Abstract
Background:
A retrospective study of lumbosacral angle (LSA) in normal lateral supine lumbosacral radiographs of 274 Nigerians (aged 15-74 years) of Southeast region. A supine lateral lumbar spine radiograph is a very accurate means of measuring lordotic angles. The LSA is one of such angles, and can be used in the investigation, treatment and follow-up of low back disorders. Little is known about what the normal value for our population is and therefore, what constitutes hypo-/hyper-lordosis; most of the data in use in medical practice are based on studies on other races.
Aim:
To quantify the normal LSA in our population.
Materials and Methods:
LSA was measured by the Ferguson's technique and the data analyzed with SPSS Statistics version 17.0 (Chicago IL, USA).
Results:
LSA varied between 18° and 71°. With a 95.0 confidence interval of 43.3-45.6°, the mean (standard deviation) was 44.5 (9.9)° and showed no significant variation with sex and between various age groups; it compared favorably (though with small difference) with some of the literature values currently in use.
Conclusion:
This study had established the normal lordosis and the possible values at which to consider hypo-lordosis (below 15°), and hyper-lordosis (above 75°) in our population. Also established is that the development of lumbar lordosis ceases at spinal maturity, and that in normal lumbar lordosis measurement, the retrospective approach is a credible alternative to the prospective method.
Keywords: Black population, Measurement, Normal lumbosacral angle
Introduction
The lumbar lordotic curve is the anterior convexity of the lumbar spine in the mid-sagittal plane.[1] It has conventionally been thought that lordosis develops in human children during the 1st year of life, in response to new biomechanical loads (which influence the growth of the vertebrae) as they begin to pull themselves up into standing postures prior to taking their first steps. However, recent research suggests that lordosis is evident in the lumbosacral region of as much as 60% of human fetuses, suggesting that there may be a genetic component to the morphology.[2] As an infant starts to stand, usually between 12 and 18 months of age, lumbar lordosis continues to develop until the completion of spinal growth, normally between 13 and 18 years.[3] Children who never assume the erect position develop a lumbar lordosis to the same degree and at the same time as other children. Growth retardation gives a delay in the emergence of the lumbar lordosis.[4] To quantify this curve, various methods have been used. They include goniometry,[5,6] radiography,[7,8,9,10,11] flexible rulers,[12,13,14,15,16] software methods,[17] spinal mouse,[18] and inclinometer.[19,20] Of all these methods, radiography remains the gold standard and lordotic measurement can accurately be measured in a supine lateral lumbosacral spine radiograph.[21,22,23] The lumbosacral angle (LSA), one of the clinically important radiographic angles related to this curve, and frequently measured by the Ferguson's technique[24,25] is important in the management of patients with low back disorders because it may be affected by disorders such as inflammation, degeneration etc., Little is known about what the normal value for our population is and therefore, what constitutes hypo-/hyper-lordosis; most of the data in use in medical practice is based on studies on other races. This study was, therefore, aimed at quantifying the normal value of this angle in our population.
Materials and Methods
The LSA was measured in a retrospective study of normal lateral lumbosacral spine radiographs taken in the recumbent position in 274 patients of all genders (132 males and 142 females) between the ages of 15 years and 74 years; mean (standard deviation [SD]) was 35.2 (11.7) years. The radiographs were from the archives of two tertiary health institutions in the Southeast part of Nigeria. The institutions are the University of Nigeria Teaching Hospital and National Orthopedic Hospital, both in Enugu state. The two study centers routinely take their lateral lumbosacral radiographs in the recumbent position The aim of using two institutions for the study was not only to widen the geographic area of coverage., but also to increase the number of radiographs studied because it was not easy to find normal radiographs in the archives; most of the archival radiographs showed pathological changes. The two tertiary institutions play host to patients from all the Southeast states of Nigeria and also to few patients from the neighboring South-South and North central parts of Nigeria. The studied radiographs spanned a 7 year period: 1994-2000. Ethical clearance was obtained from the Teaching Hospital.
