Abstract
HIV is a public health crisis that disproportionately affects Black and Latino men. To understand this crisis, syndemic theory, which takes into account multiple interrelated epidemics, should be used. A syndemic is “two or more afflictions, interacting synergistically, contributing to excess burden of disease in a population.” Vulnerability to HIV among Black and Latino men is increased as structural, social, and biological factors interact in the context of social marginalization. In New York City, Black and Latino men experience a syndemic of HIV/AIDS, substance abuse, trauma, incarceration, and poverty; however, current research has yet to fully identify the mechanisms of resilience that may reduce the negative impact of a syndemic or explore the potential adaptive functions of individual-level risk behaviors. To understand HIV risk as part of a syndemic and address HIV prevention in Black and Latino men, we propose the following: (1) the use of complex systems analysis, ethnography, and other mixed-methods approaches to observe changes in relations among social conditions and disease; (2) multidisciplinary and inter-institution collaboration; and (3) involvement of public health practitioners and researchers from diverse and underrepresented backgrounds.
Keywords: Syndemics, Blacks, Latinos, Men, HIV/AIDS
HIV is a public health crisis among Black and Latino men in the USA, notably those living in New York City (NYC). The difficulty in reducing HIV disparities among Black and Latino men is heightened by the interaction of multiple epidemics, including substance abuse, trauma, incarceration, poverty, and HIV/AIDS, within the Black and Latino communities. The complex nature of these factors highlights the necessity of developing novel research approaches to better understand how multiple epidemics interact within marginalized communities.
The HIV/AIDS Epidemic among Black and Latino Men in New York City
Black and Latino men’s increased vulnerability to HIV is exemplified by recent epidemiological data. The Centers for Disease Control and Prevention indicate that in 2009, men accounted for the majority (77 %) of new HIV diagnoses in the USA, with Black and Latino men disproportionately impacted.1 That same year, HIV incidence among Black and Latino men was 6.5 and 2.5 times greater, respectively, than it was among White men.1 In large cities across the USA, including NYC, HIV prevalence among men of color rivals prevalence in countries in sub-Saharan Africa with generalized HIV epidemics.2
In 2010, New York City had one of the highest HIV/AIDS case rates in the USA, with 1.4 % of the population in NYC living with HIV/AIDS.3 In 2008, NYC had more than three times the national average HIV/AIDS prevalence rate.4 The epidemic is particularly pronounced among Black or Latino men and men who have sex with men (MSM). There have been recent upticks in infections among MSM, and in 2010, 48.3 % of new diagnoses in NYC were among MSM,3 an increase of 4.4 % from the previous year.5
Of all MSM in NYC diagnosed with HIV, 66 % were Black or Latino.6 Overall, Blacks and Latinos accounted for 78.6 % of new HIV diagnoses in NYC in 2010.3 Additionally, among people diagnosed with HIV in NYC in 2010, 22.7 % of Black men and 21.1 % of Latino men had concurrent AIDS diagnoses,3 which result in shorter survival rates.7 Death rates among Blacks and Hispanics living with HIV/AIDS in NYC were 4 and 2.5 times that of Whites, respectively.3
Excluding the neighborhood of Chelsea-Clinton, the highest rates of infection are found in the poorest neighborhoods in NYC, which are primarily inhabited by Blacks and Latinos (Northern Manhattan, the South Bronx, and Central Brooklyn).3 In 2010, HIV prevalence in these ethnic enclaves was up to two times higher than the overall NYC prevalence,3 and these neighborhoods accounted for over three-quarters of new HIV diagnoses in NYC in 2007.8 Additionally, in 2010, these neighborhoods displayed age-adjusted death rates up to one and a half times higher than Lower Manhattan.3
The Need for a Novel Approach to Understanding HIV among Black and Latino Men
Why are HIV and AIDS disproportionately affecting Black and Latino men in NYC? Answering this question requires going beyond behavioral and biomedical approaches that assess individual-level risk factors and treat diseases and their causes as distinct from other conditions.9–11 To fully understand the problem of HIV among Black and Latino men in NYC, we must comprehensively describe how structural, social, behavioral, and biological factors operate in a dynamic fashion to create a context in which Black and Latino men are particularly vulnerable to acquiring HIV.
The urgency of reducing HIV risk among Black and Latino men necessitates the implementation of new research paradigms that are culturally relevant and have the potential to produce efficacious interventions in the communities most affected by HIV/AIDS. This research should apply novel theories that understand vulnerability for diseases such as HIV as emerging from multiple variables at different levels of analysis.9,10,12 This approach contrasts with static approaches to exploring HIV risk, which have frequently been used in public health research and focus heavily on explaining how one factor or group of factors (examined at one level of analysis) is related to risk for a single disease or pathology. Because the USA has set its sights on reducing HIV/AIDS disparities,13,14 it is imperative that public health researchers use a robust set of theories and methodologies to provide a comprehensive explanation of why and how HIV disparities exist in the USA and to implement effective multi-level interventions. By developing interventions that account for multiple interacting factors within a given community, it is more likely that these interventions will be tailored to the specific needs of community members.
Syndemic Theory and its Application to Understanding HIV among Black and Latino Men
Syndemic theory may be the theoretical framework best suited to explain high rates of HIV/AIDS among Black and Latino men in NYC, because it takes into account multiple interrelated systems that contribute to heightened vulnerability to HIV/AIDS within marginalized communities. A syndemic is defined as “two or more afflictions, interacting synergistically, contributing to excess burden of disease in a population.”15 In syndemic theory, individual epidemics are “sustained in a community/population because of harmful social conditions and injurious social connections”.16 Therefore, syndemics include epidemics both of disease and the social conditions that contribute to the proliferation of disease. Thus, epidemic must be understood in both physiological (i.e., disease) and psycho-sociological (i.e., behavioral, social, and structural) terms.16–19 The emphasis on the role of social and cultural forces in producing epidemics is one detail of syndemic theory that sets it apart from similar concepts that address the interactive effects of disease, such as “interacting epidemics” (e.g., HIV/AIDS and tuberculosis), “co-morbid conditions” (e.g., depression and substance use), and clusters of health-related crises.
