Abstract
Background:
Type 2 diabetes comes with various complications and this may be compounded by morbidities of hepatitis B virus (HBV) and hepatitis C virus (HCV) infections.
Aims:
This study examined the prevalence of HBV and HCV infectionst among type 2 diabetics as well as its associated factors. This randomized cross-sectional study was conducted at the Diabetic Clinic of the Central Regional Hospital, Cape Coast between December 2012 and April 2013.
Subjects and Methods:
A well-structured questionnaire was used to recruit 110 type 2 diabetics. Venous blood samples were collected for the estimation of blood glucose and to screen for HBV and HCV infections. Data analysis was carried out using SPSS Version 17.0. Descriptive analysis was performed and results expressed as means (SD) and n (%). P < 0.05 was considered significant.
Results:
Prevalence of HBV in type 2 diabetics was 5.5% (6/110). No type 2 diabetic was positive for HCV. The prevalence of HBV infection in the type 2 diabetes mellitus (T2DM) participants was higher (5.5% [6/110]) than that of HCV (0/110). A total of 69.1% (76/110) T2DM patients had poor glycemic control. Mean waist and hip circumference was higher among HBV-negative T2DM participants (99.3; 106.9) than HBV-positive participants (87.2; 101.8).
Conclusions:
The seroprevalence of HBV was higher than that of HCV in T2DM patients. T2DM patients would require necessary preventive measures like prophylaxis, to reduce the risk of HBV infection and its ramifications.
Keywords: Diabetes mellitus, Ghana, Hepatitis B, Hepatitis C, Prevalence
Introduction
Hepatitis B virus and hepatitis C virus (HBV and HCV) infections are common diseases of the world, infecting an estimated 2 billion and 3.9 million people including an estimated 400 million chronic cases.[1] These infections have a high rate of development of liver cirrhosis and can cause serious mortality, raising a major concern for global health.[1]
Over the years, prevalence of diabetes mellitus (DM) has been increasing worldwide, with an estimated rate of 2.8% recorded in 2000 and projected to be around 4.4% in 2030.[2]
Allison et al., in 1994, suggested that HCV may be associated with type 2 DM (T2DM).[3] The complex interaction of chronic HBV and HCV infections with the host hepatic glucose and lipid metabolism, however, has not been fully understood and remains to be determined.[4]
Various studies have reported on the prevalence of HBV and HCV in T2DM patients. In a study conducted at Multan, the seroprevalence of HCV was higher in T2DM patients than in healthy controls.[5] However, a study in Nigeria by Balogun et al., recorded no prevalence of HCV in T2DM.[6] Chen et al., (2006), found that the prevalence of hepatitis B was similar to that of the control group.[7] Furthermore, Onyekwere et al., in 2002 found that diabetics in Lagos were not more predisposed to chronic HBV infection than the rest of the population, and therefore would require no special anti-HBV prophylaxis.[8]
So far, there is a paucity of data on the prevalence of HBV and HCV infections among diabetics in Ghana. To enable better management of T2DM patients, especially to prevent such added on infections and its morbid consequences, it is prudent to study the seroprevalence of HBV and HCV infection in T2DM as well as its associated factors.
Subjects and Methods
Study area and subjects
This simple randomized cross-sectional study was conducted from December 2012 to April 2013, at the Diabetic Clinic of the Central Regional Hospital, Cape Coast, Central Region, Ghana. A total of 110 participants with diagnosed, confirmed type 2 diabetes were recruited. A structured, pretested questionnaire was administered to collect demographic and clinical information of patients. Type 1 diabetics, organ transplant recipients and dialysis patients were excluded from the study.
Ethical consent
This study was approved by authorities of the Central Regional Hospital, Cape-Coast and the Institutional Review Board of the University of Cape-Coast. Informed consent was sought from the participants before recruitment onto the study.
Blood pressure measurement
Blood pressure was measured by trained personnel (nurse), with a mercury sphygmomanometer and a stethoscope (Accoson dekamet, England). Measurements were taken only after participants had rested for at least 15 min.
