Abstract
Objective:
Intraoperative hypothermia is a common problem with anesthesia. Spinal anesthesia, the same as general anesthesia, affects the process of temperature regulation. The aim of this study was to compare the prophylactic effect of intravenous (IV) ondansetron with intrathecal (IT) meperidine on prevention of shivering during spinal anesthesia in patients underwent orthopedic surgery of the lower limb.
Methods:
In this study, 120 patients with American Society of Anesthesiologists physical status I to II, between the ages 16 and 65 were randomized into three groups. Group O and Group M were given IV ondansetron 8 mg and IT meperidine 0.2 mg/kg, before spinal anesthesia, respectively. Group C received IV saline 0.9%. The core and ambient temperatures, the incidence and intensity of shivering, blood pressure, heart rate, and maximum level of sensory block were recorded.
Findings:
Shivering was observed in 15%, 2.5%, and 37.5% of patients in Groups O, M, and C, respectively. There was a significant difference between Group O and M compared to Group C (P = 0.023 for Group O vs. Group C, P < 0.001 for Group M vs. Group C, P = 0.049 for Group M vs. Group O). Shivering incidence and intensity in Group M was significantly lower than Group O (P = 0.049 and P = 0.047, respectively). Twenty-two patients required additional IV meperidine among which 15 patients were from Group C (37.5%), six patients from Group O (15%) and one patient from Group M (2.5%).
Conclusion:
We concluded that IT meperidine and IV ondansetron comparably can decrease intensity and incidence of shivering compared to control group as well as decreasing the requirement to additional doses of meperidine for shivering the control without any hemodynamic side effect.
Keywords: Hypothermia, Meperidine, Ondansetron, orthopedic surgery, shivering, spinal anesthesia
INTRODUCTION
Intraoperative hypothermia is a common problem with the anesthesia practice. Regional anesthesia, like general anesthesia affects the process of temperature regulation.[1] Shivering after spinal and epidural anesthesia occurs in more than 56.7%.[2] Hypothermia during surgery can be associated with adverse clinical outcomes such as myocardial ischemia, infection, bleeding, chills,[3,4] increased oxygen consumption, and hypoxia.[5,6] Besides cardiovascular adverse effects, shivering can cause problems during surgery, and floating clots and increases postoperative bleeding.[7] Several studies have shown that local anesthesia can impair temperature regulation and prone patients to hypothermia.[8,9] Intravenous (IV) drugs for the treatment of postoperative shivering are considered as the gold standards.[10] Among opioids, meperidine is known for its ability to effectively treat and prevent shivering;[11,12] however, the IV injection of meperidine for shivering can cause side effects such as hemodynamic changes,[7] respiratory depression, nausea, vomiting, pruritus, sedation, hypotension, bradycardia, and bronchospasm. Chen et al. reported that low-dose intrathecal (IT) meperidine decreases anesthesia-associated shivering in the nonpregnant population.[2] In another study, Roy et al. showed that administering 0.2 mg/kg of IT meperidine decreases incidence and severity of shivering during IT anesthesia for cesarean section, with minimal adverse effects.[10] In the other study, Davoudi et al. showed that adding 15 mg meperidine to the IT anesthesia for transurethral resection of the prostate (TURP) surgery reduces the incidence of shivering without increasing side effects.[7] In a few studies, to avoid postanesthetic shivering (PAS) in patients undergoing general anesthesia, the researchers used ondansetron. Ondansetron is a 5-HT3 antagonist which usually recommended for prevention and treatment of nausea and vomiting during and after surgery. The mechanism of 5-HT3 antagonists in the regulation of body temperature has not been clarified, but it may be related to the inhibition of serotonin uptake on the preoptic anterior hypothalamus region.[5] In a study conducted by Powell and Buggy, it was shown that IV administration of 4-8 mg ondansetron prevented shivering during anesthesia without significant hemodynamic changes.[13] The incidence and severity of shivering during and after the operation are dependent to the type of surgery, maximal height of sensory block after spinal anesthesia, duration of surgery, and postoperative pain severity. The lower extremity orthopedic surgeries are different from TURP and cesarean section surgeries with respect to these variables. In the other hand, no study was conducted to compare IV ondansetron with IT meperidine in relation to shivering during IT anesthesia. Hence, the present study was designed to compare the prophylactic effect of these two drugs on the prevention of shivering during spinal anesthesia in patients underwent orthopedic surgery of the lower limb.