The anthropologist Merrill Singer was the first researcher to identify and report on a syndemic in the public health research literature. He highlighted the role of the substance abuse, violence, and AIDS (SAVA) syndemic in driving heightened vulnerability to diminished health outcomes among the poor in the northeastern USA.20 Singer noted that components of the SAVA syndemic reinforced one another and were inextricably bound to one another, such that the successful decrease of one epidemic (e.g., AIDS), would require decreases of other epidemics (e.g., substance abuse and violence).
More recently, syndemic theory has been utilized by Ron Stall and his colleagues to describe vulnerability to poor health outcomes among MSM and to inform the development of interventions targeting this population.21–24 For example, one study found that in a sample of almost 3,000 MSM (21 % ethnic/racial minorities), polydrug use, depression, childhood sexual abuse, and intimate partner violence were each related to one another and independently associated with HIV seropositivity and high-risk sexual behavior.21 Moreover, these psychosocial risks were observed to have an additive effect on HIV risks: with increasing numbers of risks, there were increases in the prevalence of high-risk sex and HIV infection. The researchers attributed this phenomenon to the presence of a syndemic. Subsequent work by Stall and colleagues identified other psychosocial risks contributing to syndemic conditions, including sexual compulsiveness, stress, and discrimination.23,24
Perry Halkitis and his colleagues25 also have employed syndemic theory to understand vulnerability to poor health outcomes among young MSM. Data were collected from 598 young (between the ages of 18 and 19 years) MSM living in NYC, the majority of whom (53 %) were Hispanic or Black. In this study, multiple indices of mental health burden (i.e., suicidal thoughts, depressive symptoms, loneliness, PTSD) and drug use were used to create a measurement model; results from a confirmatory factor analysis showed that this model was related to unprotected sex and highlighted the importance of examining the combined effects of psychosocial stressors on risk behavior.
Taken together, studies have suggested that in order to effectively reduce HIV among MSM, interventions need to address the multitude of syndemic factors that affect different populations of MSM. These include social factors, such as forms of marginalization, which may contribute to excess disease burden among Black and Latino men compared to other populations.26 We argue that the syndemic framework identified by Singer and employed by Stall, Halkitis, and others is an important conceptual tool that public health practitioners should draw upon to study the interaction of HIV/AIDS, substance abuse, trauma, incarceration, and poverty among Black and Latino men in New York City. We also provide direction on how syndemic theory may be integrated into research and intervention paradigms.
The Syndemic of HIV/AIDS, Substance Abuse, Trauma, Incarceration and Poverty Affecting Black and Latino Men
The crisis of HIV/AIDS currently affecting Black and Latino men is shaped by epidemics of substance abuse, trauma, incarceration, and poverty. These epidemics of disease and social conditions interact and propagate in a synergistic fashion; however, understanding the dynamic nature of these epidemics first requires considering their individual contributions to poor health outcomes among Black and Latino men.
Substance Abuse
Just as epidemiological data highlight the disproportionate numbers of Black and Latino men in NYC living with HIV/AIDS, studies also show that compared to other groups Black and Latino men exhibit an enhanced vulnerability to substance use disorders. Racial and ethnic disparities among drug users are profound despite lifetime substance use being similar or lower in Blacks compared to Whites.27,28 Black and Latino drug users, notably those living in poverty, are more likely to initiate injection drug use during adolescence, experience drug addiction and dependency for longer periods of time, and relapse after treatment compared to White drug users.29–31 Moreover, Blacks and Latinos who exhibit substance use disorders (often with co-occurring mental health disorders) experience less access to care and a lower rate of active treatment relative to substance-abusing Whites.32
Trauma
Numerous studies have also documented high rates of trauma (i.e., exposure to physical and sexual abuse) among Black and Latino men. Seminal work conducted by Doll and colleagues33 in the early 1990s found that Black and Latino gay and bisexual men were significantly more likely than White gay and bisexual men to report having had sexual contact with an older partner during childhood. The investigators found that 52 % of Black men and 50 % of Latino men reported abuse, while 32 % of White men reported abuse. Further evidence for the high levels of trauma experienced by members of this population can be seen in data suggesting that in inner-city neighborhoods (which are predominantly populated by Blacks and Latinos) one third of pre-teen and teenaged youth have been personally victimized, while almost all youth have been exposed to community violence.34 Traumatic experiences that occur early in the lives of Black and Latino men are likely to continue in adulthood. These experiences often lead to an increased likelihood of participating in violence and being incarcerated.35,36
Incarceration
Indeed, incarceration represents a serious issue in Black and Latino communities. As noted by Golembeski and Fullilove: “Nationally, 50 % of all prison inmates are Black and 17 % are Hispanic, proportions that differ significantly from their proportions within the general population” (p. 1702).37 The authors noted that among men aged 25–29, 1 in every 8 Black men and 1 in every 27 Latino men was in prison in 2003, compared to 1 in every 63 White men. Mass incarceration has been shown to be related to increased poverty and unemployment,9,38 experiences of violence and trauma,38 unprotected sex,39 and the disruption of existing sexual networks leading to increased HIV risk.9 In addition, offenders who are imprisoned experience high rates of recidivism compared to those who are put on probation. This disparity is exacerbated for those who were convicted of drug crimes, pointing to the role of incarceration on drug offences and substance use.40
Poverty
Poverty is an additional problem disproportionately affecting Blacks and Latinos. The 2010 census showed that between 2009 and 2010, the poverty rate increased from 25.8 to 27.4 among Blacks and from 25.3 to 26.6 among Hispanics.41 Similarly, Black and Latino workers are disproportionately impacted by joblessness and underemployment. Reports show that in May 2012 unemployment among Blacks and Latinos was at 13.6 % and 11 %, respectively, whereas the national average hovered around 8.2 %.42 A more recent report from the Pew Research Center showed that in July 2013 the unemployment rate was 12.6 % for Blacks while it was 6.6 % for Whites.43 Poverty may contribute to increased vulnerability to HIV through a lack of health resources and an increased need to engage in sex work44; poverty is also associated with substance use, neighborhood violence and trauma, and incarceration,9 making it part of a complex web of health risks to which Black and Latino men are exposed.