Although this study would have been ideally done prospectively using normal subjects, a retrospective method was adopted for the following reasons: (1) To avoid ethical issues like patient's irradiation, especially in females in their reproductive age; (2) even if some of the studied radiographs in the retrospective approach belonged to subjects that presented with back complaints, low back pain without any radiographically demonstrable vertebral pathology have been reported not to significantly affect the degree of normal lumbar lordosis;[26,27] (3) one of the drawbacks of the prospective method is the over-reliance on the history of “absence of low back complaint” as a major criterion in selecting “normal” subjects, and in most cases, without subjecting the patient to complete medical history, physical, neurological, and orthopedic examinations. Thus, some of the patients, after undergoing X-ray exposure, are discovered to have a lumbosacral pathology and, therefore, ineligible for the study.
Each radiograph, the request form, and sometimes the radiological report were contained in a film jacket. The request form had such information like patient's name, age, sex, address, clinical information etc., From the request form, the patient's Nigerian citizenship and ethnic group was deciphered. Despite the fact that some of the radiographs were filed with their radiological report, the author still reviewed all to ensure that they were normal. Only radiographs adjudged to be normal by the author, and which belonged to indigenes of Southeast geopolitical region of Nigeria were selected for study.
The criteria for normality were (1) presence of five lumbar and five sacral vertebrae; (2) progressive increase in vertebral height from L1 to L5, or the height remain the same;[28] (3) anteriorly convex lordotic curve that gives place to a concavity in the sacral region;[29] (4) posterior margins of the vertebral bodies form a smooth curved line but the superior margin of the lower vertebra may often deviate from this line;[28] (5) the corticated endplates of the vertebral bodies is filled by intervertebral discs that increase in thickness from L1 to L5;[30] the relatively narrow L5/S1 disc is wedge-shaped with its anterior vertical height greater than the posterior;[3] (6) no radiographic evidence of disease or congenital abnormality in the lumbosacral spine.
The exclusion criteria included patients below 15 years of age, or whose age and/or sex were not recorded, non-indigenes of Southeast region of Nigeria, poor quality radiographs, and radiographs showing any evidence of disease or congenital abnormality. Patients below 15 years were excluded to ensure that only those that have attained spinal maturity were studied.
