Abstract
Objective:
Type 2 diabetes mellitus (DM-T2) is commonly associated with increased triglycerides (TG), low-density lipoprotein cholesterol (LDL-C) and low high-density lipoprotein cholesterol (HDL-C) levels. Fibrates like gemfibrozil are frequently used in diabetic patients to decrease TG and increase HDL-C levels. We compared the efficacy of Vitamin C, an antioxidant vitamin, with gemfibrozil on serum HDL-C in diabetic patients.
Methods:
Type 2 diabetic patients, referred to our out-patient clinic were randomly divided into three groups. After 1 month of lifestyle and diet modifications, groups A, B, and C were prescribed 1000 mg Vitamin C, 600 mg gemfibrozil and combination of both, respectively. Before the study initiation and after 6th week of drug prescription, the blood samples were taken and analyzed for total cholesterol (Total-C), HDL-C, TG, fasting blood sugar (FBS), and hemoglobin A1c (HbA1c) levels.
Findings:
Sixty-seven patients entered, and 50 patients (18 male, 32 female) finished the study. Overall, serum HDL-C increased significantly from 39.8 to 45.2 mg/dL in the participants (P = 0.001). HDL-C increased 6.3, 4.4 and 5.0 mg/dL in groups A, B and C, respectively (related significances were 0.017, 0.022 and 0.033, respectively). Significant decrease of serum TG and Total-C occurred in gemfibrozil and combination groups, but not in Vitamin C group. Changes in serum HDL-C between three groups were not significant (P = 0.963). We found a significant decrease in TG and Total-C in the groups B and C (P < 0.05), but no significant changes of TG, Total-C, LDL-C, FBS and HbA1c in group A (P > 0.05).
Conclusion:
The results demonstrated that Vitamin C may have beneficial effects on HDL-C in diabetic patients without significant effects on plasma glucose or other lipid parameters; however, its role for the treatment of low HDL-C patients should be evaluated in larger studies.
Keywords: Diabetes mellitus, Gemfibrozil, high-density lipoprotein cholesterol, Vitamin C
INTRODUCTION
Type 2 diabetes mellitus (DM-T2) is a metabolic disorder of which hyperglycemia is the hallmark; it is also characterized by abnormalities of lipid metabolism.[1,2,3,4,5,6] In addition, generation of free radicals often worsens the complications of DM such as hypertension, atherosclerosis and microcirculatory disorders.[7,8] Hypertriglyceridemia often accompanied by low high-density lipoprotein cholesterol (HDL-C) is common in DM-T2 patients that are associated with insulin resistance.[1]
Low HDL-C is an independent risk factor for atherosclerotic cardiovascular disease.[9,10] HDL-C also exhibits a number of other potentially cardio-protective properties. These include preservation of vascular endothelial function, inhibition of platelet activation, anticoagulant and profibrinolytic activities.[11] By protection of low-density lipoprotein cholesterol (LDL-C) from oxidation, HDL-associated paraoxonase antioxidant enzyme activity is also cardio-protective,[12] because it is only oxidized LDL-C that is scavenged by macrophages and incorporated to the atherosclerotic plaques.[13]
Gemfibrozil is a widely used fibric acid derivative, which its efficacy in the treatment of diabetic dyslipidemia has been well-established.[14,15,16,17] Commonly prescribed fibrates are generally well-tolerated. The most frequent side effects include upper gastrointestinal discomfort, nausea, headache, anxiety, and skin rash.[18,19] Rhabdomyolysis is an unusual, but serious adverse event in fibrate treatment.[18,19] Rhabdomyolysis can injure the skeletal muscle or myocardium and lead to renal failure, infections, disseminated intravascular coagulation, and death.[20]
Vitamin C is the major water-soluble antioxidant within the body. The vitamin readily donates electrons to break the chain reaction of lipid peroxidation. The water-soluble properties of Vitamin C allow the scavenging of free radicals before they reach the cellular membrane.[21,22,23] As Vitamin C is a water-soluble vitamin, it is usually considered a safe supplement.[24]
The role of Vitamin C on lipid profile has been conflicting in a number of studies.[12,25,26] Some researches had demonstrated the protective role of Vitamin C on HDL-C oxidation.[27] In some studies, it has been observed that Vitamin C increases serum HDL-C levels. Unlike gemfibrozil, the incremental effects of Vitamin C on serum HDL-C are reported to be free of side effects.[26,28,29,30,31] As the efficacy of Vitamin C in comparison to standard anti-hyperlipidemic drugs was unknown, the aim of this research was to compare, for the 1st time, the effects of Vitamin C, gemfibrozil and their combination on serum HDL-C in diabetic patients.