Examining the epidemics of HIV/AIDS, substance abuse, trauma, incarceration, and poverty among Black and Latino men in isolation from one another will not fully explicate heightened vulnerability for poor health outcomes, notably HIV and AIDS, within this population. Findings show that factors individually related to HIV risk may also have complex relations with other variables. For example, research studies suggest that the high likelihood of living in impoverished neighborhoods mediates the relationship between minority race and the increased likelihood of using/injecting drugs.35,45–49 Furthermore, studies have shown that experiences of trauma, incarceration, and living in poverty each contribute to Black and Latino men’s increased likelihood of being infected with HIV.35,50–54 This demonstrates the importance of examining how the epidemics of substance abuse, trauma, incarceration, and poverty interact and overlap in a dynamic fashion to increase HIV vulnerability among Black and Latino men in NYC.
Racism and the Historical Underpinnings of the Syndemic Affecting Black and Latino Men
In order to comprehensively describe and intervene upon the syndemic affecting Black and Latino men, it is important to understand the social context out of which the syndemic emerges. The life experiences of Black and Latino men are shaped by the legacy of racism in the USA.55 Experiences of racism are related to health risk through a variety of physiological, psychosocial, and behavioral mediators.56,57
Studies conducted with Latino and Black men in the USA have shown that experiencing discrimination is associated with poor mental health,52,58,59 sexual risk behavior,60 and increased substance use.61 MSM of color, who are most at risk for contracting HIV, also experience the interactive effects of racism and homophobia.62 Diaz, Ayala, and Bein’s study on 912 Latino gay men living in three US cities showed high rates of racial discrimination in the gay community; furthermore, experiencing race-based sexual objectification and racial discomfort in gay venues was related to sexual risk behavior.58 No studies have further documented the synergistic ways in which discrimination based on race and sexual identity/behavior affect health among MSM of color, although available research shows that racism and homophobia are independently correlated with HIV risk among Latino MSM.58,60
Racism may also contribute to negative outcomes by fueling the social context that drives the syndemic of HIV/AIDS, substance use, trauma, incarceration, and poverty impacting Black and Latino men. The marginalization of Black and Latino men in the USA stems from a complex web of historical events, politics, and belief systems.63 There are many institutional and cultural practices shaped by the USA’s history of racism that perpetuate the marginalization of Black and Latino men and have been associated with other factors that serve to enhance the poor social conditions that make Black and Latino men disproportionately vulnerable to poverty, violence, incarceration, and trauma compared to other populations. Moreover, historical and contemporary racism and other forms of stigma reinforce societal notions that the negative outcomes experienced by Black and Latino men are a consequence of personal choices and individual deficits, thereby limiting social and political capital to effectively intervene to change social conditions.55,64
The criminal justice system and residential segregation are two examples of systems that contribute to the continued marginalization of Black and Latino men and fuel the syndemic of poverty, violence, incarceration, trauma, and HIV/AIDS that impacts these men. With regard to the criminal justice system, Black and Latino men in the USA are more likely to be excluded from jury panels,65 receive harsher sentences, and face the negative consequences of drug policy, compared to White Americans.66,67 The Harrison Act, the Rockefeller Drug Laws, Reagan’s proclaimed “War on Drugs,” and New York City’s “Stop and Frisk” program are examples of legislative acts that have led to an increase in Black and Latino men being searched, detained, and imprisoned at disproportionate rates compared to other populations.66–68 Moreover, these policies have led to an epidemic of mass incarceration among men of color, resulting in increased poverty and conflict and violence in minority communities.37,38 This clearly highlights the potential role of the criminal justice system in enhancing syndemic conditions affecting Black and Latino men.
Like the criminal justice system, residential segregation has been shown to negatively affect minority communities and contribute to the syndemic affecting Black and Latino men. Efforts to separate minority communities from White communities started with slavery and Jim Crow laws, and many factors, such as discriminatory housing practices, have been implicated in the creation and continued existence of contemporary urban ghettos and resource-poor areas populated by minorities.69 Residential segregation has been shown to be associated with poverty, lack of educational and job opportunities, lack of health resources, poor housing quality, environmental health stressors, violence, and substance use.69–71 A 2005 study showed that living in a city with a higher index of black isolation was significantly related to poor self-reported health among Black adults; White adults did not show significant health differences when living in cities with a higher index of white or black isolation, pointing to the disproportionate negative effects of segregation on the health of minority individuals.72 Segregation also intensifies and concentrates the effects of mass incarceration in minority neighborhoods; this is especially true of the poorest Black neighborhoods in New York City.38 Thus, residential segregation may be one aspect of social context that increases the prevalence of poverty, trauma, and violence in minority communities in NYC.38,70
Addressing Gaps in Syndemic Theory
While Syndemic Theory represents an ideal framework through which to explore the co-occurring epidemics of HIV/AIDS, substance abuse, trauma, incarceration, and poverty affecting Black and Latino men, there are two important gaps in the theory that should be addressed. One limitation of the theory is that it lacks explicit reference to the potential adaptive functions of individual-level risk behaviors such as substance use and sexual risk taking. A second limitation is that syndemic theory does not explicitly account for mechanisms of resilience that may reduce the impact of a syndemic has on an individual or population.
For many Black and Latino men, substance use and sexual risk behavior may serve as a method for coping with the very social conditions that in part constitute the syndemic (such as poverty or incarceration). For example, substance use and sexual risk taking behaviors among MSM have been described as potentially serving adaptive functions through promoting cognitive escape.73,74 Many MSM must cope with structural and interpersonal stressors tied to their ethnic and sexual identities,75,76 and engaging in risk behaviors such as substance use and unprotected sex may represent one way MSM cope with being marginalized and/or victimized. For example, a series of studies exploring mental health and HIV risk among Latino MSM found that exposure to homophobia and racism were independently related to higher levels of psychological distress and unprotected anal intercourse among Latino gay men.52,58 These studies and others suggest a dynamic process in which individual-level risk behaviors that result from syndemic conditions may in turn increase vulnerability to the syndemic.