Anthropometric measurements
The height (to the nearest 0.1 cm) without footwear, with a stadiometer (Lindels, Klippan, Sweden) and weight (to the nearest 0.1 kg) in light clothing, with a weighing balance (Seca, Hamburg, Deutschland) were measured. The body mass index (BMI) was then calculated as the ratio of the weight (kg) and the square of the height (m2).
The hip circumference at the widest portion of the buttocks and waist circumference midway between the inferior margin of the last palpable rib and the suprailiac crest (both to the nearest 0.1 cm) were also measured using a measuring tape. The waist-to-hip ratio was calculated from the waist circumference/hip circumference.
Blood sample collection
About 3 ml venous blood was drawn from each study participant after an overnight fast (12-14 h). 2 ml was dispensed into a serum separator tube and centrifuged at 1500 rpm for 5-10 min. The serum was dispensed into cryovials and aliquots stored at -80°C until assayed. The remaining 1 ml was dispensed into fluoride oxalate anticoagulated tubes for estimation of blood glucose.
Serological tests
The serum was analyzed for the detection of hepatitis B surface antigen (HBsAg) using a One-step HBsAg Test Strip (Runbio Biotech Co. Limited, Guangdong, China), and anti-HCV antibodies using advanced quality rapid anti-HCV test strip (InTec Products, Inc., Xiamen, China).
Biochemical tests
Glucose estimation
Glucose from blood in the fluoride oxalate tube was estimated using the glucose oxidase/peroxidase method (Barham and Trinder, 1972), as per manufacturer's instructions. All reagents were from Fortress diagnostics (Fortress diagnostics, Antrim, United Kingdom).
Statistical analysis
Data analysis was carried out using the Statistical Package for Social Scientists (SPSS) Version 17.0 (Chicago IL, USA). Descriptive analysis with frequency distribution tables was performed and the results expressed as means (SD) and n (%). The t-test, Chi-square and Fischer's test were used for comparisons as appropriate. P < 0.05 was considered significant.
Results
Of the total population, 5.5% (6/110) of the type 2 diabetics were positive for HBV. None of the type 2 diabetics was positive for HCV. The prevalence of HBV infection in the T2DM participants was higher (5.5% [6/110]) than that of HCV (0/110).
Tables 1 and 2 describe the demographic and clinical characteristics of T2DM participants in relation to gender. Of the total number of females, 43.5% (40/92) were in their fifth decade of life and 53.3% (49/92) had had secondary education. Present family history of diabetes (55.4% [51/92]), obesity (51.1% [47/92]), high blood pressure (92.4% [85/92]), and high waist-hip ratio (85.9% [79/92]) were more prevalent in female T2DM participants. There was a significant difference in level of education, occupation, duration of diabetes, BMI, and blood pressure (P = 0.02; P < 0.01; P < 0.001; P = 0.03; P = 0.03 respectively) when compared between males and females. A total of 69.1% T2DM patients (76/110) had poor glycemic control, of which 66.7% (12/18) were males and 69.6% (64/92) were females.
Table 1.
Demographic characteristics of study participants

Table 2.
Clinical characteristics of study participants
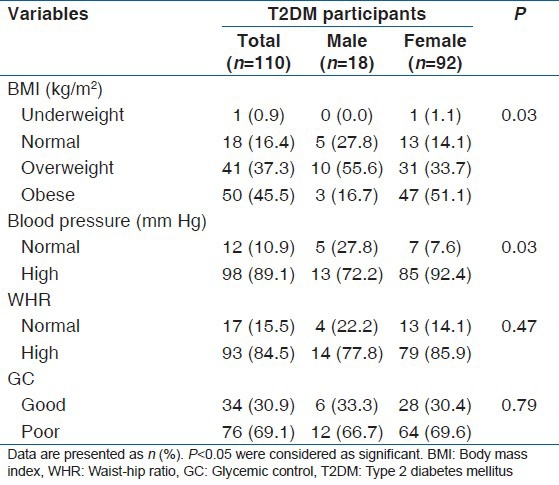
Table 3 shows the demographic, clinical, and biochemical characteristics of participants, relative to hepatitis B status. The mean waist and hip circumference was higher among the HBV-negative T2DM participants (99.3 and 106.9 respectively) compared to the HBV-positive participants (87.2 and 101.8 respectively).
