Abstract
Background:
Anemia in the postnatal period is a common problem, which has been subject of research recently. Though, it is a common problem, it is a less researched topic in India. Hence, this study was undertaken.
Aim:
The aim was to know the clinic-social factors associated with anemia in the postpartum period.
Materials and Methods:
This is a retrospective record-based study conducted in Government Lady Goschen Hospital, Kasturba Medical College, Mangalore. All the women in the postpartum period who had hemoglobin (%) <11 g/dl were included for the study. Information about various social and clinical factors was collected on a pretested semi-structured proforma. Multivariate analyses were used to get adjusted odds ratio. P < 0.05 was considered to be significant.
Results:
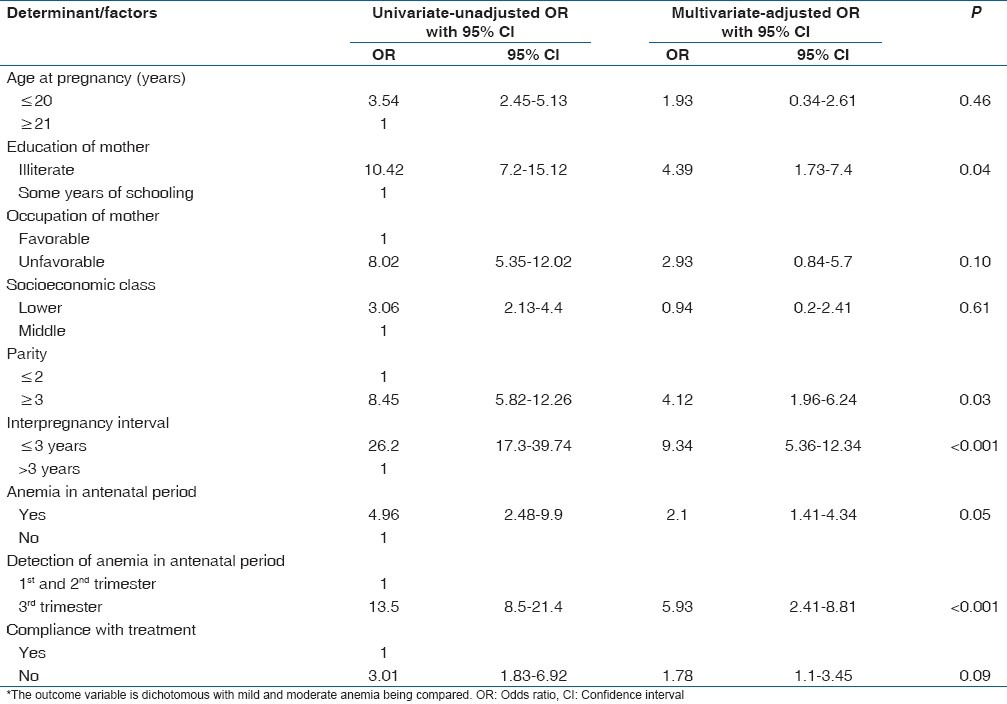
About 16.7% (165/988) had moderate anemia. The rest that is 83.3% (823/988) had mild anemia. Multivariate analysis reveals that following factors were significantly associated with moderate anemia: Illiterate mothers, parity (≥3), short interpregnancy interval (<3 years), presence of anemia in the antenatal period, late diagnosis in the antenatal period and poor compliance with treatment.
Conclusion:
Majority had mild anemia. Further research should be focused to (1) reasons for persistence of anemia from antenatal to postpartum period. (2) Find out the reason for failure to come for follow-up in the postpartum period even though services are free.
Keywords: Anemia, Postpartum women, Retrospective study
Introduction
Anemia in the antenatal period is a common problem in India as revealed by nationwide family health surveys.[1,2] Government of India has launched Reproductive Child Health program (RCH) under which, iron and folic acid (IFA) tablets are given routinely to all the pregnant women and lactating mothers free of cost in all the government hospitals.[3]
Anemia in the postpartum period is also a common problem which has been subject to research.[4,5,6,7] Apart from the family health surveys,[1,2] there are two published studies which report that anemia in the postpartum period is a common problem in India.[8,9] There are no studies which quantify the associations of known clinical factors (based on review of literature) with anemia in the postpartum period.[1,2,3,4,5,6,7,8,9] Hence, this study was undertaken in a Government Referral Maternity Hospital to know the (1) severity of anemia in postpartum mothers. (2) Clinicosocial factors associated with anemia in the postpartum period. Such studies help us to better understand the problem of anemia in the postpartum period.