In addition to considering the adaptive functions of risk behaviors, it is also important to understand how protective factors may reduce the impact of a syndemic on an affected population. Protective factors exist at the same levels as risk factors—there are personal, social, and structural protective factors that may help to explain how a syndemic fails to develop in particular communities or affect specific individuals. Even more importantly, these factors represent targets for interventions that aim to prevent and eradicate syndemics. Psychological resilience is an important personal factor that can serve to protect Black and Latino MSM from the negative health outcomes associated with a syndemic. Resilience has been operationalized in terms of psychological assets including self-efficacy, empowerment, and adaptive coping.77–79 The concept of resilience is complementary to syndemic theory in that it suggests positive adaptation to social and environmental stressors. Syndemic conditions constitute an environment that could threaten the health and well-being of Black and Latino men; the extent to which these men are able to emerge from these environments as healthy and disease-free may be a function of individual-level resilience.
Protective factors like resilience that may mitigate the impact of a syndemic do not only exist at the individual level, however. There are several community, institutional, and structural factors that may reduce Black and Latino men’s vulnerability to poor health outcomes and exposure to the syndemic of HIV/AIDS, substance abuse, trauma, incarceration, and poverty. For example, the interrelated concepts of social capital, community mobilization, and neighborhood cohesion each are social factors that may be protective against the development and maintenance of a syndemic. Studies have documented associations between social capital and neighborhood cohesion (measured at the community level) and an assortment of health outcomes in population-based samples,80–82 providing strong evidence for the health-promoting features of these factors. Moreover, research examining responses to the HIV/AIDS epidemic in the USA and abroad suggests that community mobilization has played a critical role to population-level changes in health behavior and susceptibility to infection.83,84 Thus, social capital, community mobilization, and neighborhood cohesion are important social factors to consider as protective and potentially operating to reduce the impact of a syndemic. These factors may help to explain the social conditions that need to be in place to avoid the emergence of a syndemic.
Lastly, structural factors may be protective and help to mitigate the underlying epidemic fueling a syndemic. Social welfare programs that promote health/medical, educational, housing, and financial resources can help to address some historical and structural factors that have created and enhanced existing health disparities. As we describe in the following sections, policies that aim to increase racial/ethnic and sexual diversity in health research, practice and advocacy can allow for more robust responses to reducing syndemic conditions affecting Black and Latino men in New York City. In sum, it is critical to understand that personal, social, and structural factors each function in such a way that they support the creation and propagation of a syndemic, but each set of factors can also function in such a way that they reduce syndemic conditions via protective effects at each level.
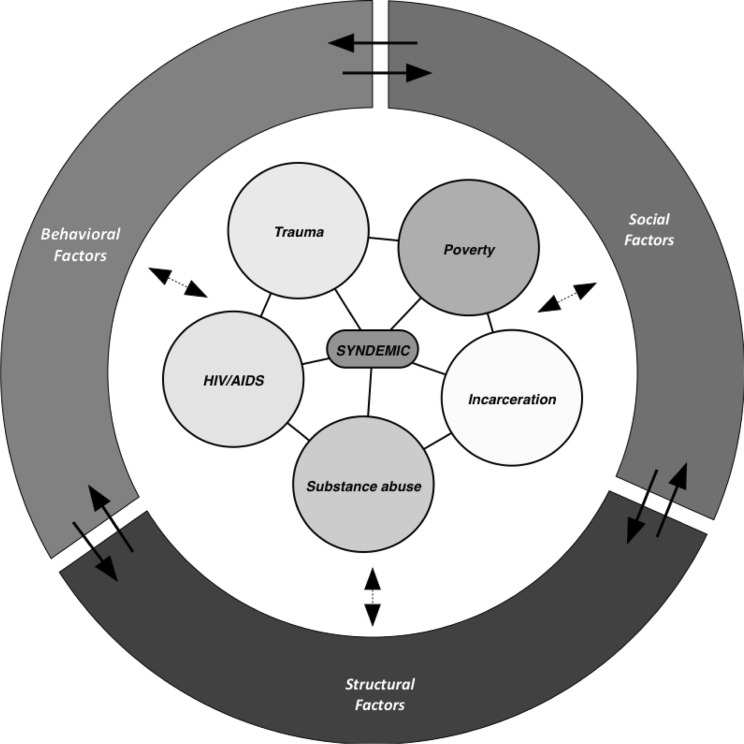
Figure 1 provides a conceptual model to highlight the key components of the syndemic affecting Black and Latino men in NYC. The separate epidemics of HIV/AIDS, substance abuse, trauma, incarcerations, and poverty are shown to be interconnected and comprising a syndemic. Surrounding the syndemic are behavioral, social, and structural factors, each of which influence and are influenced by the others. Lastly, these behavioral, social, and structural factors can both enhance and hinder vulnerability to the syndemic as risk and resilience factors, respectively. The double-headed arrows connecting these three sets of factors to the syndemic denote the dual functions of these factors.
FIG. 1.
Conceptual model of the syndemic affecting Black and Latino men in New York City.
Approaches to Exploring and Responding to a Syndemic
Effectively studying how a syndemic operates requires taking methodological approaches that allow for the simultaneous exploration of diseases and the social conditions out of which they emerge.10 Some public health researchers spend years focused on a particular disease outcome, pouring over variables and data points until they believe they understand the etiology of the pathology. However, compartmentalizing research endeavors will not allow the scientific community to properly measure the role that context plays in research participants’ lives. Implementing research and programs to reduce the syndemic affecting Black and Latino men can be challenging, and researchers and practitioners should consider how individual-level motivation to adopt health protective behaviors is linked to structural violence, systemic racism, heterosexism, and a variety of other extra individual-level factors.15,85–88 These factors are not easily measured or observed; nonetheless, they contribute to the syndemic of HIV/AIDS, substance abuse, trauma, incarceration, and poverty that impacts Black and Latino men in NYC. Consequently, to better identify and understand these interacting factors, a variety of approaches tailored for use in syndemics research should be utilized.
One such methodological approach is complex systems analysis, a promising theoretical tool for observing and explaining syndemics. This approach involves understanding a system as consisting of elements (i.e., sociological and physiological problems), interconnections (i.e., relationships that hold elements together, such policies/laws, social network configurations, and individual-level risk-reduction practices), and functions (i.e. the true purpose that the system has, which is not always apparent; it may include increasing the health of one group at the expense of another or reproducing social inequalities that increase racial/ethnic minority groups’ likelihood of experiencing negative health outcomes).89 The defining feature of complex systems analysis is that the dynamic of a social context, which includes elements, interconnections, and purposes, perpetuates a syndemic.12
In addition to complex systems analysis, ethnographic approaches can be useful in exploring syndemics.17,90 Ethnography, which is a primarily descriptive and inductive research method, provides descriptions of the multitude of factors that work in concert to shape social contexts. These social contexts can create environments that heighten risk for syndemics in certain populations.91,92 Singer and colleagues90 used ethnography to explore the SAVA syndemic among the urban poor and, more recently, to examine the high rates of STIs among Black and Puerto Rican adolescents in Hartford, CT, highlighting the appropriateness for ethnographic research in studying HIV risk.
