Abstract
Clopidogrel is an antiplatelet prodrug that is recommended to reduce the risk of recurrent thrombosis in coronary artery disease (CAD) patients. Paraoxonase 1 (PON1) is suggested to be a rate-limiting enzyme in the conversion of 2-oxo-clopidogrel to active thiol metabolite with inconsistent results. Here, we sought to determine the associations of CYP2C19 and PON1 gene polymorphisms with clopidogrel response and their role in ADP-induced platelet aggregation. Clopidogrel response and platelet aggregation were determined using Multiplate aggregometer in 211 patients with established CAD who received 75 mg clopidogrel and 75–325 mg aspirin daily for at least 14 days. Polymorphisms in CYP2C19 and PON1 were genotyped and tested for association with clopidogrel resistance. Linkage disequilibrium (LD) and their epistatic interaction effects on ADP-induced platelet aggregation were analysed. The prevalence of clopidogrel resistance in this population was approximately 33.2% (n = 70). The frequencies of CYP2C19*2 and *3 were significantly higher in non-responder than those in responders. After adjusting for established risk factors, CYP2C19*2 and *3 alleles independently increased the risk of clopidogrel resistance with adjusted ORs 2.94 (95%CI, 1.65–5.26; p<0.001) and 11.26 (95%CI, 2.47–51.41; p = 0.002, respectively). Patients with *2 or *3 allele and combined with smoking, diabetes and increased platelet count had markedly increased risk of clopidogrel resistance. No association was observed between PON1 Q192R and clopidogrel resistance (adjusted OR = 1.13, 95%CI, 0.70–1.82; p = 0.622). Significantly higher platelet aggregation values were found in CYP2C19*2 and *3 patients when compared with *1/*1 allele carriers (p = 1.98×10−6). For PON1 Q192R genotypes, aggregation values were similar across all genotype groups (p = 0.359). There was no evidence of gene-gene interaction or LD between CYP2C19 and PON1 polymorphisms on ADP-induced platelet aggregation. Our findings indicated that only CYP2C19*2 and *3 alleles had an influence on clopidogrel resistance. The risk of clopidogrel resistance increased further with smoking, diabetes, and increased platelet count.
Introduction
Acute coronary syndromes (ACS), the leading cause of sudden death worldwide, including Thailand [1], occurs as a result of platelet aggregation (thrombosis) within the human artery. Clopidogrel and aspirin are dual antiplatelet therapy that inhibit platelet function, preventing ischemic events and improving outcomes following ACS and percutaneous coronary intervention (PCI) with stent implantation [2]. Clopidogrel is a thienopyridine prodrug that requires enzymatic biotransformation into the active thiol metabolite to inhibit platelet ADP P2Y12 receptor. Aspirin (acetylsalicylic acid) is a cyclooxygenase-1 (COX-1) inhibitor, thereby preventing the production of thromboxane A2, which plays a prominent role in platelet aggregation. Due to the different pathways that clopidogrel and aspirin inhibit platelet aggregation, combined antiplatelet therapy provides additive benefit compared with either agent alone and is considered as a therapy of choice for preventing thrombosis in patients undergoing coronary stenting [3]. However, inter-individual variability in the response to clopidogrel is multifactorial and can be influenced by environmental, clinical, and genetic factors [4]–[6]. Many investigations have indicated that 4% to 44% of patients fail to attain platelet inhibition after clopidogrel therapy [7]–[12]. Recent studies have confirmed that in vivo bioactivation of clopidogrel is a two-step process which is closely linked to the cytochrome P450 (CYP) 2C19 enzyme [13]. The common genetic variants within the CYP2C19 gene, the loss-of-function hepatic CYP2C19*2 (rs4244285) and *3 (rs4986893) polymorphisms were found to be dominantly associated with a lower clopidogrel responsiveness [14]–[16] and a higher risk of adverse cardiac events such as the occurrence of stent thrombosis and recurrent myocardial infarction [17]–[19].