METHODS
After obtaining institutional approval from Ethics Committee of the Isfahan University of Medical Sciences, and written informed consent from all patients, 120 patients with American Society of Anesthesiologists physical status I to II, between the ages 16 and 65 who were scheduled for elective orthopedic surgery of lower organs under spinal anesthesia in Kashani Hospital, Isfahan, Iran (2011-2012) were enrolled in this double-blind randomized clinical trial. Patients with body mass index lower than 30, without preoperative fever (T < 38°C), and some other clinical conditions such as hypo or hyperthyroidism, Parkinson disease, Raynaud's syndrome, dysautonomia, who are not requiring blood transfusion during surgery or not receiving vasodilators or medications likely to alter thermoregulation were entered the study. Patients for whom anesthesia technique was changed or were died before the study completion or their surgery was cancelled were excluded from the study. On arrival to the operating room, all patients had IV line and 10 ml/kg/h Lactate Ringer's solution warmed to 37°C was infused (over) 30 min before spinal anesthesia. Then the infusion rate was reduced to 2 ml/kg/h at the same temperature. Syringes were provided in the equal volumes and the same shapes by an anesthesiologist who was blinded to data collection. Before spinal anesthesia, patients were divided into three groups by a computer-generated randomization method: Group O receiving 8 mg IV ondansetron before spinal anesthesia; Group M receiving 0.2 mg/kg IT meperidine in addition to bupivacaine; Group C receiving saline 0.9% before spinal anesthesia. Studied drugs were administered to patients by an anesthesiologist blinded to data collection. Supplemental oxygen (5 L/min) was delivered via facemask during operation. Spinal anesthesia was performed with a 22-guage spinal needle in L3-L4 interspace in sitting position and hyperbaric bupivacaine 0.5% was injected. Shivering was evaluated after the injection completion of the subarachnoid drug, and maximum spinal sensory block level was investigated by pinprick. Systolic and diastolic blood pressures, also mean arterial pressure, heart rate, and peripheral oxygen saturation percentage were measured and recorded before and 5, 15, 30 min after spinal anesthesia induction. More than 20% decrease in systolic blood pressure was treated by crystalloid infusion, if necessary ephedrine 5 mg was administered intravenously. The ambient temperature was measured by an accurate thermometer and maintained at 21–22°C with constant humidity. Core temperature was measured by a tympanic thermometer. Skin temperature was measured and recorded by an axillary thermometer in the axillary region. The core and skin temperatures were evaluated and recorded 3 min before spinal anesthesia and then at 20-min intervals during spinal anesthesia. Shivering incidence was also evaluated and recorded in the same times. All patients were covered with a cloth over the chest, thighs and calf during surgery and one laminated linen over the whole body postoperatively (after operation). No other warming device was used. Shivering was evaluated during and after operation (during the intraoperative and postoperative periods) by observing pectoralis major muscles for fasciculation longer than 10 s and was noted by a blinded observer. Shivering was graded with a defined scale by Crossley and Mahajan[14] including: (0)-no shivering, (I)-piloerection or peripheral vasoconstriction but no visible shivering, (II)-muscular activity observed only in one muscle group, (III)-muscular activity observed in more than one muscle group without generalized shivering, and (IV)-all body shivering. If the patients had shivering with grade ≥2, 0.3 mg/kg IV meperidine was administered. The number of patients who needed the additional meperidine were recorded. Furthermore, the additional dosages of meperidine were calculated. Nausea, vomiting, and itching were noted as drugs side effects. Promethazine 25 mg was infused within 15 min for itching treatment. Nausea and vomiting was also managed by 10 mg metoclopramide injection.