Furthermore, researchers should utilize other multidisciplinary, mixed-methods research strategies that allow for the analysis of multiple interrelated factors.17,26 For example, large-scale longitudinal studies that aim to document and tie together patterns in diseases and social conditions among individuals within a specific community are appropriate for future research endeavors. Public health research that integrates prevention and treatment of disease, substance use, and mental illness may also contribute to understanding and reducing risk and vulnerability.
Efforts to address syndemic conditions will also be enhanced through the formation of interdisciplinary and multidisciplinary research teams composed of public health practitioners, physicians, nurses, epidemiologists, mental health professionals, behavioral scientists, and other community experts. These stakeholders have varied areas of expertise that allow for the examination of factors spanning disciplines and multiple levels of analysis. The importance of diverse collaborations is noted by Mays, Cochran, and Zamudio,93 who suggest including political organizations, justice systems, faith-based organizations, and other community-based organizations in efforts to address social conditions that promote vulnerability to HIV and other poor outcomes.
Although many fields could benefit from multi- and interdisciplinary research teams, the specific and unique emphasis that syndemic theory places on the role of cultural marginalization in driving complex interactions suggests researchers and practitioners carefully consider the ways in which cultural forces act upon not only the communities impacted by a syndemic, but also the course of the research and intervention. The subjective cultural experiences of researchers, practitioners, and community members can shape how social factors are explored and interpreted. The role of personal insight in understanding nuances of culture and marginalization can be of great benefit if active efforts are taken to use diverse collaborative teams and reflexive research methods that foster a productive dialogue.94,95 For example, contributions from researchers with experience working and living within communities affected by syndemics may allow for an enhanced understanding of the functioning of a syndemic within a particular community. An important approach that the scientific and public health communities should continue to take to explain and reduce the impact of a syndemic affecting marginalized groups is to increase the number of public health researchers from diverse backgrounds, including ethnic/racial minority and socially marginalized communities, who are trained and funded to conduct disparities research.96–98 Stoff et al.99 provide key rationale for increasing ethnic and racial diversity among HIV/AIDS researchers in the USA. They note that (1) the needs of racially/ethnically marginalized groups can be better met with an ethnically diverse research workforce; (2) a broadening of the US research agenda on racial disparities in HIV/AIDS in the USA can be achieved with a more diverse HIV/AIDS workforce; (3) more culturally appropriate health care can be provided to ethnic and racial minority populations with increased diversity among HIV/AIDS researchers; and (4) increased access to health care and HIV/AIDS treatment among ethnic and racial minorities can be achieved with greater diversity among HIV/AIDS researchers and practitioners. Overall, there is strong support for the idea that increasing diversity among researchers and practitioners will improve not just the ability to understand the syndemic of HIV/AIDS, substance use, trauma, incarceration, and poverty affecting Black and Latino men, but also the chances of implementing programs and policies that can mitigate the impact of and ultimately eradicate the syndemic.
We propose that the application of syndemic theory, using the approaches described previously, provides assurances that we have accounted for the issues raised in these important questions. Comprehensively examining physical and social contexts and the syndemics that emerge out of these contexts is one attempt at moving closer to a truly scientific understanding of how health disparities develop and proliferate.
The paradigm outlined in this article provides a novel approach to examining HIV and other health disparities among Black and Latino men in NYC; clinical, community, and policy interventions developed considering this paradigm may have a better chance of improving health outcomes and overall well-being among Black and Latino men in NYC.
Acknowledgments
This research was supported by the US Centers for Disease Control and Prevention (U01 PS000700—Minority HIV/AIDS Research Initiative). The authors thank Madeline Sutton, MD, MPH, Dawn Smith, MD, MPH, Leigh Willis, PhD, MPH, and Ted Castellanos, MPH for the commitment to and support of this research.
References
- 1.Prejean J, Song R, Hernandez R, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.El-Sadr W, Mayer K, Hodder S. AIDS in America—forgotten but not gone. N Engl J Med. 2010;362:967–70. doi: 10.1056/NEJMp1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.HIV Epidemiology and Field Services Program, New York City Department of Health and Mental Hygiene. New York City HIV/AIDS annual surveillance statistics 2010. http://www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2010-tables-all.pdf. 2010. Updated 2012. Accessed June 2012.
- 4.Centers for Disease Control and Prevention. HIV surveillance—United States, 1981–2008. Morbidity and Mortality Weekly Report (MMWR). 2011;60;21:689–683. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6021a2.htm. Accessed June 27, 2012. [PubMed]
- 5.HIV Epidemiology and Field Services Program, New York City Department of Health and Mental Hygiene. New York City HIV/AIDS annual surveillance statistics 2009. http://www.nyc.gov/html/doh/downloads/pdf/ah/surveillance2009-tables-all.pdf. 2012. Accessed July 27, 2012.
- 6.Department of Health and Mental Hygiene. Unprotected anal intercourse among Young Men who Have Sex with Men (MSM) in New York City. Epi Data Brief. 2012;13. http://www.nyc.gov/html/doh/downloads/pdf/epi/databrief13.pdf. Accessed August 9, 2013.
- 7.Grigoryan A, Hall HI, Durant T, Wei X. Late HIV diagnosis and determinants of progression to AIDS or death after HIV diagnosis among injection drug users, 33 US states, 1996–2004. PLoS ONE. 2009;4(2):e4445. doi: 10.1371/journal.pone.0004445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.New York City HIV/AIDS Surveillance Slide Sets. New York: New York City Department of Health and Mental Hygiene, 2007. Updated November 2007. Accessed February 19, 2010 at http://www.nyc.gov/html/doh/html/dires/epi_surveillance.shtml.