The LSA [formed between a line across the plane of the superior margin of S1 and a horizontal line, Figure 1] was measured by mounting each radiograph on a viewing screen with good illumination. With a 30 cm long transparent ruler, lines for the measurement of the angle were drawn with a pencil, using appropriate landmarks. The angle was measured in degrees using a protractor. All measurements were made by the author in order to remove inter-observer error. The radiographs were grouped into six age groups with a class interval size of 10. The age groups included: (1) 15-24; (2) 25-34; (3) 35-44; (4) 45-54; (5) 55-64; and (6) 65-74 years old. The data was analyzed with SPSS Statistics version 17.0 (Chicago IL, USA), and P < 0.05 was considered significant. Some of the statistical methods employed included frequency distribution curve, mean and SD, test of significance, and confidence interval (CI).
Figure 1.
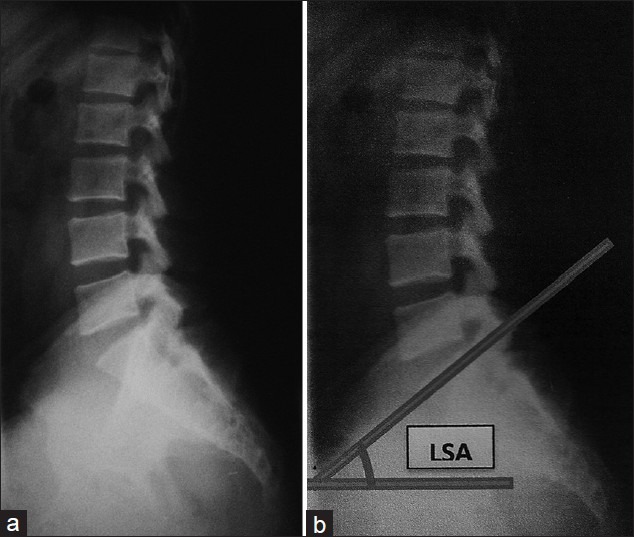
(a) Radiograph of normal lateral lumbosacral spine (b) measurement lines for the normal lumbosacral angle (LSA): LSA is the angle formed between a line across the plane of superior margin of S1 and a horizontal line (Ferguson's technique)
Results
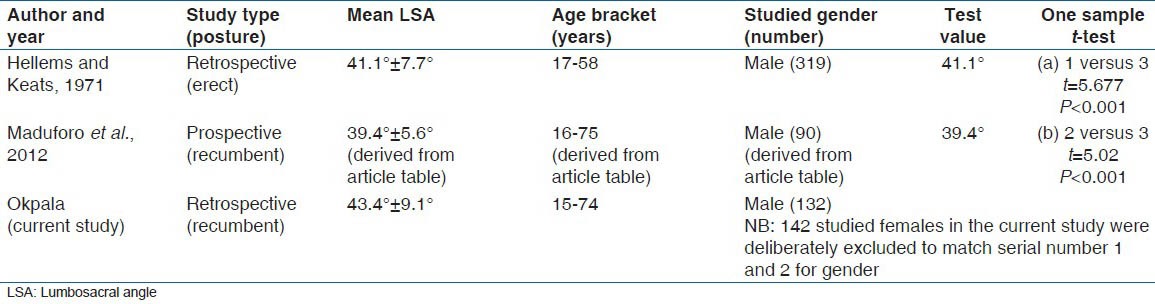
A total of 274 normal lateral recumbent lumbosacral spine radiographs were assessed (males = 132; females = 142). The mean age (SD) of the patients was 35.2 (11.7) years [Figure 2]; 34.1 (11.1) years for the males, and 36.3 (12.1) years for the females. There was no significant difference between the mean ages of the males and females (t = 1.55, P = 0.12). With a 95.0 CI of 43.3-45.6°, the LSA was 44.5 (9.9)° (range = 18-71°), and showed no significant variation with sex [Table 1, Figure 3], nor between the various age groups [Figure 4, Table 2]. There was significant difference between this LSA and all the literature values cited in this study [Table 3]; the differences were however small in most cases [Table 4]. It can therefore be stated that the LSA obtained in this study compared favorably with most of the literature values cited in this study, irrespective of the fact that some of these literature values were obtained in prospective studies in either erect or recumbent positions.
Figure 2.
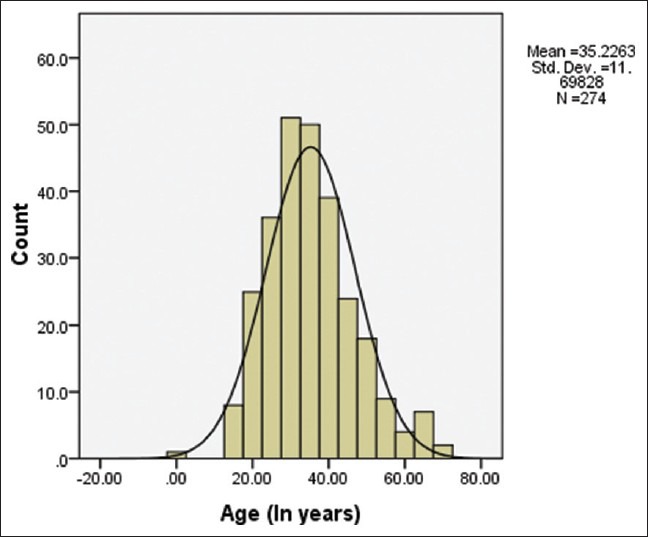
Histogram with normal frequency distribution curve of the total mean age of the patients
Table 1.
LSA according to gender
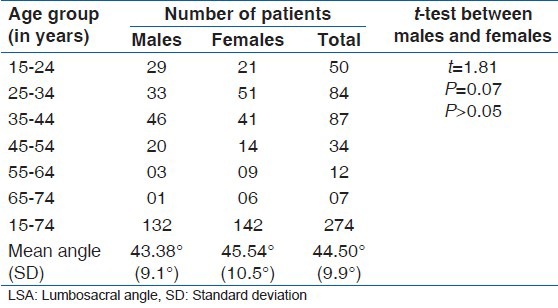
Figure 3.