METHODS
In this prospective single blind clinical study, type 2 diabetic patients who were referred to us at Isfahan Endocrine and Metabolism Research Center of Isfahan University of Medical Sciences, Isfahan, Iran, were selected based on the following criteria: Age 30-80 years with DM-T2, hemoglobin A1c (HbA1c) <10%, normal renal and liver function, triglycerides (TG) <400 mg/dL and LDL-C <130 mg/dL. Patients with current statin, warfarin or ursodiol therapy, recent (≤4 weeks) anti-hyperlipidemic therapy, positive history of renal or gall stones, pregnancy, previous complications of gemfibrozil and those with serum TG > 400 mg/dL or LDL-C > 130 mg/dL were excluded from the study.
Two hundred and thirty-three patients were referred to our outpatient clinic. Sixty-seven patients participated in the study based on the above-mentioned criteria [Figure 1]. After an educational course of diet and lifestyle, the study design was explained, and then written consent was obtained from the participants. After 1 month of lifestyle and diet modifications, the blood samples were obtained and analyzed for HDL-C, TG, total cholesterol (Total-C), fasting blood sugar (FBS), and HbA1c. Then the patients were randomly divided into three groups. The first patient selected his group from a box of mixed letters, and the next ones regularly followed him. Groups A, B and C were prescribed 1000 mg Vitamin C, 600 mg gemfibrozil or their combination, respectively. These doses were selected based on the previous studies and are usual therapeutic doses. In each follow-up visit, we evaluated the drug side-effects and the patients’ adherence to the protocol by interview and also by counting remaining drugs. After 6th weeks the final blood samples were obtained and analyzed for the above parameters.
Figure 1.
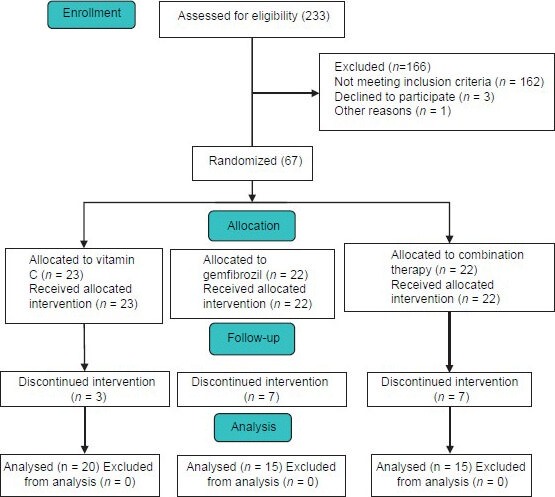
CONSORT diagram of the study
Baseline data of the participants and also changes of FBS, TG, Total-C, HDL-C, LDL-C and HbA1c were compared between groups by ANOVA. Paired t-test was used to compare these variables at two steps in each group. Nonparametric variables (like female/male ratio) were compared by appropriate statistical methods like Chi-square. Data were analyzed using SPSS software (SPSS, Inc., Chicago, IL, USA), version 16.