Table 3.
Demographic, clinical, and biochemical characteristics of participants relative to Hepatitis B status

Discussion
The current study determined the seroprevalence of HBV and HCV infections among T2DM patients. It also determined possibility of associated factors with these infections. The prevalence of HBV infection was low, but higher than that HCV in type 2 diabetics.
This lower seroprevalence of HBV is contrary to other studies conducted in various countries,[7,8,9,10] all of which reported a higher seroprevalence rate of HBV in diabetic patients than in nondiabetics. The contrastingly low prevalence of hepatitis B in this study might be due to differences in geographical location or failure to identify infected patients because of the serologic window during the incubation period following infection. It could also be due to the presence of some rare variants escaping the serologic assay for HBsAg,[11] and the problem of occult HBV infections,[11,12] in which neither HBsAg nor anti-HBc are detected. Therefore, since we performed a serologic assay, the possibility of false negatives cannot be ruled out. Furthermore, patient antibody may also have been bound with viral antigen in immune complexes, thereby preventing antibody detection.[13] In endemic areas such as Africa and Asia, most infections are known to occur in infants and children as a result of maternal-neonatal transmission or close childhood contact.[14] This study however was conducted on adults and this group is thought to have comparatively lower prevalence rates.
Yet another theory could be the uptake of preventive measures by participants, especially through vaccination. The current study however is limited by the nondetermination of HBV antibody titer levels, thus this cannot be ascertained.
The seroprevalence of hepatitis C in the T2DM patients is in consonance with a study conducted in Nigeria,[6] which recorded no prevalence of HCV infection among T2DM individuals, in a descriptive case-control study.
The seroprevalence of HBV infection was higher than HCV infection in T2DM, just as found in a study conducted in Nigeria, where no HCV infection was found among diabetics.[6] This contrasts the findings in other studies, which found a higher seroprevalence of HCV than HBV in the T2DM patients.[7] This might be due to the higher endemicity of the HBV in Ghana.[15]
Hepatitis B-negative participants had a higher waist circumference with a significant difference in waist-hip ratio. Interestingly, other studies have proved otherwise.[16,17] Others have argued that high waist circumference and waist-hip ratio (a measure of visceral obesity) can lead to the development of type 2 diabetes,[18] and hence frequent use of intramuscular injections, a risk factor for HBV infection. Another theory to support this association is the complex interaction of chronic HBV and HCV infections with the host hepatic glucose and lipid metabolism. However, this has not been fully understood and remains to be determined.[4]
In contrast, the current study found otherwise and this could be that in this era of disposable sharps used in these procedures, risk of contracting HBV infection is relatively low and thus individuals may have contracted these infections from other sources, rather than through diabetes management procedures.
Similar schools of thought have reported that glycemic control may be associated with the development of HCV infection.[5,7] However, the findings in this study reported no prevalence of HCV infection among the T2DM participants, thus this association couldn’t be ascertained.
This study has some limitations. Our inability to confirm the results of screening by polymerase chain reaction to detect HBV and HCV might have led to many false-negatives. The cross-sectional design of our study precluded drawing a pathophysiological causal inference between T2DM and the risks of HBV and HCV. Furthermore, fasting blood glucose, which gives a crude estimate of glycemic control, was used instead of glycated hemoglobin.
Conclusion
The seroprevalence of HBV was higher than that of HCV in T2DM patients. T2DM patients would require necessary preventive measures like prophylaxis, to reduce the risk of HBV infection and its ramifications.