- 9.Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(Suppl 1):S115–22. doi: 10.1086/425280. [DOI] [PubMed] [Google Scholar]
- 10.Galea S, Hall C, Kaplan GA. Social epidemiology and complex system dynamic modeling as applied to health behavior and drug use research. Int J Drug Policy. 2009;20:209–16. doi: 10.1016/j.drugpo.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health. 2009;96:452–8. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hawe P, Shiell A, Riley T. Theorising interventions as events in systems. Am J Community Psychol. 2009;43:267–76. doi: 10.1007/s10464-009-9229-9. [DOI] [PubMed] [Google Scholar]
- 13.White House, The. The Agenda-Civil Rights. Available at: http://www.whitehouse.gov/issues/civil-rights. 2009. Accessed February 25, 2010.
- 14.White House, The. The Agenda-Additional Issues. Available at: http://www.whitehouse.gov/issues/additional-issues. 2009. Accessed on February 25, 2010.
- 15.Syndemics Prevention Network, CDC. Syndemics Overview. http://www.cdc.gov/syndemics/overview.htm. Updated January 30, 2008. Accessed February 25, 2010.
- 16.Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17:423–41. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- 17.Singer MC, Erickson PI, Badiane L, et al. Syndemics, sex and the city: understanding sexually transmitted diseases in social and cultural context. Soc Sci Med. 2006;63:2010–21. doi: 10.1016/j.socscimed.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallace R. Urban desertification, public health and public order: planned shrinkage, violent death, substance abuse and AIDS in the Bronx. Soc Sci Med. 1990;31:801–13. doi: 10.1016/0277-9536(90)90175-R. [DOI] [PubMed] [Google Scholar]
- 19.Wallace D, Wallace R. A Plague on your houses: how New York was burned down and national public health crumbled. New York, NY: Verso; 1998. [Google Scholar]
- 20.Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq Creativ Sociol. 1996;24(2):99–110. [Google Scholar]
- 21.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42. doi: 10.2105/AJPH.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stall R, Friedman MS, Catania J. Interacting epidemics and gay men’s health: a theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: health disparities affecting gay and bisexual men in the United States. Oxford, IN: Oxford University Press; 2007. [Google Scholar]
- 23.Guadamuz T, Friedman M, Marshal M, Herrik A, Lim SH, Wei C, et al. Health, sexual health, and syndemics: toward a better approach to STI and HIV prevention interventions for men who have sex with men (MSM) in the United States. In: Aral S, Fenton J, Lipshuz FJ, et al., editors. The new public health and STD/HIV prevention: personal, public and health systems approaches. New York, NY: Springer Sciences and Business Media; 2013. [Google Scholar]
- 24.Penniman DT, Shoptaw S, Guadamuz TE, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012 doi: 10.1007/s11524-012-9674-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Halkitis PN, Moeller RW, Siconolfi DE, Storholm ED, Solomon TM, Bub KL. Measurement model exploring a syndemic in emerging adult gay and bisexual men. AIDS Behav. 2013;17(2):662–73. doi: 10.1007/s10461-012-0273-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halkitis PN, Wolitski RJ, Millett GA. A holistic approach to addressing HIV infection disparities in gay, bisexual, and other men who have sex with men. Am Psychol. 2013;68(4):261. doi: 10.1037/a0032746. [DOI] [PubMed] [Google Scholar]
- 27.Des Jarlais DC, Arasteh K, Hagan H, McKnight C, Perlman D, Friedman S. Persistence and change in disparities in HIV infection among injection drug users in New York City after large-scale syringe exchange programs. AJPH. 2009;99:S445–51. doi: 10.2105/AJPH.2008.159327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des JD. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. JAIDS. 2002;30:95–104. doi: 10.1097/00042560-200205010-00013. [DOI] [PubMed] [Google Scholar]
- 29.Broz D, Ouellet LJ. Racial and ethnic changes in heroin injection in the United States: implications for the HIV/AIDS epidemic. Drug Alcohol Depend. 2008;94:221–33. doi: 10.1016/j.drugalcdep.2007.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention . Drug-associated HIV transmission continues in the United States. Atlanta, GA: CDC DHHS; 2002. [Google Scholar]
- 31.Fuller CM, Borrell LN, Latkin CA, Galea S, Ompad DC, Strathdee SA, et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. AJPH. 2005;95:689–95. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. Am J Psychiatry. 2001;158:2027–32. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 33.Doll LS, Joy D, Bartholow BN, et al. Self-reported childhood and adolescent sexual abuse among adult homosexual and bisexual men. Child Abuse Negl. 1992;16:855–64. doi: 10.1016/0145-2134(92)90087-8. [DOI] [PubMed] [Google Scholar]
- 34.Margolin G, Gordis EB. The effects of family and community violence on children. Anny Rev Psychol. 2000;51:445–79. doi: 10.1146/annurev.psych.51.1.445. [DOI] [PubMed] [Google Scholar]
- 35.Morton L. MSM, the streets, and lockdown: sexual threat and social dominance in America. J Afr Am Stud. 2007;11:225–38. doi: 10.1007/s12111-007-9024-3. [DOI] [Google Scholar]
- 36.Williams JK, Wyatt GE, Resell J, Peterson J, Asuan-O’Brien A. Psychosocial issues among gay- and non-gay-identifying HIV-seropositive African American and Latino MSM. Cultur Divers Ethnic Minor Psychol. 2004;10:268–86. doi: 10.1037/1099-9809.10.3.268. [DOI] [PubMed] [Google Scholar]
- 37.Golembeski C, Fullilove R. Criminal (in)justice in the city and its associated health consequences. Am J Public Health. 2004;95:1701–6. doi: 10.2105/AJPH.2005.063768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts DE. Social and moral cost of mass incarceration in African American communities. Stan L Rev. 2003;56:1271. [Google Scholar]
- 39.Jones KT, Johnson WD, Wheeler DP, Gray P, Foust E, Gaiter J. Nonsupportive peer norms and incarceration as HIV risk correlates for young black men who have sex with men. AIDS Behav. 2008;12(1):41–50. doi: 10.1007/s10461-007-9228-5. [DOI] [PubMed] [Google Scholar]
- 40.Spohn C, Holleran D. The effect of imprisonment on recidivism rates of felony offenders: a focus on drug offenders*. Criminology. 2002;40(2):329–58. doi: 10.1111/j.1745-9125.2002.tb00959.x. [DOI] [Google Scholar]
- 41.DeNavas-Walt C, Proctor BD, Smith JC, U.S. Census Bureau. Income, poverty, and health insurance coverage in the United States: 2010. Current Population Reports. 2011:60–239. http://www.census.gov/prod/2011pubs/p60-239.pdf. Accessed June 27, 2011.