RESULTS
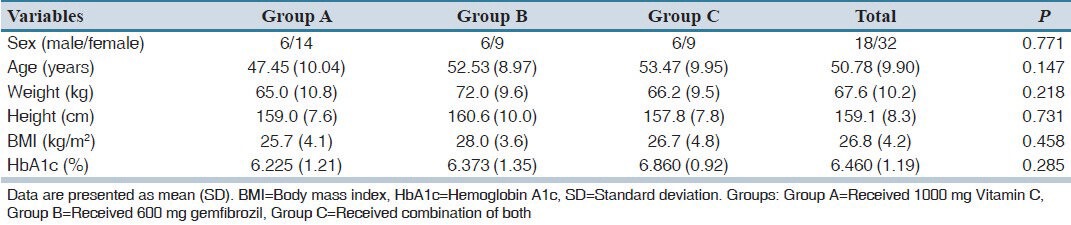
During the entrance phase of the study, 233 patients were referred to us for diabetes control. Sixty-seven participated in this study. Seventeen were excluded because of intolerance to gemfibrozil or diet incompliance. Fifty patients (18 male, 32 female) finished the study and were included in the final analysis. Baseline data of the participants are presented in Table 1. There was no statistically significant difference of the baseline data of the participants between three groups.
Table 1.
Baseline demographic and clinical data of participants
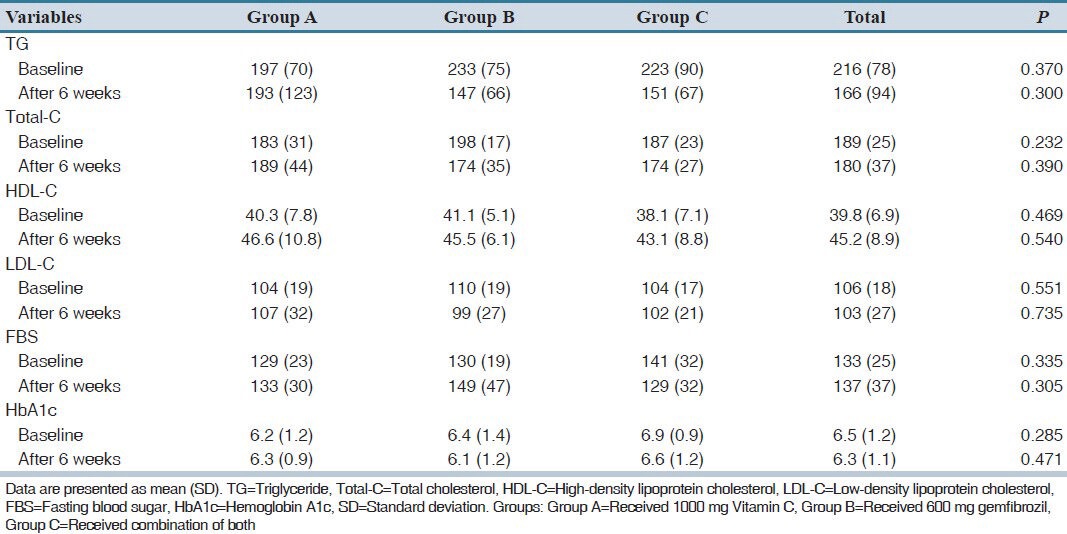
High-density lipoprotein cholesterol increased in 36 (72%) patients (80% of group A, 66.7% of group B and 66.7% of group C, P = 0.589). HDL-C increased 6.3, 4.4 and 5.0 mg/dL in groups A, B and C, respectively (related significances were 0.017, 0.022 and 0.033, respectively). Significant decrease of serum TG and Total-C occurred in gemfibrozil and combination groups, but not in Vitamin C group [Table 2].
Table 2.
Mean (SD) of measured variables before and after 6 weeks of trial
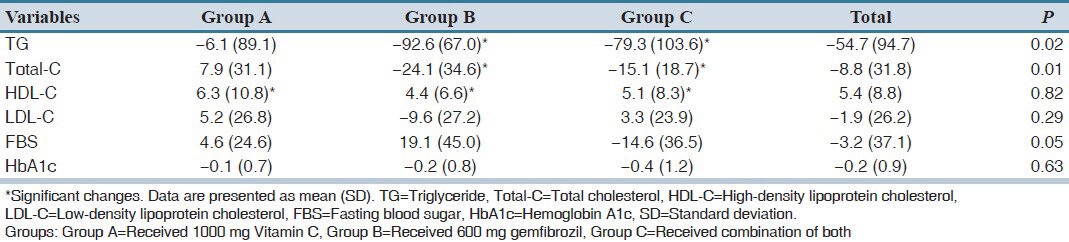
Comparison of changes of different variables between three groups using ANOVA is presented in Table 3. The change in HDL-C between the three groups was not significant (P = 0.96). Similarly, we did not observe significant differences between three groups regarding changes in LDL-C and HbA1c (P > 0.05). In contrast, the changes in serum TG and Total-C between the three groups were significant (P < 0.05). FBS increased in groups A and B, but decreased in group C (P = 0.43, 0.136 and 0.159, respectively).
