliminary project. (a) A more detailed evaluation of the reliability and validity of the Chinese versions of the two instruments used to assess stigma in this study (ISMI and MCESQ) is needed and the scales may need to be adapted for use in mainland China. (b) The classification of insight used in this study was based on the score of a single BPRS item so it may not have captured all important aspects of the construct. (c) Insight can change rapidly as a patient's condition improves or gets worse, whereas stigma is typically experienced over longer periods of time, so longitudinal studies that monitor levels of insight and stigma over time are needed to get a more sensitive evaluation of the relationship of these phenomena. (d) The power of the comparison of subscale scores between patients with and without insight was quite low so the negative findings may have been due to Type II errors; larger samples will be needed confirm or disprove the significance of the findings. (e) The relatively small sample size also made it impossible to compare the relationship of stigma and insight in important subgroups such as inpatients versus outpatients, first-onset versus chronic patients, males versus females, and so forth. (f) The median duration of illness in the patients included in the study was four years; the relationship between insight and stigma may be different in patients with shorter durations of illness.
4.3. Significance
One of the currently most influential theories of stigma in mental illness is a modified labeling theory proposed by Link and colleagues.[16] According to this theory members of a society internalize stereotyped beliefs about mentally ill individuals (e.g., a burden on society, potentially dangerous, etc.) which are then used to ‘label’ psychiatric patients when they make contact with the health care system. Patients then have to use cognitive and behavioral strategies to deal with these external labels. These strategies include keeping their psychiatric treatment secret, refusing to come into contact with the medical system, and intentional restriction of their social worlds (which may magnify their disability).
Compared with Western countries, the dominant ideology in China for the last 2000 years has been Confucianism which promotes loyal and supportive relationships among family members and a relatively rigid social and interpersonal support network. In this sociocultural setting ‘face’, the status ascribed to a person by those in his or her social network, is an integral component of an individual's social identity. ‘Never lose face’ is a paramount social objective because loss of face inevitably isolates one from the social network. Because of the public's negative stereotypes about mental disorders,[17],[18] once a individual is identified as a psychiatric patient the negative information conveyed by such a label will make the patient lose face and, thus, suffer a serious blow to his or her social status and a corresponding decrease in self-esteem.[19]
Previous research from other countries suggests that as a patient with schizophrenia regains insight during the course of treatment there is an increased awareness of the negative social stereotypes associated with their illness and, thus, increased internalized stigma.[4] In the Chinese context this potentially serious loss of face often causes patients and their family members to go to great lengths to keep information about the illness secret (45% of the patients in the current study had done so). It is important that clinicians are aware of this tendency and actively take steps to reduce internalized stigma both in patients and in their family members because this can directly affect adherence to treatment regimens and social re-integration. More research is urgently needed to determine how best to achieve this goal.
Footnotes
Conflict of interest: The authors report no conflict of interest related to this study.
Funding: The study was supported by the Shanghai Key Laboratory of Forensic Medicine (grant number: KF0908).
References
- 1.Goffman E. Stigma: notes on the management of spoiled identity. New York: Prentice Hall; 1963. p. 3. [Google Scholar]
- 2.Link BG, Phelan M, Bresnhahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness and social distance. Am J Public Health. 1999;89(9):1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? Journal of Health and Social B. 2000;41(2):188–207. [Google Scholar]
- 4.Ritsher JB, Phelan JC. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. 2004;129(3):257–265. doi: 10.1016/j.psychres.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Phillips MR, Pearson V, Li FF, Xu MJ, Yang L. Stigma and expressed emotion: a study of people with schizophrenia and their family members in China. Br J Psychiatry. 2002;181:488–493. doi: 10.1192/bjp.181.6.488. [DOI] [PubMed] [Google Scholar]
- 6.Gao SY, Fei LP, Wang XQ, Xu D, Jia ZM, Gao WC. Experience of stigma among patients with schizophrenia and their family members and attitudes of different groups about this stigma. Chinese Mental Health Journal. 2005;19(2):82–85. (in Chinese) [Google Scholar]
- 7.Guo QF, Lu SC, Zhang YH. Experience of discrimination and coping styles of schizophrenia patients in the convalescent period. Chinese Journal of Nursing. 2010;45(8):677–680. (in Chinese) [Google Scholar]
- 8.Liu WQ, Tan LW, Wan F, Wang LF. Social discrimination on patients with mental disorders: Status quo, reasons, and countermeasures. Medicine and Philosophy (Clinical Decisionmaking) 2008;29(1):69–71. (in Chinese) [Google Scholar]
- 9.Mak WWS, Wu CFM. Cognitive insight and causal attribution in the development of self-stigma among individuals with schizophrenia. Psychiatric Serv. 2006;57(12):1800–1802. doi: 10.1176/ps.2006.57.12.1800. [DOI] [PubMed] [Google Scholar]
- 10.Lysaker PH, Roe D, Yanos PT. Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophr Bull. 2007;33(1):192–199. doi: 10.1093/schbul/sbl016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang MY. Handbook of Evaluation Scales in Psychiatry. Changsha: Hunan Science and Technology Press; 2003. pp. 81–94.pp. 94–111. (in Chinese) [Google Scholar]
- 12.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121(1):31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 13.Wahl OF. Mental health consumers' experience of stigma. Schizophr Bull. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- 14.Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Experiences of stigma among outpatients with schizophrenia. Schizophr Bull. 2002;28(1):143–155. doi: 10.1093/oxfordjournals.schbul.a006917. [DOI] [PubMed] [Google Scholar]
- 15.Phillips MR, Xiong W, Wang RW, Gao YH, Wang XQ, Zhang NP. Reliability and validity of the Chinese versions of the scales for assessment of positive and negative symptoms. Acta Psychiatr Scand. 1991;84(4):364–370. doi: 10.1111/j.1600-0447.1991.tb03161.x. [DOI] [PubMed] [Google Scholar]
- 16.Link BG, Cullen FT, Struening E, Shrout PE, Dohrenwend BP. A modified labeling theory approach to mental disorders: an empirical assessment. Am Sociol Rev. 1989;54(3):400–423. [Google Scholar]
- 17.Gao SY, Fei LP. Attitudes about mental illness of different types of respondents in Beijing. Chinese Mental Health Journal. 2001;15(2):107–109. (in Chinese) [Google Scholar]
- 18.Tsang HWH, Tam PKC, Chan F, Cheung WM. Stigmatizing attitudes towards individuals with mental illness in Hong Kong: implications for their recovery. J Community Psychol. 2003;31(4):383–396. [Google Scholar]
- 19.Livingston JD, Rossiter KR, Verdun-Jones SN. ‘Forensic’labelling: an empirical assessment of its effects on self-stigma for people with severe mental illness. Psychiatry Res. 2011;188(1):115–122. doi: 10.1016/j.psychres.2011.01.018. [DOI] [PubMed] [Google Scholar]