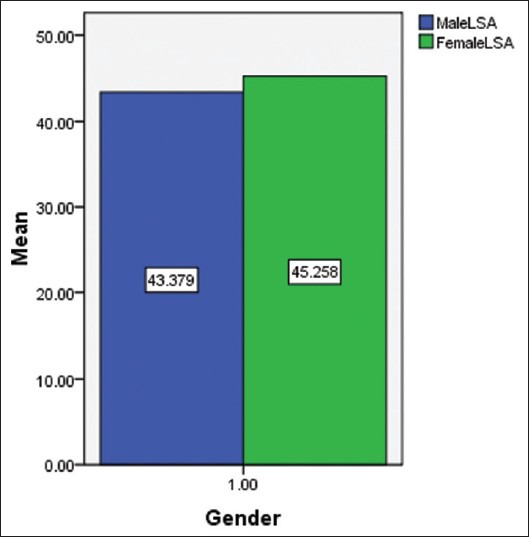
Bar chart of the mean lumbosacral angle by gender
Figure 4.
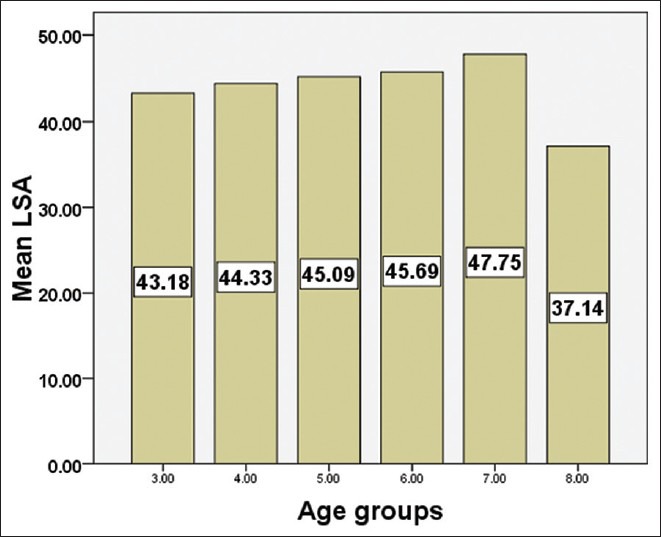
Histogram of the mean lumbosacral angle according to age groups. Key: 3 = 15-24 years, 4 = 25-34 years, 5 = 35-44 years, 6 = 45-54 years, 7 = 55-64 years, and 8 = 65-74 years
Table 2.
LSA according to age groups
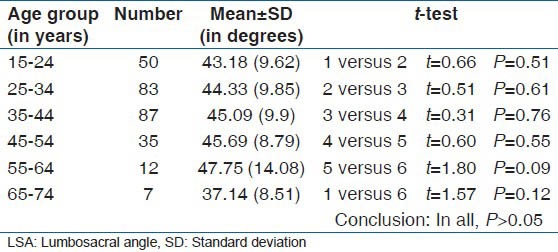
Table 3.
Comparison of the total mean LSA (44.5°) of the current study with some literature values
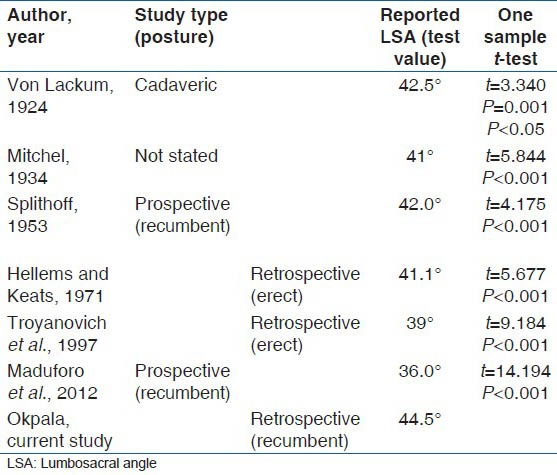
Table 4.
Comparison of the male mean LSA (43.4°) of the current study with some literature values
Discussion
The lumbar spine is convex anteriorly and this curve is known as the lumbar lordosis. The development of the lumbar lordosis begins as an infant starts to stand, usually between 12 and 18 months of age, and it continues to develop until the completion of spinal growth, normally between 13 and 18 years.[3] Since the age range of the subjects in this study is 15-74 years, it means that virtually all have completed spinal growth. The degree of curvature of lumbar lordosis is believed to be affected by factors like position, sex, age, and pathological conditions. Some authors believe that it increases with a change from the recumbent to the upright position; others believe that it flattens with age and some that it is higher in females of reproductive age than in males due to the increased secretion of a hormone called relaxin during this period. However, most authors believe that pathological conditions like birth defects, trauma, inflammatory, and degenerative disorders may affect it.