Table 3.
Changes of different variables after trial in three groups
DISCUSSION
In the present study, we observed significant increase of serum HDL-C in patients who used Vitamin C, gemfibrozil or their combination by an average of 5.3 mg/dL. This amount of HDL-C increase may have clinical significance.[10]
Type 2 diabetes mellitus is commonly associated with dyslipidemia, which further increases the already elevated cardiovascular risk associated with diabetes. The classical dyslipidemia pattern in DM-T2 is increased TG, low HDL-C levels and structural changes in the LDL-C particles.[32,33] Thus, anti-hyperlipidemic treatment by drugs such as gemfibrozil is a common practice in diabetic patients with its relevant side effects.[18] Results from epidemiologic studies have demonstrated that low blood levels of HDL-C are associated with increased risk for heart disease. A substantial body of evidence from major epidemiologic studies has established that this coronary artery disease risk associated with low HDL-C is entirely independent of plasma LDL-C, other lipid parameters (TG, Total-C), and other nonlipid risk factors.[9] Epidemiologic studies have also shown that every 1-mg/dL increase in HDL-C is associated with a 2% decreased risk of coronary artery disease in men and 3% decreased risk in women.[10]
Vitamin C has also been shown to protect HDL-C from lipid oxidation during reverse cholesterol transport process.[27] Reverse cholesterol transport involves the removal of unesterified cholesterol from extrahepatic cell membranes by HDL-C particles, where it is esterified via lecithin-cholesterol acyltransferase. The cholesterol esters inside the HDL-C lipoproteins are then finally transferred back to the liver for further processing and excretion via the bile. It is known that HDL-C oxidation modifies apolipoprotein A-I structure, which alters the ability of the HDL-C lipoproteins to activate lecithin-cholesterol acyltransferase, therefore inhibiting the esterification and removal of extrahepatic cholesterol.[34,35] Vitamin C supplementation has been shown to increase apolipoprotein A-I concentrations significantly and therefore preserve the reverse cholesterol transport process.[36] On the other hand, gemfibrozil increases serum HDL by decreasing triglyceride. As the mechanisms of Vitamin C and gemfibrozil for increasing HDL are different, it is expected that their combination may have added beneficial effect, a point that was not confirmed in our study. We did not observe any significant change in TG, Total-C, LDL-C, FBS and HbA1c in the group A (P > 0.05), but TG and Total-C decreased in groups B and C (P < 0.05).
As indicated before, the role of Vitamin C on lipid profile has been conflicting in some animal and human studies. In a study by Eteng et al. on Wistar rats, the effect of oral administration of Vitamin C on serum lipids was demonstrated, but there was no effect on serum HDL-C.[37] Owu et al. observed Vitamin C significantly decreases TG, LDL-C, and Total-C but has no effect on HDL-C in diabetic rats.[38] Kim et al. reported Vitamin C has no effect on lipid profile.[39] McRae in a meta-analysis of 13 randomized controlled trials concluded supplementation with at least 500 mg/dL of Vitamin C, for a minimum of 4 weeks, can result in a significant decrease in serum LDL-C and TG concentrations. However, there was a nonsignificant elevation of serum HDL-C.[40] The important question is “why the results of these studies are so different?” One explanation can be the limitations of different studies regarding control of diet quality and quantity during participation. Even during the trial phase of one study the quality and quantity of the food does not remain constant. Another explanation is the frequent intervening factors that can affect the results.[41,41] Fixing the role of these conflicting items and controlling them are a difficult clinical practice.