Required sample size was evaluated using a sample size evaluation formula in order to compare following ratios and by considering confidence level 95%, test power 80%, postoperative shivering incidence 50% for patients not receiving any drug and 30% effect of ondansetron for shivering reduction (from 50% to 20%) for 40 patients in every group. Quantity variables like additional dosages of meperidine administered were analyzed by one-way analysis of variances (ANOVA). Shapiro–Wilk test was used for evaluating the normality of variables’ distribution. Quality variables like number of patients who needed additional meperidine were analyzed by Chi-square (if necessary by Fisher exact test) and Mann-Whitney tests. The Kruskal-Wallis test was used to determine if there are statistically significant differences between two or more groups of independent or ordinal dependent (such as shivering intensity) variables. Repeated quantity variables were analyzed by repeated measurement ANOVA test. Values (data) were given at mean ± standard deviation or frequency (percentage). P < 0.05 was considered significant.
RESULTS
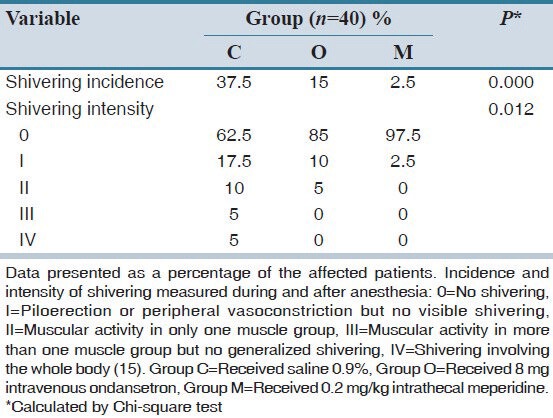
The present study was performed on 120 patients. Related flow diagram is shown in Figure 1. Demographic data, surgery duration, type of surgery, and maximum level of sensory blockade are given in Table 1. Data of all variables were normally distributed according to the results of Shapiro-Wilk test. This table shows there were no significant differences between groups (P > 0.05). The mean core and skin temperatures were measured before and during spinal anesthesia and are shown in Table 2. There were not observed any significant difference between groups in this regard (P > 0.05). Systolic, diastolic, and mean arterial pressures, and heart rate were somehow similar in all groups with no significant difference (P > 0.05). Oxygen saturation percentage for no patient was lower than 90% during the study, and no clear difference was observed between groups. Intensity and incidence of shivering are shown in Table 3. The incidence of shivering was significantly lower in Group O compared to Group C (P = 0.023). Shivering incidence in Group M was significantly lower compared to the control group (P < 0.001). Shivering incidence in Group M was lower than Group O with a clear statistical difference (P = 0.049). Shivering intensity in Groups O and M were significantly lower than Group C (P = 0.016 and P < 0.001, respectively). Shivering intensity in Group M was lower than Group O, and there was a clear statistical difference in this regard (P = 0.047). In the present study, 15 patients required ephedrine for hypotension among which nine patients were from Group C (22.5%), three patients from Group O (7.5%) and three patients from Group M (7.5%) and no significant difference was observed between groups (P > 0.05). Bradycardia was observed in three patients from Group C and O and was not seen in Group M. In these three patients, it was treated by atropine (2.5% in one patient from Group C and 5% in two patients from Group O). There was a significant difference between Groups O and C regarding the administration of atropine (P < 0.001). Nausea, vomiting, and itching were not seen in any patient. Twenty-two patients required additional IV meperidine among which 15 patients were from Group C (37.5%), six patients from Group O (15%), and one patient from Group M (2.5%) [Table 1]. There was a significant difference between Groups O and M with Group C (P < 0.001 for Group O vs. Group C; P < 0.001 for Group M vs. Group C), while no significant differences were seen between Group M and Group O regarding administering the additional meperidine (P = 0.061).
Figure 1.