In comparison to the radiographic method, the clinical methods of lumbar lordosis measurement such as goniometry, the software method, flexible ruler, inclinometer, spinal mouse etc., are noninvasive, but since the necessary reliability and validity studies have not been done on them, they lack test standardization and the tests largely depend on the experience of the examiner. Furthermore, some of the clinical methods like spinal mouse and flexible ruler are time consuming and can therefore not be easily employed where there is a need for quick feedback. The drawbacks of the radiographic method include irradiation (this makes periodic examination not advisable), relatively high cost of the examination, limited equipment portability, time to obtain and read the image. Despite these drawbacks of the radiographic technique, it remains the gold standard and lordotic measurement can accurately be measured in a supine lateral lumbosacral spine radiograph.[21,22,23] The LSA has been variously called the “sacro-horizontal angle”, the “sacral angle”, the “sacral LSA.”, the “Ferguson's angle”, and the “LSA;”[31] it is the angle formed between a line across the plane of the superior margin of the sacrum and a horizontal line. The normal value reported by many authors show great variation. Von Lackum reported a value of 42.5° in a study of 30 cadavers.[32] Mitchell reported an average angle of 41° in a study of 28 persons but did not state the method by which the radiographs were obtained.[33] Splithoff recorded 40-44° as the largest number of angles in a prospective study of 100 subjects in the recumbent position;[34] however, other than a bar graph, he did not state what range of values might be expected in a normal population. In the erect position, Hellems and Keats have shown in a retrospective study of 319 normal males aged 17-58 years, who undertook X-ray as part of routine pre-employment examination, that the LSA measures 41.1 (7.7)°.[35] Bryan reported that it varies between 15° and 25° in the Caucasians in erect position and that females have higher values than males.[36] Ferguson reported that when it exceeds 34°, an abnormality in stability exists between the lumbar and sacral spines.[28] Troyanovich et al. in their retrospective study of 50 normal healthy subjects in the erect posture recorded 39°.[37] Maduforo et al. reported a value of 36.0 (9.4)° in a prospective study of 100 male subjects (aged 0-75 years) of South-South region of Nigeria.[38] In the current study, the LSA is 44.5 (9.9)° [Table 1] irrespective of gender. Thus, while some authors studied the LSA of only the male gender using prospective method probably to avoid the ethical issue of irradiating the female pelvis, the retrospective approach used in the current study obviated this and enabled the study of both gender. The 44.5 (9.9)° LSA mean obtained in this study in the recumbent position compared favorably (though with small differences) with many of the literature values currently in use [Table 3]; this was despite the fact that at least one of these literature values was obtained during a prospective study. For example, since 43.4 (9.1)°, my male mean LSA is only about 2.3° higher (t = 2.88; P = 0.01) than that obtained in the erect position by Hellems and Keats in their retrospective study of 319 males, and since both have almost equal SD, both could be assumed to be equal [Table 4]. Furthermore, the mean LSA is only about 5.5° greater (t = 9.18; P < 0.01) than the 39° obtained in the erect position by Troyanovich et al. in their retrospective study of 50 subjects; perhaps, this difference could have been less if their sample size was higher [Table 3]. Thus the result of this study appeared to be in agreement with the results obtained in 1992 by Bogduk et al.[39] that lumbar lordosis is not significantly different in the recumbent and upright positions. In healthy individuals, the tone of the spinal muscles was thought to be sufficient to prevent such an increase in the upright position.[9]
Also, my male LSA mean of 43.4 (9.1)° is about 7.4° higher (t = 9.32; P < 0.01) than the 36.0 (9.4)° obtained by Maduforo et al. in their study of 100 males aged 0-75 years [Table 3]. Perhaps, their inclusion of children below 15 years of age whose lordotic angles were still developing might partly account for this difference; this is because they noted the LSA to be greater in adults than in children less than 14 years of age. However, the mean LSA for the 16-75 years age bracket derived from their table was 39.4 (5.6)°, and this is about 4° less (t = 5.02; P < 0.01) than the male mean LSA of the present study [Table 4]. Notwithstanding this nearly 4° difference between my male mean LSA (obtained in a retrospective study of 15-74 years age group) and that of 16-75 years age group derived from the table of Maduforo et al. (in a prospective study), it is apparent that the two results, obtained in neighboring geopolitical regions of Nigeria, compared favorably. It is important to remember that the reported literature values of the normal lumbar lordosis measured by the prospective method by different authors showed great variation even among the same racial group.