Acknowledgment
Gratitude goes to the patients and staff of the diabetic clinic of the Central Regional Hospital, Cape Coast, Ghana.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Nkrumah B, Owusu M, Frempong HO, Averu P. Hepatitis B and C viral infections among blood donors from rural Ghana. Ghana Med J. 2011;45:97–100. [PMC free article] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Allison ME, Wreghitt T, Palmer CR, Alexander GJ. Evidence for a link between hepatitis C virus infection and diabetes mellitus in a cirrhotic population. J Hepatol. 1994;21:1135–9. doi: 10.1016/s0168-8278(05)80631-2. [DOI] [PubMed] [Google Scholar]
- 4.Naing C, Mak JW, Ahmed SI, Maung M. Relationship between hepatitis C virus infection and type 2 diabetes mellitus: Meta-analysis. World J Gastroenterol. 2012;18:1642–51. doi: 10.3748/wjg.v18.i14.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jadoon NA, Shahzad MA, Yaqoob R, Hussain M, Ali N. Seroprevalence of hepatitis C in type 2 diabetes: Evidence for a positive association. Virol J. 2010;7:304. doi: 10.1186/1743-422X-7-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balogun WO, Adeleye JO, Akinlade KS, Kuti M, Otegbayo JA. Low prevalence of hepatitis-C viral seropositivity among patients with type-2 diabetes mellitus in a tertiary hospital. J Natl Med Assoc. 2006;98:1805–8. [PMC free article] [PubMed] [Google Scholar]
- 7.Chen HF, Li CY, Chen P, See TT, Lee HY. Seroprevalence of hepatitis B and C in type 2 diabetic patients. J Chin Med Assoc. 2006;69:146–52. doi: 10.1016/S1726-4901(09)70195-9. [DOI] [PubMed] [Google Scholar]
- 8.Onyekwere CA, Anomneze EE, Wali SS. Prevalence of serological markers of chronic hepatitis B virus infection in diabetics in the Lagos University Teaching Hospital, Lagos. Niger Postgrad Med J. 2002;9:129–33. [PubMed] [Google Scholar]
- 9.Gulcan A, Gulcan E, Toker A, Bulut I, Akcan Y. Evaluation of risk factors and seroprevalence of hepatitis B and C in diabetic patients in Kutahya, Turkey. J Investig Med. 2008;56:858–63. doi: 10.2310/JIM.0b013e3181788d28. [DOI] [PubMed] [Google Scholar]
- 10.Kew MC. Progress towards the comprehensive control of hepatitis B in Africa: A view from South Africa. Gut. 1996;38(Suppl 2):S31–6. doi: 10.1136/gut.38.suppl_2.s31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knipe DM, Howley PM. 5th ed. Vol. 1. Philadelphia: Lippincott Williams and Wilkins; 2007. Fields Virology; p. 2664. [Google Scholar]
- 12.Lok AS, McMahon BJ. Chronic hepatitis B: Update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 13.Murray PR, Rosenthal KS, Pfaller MA. 5th ed. Philadelphia: Elsevier Mosby; 2005. Medical Microbiology. [Google Scholar]
- 14.WHO. Geneva: World Health Organization; 2002. Global Alert and Response (GAR) – Hepatitis B; p. 76. [Google Scholar]
- 15.Blankson A, Wiredu EK, Gyasi RK, Adjei A, Tettey Y. Sero-prevalence of hepatitis B and C viruses in cirrhosis of the liver in Accra, Ghana. Ghana Med J. 2005;39:132–7. [Google Scholar]
- 16.Qiao Q, Keinanen-Kiukaanniemi S, Kivela SL. Association of waist to hip ratio with diabetes among middle-aged subjects with impaired glucose tolerance. Eur J Public Health. 1997;7:106–8. [Google Scholar]
- 17.Shah A, Bhandary S, Malik SL, Risal P, Koju R. Waist circumference and waist-hip ratio as predictors of type 2 diabetes mellitus in the Nepalese population of Kavre District. Nepal Med Coll J. 2009;11:261–7. [PubMed] [Google Scholar]
- 18.Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Invest. 2000;106:473–81. doi: 10.1172/JCI10842. [DOI] [PMC free article] [PubMed] [Google Scholar]


