Abstract
Background:
Patients in Intensive Care Units (ICUs) are a significant subgroup of all hospitalized patients, accounting for about a quarter of all hospital infections.
Aim:
The aim was to study, the current status of nosocomial infection, rate of infection and distribution of infection among patients admitted in Medical Intensive Care Unit (MICU) of a District Hospital.
Subjects and Methods:
Data were collected retrospectively from 130 patient's records presented with symptoms of nosocomial infection in MICU of a Tertiary Health Center, Tumkur from August 2012 to May 2013. Descriptive statistics using percentage was calculated.
Results:
Incidence of nosocomial infections in MICU patients was 17.7% (23/130). Of which 34.8% (8/130) was urinary tract infection (UTI) being the most frequent; followed by pneumonia 21.7% (5/130), 17.4% (4/130) surgical site infection, 13.0% (3/130) gastroenteritis, 13.0% (3/130) blood stream infection and meningitis. The nosocomial infection was seen more in the 40-60 year of age. The male were more prone to nosocomial infections than the female.
Conclusion:
The most frequent nosocomial infections (urinary, respiratory, and surgical site) were common in geriatric patients in the MICU setting and are associated with the use of invasive device. Large-scale studies are needed to be carried out in Indian population to plan long-term strategies for prevention and management of nosocomial infections.
Keywords: Medical Intensive Care Unit, Nosocomial infections, Tertiary health centre
Introduction
Infections in critical care unit are high, and of serious hospital problems. Infections acquired during the hospital stay are generally called nosocomial infections, initially known as infections arising after 48 h of hospital admission.[1,2] National Nosocomial Infections Surveillance system defines a nosocomial infection as a localized or systemic condition that results from adverse reaction to the presence of an infectious agent (s) or its toxin (s) that was not present or incubating at the time of admission to the hospital.[1] These infections are opportunistic, and microorganisms of low virulence can also cause disease in hospital patients whose immune mechanisms are impaired. Hence, antimicrobial resistance increases in such cases making increase in morbidity and mortality. Nosocomial infections are typically exogenous, the source being any part of the hospital ecosystem, including people, objects, food, water, and air in the hospital.[3]
In addition, they impose heavy cost on hospitals causing increased hospitalization time, increased morbidity, and mortality.[4] The risk factors for nosocomial infections include: Diabetes mellitus, intubation, persistent sounding, surgical drains, poor health status, lack of using gloves, irregular and inappropriate debridement and wound bandage. Although the Intensive Care Units (ICUs) account for fewer than 10% of total beds in most hospitals, more than 20% of all nosocomial infections are acquired in ICUs.[5] According to published literature the most prevalent nosocomial infections among patients in ICU are urinary tract infection (UTI), pneumonia, bloodstream infections, skin and soft tissue infections, gastroenteritis, hepatitis and central nervous system infections like meningitis.[6,7,8,9]
Hospital acquired infections involves yearly about 2 millions in US and accounts approximately for a cost of 4.5 billion dollars.[4] The magnitude of this problems in a developing country like India is even more serious since there is no available established statistics. Situation will be still pathetic when it comes for a government sector as maintenance and monitoring are questionable. Even though, it is not possible to eradicate the nosocomial or hospital acquired infections entirely, many of them can be prevented by proper control measures. Hence, the objective of the present study is to know the prevalence and nature of nosocomial infections in ICU of a government district hospital.
Subjects and Methods
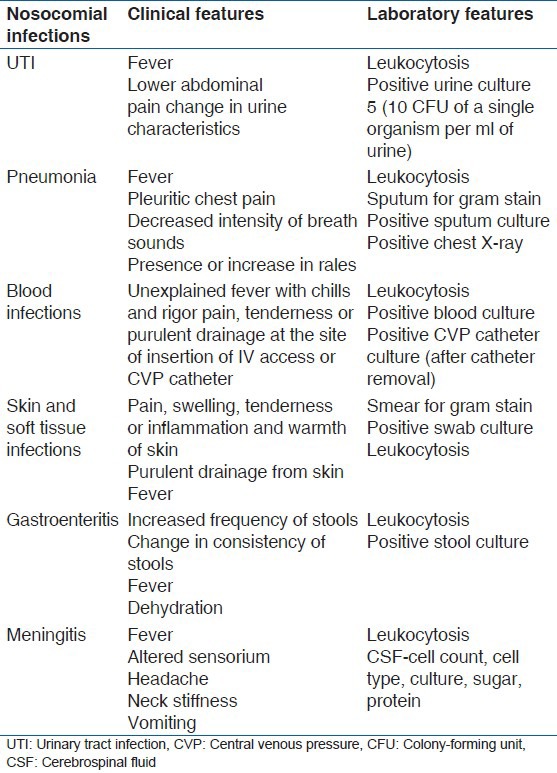
The study was a retrospective analytical study. Methodology involved collection of data of nosocomial infections from patient records, analysis of infections, and their causes. A total of 130 records of patients admitted to ICU of a tertiary health center, Tumkur, Karnataka during August 2012 to May 2013 were considered and out of these 23 belonged to medical (nonsurgical) cases. This tertiary health center covers a population of Tumkur District, with approximately 1000 patients input per day. Prior permission was obtained from district surgeon and ethical clearance was obtained from Ethical Clearance Committee of Sri Siddhartha Dental College. Detailed history and physical examination notes were reviewed in all patients’ records. A diagnostic criteria for nosocomial infection by Mukherjee et al.[10] [Table 1] was used for categorizing the cases. Descriptive statistics was used for analysis.