Recently, Bouman et al [20] reported that clopidogrel metabolism involved in two steps of bioactivation. First, clopidogrel undergoes oxidation to 2-oxo-clopidogrel by hepatic CYP450 enzyme. Then, in the second step, PON1 and PON3, the paraoxonases synthesized in the liver associated with HDL, play a crucial role in clopidogrel biotransformation to convert clopidogrel to its thiol active metabolite. Contrary to the prior observations, Bouman identified PON1 Q192R (rs662) as a single key factor for the bioactivation and clinical response of clopidogrel, and found no evidence for CYP2C19 involvement in this step of clopidogrel activation. Specifically, carriers of the QQ genotype were found to have a significantly higher risk of stent thrombosis after PCI as compared with individual with QR or RR genotype with an odds ratio (OR) of 3.3 (95% CI, 1.6–7.9; p = 0.003). However, other investigators had found no association between PON1 Q192R genotype and platelet response to clopidogrel in either Caucasian populations or populations with mixed racial background [21]–[23]. This may be due to the lower enzymatic activity of Q allele in a dose dependent manner (QQ<QR<RR) [24], [25]. Additionally, PON1 also contains the antioxidant property by breaking down biologically active oxidized phospholipids and oxidized cholesteryl esters [26], thereby preventing oxidation of HDL and LDL. Therefore, PON1 has been proposed as an atherosclerotic susceptibility gene. Many studies have reported the association between PON1 Q192R polymorphism and coronary artery disease (CAD) with mixed results. A meta-analysis of 39 studies (10,738 cases and 17,068 controls) reported a pooled OR of 1.10 (95%CI, 1.06–1.13; p<0.001) per R allele for CAD [27]. The prospective REGRESS study in 739 secondary prevention patients reported a hazard ratio (HR) of 1.71 (95%CI, 1.0–2.8; p = 0.03) per Q allele for death due to ischemic disease [28]. The GeneBank study in 1,399 sequential patients undergoing diagnostic coronary angiography reported that the Q allele was associated with an increased risk of major adverse cardiovascular events (HR, 1.48; 95%CI, 1.09–2.03; p = 0.01) [25]. This discrepancy may be due to the PON1 allele frequency which vary greatly across human populations; a relatively high frequency of the PON1 R192 allele is reported in Blacks, Japanese, Chinese and Thai ranging from 58% to 65% [29]–[31] as compared with Caucasians (25% to 30%) [32]. The frequency of CYP2C19 alleles associated with poor metabolizer phenotype also showed high variability from 2–6% in Caucasians to 13–23% in Asians [33]. Since most studies were in Caucasians, there was a paucity of data in Asian populations who have different genetic background. Therefore, the aim of this study was to investigate the impact and interaction of PON1 Q192R, CYP2C19*2 and CYP2C19*3 genotypes on clopidogrel platelet inhibition using multiple electrode platelet aggregometry (MEA) in Thai population.
Methods
Study population
211 patients who resided in Bangkok with aged-range from 39–94 years were recruited if they had established CAD and were on dual antiplatelet therapy with clopidogrel 75 mg and aspirin 75–325 mg daily at least 14 days prior to enrollment for secondary prevention. Subjects were excluded if they had a history of drug or alcohol abuse, bleeding disorder, current warfarin use, myelodysplastic or myeloproliferative disorders, chronic liver disease or any contraindication against aspirin or clopidogrel. Subjects were also excluded if they were pregnant, if the platelet count was less than 105 cell/mm3 (thrombocytopenia), or if there was prior usage of glycoprotein IIb/IIIa antagonist. Questionnaires and medical records were used to collect family and medical history, smoking habit, platelet count, diabetic status, and physical activities. The study protocols were approved by Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University. Informed consent was signed by all subjects after explanation on aims and benefits of this research project.
Platelet aggregation assays
After 14 days of taking 75 mg clopidogrel combined with 75–325 mg aspirin daily, peripheral venous blood samples were obtained from subjects in a catheterization laboratory prior to the next dose of clopidogrel and aspirin. Platelet aggregation was measured using MEA on the Multiplate analyser (Dynabyte, Munich Germany). Blood was placed in 4.5 ml plastic tubes containing hirudin with a final concentration of 25 µg/ml. The final concentration of ADP (6.5 µM) -induced platelet aggregation was assessed as previously reported [34]. Platelet aggregation measured with MEA was quantified as area under the curve (AUC = AU×min) of aggregation unit (AU). A 10 AU×min corresponds to 1 unit (U). The cut off point for this clopidogrel resistance was 50 U as previously reported [35]. All material used for platelet aggregation study was obtained from the manufacturer.