Thus, what can be concluded from the comparison of the results of the present study with that of Maduforo et al., Troyanovich et al., as well as Hellems and Keats, is that the retrospective approach employed in the present study is a reliable and accurate method of measuring normal lumbar lordosis. Also, the male mean LSA of the present study obtained in the recumbent position compared favorably with the mean LSA obtained by Hellems and Keats (in erect position) and the mean LSA derived from the article table of Maduforo et al. for the 16-75 years age bracket (obtained in the recumbent position); this thus suggests that posture has no appreciable effect on the degree of lumbar lordosis. The result of the LSA (44.5°) is contrary to the opinion of Ferguson[28] that an abnormality in stability between the lumbar and sacral spines exists when the LSA exceeds 34°. This may be due to racial differences in the structures of the lumbosacral spines. In the current study, there is no significant variation (t = 1.81, P = 0.07) between the male LSA of 43.4 (9.1)° when compared to the female LSA of 45.5 (10.5)° contrary to the opinion of some authors like Bryan that females have higher value. Also, no significant variation of the LSA was observed between the various age groups [Table 2]; this agrees with the fact that the development of the lumbar lordosis reaches a plateau at spinal maturity.[3,9]
The main limitation in this study was the inability of the author to be involved in the technique of obtaining the radiographs since it was a retrospective study; this is notwithstanding the fact that the two study centers routinely take their lateral lumbosacral radiographs in the recumbent position. Even if a few of the radiographs were taken in the upright position, the large number of the sample size would have annulled whatever effect that this might have. Furthermore, some authors have shown that the lumbar lordosis is not significantly different in the erect and recumbent positions,[39] a fact that appeared to have been justified by the present study because the male mean LSA of 43.4 (9.1)° obtained in this retrospective study of 132 radiographs (if the 142 females were excluded) taken in the recumbent position, compared favorably with the 41.1 (7.7)° reported by Hellems and Keats in their retrospective study of 319 male subjects in the erect posture. Also the studied age bracket in the present study (15-74 years) is not too different from the 17 to 58 years age bracket studied by them.
A prospective study involving the use of any of the more likely available and affordable non-radiographic methods of lumbar lordosis measurement is recommended as a further study. If the more reliable radiographic technique is used for initial examination, the clinical method may be used for monitoring and follow-up and thus substantially reducing patient's irradiation and cost of treatment.
Conclusion
In this study of 274 Nigerians of mostly Southeast geo-political region who have attained spinal maturity, the range of the normal LSA is 18-71° and the mean (SD), 44.5 (9.9)°, irrespective of gender or age group. This mean value, obtained in a retrospective study, compared favorably (though with a small difference) with some of the literature values (obtained in both prospective and retrospective studies) currently in use. Thus, this retrospective approach is a reliable and accurate method of measuring normal lumbar lordosis and seems therefore to be a credible alternative to the prospective method. Furthermore, using the LSA, it is now possible to have an idea of the possible values at which to consider hypo-lordosis (below 15°)/and hyper-lordosis (above 75°) in our population. This study have also established that in all the various age groups between 15 and 72 years (which were the smallest and the highest ages of the studied population), the mean LSA showed no significant difference between the groups, and this confirms that the development of lumbar lordosis reaches a plateau at spinal maturity, usually between 13 and 18 years.[3,9]
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Bogduk N, Twomey LT. 2nd ed. New York: Churchill Livingstone; 1991. Clinical Anatomy of the Lumbar Spine; pp. 45–7. [Google Scholar]
- 2.Beasley M. Lumbar Lordosis. 2013. [Last accessed on 2013 Aug 26]. Available from: http://www.Carta.anthropogeny.org.moca/topics/lumbar-lordosis .