Table 1.
Diagnostic criteria for nosocomial infections
Results
This study was conducted on 130 patients in hospital Medical Intensive Care Unit (MICU). Twenty-three out of 130 (23/130-17.7%) admitted to the MICU suffered from nosocomial infection, there were 18 males, five females. The age ranged from 43 to 72 years, mean age being 56 years. The mean duration of stay of the patients in the hospital was 8.1 days. Table 2 shows the distribution of the nosocomial infections in those patients.
Table 2.
Distribution of nosocomial infections among nosocomial positive patients
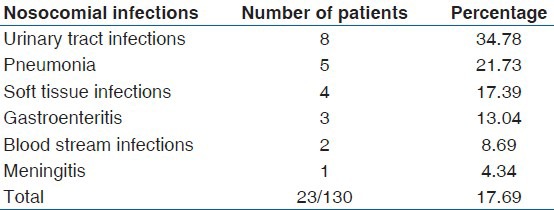
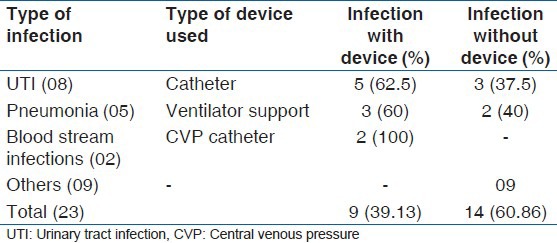
In our study, it was observed that distribution of nosocomial infections in MICU were UTI (34.8% - 8/130), pneumonia (21.7% - 5/130), soft tissue infections (17.4% - 4/130), gastrointestinal (13.0% - 3/130), blood stream infections (8.7% - 2/130) and meningitis (4.3% - 1/130). Table 3 depicts that most nosocomial infections are device related. UTI was related to the catheter and pneumonia to ventilator.
Table 3.
Devices related to nosocomial infections
Discussion
The incidence of Nosocomial infections in our study was 17.69% similar to hospital record statement of NM hospital and heart center and their own study, mentioned in Pratham et al.[6] Vincent et al.,[11] but less compared to 33.5% by Beaujean et al.[12] This may be due to the relative small sample size of the present study. The general distribution pattern of the nosocomial infections in our study showed UTI to be the most common, followed by pneumonia, skin and soft tissue infections, gastroenteritis, bloodstream infections and meningitis. It is similar to Lee et al.,[13] Richards et al.[2] and Pratham et al.[6] but in studies conducted by Vincent et al.[11] and Michael et al.[9] incidence of pneumonia was followed by UTI.
Male patients were predominant in the present study with overall mean age being 56 years. The increase incidence in geriatric age group may be due to their defective host defense mechanism. Similarly with respect to the role played by invasive devices in contributing to nosocomial infections, present study showed that 62.5% of UTI occurred in catheterized patients, 60% of pneumonia was associated with mechanical ventilation and 100% of bloodstream infections with catheters could be attributed to the use of invasive devices. The findings were similar to Richards et al.,[2] Pratham et al.,[6] Suman.[14]
Intensive care unit acquired infections account for substantial morbidity, mortality, and expensive. Nosocomial infections increase the cost of healthcare in the countries least able to afford them through increased: Length of hospitalization; treatment with expensive medications (e.g. antibiotics); and use of other services (e.g. laboratory tests, X-rays and transfusions).[15]
Major infections found in ICU were due to Acinetobacter baumannii, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus and Streptococcus pyogenes.[3] The infection rate was maximum in the urinary tract (44.4%) followed by wound infections (29.4%), pneumonia (10.7%) and bronchitis (7.4%). A. baumannii was found to be associated with UTIs, respiratory tract infections, septicemia, bacteremia, meningitis and wound infections. A. Baumannii displayed higher resistance to more number of antibiotics than other nosocomial pathogens from ICU. Hence, it is very important to target the nosocomial infections.[3]
However, in this study, due to lack of proper care, it was observed that the majority of the cases from the tertiary health center were referred to higher specialty centers; hence, the magnitude of incidence of nosocomial infections may be under looked, also limiting to assess the mortality associated with these infections. Hence, the impact of nosocomial infections is more significant in resource-poor countries.