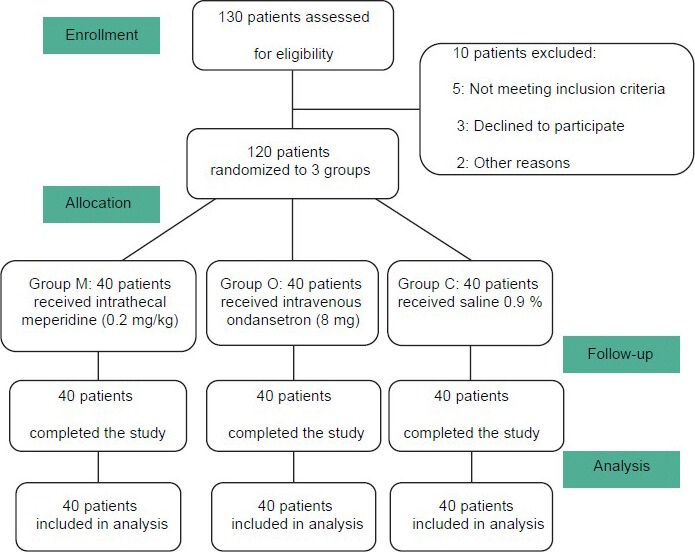
CONSORT diagram of the study
Table 1.
Demographic characteristics and paraclinical data of the studied patients
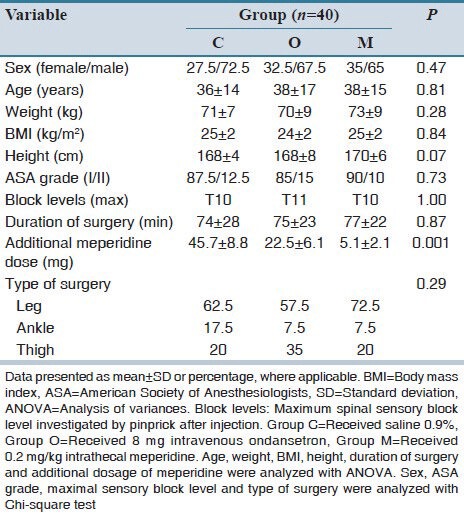
Table 2.
Core temperature and axillary temperature measured during anesthesia
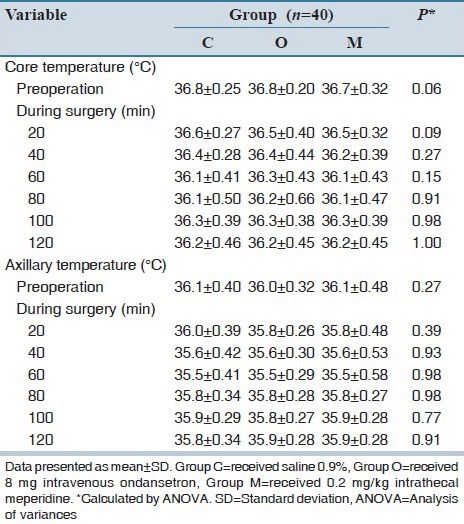
Table 3.
Incidence and intensity of shivering in all treatment groups
DISCUSSION
We found that core temperature during the intraoperative phase after spinal anesthesia was similar in Groups O and M, and both groups were similar to that seen in Group C. Furthermore, there was no clear difference for mean skin temperature in the three groups. We observed that incidence and intensity of shivering as the main outcome was the highest in the placebo group while IV ondansetron and IT meperidine significantly prevented it with the lowest incidence and intensity following IT meperidine. Requirement to the additional meperidine was higher in the patients in Group C (n = 15) compared to Groups O (n = 6) and M (n = 1); while in Group M it was lower than Group O. In the present study, bradycardia was not observed for patients in Group M in comparison with Groups O and C and patients of this group did not need Atropine. There was no significant difference between three groups in demographic data, surgery duration, maximum sensory blockade, and kind of surgery. No patient in three groups had shown side effects such as nausea, vomiting, and itching.