- 3.Oliver J, Middleditch A. Functional Anatomy of the Spine. Oxford: Butterworth-Heinemann; 1998. Lumbar spine; pp. 36–58. [Google Scholar]
- 4.Reichmann S, Lewin T. The development of the lumbar lordosis. A post mortem study on excised lumbar spines. Arch Orthop Unfallchir. 1971;69:275–85. doi: 10.1007/BF00416265. [DOI] [PubMed] [Google Scholar]
- 5.Norkin CC, White DJ. Chicago: Am Acad Orthop Surg; 1965. Joint Motion: Method of Measuring and Recording; pp. 48–9. [Google Scholar]
- 6.Burdett RG, Brown KE, Fall MP. Reliability and validity of four instruments for measuring lumbar spine and pelvic positions. Phys Ther. 1986;66:677–84. doi: 10.1093/ptj/66.5.677. [DOI] [PubMed] [Google Scholar]
- 7.Cobb JR. Outline for the study of scoliosis. In: Thomson JE, Blount WP, editors. American Academy of Orthopaedic Surgeons, Instructional Course Lectures. Vol. 5. Ann Arbor: JW Edwards; 1948. pp. 261–75. [Google Scholar]
- 8.Troyanovich SJ, Harrison DE, Harrison DD, Holland B, Janik TJ. Further analysis of the reliability of the posterior tangent lateral lumbar radiographic mensuration procedure: Concurrent validity of computer-aided X-ray digitization. J Manipulative Physiol Ther. 1998;21:460–7. [PubMed] [Google Scholar]
- 9.Chernukha KV, Daffner RH, Reigel DH. Lumbar lordosis measurement. A new method versus Cobb technique. Spine (Phila Pa 1976) 1998;23:74–9. doi: 10.1097/00007632-199801010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Chen YL. Vertebral centroid measurement of lumbar lordosis compared with the Cobb technique. Spine (Phila Pa 1976) 1999;24:1786–90. doi: 10.1097/00007632-199909010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Hong JY, Suh SW, Modi HN, Hur CY, Song HR, Park JH. Reliability analysis for radiographic measures of lumbar lordosis in adult scoliosis: A case-control study comparing six methods. Eur Spine J. 2010;19:1551–7. doi: 10.1007/s00586-010-1422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hart DL, Rose SJ. Reliability of a noninvasive method for measuring the lumbar curve. J Orthop Sports Phys Ther. 1986;8:180–4. doi: 10.2519/jospt.1986.8.4.180. [DOI] [PubMed] [Google Scholar]
- 13.Youdas JW, Suman VJ, Garrett TR. Reliability of measurements of lumbar spine sagittal mobility obtained with the flexible curve. J Orthop Sports Phys Ther. 1995;21:13–20. doi: 10.2519/jospt.1995.21.1.13. [DOI] [PubMed] [Google Scholar]
- 14.Rajabi R, Seidi F, Mohamadi F. Which method is accurate when using the flexible ruler to measure the lumbar curvature angle? Deep pint or midpoint of arch? World Appl Sci J. 2008;4:849–52. [Google Scholar]
- 15.Seidi F, Rajabi R, Ebrahimi TI, Tavanai AR, Moussavi SJ. The Iranian flexible ruler reliability and validity in lumbar lordosis measurements. World J. Sport Sci. 2009;2:95–9. [Google Scholar]
- 16.de Oliveira TS, Candotti CT, La Torre M, Pelinson PP, Furlanetto TS, Kutchak FM, et al. Validity and reproducibility of the measurements obtained using the flexicurve instrument to evaluate the angles of thoracic and lumbar curvatures of the spine in the sagittal plane. Rehabil Res Pract 2012. 2012:186156. doi: 10.1155/2012/186156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babai E, Khodamoradi A, Mosavi Z, Bahari S. An innovative software method for measuring lumbar lordosis. [Last accessed on 2013 Oct 06];Ann Biol Res. 2012 3:204–13. Available from: http://www.scholarsresearchlibrary.com . [Google Scholar]
- 18.López-Miñarro PA, Muyor JM, Belmonte F, Alacid F. Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. J Hum Kinet. 2012;31:69–78. doi: 10.2478/v10078-012-0007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Souza Filho JC, Abras AC, Carvalho MT, Souza MG, Souza AT, Costa LO. Analysis of the interexaminer reliability of two clinical tests to measure the flexion range of motion of the lumbar spine. Acta Fisiatr. 2007;14:214–8. [Google Scholar]