Our study had some limitations: First, it included a relatively short period of 6 weeks, so the effects of long-term Vitamin C supplementation on plasma lipoproteins were not investigated. Second, the study evaluated serum HDL-C concentration, not long-term cardiovascular mortality, which could be a better clinical outcome.
We found that Vitamin C supplementation had similar incremental effects to gemfibrozil on plasma HDL-C, but adding it to gemfibrozil did not produced additional benefit. We suggest larger randomized trials for the evaluation of Vitamin C effects on long-term cardiovascular mortality and morbidity.
AUTHORS’ CONTRIBUTION
Mansour Siavash: Study idea, design and conduct, Masoud Amini: Supervisor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Betteridge DJ. Diabetic dyslipidemia. Am J Med. 1994;96:25S–31. doi: 10.1016/0002-9343(94)90228-3. [DOI] [PubMed] [Google Scholar]
- 2.Howard BV, Howard WJ. Dyslipidemia in non-insulin-dependent diabetes mellitus. Endocr Rev. 1994;15:263–74. doi: 10.1210/edrv-15-3-263. [DOI] [PubMed] [Google Scholar]
- 3.Howard BV. Lipoprotein metabolism in diabetes. Curr Opin Lipidol. 1994;5:216–20. doi: 10.1097/00041433-199405030-00009. [DOI] [PubMed] [Google Scholar]
- 4.Tomkin GH, Owens D. Insulin and lipoprotein metabolism with special reference to the diabetic state. Diabetes Metab Rev. 1994;10:225–52. doi: 10.1002/dmr.5610100303. [DOI] [PubMed] [Google Scholar]
- 5.Laakso M. Dyslipidemia, morbidity, and mortality in non-insulin-dependent diabetes mellitus. Lipoproteins and coronary heart disease in non-insulin-dependent diabetes mellitus. J Diabetes Complications. 1997;11:137–41. doi: 10.1016/s1056-8727(96)00092-x. [DOI] [PubMed] [Google Scholar]
- 6.Laakso M. Lipid disorders in type 2 diabetes. Endocrinol Nutr. 2009;56(Suppl 4):43–5. [PubMed] [Google Scholar]
- 7.Caballero AE, Arora S, Saouaf R, Lim SC, Smakowski P, Park JY, et al. Microvascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetes. Diabetes. 1999;48:1856–62. doi: 10.2337/diabetes.48.9.1856. [DOI] [PubMed] [Google Scholar]
- 8.Sowers JR, Lester MA. Diabetes and cardiovascular disease. Diabetes Care. 1999;22(Suppl 3):C14–20. [PubMed] [Google Scholar]
- 9.Franceschini G. Epidemiologic evidence for high-density lipoprotein cholesterol as a risk factor for coronary artery disease. Am J Cardiol. 2001;88(12A):9N–13. doi: 10.1016/s0002-9149(01)02146-4. [DOI] [PubMed] [Google Scholar]
- 10.Maron DJ. The epidemiology of low levels of high-density lipoprotein cholesterol in patients with and without coronary artery disease. Am J Cardiol. 2000;86:11L–14. doi: 10.1016/s0002-9149(00)01462-4. [DOI] [PubMed] [Google Scholar]
- 11.Nofer JR, Kehrel B, Fobker M, Levkau B, Assmann G, von Eckardstein A. HDL and arteriosclerosis: Beyond reverse cholesterol transport. Atherosclerosis. 2002;161:1–16. doi: 10.1016/s0021-9150(01)00651-7. [DOI] [PubMed] [Google Scholar]
- 12.Calla MS, Lynch SM. Vitamin C preserves the cardio-protective paraoxonase activity of high-density lipoprotein during oxidant stress. Arch Biochem Biophys. 2006;452:129–37. doi: 10.1016/j.abb.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 13.Kita T, Ishii K, Yokode M, Kume N, Nagano Y, Arai H, et al. The role of oxidized low density lipoprotein in the pathogenesis of atherosclerosis. Eur Heart J. 1990;11(Suppl E):122–7. doi: 10.1093/eurheartj/11.suppl_e.122. [DOI] [PubMed] [Google Scholar]