Materials and Methods
Background
Mangalore is a coastal border district in the state of Karnataka with a total population of about 1.8 million. The Government District Lady Goschen Hospital provides maternity services to not only the pregnant women of this district, but also to the districts of the neighboring state of Kerala. This government is affiliated to Kasturba Medical College, Mangalore.
Design
This is a retrospective record-based study of women who delivered in the Lady Goschen Hospital.
Subjects
All the women in the postpartum period whose hemoglobin (Hb%) levels were <11 g/dl were included for the study. Records which had no information no Hb% levels in the postpartum period were excluded. Similarly, records which did not have most of information were discarded.
Sample size
There is no published information about the magnitude of contribution of each of the known clinical factors.[1,2,3,4,5,6,7,8,9] Assuming that at least 28% of women will have anemia in the postpartum period, with a 95% confidence interval and absolute precision of 10% using the formula for infinite population, a sample size of 988 was obtained.
Sampling
Nonrandom sampling
Every case file was scrutinized to see if it met the study criteria. If it met the criteria, it was included. The process was repeated until the required number was reached.
Study instrument
A semi-structured proforma was devised to collect the following components of information form the records: (1) Basic sociodemographic information (such as age, occupation of the female and her spouse, education of the couple, parity, etc.). (2) Workup and problems in the antenatal period (like number of visits, investigation performed, and management in each trimester). (3) Details of the delivery (like mode of delivery, complications encountered, and management). (4) Workup and management of problems in the postpartum period.
Operational definitions
Postpartum period was taken to be 6 weeks
Hemoglobin% of 10-11 g/dl was considered as “mild”, 6-<10 g/dl “moderate” and <6 g/dl as “severe” anemia
Failure to stick with follow-up schedule as advised by the doctors was taken as noncompliance with treatment
Presentation after 28 weeks of gestation (as it is considered as the period of viability of the fetus) was considered “late”
The term “nuclear family” refers to a family of parents with their children living in house
Socioeconomic status: Was based on “Kuppuswamy Classification”.[10] This classification is commonly followed in India.
Pretesting
the proforma was pretested on few medical records to know the feasibility of use and some modifications were made to suit our purpose.
Data collection
Permission was obtained from the time bound research sub-committee to conduct the study. This study protocol was cleared by the Institutional Ethics Committee. Records at the hospitals were assessed and the information was noted down in the proforma.
Statistical analysis
The data were fed into SPSS version 15 (Chicago III, USA) and analyzed. The results are expressed in proportions in appropriate tables. Comparisons were made between “mild” and “severe” anemia. Uni- and multi-variate analysis with “severity of anemia” as the dependent variable (i.e., mild anemia vs. moderate anemia) and patient characteristics as the independent variable to get unadjusted and adjusted odds ratio with its 95% confidence intervals were carried out. P < 0.05 was considered to be significant.
Results
About 16.7% (165/988) had moderate anemia and the rest that is 83.3% (823/988) had mild anemia. None had severe anemia in the postpartum period. Breakup of proportions among moderate anemia is as follows (Hb g/dl) (%) [numerator/denominator]: 9-10 (43.2) [427/988], 8-<9 (48.8) [482/988], 7–<8 (8) [79/988].
Sociodemographic characteristics of the study population are presented in Table 1. This shows that the majority of the women belonged to nuclear families. Clinical characteristics of the study population [Table 2] show that majority that is 80.6% [796/988] of the women had anemia in the antenatal period. Majority did not return for follow-up in antenatal and postpartum periods.
Table 1.