- 20.Macintyre NJ, Bennett L, Bonnyman AM, Stratford PW. Optimizing reliability of digital inclinometer and flexicurve ruler measures of spine curvatures in postmenopausal women with osteoporosis of the spine: An illustration of the use of generalizability theory. ISRN Rheumatol 2011. 2011:571698. doi: 10.5402/2011/571698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fernand R, Fox DE. Evaluation of lumbar lordosis. A prospective and retrospective study. Spine (Phila Pa 1976) 1985;10:799–803. doi: 10.1097/00007632-198511000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Salisbury PJ, Porter RW. Measurement of lumbar sagittal mobility. A comparison of methods. Spine (Phila Pa 1976) 1987;12:190–3. doi: 10.1097/00007632-198703000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Vrtovec T, Pernus F, Likar B. A review of methods for quantitative evaluation of spinal curvature. Eur Spine J. 2009;18:593–607. doi: 10.1007/s00586-009-0913-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferguson AB. Clinical and roentgen interpretation of lumbosacral spine. Radiology. 1934;22:548–58. [Google Scholar]
- 25.Ferguson AB. 2nd ed. New York: Paul B Hoeber, Inc; 1949. Roentgen Diagnosis of the Extremities and Spine; pp. 382–3. [Google Scholar]
- 26.Hansson T, Bigos S, Beecher P, Wortley M. The lumbar lordosis in acute and chronic low-back pain. Spine (Phila Pa 1976) 1985;10:154–5. doi: 10.1097/00007632-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis: Study of patients with and without low back pain. Clin Anat. 2003;16:144–7. doi: 10.1002/ca.10114. [DOI] [PubMed] [Google Scholar]
- 28.Meschan I. An Atlas of Anatomy basic to Radiology. Philadelphia: W. B. Sanders Company; 1975. The Lumbar spine; pp. 550–1. [Google Scholar]
- 29.Clark KC. Clark's Positioning in Radiography. 10th ed. Vol. 1. London: William Heinemann Medical Books Ltd; 1979. Vertebral column: Curves, postures, levels; p. 172. [Google Scholar]
- 30.Sutton D. A Textbook of Radiology and Imaging. 6th ed. Vol. 2. London: Churchill Livingstone; 1998. Intervertebral disc prolapse and degeneration; p. 1508. [Google Scholar]
- 31.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65:768–72. [PubMed] [Google Scholar]
- 32.Von Lackum HI. Lumbosacral region. J Am Med Assoc. 1924;82:1109–14. [Google Scholar]
- 33.Mitchell GA. The lumbosacral junction. J Bone Joint Surg. 1934;16:233–54. [Google Scholar]
- 34.Splithoff CA. Lumbosacral junction; roentgenographic comparison of patients with and without backaches. J Am Med Assoc. 1953;152:1610–3. doi: 10.1001/jama.1953.03690170024008. [DOI] [PubMed] [Google Scholar]
- 35.Hellems HK, Jr, Keats TE. Measurement of the normal lumbosacral angle. Am J Roentgenol Radium Ther Nucl Med. 1971;113:642–5. doi: 10.2214/ajr.113.4.642. [DOI] [PubMed] [Google Scholar]
- 36.Bryan GJ. Diagnostic Radiography, A Concise Practical Manual. 4th ed. London: Churchill Livingstone; 1987. Lumbar vertebrae; p. 152. [Google Scholar]
- 37.Troyanovich SJ, Cailliet R, Janik TJ, Harrison DD, Harrison DE. Radiographic mensuration characteristics of the sagittal lumbar spine from a normal population with a method to synthesize prior studies of lordosis. J Spinal Disord. 1997;10:380–6. [PubMed] [Google Scholar]
- 38.Maduforo C, West O, Nwankwo N, Onwuchekwa R, Etawo US, Ogbulu D. Study of the lumbosacral angles of males in Port Harcourt, South-South, Nigeria. Niger Health J. 2012;12:22–4. [Google Scholar]
- 39.Bogduk N, Macintosh JE, Pearcy MJ. A universal model of the lumbar back muscles in the upright position. Spine (Phila Pa 1976) 1992;17:897–913. doi: 10.1097/00007632-199208000-00007. [DOI] [PubMed] [Google Scholar]