Main problems in developing countries are understaffing, poor infrastructure in ICU and poor maintenance of records making situation difficult to get clarity on the incidence of these infections. Although it is difficult to solve some problems associated with financial hardship in developing countries, most solutions are simple and not resource demanding. Infection control strategies such as hand hygiene and wearing gloves; paying attention to well established processes for decontamination and cleaning of soiled instruments and other items, followed by either sterilization or high-level disinfection; and improving safety in operating rooms and other high-risk areas where the most serious and frequent injuries and exposures to infectious agents can resolve the problem to a major extent.
Limitation
Even though the sample size was very less, unequal distribution of samples according to gender and age due to which exact prevalence of nosocomial infections was not calculated for independent variables, nosocomial infections mere presence among the present study cases cannot be ruled out. Hence, further systematic and standardized large scale studies are suggested in government sectors for prevention and management of these nosocomial infections.
Conclusion
This study showed UTIs and pneumonias are the common nosocomial infections among patients in ICU. Our study also revealed that the incidence of infections increases with the use of invasive devices and the geriatric population is highly vulnerable to nosocomial infections. Early recognition of infections and short term use of invasive devices along with proper infection control procedures can significantly decrease the incidence of nosocomial infections in geriatric patients.
Acknowledgment
We thank Dr. Rudra Murthy, Resident Medical Officer, District Hospital, Tumkur and Mr. Devraj, in charge of Medical Records Department for their support during the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM. CDC definitions for nosocomial infections, 1988. Am J Infect Control. 1988;16:128–40. doi: 10.1016/0196-6553(88)90053-3. [DOI] [PubMed] [Google Scholar]
- 2.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. National Nosocomial Infections Surveillance System. Crit Care Med. 1999;27:887–92. doi: 10.1097/00003246-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 3.Patwardhan RB, Dhakephalkar PK, Niphadkar KB, Chopade BA. A study on nosocomial pathogens in ICU with special reference to multiresistant Acinetobacter baumannii harbouring multiple plasmids. Indian J Med Res. 2008;128:178–87. [PubMed] [Google Scholar]
- 4.Rahim B, Peyman M, Davood N, Hamid RK. An epidemiological study of nosocomial infections in the patients admitted in the intensive care unit of Urmia Imam Reza Hospital: An etiological investigation. Ann Biol Res. 2011;2:172–8. [Google Scholar]
- 5.Ulu-Kilic A, Ahmed SS, Alp E, Doğanay M. Challenge of intensive care unit-acquired infections and Acinetobacter baumannii in developing countries. OA Crit Care. 2013;1:2. [Google Scholar]
- 6.Pratham R, Manmohan S, Vipin R. A retrospective study of nosocomial infections in patients admitted in M.I.C.U. Indian J Pharm Pract. 2011;4:62–5. [Google Scholar]
- 7.Crossley KB, Peterson PK. 5th ed. Philadelphia: 2000. Infection in Elderly, Principles and Practice of Infectious Diseases; pp. 3164–9. [Google Scholar]
- 8.Emori TG, Banerjee SN, Culver DH, Gaynes RP, Horan TC, Edwards JR, et al. Nosocomial infections in elderly patients in the United States, 1986-1990. National Nosocomial Infections Surveillance System. Am J Med. 1991;91:289S–93. doi: 10.1016/0002-9343(91)90384-a. [DOI] [PubMed] [Google Scholar]
- 9.Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in combined medical-surgical intensive care units in the United States. Infect Control Hosp Epidemiol. 2000;21:510–5. doi: 10.1086/501795. [DOI] [PubMed] [Google Scholar]
- 10.Mukherjee T, Pramod K, Srinivasan G, Rao MY. Nosocomial infections in geriatric patients admitted in ICU. J Indian Acad Geriatric. 2005;2:61–4. [Google Scholar]
- 11.Vincent JL, Bihari DJ, Suter PM, Bruining HA, White J, Nicolas-Chanoin MH, et al. The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA. 1995;274:639–44. [PubMed] [Google Scholar]
- 12.Beaujean DJ, Blok HE, Vandenbroucke-Grauls CM, Weersink AJ, Raymakers JA, Verhoef J. Surveillance of nosocomial infections in geriatric patients. J Hosp Infect. 1997;36:275–84. doi: 10.1016/s0195-6701(97)90054-2. [DOI] [PubMed] [Google Scholar]
- 13.Lee YL, Thrupp LD, Friis RH, Fine M, Maleki P, Cesario TC. Nosocomial infection and antibiotic utilization in geriatric patients: A pilot prospective surveillance program in skilled nursing facilities. Gerontology. 1992;38:223–32. doi: 10.1159/000213332. [DOI] [PubMed] [Google Scholar]
- 14.Suman SM, Alexander AP. Nosocomial infections in the intensive care unit. Anaesth Intensive Care Med. 2012;13:204–8. [Google Scholar]
- 15.Dror M, Keith K. Epidemiology and prevention of infections and antimicrobial resistance in the intensive care unit. [Last cited on 2013 Nov 10]. Available from: http://www.uptodate.com//epidemiology-and-prevention-of-infections-and-a .