Shivering is a current and usual problem after surgery under spinal anesthesia. Exact mechanism of the shivering in spinal anesthesia has not been investigated and published comprehensively. There are some hypotheses in this respect:[15,16] (1) Heat is transferred from the core to peripheral parts in general anesthesia. (2) Any contraction of vessels for thermoregulation under blockade level reduces skin heat. (3) There are some characters regulating temperature that cause hypothermia by vessels contraction reduction and sweat threshold increase.[10] IV drugs are the gold standard treatment for postoperative shivering. IV meperidine and ondansetrone can decrease intensity and incidence of shivering after spinal anesthesia. Meperidine as a unique drug usually has been applied between 0.5 and 1.8 mg/kg for spinal anesthesia[17,18] and has caused many side effects including nausea, vomiting, itching, sleepiness, hypotension, bronchospasm, bradycardia, and breathing depression,[17,19] all related to the drug dose.[20] After IT administration of 50 mg meperidine for 70-year-old patient in bladder surgery by lithotomy position, transient neurologic signs were observed.[21] Furthermore, breathing depression of opioids has been reported in very high doses (50 mg) of IT meperidine.[22] According to previous studies, IV meperidine for shivering removing has shown these side effects and other problems of opioids. But IT meperidine in a lower dose compared to IV one can decrease intensity and incidence of shivering and does not cause these side effects.[2,23] In this study, like the study of Davoudi et al.[7] found that IT meperidine did not have any side effect. Kelsaka et al. concluded that IV ondansetron (8 mg) and meperidine (0.4 mg/kg) had similar anti-shivering effects;[1] however, in the present study, IT meperidine (0.2 mg/kg) could reduce intensity and incidence of shivering and requirement to an additional dose of meperidine without any hemodynamic side effect, compared to IV ondansetron. Also, Roy et al. explained that although shivering was a common problem after spinal anesthesia, IT meperidine was able to decrease intensity and incidence of shivering without changing the level of motor and sensory blockade.[10] Based on Roy study, using IT meperidine had two advantages:[10] (1) As a preventive therapy, patients have not experienced discomfort and adverse effects associated with shivering. (2) IV meperidine for women in the painless cesarean section could have unwanted and undesired side effects. Meperidine is composed of k- and μ-receptor agonist. In comparison with μ-opioid agonists such as fentanyl, sufentanil, and morphine, IV meperidine is very more effective for shivering treatment.[24] Meperidine effect on shivering is related to non-μ-opioid receptors and more to k-receptors. Because meperidine has activity in k-receptors, correlation between anti-shivering effect of meperidine, and agonist activity of k-receptor has been suggested in many studies.[24,25,26] It can be said that anti-shivering effects of meperidine in spinal anesthesia are resulted by its systemic absorption. It has been shown that the anti-shivering effects of IV meperidine are seen in 0.6 and 1.8 μg/ml of plasma concentration,[27] while plasma level of meperidine 400-700 ng/ml is related to its analgesic effects.[20] In contrast, after 1 mg/kg IT meperidine injection, its level in plasma has been 107 ± 20 ng/ml[20] which is 5 times more than amounts used in our study. In the present study, it seems that anti-shivering effects were impossible to be caused by systemic absorption of IT meperidine. In a few studies, 5-HT3 antagonists have been used for PAS in patients undergoing general anesthesia. The mechanism of these drugs in the regulation of body temperature has not been clarified but may be related to the inhibition of serotonin uptake on the preoptic anterior hypothalamus region.[5] 5-HT3 receptors may control both pathways of heat production and loss. Injection of these drugs into the preoptic hypothalamus in cat resulted in vasodilatation.[28] Ondansetron as an exclusive 5-HT3 antagonist is widely used due to its anti-vomiting effects. Powell and Buggy[13] shown that 8 mg ondansetron was more effective than 4 mg ondansetron for PAS in patients receiving general anesthesia and did not alter the hemodynamic profile of patients. In the present study, IV ondansetron and IT meperidine were administrations only in a single dose and were not repeated. Other dosages of IT meperidine were not investigated. The present study has not been performed in the epidural meperidine injection yet. Furthermore, more researches are needed for studying the effects of spinal administration of meperidine.