Sociodemographic characteristics of study population
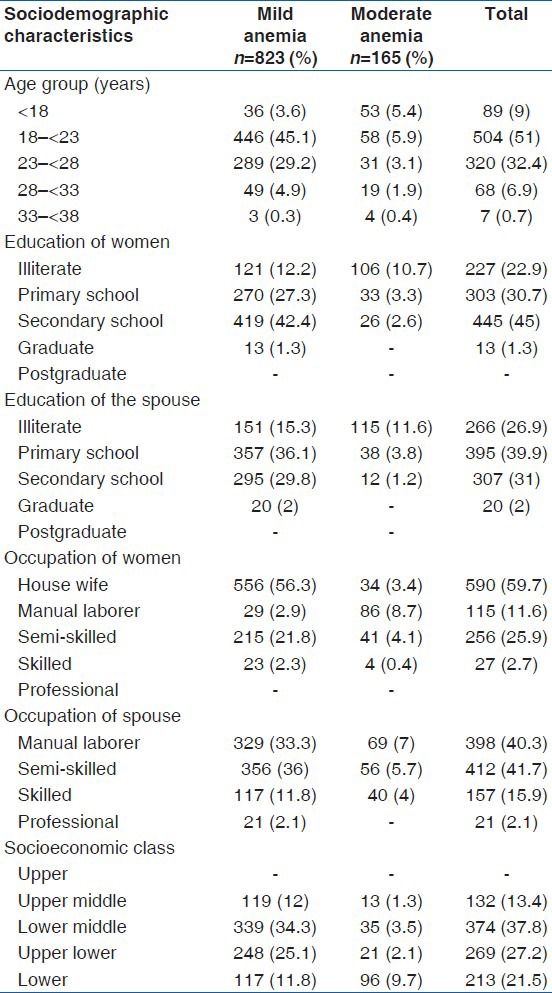
Table 2.
Comparison of antenatal characteristics according to grade of anemia
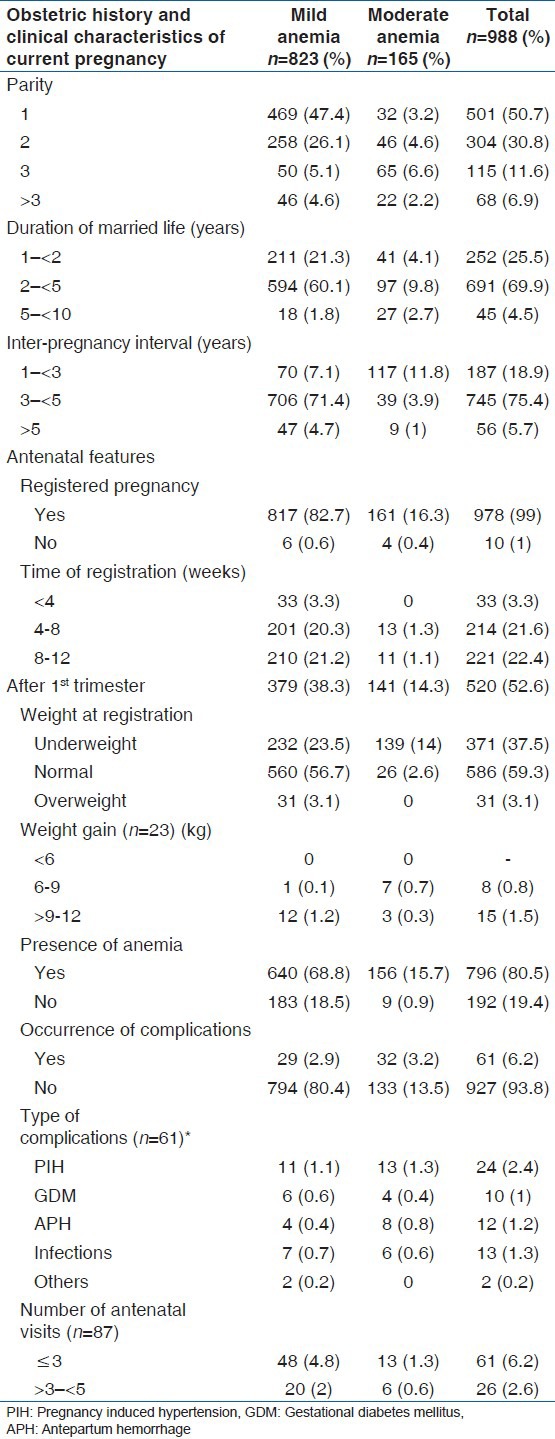
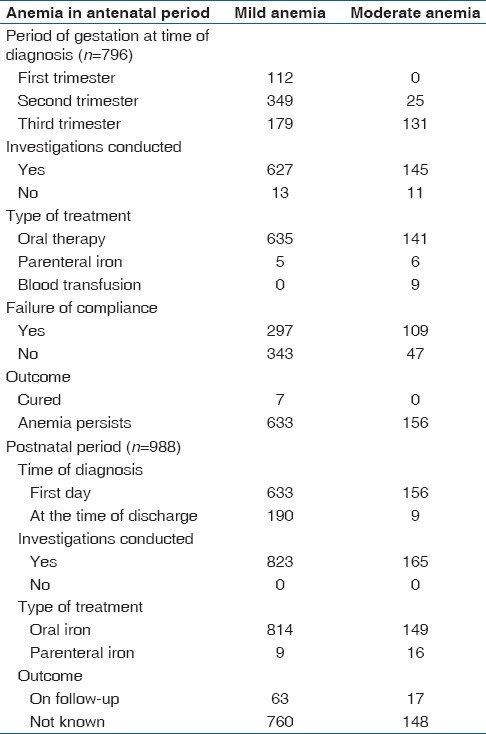
As the majority of the women had anemia in the antenatal period, which persisted into the postpartum period, they have been presented separately in Table 3. Features of anemia and its workup reveal that anemia did not get “cured in the antenatal period” and persisted into postnatal period [Table 4]. Most of them did not come for follow-up as well [Table 4].
Table 3.
Comparison of intra- and post-natal characteristics according to grade of anemia
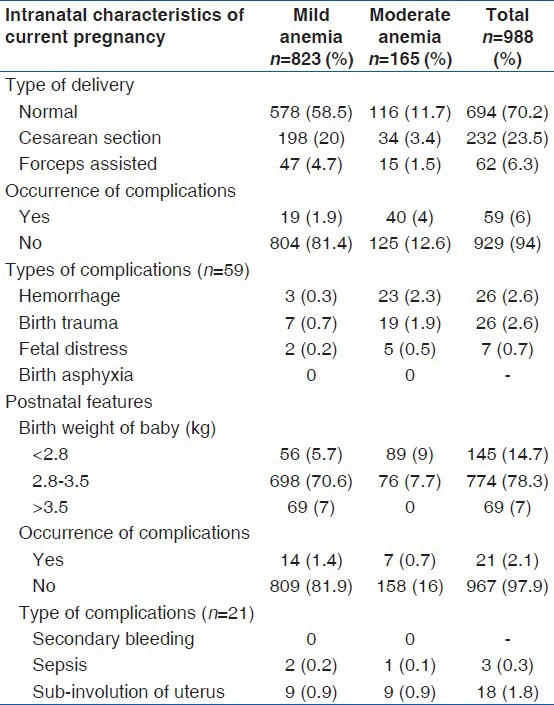
Table 4.
Features of anemia and its workup in the ante- and post-natal period
Multivariate analysis reveals that: Illiterate mothers, parity (≥3), short interpregnancy interval (<3 years), presence of anemia and its late diagnosis in the antenatal period and poor compliance with treatment were significantly independently associated with Moderate anemia in the postpartum period [Table 5].
Table 5.
Factors associated with anemia* in postpartum woman - results of uni- and multi-variate analysis
Discussion
Severity of anemia
Majority of the women had mild anemia. This is in contrast to that reported by the Nationwide Family Health Surveys (NFHS)-2 and 3 conducted in India.[1,2] Both the surveys have reported that the majority of the women had Hb levels in the range of 7-9.9 g/dl. Agarwal et al. have also reported higher prevalence (84%) of moderate anemia.[9] Our study was conducted on women in the immediate postpartum period, whereas in the national surveys[1,2] and the above-mentioned study were conducted on “postpartum” women, which included mothers up to 6 months after the delivery of the baby. Hb levels tend to fall over a period of time if the IFA tablets are not continued following the discharge of the mother from the hospital. Our records indicate the majority of the women did not turn up for the follow-up after the discharge. The differences observed between our study and the others explain the need for research that focuses on “the reasons for failure of women to come for follow-up in the postpartum period though the services are free”.