- 42.Bureau of Labor Statistics. Employment situation summary. 2012. http://www.bls.gov/news.release/empsit.nr0.htm. Accessed July 27, 2012.
- 43.DeSilver D. Black unemployment rate is consistently twice that of whites. Pew Research Center:http://www.pewresearch.org/fact-tank/2013/08/21/through-good-times-and-bad-black-unemployment-is-consistently-double-that-of-whites. 2013. Accessed 27 July 2012.
- 44.Marín BV. HIV prevention in the Hispanic community: sex, culture, and empowerment. J Transcult Nurs. 2003;14(3):186–92. doi: 10.1177/1043659603014003005. [DOI] [PubMed] [Google Scholar]
- 45.Lillie-Blanton M, Anthony JC, Schuster CR. Probing the meaning of racial/ethnic group comparisons in crack cocaine smoking. JAMA. 1993;269(8):993–7. doi: 10.1001/jama.1993.03500080041029. [DOI] [PubMed] [Google Scholar]
- 46.Ellickson P, Morton S. Identifying adolescents at risk for hard drug use: racial/ethnic variations. J Adolesc Health. 1999;25:382–95. doi: 10.1016/S1054-139X(98)00144-X. [DOI] [PubMed] [Google Scholar]
- 47.Fuller CM, Vlahov D, Arria AM, Ompad DC, Garfein R, Strathdee SA. Factors associated with adolescent initiation of injection drug use. Public Health Rep. 2001;116(suppl 1):136–45. doi: 10.1093/phr/116.S1.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fuller CM, Vlahov D, Ompad DC, Shah N, Arria A, Strathdee SA. High-risk behaviors associated with transition from illicit non-injection to injection drug use among adolescent and young adult drug users: a case-control study. Drug Alcohol Depend. 2002;66:189–98. doi: 10.1016/S0376-8716(01)00200-9. [DOI] [PubMed] [Google Scholar]
- 49.Golub A, Johnson BD. Variation in youthful risks of progression from alcohol and tobacco to marijuana and to hard drugs across generations. Am J Public Health. 2001;91:225–32. doi: 10.2105/AJPH.91.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bartholow B, Dan D, Lynda S, et al. Emotional, behavioral, and HIV risks associated with sexual abuse among adult homosexual and bisexual men. Child Abuse Negl. 1994;18:745–61. doi: 10.1016/0145-2134(94)00042-5. [DOI] [PubMed] [Google Scholar]
- 51.Carballo-Diéguez A, Dolezal C. Association between history of childhood sexual abuse and adult HIV-risk sexual behavior in Puerto Rican men who have sex with men. Child Abuse Negl. 1995;19:595–605. doi: 10.1016/0145-2134(95)00018-4. [DOI] [PubMed] [Google Scholar]
- 52.Diaz RM, Ayala G, Bein E, Henne J, Marin BV. The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: findings from 3 US cities. Am J Public Health. 2001;91:927–32. doi: 10.2105/AJPH.91.6.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117(Suppl 1):S135. [PMC free article] [PubMed] [Google Scholar]
- 54.Singer M. AIDS and the health crisis of the US urban poor: the perspective of critical medical anthropology. Soc Sci Med. 1994;39:931–48. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- 55.Feagin JR. Racist America: Roots, current realities, and future reparations: New York, NY: Routledge; 2014.
- 56.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54(10):805. doi: 10.1037/0003-066X.54.10.805. [DOI] [PubMed] [Google Scholar]
- 57.Macera C, Armstead C, Anderson N. Sociocultural influences on health. Handb Health Psychol. 2001:427–440.
- 58.Diaz RM, Ayala G, Bein E. Sexual risk as an outcome of social oppression: data from a probability sample of Latino gay men in three US cities. Cult Divers Ethn Minor Psychol. 2004;10(3):255. doi: 10.1037/1099-9809.10.3.255. [DOI] [PubMed] [Google Scholar]
- 59.Williams DR, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5(3/4):243–68. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- 60.Jarama SL, Kennamer JD, Poppen PJ, Hendricks M, Bradford J. Psychosocial, behavioral, and cultural predictors of sexual risk for HIV infection among Latino men who have sex with men. AIDS Behav. 2005;9(4):513–23. doi: 10.1007/s10461-005-9022-1. [DOI] [PubMed] [Google Scholar]
- 61.Gibbons FX, Gerrard M, Cleveland MJ, Wills TA, Brody G. Perceived discrimination and substance use in African American parents and their children: a panel study. J Pers Soc Psychol. 2004;86(4):517. doi: 10.1037/0022-3514.86.4.517. [DOI] [PubMed] [Google Scholar]
- 62.Wilson PA. A dynamic-ecological model of identity formation and conflict among bisexually-behaving African-American men. Arch Sex Behav. 2008;37(5):794–809. doi: 10.1007/s10508-008-9362-9. [DOI] [PubMed] [Google Scholar]
- 63.Collins PH. Black sexual politics: African Americans, gender, and the new racism: New York, NY: Routledge; 2005.
- 64.Feagin JR. The continuing significance of racism: discrimination against Black students in White colleges. J Black Stud. 1992:546–578.
- 65.Fukurai H, Butler EW, Krooth R. Where did Black jurors go? A theoretical synthesis of racial disenfranchisement in the jury system and jury selection. J Black Stud.
- 66.Demuth S, Steffensmeier D. Ethnicity effects on sentence outcomes in large urban courts: comparisons among white, black, and hispanic defendants*. Soc Sci Q. 2004;85(4):994–1011. doi: 10.1111/j.0038-4941.2004.00255.x. [DOI] [Google Scholar]
- 67.Nunn KB. Race, crime and the pool of surplus criminality: or why the war on drugs was a war on blacks. J Gend Race Just. 2002;6:381. [Google Scholar]
- 68.Small D. The war on drugs is a war on racial justice. Soc Res. 2001;68(3):896–903. [Google Scholar]
- 69.Charles CZ. The dynamics of racial residential segregation. Annu Rev Sociol. 2003:167–207.