- 14.Garg A, Grundy SM. Management of dyslipidemia in NIDDM. Diabetes Care. 1990;13:153–69. doi: 10.2337/diacare.13.2.153. [DOI] [PubMed] [Google Scholar]
- 15.Garg A, Grundy SM. Gemfibrozil alone and in combination with lovastatin for treatment of hypertriglyceridemia in NIDDM. Diabetes. 1989;38:364–72. doi: 10.2337/diab.38.3.364. [DOI] [PubMed] [Google Scholar]
- 16.Tong N, Liang J. The effect of gemfibrozil on serum apo C II and C III in diabetic hyperlipidemia. Hua Xi Yi Ke Da Xue Xue Bao. 1991;22:409–11. [PubMed] [Google Scholar]
- 17.Goldberg R, La Belle P, Zupkis R, Ronca P. Comparison of the effects of lovastatin and gemfibrozil on lipids and glucose control in non-insulin-dependent diabetes mellitus. Am J Cardiol. 1990;66:16B–21. doi: 10.1016/0002-9149(90)90436-5. [DOI] [PubMed] [Google Scholar]
- 18.Davidson MH, Armani A, McKenney JM, Jacobson TA. Safety considerations with fibrate therapy. Am J Cardiol. 2007;99:3C–18. doi: 10.1016/j.amjcard.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Baer AN, Wortmann RL. Myotoxicity associated with lipid-lowering drugs. Curr Opin Rheumatol. 2007;19:67–73. doi: 10.1097/BOR.0b013e328010c559. [DOI] [PubMed] [Google Scholar]
- 20.Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553–61. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 21.Chi X, May JM. Oxidized lipoprotein induces the macrophage ascorbate transporter (SVCT2): Protection by intracellular ascorbate against oxidant stress and apoptosis. Arch Biochem Biophys. 2009;485:174–82. doi: 10.1016/j.abb.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinchuk I, Shoval H, Dotan Y, Lichtenberg D. Evaluation of antioxidants: Scope, limitations and relevance of assays. Chem Phys Lipids. 2012;165:638–47. doi: 10.1016/j.chemphyslip.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Niki E, Yamamoto Y, Komuro E, Sato K. Membrane damage due to lipid oxidation. Am J Clin Nutr. 1991;53:201S–05. doi: 10.1093/ajcn/53.1.201S. [DOI] [PubMed] [Google Scholar]
- 24.Shibuya N, Humphers JM, Agarwal MR, Jupiter DC. Efficacy and safety of high-dose vitamin C on complex regional pain syndrome in extremity trauma and surgery – Systematic review and meta-analysis. J Foot Ankle Surg. 2013;52:62–6. doi: 10.1053/j.jfas.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Aro A, Kyllästinen M, Kostiainen E, Gref CG, Elfving S, Uusitalo U. No effect on serum lipids by moderate and high doses of vitamin C in elderly subjects with low plasma ascorbic acid levels. Ann Nutr Metab. 1988;32:133–7. doi: 10.1159/000177426. [DOI] [PubMed] [Google Scholar]
- 26.Bazzarre TL, Kleiner SM, Ainsworth BE. Vitamin C intake and lipid profiles of competitive male and female bodybuilders. Int J Sport Nutr. 1992;2:260–71. doi: 10.1123/ijsn.2.3.260. [DOI] [PubMed] [Google Scholar]
- 27.Hillstrom RJ, Yacapin-Ammons AK, Lynch SM. Vitamin C inhibits lipid oxidation in human HDL. J Nutr. 2003;133:3047–51. doi: 10.1093/jn/133.10.3047. [DOI] [PubMed] [Google Scholar]