Poor treatment compliance and late diagnosis
Late diagnosis in the antenatal period and poor compliance with treatment has played a significant role in persistence of anemia in the postpartum period. This can be inferred from the inadequate number of antenatal visits considering the fact that these were cases of anemia. Both the national surveys[1,2] and Agarwal et al. have reported inadequate number of visits in the antenatal period.[9] Though IFA tablets are available free of cost in the government hospitals the women did not turn up for follow-up. Separate exploratory qualitative studies are needed to further understand the factors which influence the “health care seeking behavior” of pregnant women and lactating mothers.
Prepregnancy anemia
Short interpregnancy interval had significant independent association with anemia in the postpartum period. Some women had anemia in the first trimester. This indicates that women had “anemia” in the preconceptional period. Multiparty with short interpreganancy interval results in depletion of maternal stores of iron resulting in anemia in the preconceptional period. Contraceptive services for spacing births are available freely to couples under RCH program. Further research is needed to identify the motivating factors that play a role in adoption of contraceptive services by a married couple.
Limitations
Our study has some limitations. As the “health care seeking behavior” of the women in the postpartum period could not be studied by community-based interviews, the reasons for “failure of compliance” could not be understood. However, this study brings out future research priorities. They are the “factors,” which play a role in “persistence of anemia in postpartum mothers” and “reasons for failure to come for follow-up though the services are free.”
Conclusions
Majority had mild anemia. The following factors were found to be significantly associated with anaemia in Postnatal period: Illiterate mothers, parity (≥3), short interpregnancy interval (<3 years), presence of anemia and its late diagnosis in the antenatal period and poor compliance with treatment. However, further research is needed to better understand some of the factors like: (1) Reasons for persistence of anemia from antenatal to postpartum period. (2) Find out the reason for failure to come for follow-up in the postpartum period even though services are free.
Acknowledgments
We acknowledge the help received from the staff working in Medical Records Department of government Lady Goschen referral hospital, Mangalore.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Mumbai: International Institute of Population Sciences; 2002. National Family Health Survey– II (NFHS 2) 1998-99. [Google Scholar]
- 2.Mumbai: International Institute of Population Sciences; 2007. National Family Health Survey– III (NFHS 3) 2005-06. [Google Scholar]
- 3.Reproductive Child Health Programme, National Institute of Health and Family Welfare, Government of India. [Last accessed on 2012 July 24th]. Available from: http://www.nihfw.org/NDC/DocumentationServices/NationalHealthProgramme/REPRODUCTIVEANDCHILDHEALTH.html# .
- 4.Baker SJ, DeMaeyer EM. Nutritional anemia: Its understanding and control with special reference to the work of the World Health Organization. Am J Clin Nutr. 1979;32:368–417. doi: 10.1093/ajcn/32.2.368. [DOI] [PubMed] [Google Scholar]
- 5.Stoltzfus RJ. Iron-deficiency anemia: Reexamining the nature and magnitude of the public health problem. Summary: Implications for research and programs. J Nutr. 2001;131:697S–700S. doi: 10.1093/jn/131.2.697S. 700S. [DOI] [PubMed] [Google Scholar]
- 6.Bergmann RL, Richter R, Bergmann KE, Dudenhausen JW. Prevalence and risk factors for early postpartum anemia. Eur J Obstet Gynecol Reprod Biol. 2010;150:126–31. doi: 10.1016/j.ejogrb.2010.02.030. [DOI] [PubMed] [Google Scholar]
- 7.Sserunjogi L, Scheutz F, Whyte SR. Postnatal anaemia: Neglected problems and missed opportunities in Uganda. Health Policy Plan. 2003;18:225–31. doi: 10.1093/heapol/czg027. [DOI] [PubMed] [Google Scholar]
- 8.Somdatta P, Reddaiah VP, Singh B. Prevalence of anaemia in the postpartum period: A study of a North Indian village. Trop Doct. 2009;39:211–5. doi: 10.1258/td.2009.080347. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal KN, Agarwal DK, Sharma A, Sharma K, Prasad K, Kalita MC, et al. Prevalence of anaemia in pregnant and lactating women in India. Indian J Med Res. 2006;124:173–84. [PubMed] [Google Scholar]
- 10.Kumar N, Gupta N, Kishore J. Kuppuswamy's socioeconomic scale: Updating income ranges for the year 2012. Indian J Public Health. 2012;56:103–4. doi: 10.4103/0019-557X.96988. [DOI] [PubMed] [Google Scholar]