The present study has shown that both IT meperidine 0.2 mg/kg and IV ondansetron 8 mg can decrease intensity and incidence of shivering compared to control group and also a requirement to additional dose of meperidine for shivering control without any homodynamic side effect.
AUTHORS’ CONTRIBUTION
MRS has planned the study and finalized it; AH and MN have planned the study and finalized it too; MRS and AH did the evaluation statistical analysis and prepared the first version of the article. All authors read and approved the article.
Footnotes
Source of Support: Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Kelsaka E, Baris S, Karakaya D, Sarihasan B. Comparison of ondansetron and meperidine for prevention of shivering in patients undergoing spinal anesthesia. Reg Anesth Pain Med. 2006;31:40–5. doi: 10.1016/j.rapm.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Chen JC, Hsu SW, Hu LH, Hong YJ, Tsai PS, Lin TC, et al. Intrathecal meperidine attenuates shivering induced by spinal anesthesia. Ma Zui Xue Za Zhi. 1993;31:19–24. [PubMed] [Google Scholar]
- 3.Frank SM, Beattie C, Christopherson R, Norris EJ, Perler BA, Williams GM, et al. Unintentional hypothermia is associated with postoperative myocardial ischemia. The Perioperative Ischemia Randomized Anesthesia Trial Study Group. Anesthesiology. 1993;78:468–76. doi: 10.1097/00000542-199303000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- 5.Alfonsi P. Postanaesthetic shivering: Epidemiology, pathophysiology, and approaches to prevention and management. Drugs. 2001;61:2193–205. doi: 10.2165/00003495-200161150-00004. [DOI] [PubMed] [Google Scholar]
- 6.De Witte J, Sessler DI. Perioperative shivering: Physiology and pharmacology. Anesthesiology. 2002;96:467–84. doi: 10.1097/00000542-200202000-00036. [DOI] [PubMed] [Google Scholar]
- 7.Davoudi M, Mousavi-Bahar SH, Farhanchi A. Intrathecal meperidine for prevention of shivering during transurethral resection of prostate. Urol J. 2007;4:212–6. [PubMed] [Google Scholar]
- 8.Leslie K, Sessler DI. Reduction in the shivering threshold is proportional to spinal block height. Anesthesiology. 1996;84:1327–31. doi: 10.1097/00000542-199606000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Matsukawa T, Sessler DI, Sessler AM, Schroeder M, Ozaki M, Kurz A, et al. Heat flow and distribution during induction of general anesthesia. Anesthesiology. 1995;82:662–73. doi: 10.1097/00000542-199503000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Roy JD, Girard M, Drolet P. Intrathecal meperidine decreases shivering during cesarean delivery under spinal anesthesia. Anesth Analg. 2004;98:230–4. doi: 10.1213/01.ANE.0000093251.42341.74. [DOI] [PubMed] [Google Scholar]
- 11.Alfonsi P, Hongnat JM, Lebrault C, Chauvin M. The effects of pethidine, fentanyl and lignocaine on postanaesthetic shivering. Anaesthesia. 1995;50:214–7. doi: 10.1111/j.1365-2044.1995.tb04559.x. [DOI] [PubMed] [Google Scholar]
- 12.Monsó A, Riudeubas J, Barbal F, Laporte JR, Arnau JM. A randomized, double-blind, placebo-controlled trial comparing pethidine to metamizol for treatment of post-anaesthetic shivering. Br J Clin Pharmacol. 1996;42:307–11. doi: 10.1046/j.1365-2125.1996.04124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powell RM, Buggy DJ. Ondansetron given before induction of anesthesia reduces shivering after general anesthesia. Anesth Analg. 2000;90:1423–7. doi: 10.1097/00000539-200006000-00032. [DOI] [PubMed] [Google Scholar]