- 28.Bates CJ, Mandal AR, Cole TJ. H.D.L. cholesterol and vitamin-C status. Lancet. 1977;2:611. doi: 10.1016/s0140-6736(77)91461-1. [DOI] [PubMed] [Google Scholar]
- 29.Bates CJ, Burr MK, St Leger AS. Vitamin C, high density lipoproteins and heart disease in elderly subjects. Age Ageing. 1979;8:177–82. doi: 10.1093/ageing/8.3.177. [DOI] [PubMed] [Google Scholar]
- 30.Rezaian GR, Taheri M, Mozaffari BE, Mosleh AA, Ghalambor MA. The salutary effects of antioxidant vitamins on the plasma lipids of healthy middle aged-to-elderly individuals: A randomized, double-blind, placebo-controlled study. J Med Liban. 2002;50:10–3. [PubMed] [Google Scholar]
- 31.Yanai H, Morimoto M. Effect of ascorbate on serum lipids and urate metabolism during exhaustive training. Clin Sci (Lond) 2004;106:107–9. doi: 10.1042/CS20030266. [DOI] [PubMed] [Google Scholar]
- 32.Taskinen MR. Diabetic dyslipidemia. Atheroscler Suppl. 2002;3:47–51. doi: 10.1016/s1567-5688(01)00006-x. [DOI] [PubMed] [Google Scholar]
- 33.Taskinen MR. Pathogenesis of dyslipidemia in type 2 diabetes. Exp Clin Endocrinol Diabetes. 2001;109(Suppl 2):S180–8. doi: 10.1055/s-2001-18580. [DOI] [PubMed] [Google Scholar]
- 34.Anantharamaiah GM, Hughes TA, Iqbal M, Gawish A, Neame PJ, Medley MF, et al. Effect of oxidation on the properties of apolipoproteins A-I and A-II. J Lipid Res. 1988;29:309–18. [PubMed] [Google Scholar]
- 35.Nagano Y, Arai H, Kita T. High density lipoprotein loses its effect to stimulate efflux of cholesterol from foam cells after oxidative modification. Proc Natl Acad Sci U S A. 1991;88:6457–61. doi: 10.1073/pnas.88.15.6457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jacques PF, Sulsky SI, Perrone GE, Jenner J, Schaefer EJ. Effect of vitamin C supplementation on lipoprotein cholesterol, apolipoprotein, and triglyceride concentrations. Ann Epidemiol. 1995;5:52–9. doi: 10.1016/1047-2797(94)00041-q. [DOI] [PubMed] [Google Scholar]
- 37.Eteng MU, Ibekwe HA, Amatey TE, Bassey BJ, Uboh FU, Owu DU. Effect of vitamin C on serum lipids and electrolyte profile of albino Wistar rats. Niger J Physiol Sci. 2006;21:15–9. doi: 10.4314/njps.v21i1-2.53928. [DOI] [PubMed] [Google Scholar]
- 38.Owu DU, Antai AB, Udofia KH, Obembe AO, Obasi KO, Eteng MU. Vitamin C improves basal metabolic rate and lipid profile in alloxan-induced diabetes mellitus in rats. J Biosci. 2006;31:575–9. doi: 10.1007/BF02708409. [DOI] [PubMed] [Google Scholar]
- 39.Kim MK, Sasaki S, Sasazuki S, Okubo S, Hayashi M, Tsugane S. Long-term vitamin C supplementation has no markedly favourable effect on serum lipids in middle-aged Japanese subjects. Br J Nutr. 2004;91:81–90. doi: 10.1079/bjn20031024. [DOI] [PubMed] [Google Scholar]
- 40.McRae MP. Vitamin C supplementation lowers serum low-density lipoprotein cholesterol and triglycerides: A meta-analysis of 13 randomized controlled trials. J Chiropr Med. 2008;7:48–58. doi: 10.1016/j.jcme.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ness AR, Khaw KT, Bingham S, Day NE. Vitamin C status and serum lipids. Eur J Clin Nutr. 1996;50:724–9. [PubMed] [Google Scholar]
- 42.Slattery ML, Jacobs DR, Jr, Dyer A, Benson J, Hilner JE, Caan BJ. Dietary antioxidants and plasma lipids: The CARDIA Study. J Am Coll Nutr. 1995;14:635–42. doi: 10.1080/07315724.1995.10718553. [DOI] [PubMed] [Google Scholar]