- 70.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health sociological contributions. J Health Soc Behav. 2010;51(1 suppl):S15–27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404. doi: 10.1016/S0033-3549(04)50068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Subramanian S, Acevedo-Garcia D, Osypuk TL. Racial residential segregation and geographic heterogeneity in black/white disparity in poor self-rated health in the US: a multilevel statistical analysis. Soc Sci Med. 2005;60(8):1667–79. doi: 10.1016/j.socscimed.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 73.Folkman S, Chesney MA, Pollack L, Phillips C. Stress, coping, and high-risk sexual behavior. Health Psychol. 1992;11(4):218. doi: 10.1037/0278-6133.11.4.218. [DOI] [PubMed] [Google Scholar]
- 74.McKirnan DJ, Ostrow DG, Hope B. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS Care. 1996;8(6):655–70. doi: 10.1080/09540129650125371. [DOI] [PubMed] [Google Scholar]
- 75.Hatzenbuehler ML. Social factors as determinants of mental health disparities in LGB populations: implications for public policy. Soc Issues Policy Rev. 2010;4(1):31–62. doi: 10.1111/j.1751-2409.2010.01017.x. [DOI] [Google Scholar]
- 76.Meyer IH. Identity, stress, and resilience in lesbians, gay men, and bisexuals of color. Couns Psychol. 2010;38(3):442–54. doi: 10.1177/0011000009351601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 78.Masten W, Wright M. Resilience over the lifespan. Handb Adult Resilience. 2009:213–237.
- 79.Rutter M. Psychosocial resilience and protective mechanisms. Am J Orthopsychiatry. 1987;57(3):316–31. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 80.Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–8. doi: 10.2105/AJPH.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kawachi I, Kennedy BP, Glass R. Social capital and self-rated health: a contextual analysis. Am J Public Health. 1999;89(8):1187–93. doi: 10.2105/AJPH.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lomas J. Social capital and health: implications for public health and epidemiology. Soc Sci Med. 1998;47(9):1181–8. doi: 10.1016/S0277-9536(98)00190-7. [DOI] [PubMed] [Google Scholar]
- 83.Parker RG. Empowerment, community mobilization and social change in the face of HIV/AIDS. AIDS. 1996. [PubMed]
- 84.Yoshikawa H, Wilson P, Peterson J, Shinn M. Multiple pathways to community-level impacts in HIV prevention: implications for conceptualization, implementation, and evaluation of interventions. Communities AIDS. 2005:28–55.
- 85.Bourgois P. US inner-city apartheid: the contours of structural and interpersonal violence. In: Scheper-Hughes N, Bourgois P, editors. Violence in war and peace: an anthology. Oxford, IN: Blackwell; 2003. pp. 297–303. [Google Scholar]
- 86.Nanín J, Fontaine Y, Wallace B. Recommendations for researchers and clinicians working at the intersection of the HIV/AIDS and methamphetamine epidemics with MSM. In: Wallace B, editor. Toward equity in health: a new global approach to health disparities. New York, NY: Springer; 2008. pp. 393–412. [Google Scholar]
- 87.Wallace B, Carter R, Nanín J, Keller R, Alleyne V. Identity development for “diverse and different others”: integrating stages of change, motivational interviewing, and identity theories for race, people of color, sexual orientation, and disability. In: Wallace B, Carter R, editors. Understanding and dealing with violence: a multicultural approach (Roundtable Series on Psychology and Education, 379) Thousand Oaks, CA: Sage; 2002. pp. 41–92. [Google Scholar]
- 88.Wilson PA, Yoshikawa H. Improving access to quality healthcare among African-American, Asian & Pacific Islander, and Latino lesbian, gay and bisexual populations. In: Meyer I, Northridge ME, editors. The health of sexual minorities: public health perspectives on lesbian, gay, bisexual, and transgender populations. New York, NY: Springer; 2007. pp. 607–37. [Google Scholar]
- 89.Meadows DH. Thinking in systems: a primer. White River Junction, VT: Chelsea Green; 2008. [Google Scholar]
- 90.Singer M, Romero-Daza N. A notable connection between substance abuse, violence, and AIDS: initial findings from research in the Puerto Rican community of Hartford. Bull Alcohol Drug Study Group. 1999;34(2):9–12. [Google Scholar]
- 91.Parker R. Sexuality, culture and power in HIV/AIDS research. Annu Rev of Anthropology. 2001;30:163–179.
- 92.Parker R, Ehrhardt AA. Through an ethnographic lens: ethnographic methods, comparative analysis, and HIV/AIDS research. AIDS Behav. 2001;5:105–14. doi: 10.1023/A:1011399426632. [DOI] [Google Scholar]
- 93.Mays VM, Cochran SD, Zamudio A. HIV prevention research: are we meeting the needs of African American men who have sex with men? J Black Psychol. 2004;30(1):78–105. doi: 10.1177/0095798403260265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Minkler M. Community-based research partnerships: challenges and opportunities. J Urban Health. 2005;82(2):ii3–12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tervalon M, Murray-Garcia J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117–25. doi: 10.1353/hpu.2010.0233. [DOI] [PubMed] [Google Scholar]
- 96.Cargill VA. Recruiting, retaining, and maintaining racial and ethnic minority investigators: why we should bother, why we should care. Am J Public Health. 2009;99(S1):S5–7. doi: 10.2105/AJPH.2008.147645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Satcher D. Embracing culture, enhancing diversity, and strengthening research. Am J Public Health. 2009;99(S1):S4. doi: 10.2105/AJPH.2009.159749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sutton MY, Lanier YA, Willis LA, et al. Strengthening the network of mentored, underrepresented minority scientists and leaders to reduce HIV-related health disparities. Am J Public Health. 2013;103(12):2207–14. doi: 10.2105/AJPH.2013.301345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stoff DM, Forsyth A, Marquez E, McClure S. Introduction: the case for diversity in research on mental health and HIV/AIDS. Am J Public Health. 2010;99(Suppl 1):S8–15. doi: 10.2105/AJPH.2008.153536. [DOI] [PMC free article] [PubMed] [Google Scholar]