- 14.Crossley AW, Mahajan RP. The intensity of postoperative shivering is unrelated to axillary temperature. Anaesthesia. 1994;49:205–7. doi: 10.1111/j.1365-2044.1994.tb03422.x. [DOI] [PubMed] [Google Scholar]
- 15.Matsukawa T, Sessler DI, Christensen R, Ozaki M, Schroeder M. Heat flow and distribution during epidural anesthesia. Anesthesiology. 1995;83:961–7. doi: 10.1097/00000542-199511000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Ozaki M, Kurz A, Sessler DI, Lenhardt R, Schroeder M, Moayeri A, et al. Thermoregulatory thresholds during epidural and spinal anesthesia. Anesthesiology. 1994;81:282–8. doi: 10.1097/00000542-199408000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Patel D, Janardhan Y, Merai B, Robalino J, Shevde K. Comparison of intrathecal meperidine and lidocaine in endoscopic urological procedures. Can J Anaesth. 1990;37:567–70. doi: 10.1007/BF03006327. [DOI] [PubMed] [Google Scholar]
- 18.Hansen D, Hansen S. The effects of three graded doses of meperidine for spinal anesthesia in African men. Anesth Analg. 1999;88:827–30. doi: 10.1097/00000539-199904000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Sangarlangkarn S, Klaewtanong V, Jonglerttrakool P, Khankaew V. Meperidine as a spinal anesthetic agent: A comparison with lidocaine-glucose. Anesth Analg. 1987;66:235–40. [PubMed] [Google Scholar]
- 20.Tauzin-Fin P, Maurette P, Vincon G, Hecquet D, Houdek MC, Bonnet F. Clinical and pharmacokinetic aspects of the combination of meperidine and prilocaine for spinal anaesthesia. Can J Anaesth. 1992;39:655–60. doi: 10.1007/BF03008225. [DOI] [PubMed] [Google Scholar]
- 21.Lewis WR, Perrino AC., Jr Transient neurological symptoms after subarachnoid meperidine. Anesth Analg. 2002;94:213–4. doi: 10.1097/00000539-200201000-00041. [DOI] [PubMed] [Google Scholar]
- 22.Ong B, Segstro R. Respiratory depression associated with meperidine spinal anaesthesia. Can J Anaesth. 1994;41:725–7. doi: 10.1007/BF03015628. [DOI] [PubMed] [Google Scholar]
- 23.Kranke P, Eberhart LH, Roewer N, Tramèr MR. Pharmacological treatment of postoperative shivering: A quantitative systematic review of randomized controlled trials. Anesth Analg. 2002;94:453–60. doi: 10.1097/00000539-200202000-00043. [DOI] [PubMed] [Google Scholar]
- 24.Pauca AL, Savage RT, Simpson S, Roy RC. Effect of pethidine, fentanyl and morphine on post-operative shivering in man. Acta Anaesthesiol Scand. 1984;28:138–43. doi: 10.1111/j.1399-6576.1984.tb02029.x. [DOI] [PubMed] [Google Scholar]
- 25.Kurz M, Belani KG, Sessler DI, Kurz A, Larson MD, Schroeder M, et al. Naloxone, meperidine, and shivering. Anesthesiology. 1993;79:1193–201. doi: 10.1097/00000542-199312000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Wang JJ, Ho ST, Lee SC, Liu YC. A comparison among nalbuphine, meperidine, and placebo for treating postanesthetic shivering. Anesth Analg. 1999;88:686–9. doi: 10.1097/00000539-199903000-00041. [DOI] [PubMed] [Google Scholar]
- 27.Kurz A, Ikeda T, Sessler DI, Larson MD, Bjorksten AR, Dechert M, et al. Meperidine decreases the shivering threshold twice as much as the vasoconstriction threshold. Anesthesiology. 1997;86:1046–54. doi: 10.1097/00000542-199705000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Komiskey HL, Rudy TA. Serotonergic influences on brain stem thermoregulatory mechanisms in the cat. Brain Res. 1977;134:297–315. doi: 10.1016/0006-8993(77)91075-7. [DOI] [PubMed] [Google Scholar]