Genotyping
Genomic DNA was isolated from whole blood by guanidine-HCl methods. Subjects were genotyped for CYP2C19*2 (681 G>A), CYP2C19*3 (636 G>A), and PON1 Q192R (575 A>G) using PCR-RFLP as previously described [36]–[38]. Sequence specific primers were used to amplify the alleles of interest. Primers 5′ AATTACAACCAGAGCTTGGC 3′ and 5′ TATCACTTTCCATAAAAGCAAG 3′ were used to amplified the sequence of the CYP2C19*2 in exon 5 of the gene. Primers 5′ AAATTGTTTCCAATCATTTAGCT 3′ and 5′ ACTTCAGGGCTTGGTCAATA 3′ were used to amplified the sequence of the CYP2C19*3 in exon 4. Primers 5′ TATTGTTGCTGTGGGACCTGAG 3′ and 5′ CCTGAGAATCTGAGTAAATCCACT 3′ were used to amplify the sequence of the PON1 gene containing the Q192R polymorphism in exon 6. PCR cycles for denaturation, annealing and extension were 35 cycles for all polymorphism with initial denaturation at 94°C for 5 min and final extension at 72°C for 5 min. PCR profile of CYP2C19*2 polymorphism was denatured at 94°C for 30 sec, annealing at 60°C for 30 sec and extension at 72°C for 30 sec. PCR profile for CYP2C19*3 polymorphism was denatured at 94°C for 30 sec, annealing at 58°C for 30 sec and extension at 72°C for 30 sec. For PON1 polymorphism, denaturation was at 94°C for 1 min, annealing at 60°C for 1 min, and extension at 72°C for 30 sec. The PCR product for CYP2C19*2, CYP2C19*3 and PON1 were 169, 271 and 238 bp, and were cut by 10 units of SmaI, BamHI, and BspPI restriction enzymes, respectively. Products from SmaI enzyme were 120 and 49 bp for G allele and 169 bp for A allele. For BamHI, the products were 175 and 96 bp for G allele and 271 bp for A allele and the products from BspPI were 175 and 63 bp for R192 allele and 238 bp for Q192 allele. The restriction site cut products were detected by 3.5% agarose gel electrophoresis.
Statistical analyses
Variables were presented as mean ± standard deviation (SD). Chi-square goodness-of-fit test or Fisher's exact test was used to test for a possible deviation of genotype distribution from Hardy-Weinberg equilibrium (HWE) proportions. Normally distributed continuous variables were compared across two groups with the two-sided student's t-test and for genotype group comparisons with the one-way ANOVA test. The differences in allele and genotype frequencies between groups were compared using Chi-square test. A nominal p value <0.05 was considered statistically significant.
Univariable and multivariable logistic regression analyses were applied to examine whether PON1 Q192R, CYP2C19*2 and *3 genotypes were associated with clopidogrel resistance after adjusting for age, sex, diabetes, smoking status and platelet count, assuming an additive genetic model coded as the number of mutated allele. Bonferroni's method was used for multiple testing correction considering three genetic loci tests. Statistical significant level was set at p≤0.017.
Interaction between PON1 variants and CYP2C19*2 and *3 was performed using Cordell's test for epistatic interactions [39], using models containing two genetic markers with and without interaction term and covariates (age, sex, diabetic status, smoking status, and platelet count). Likelihood ratio test was performed with 10,000 permutations to calculate the empirical significance of the interaction term, and empirical statistically significant level was set to p<0.05. All analyses were performed using SPSS 13 (SPSS Inc. Chicago, IL, USA) and R version 2.14.2. Cordell's test was performed using scrime package in R [40], [41]. To determine the extent of linkage disequilibrium (LD) in our samples, standardized LD coefficient (D′) and correlation coefficient (r) were calculated for all pairs of polymorphism.
Results
Baseline characteristics of study participants
Based on the result from platelet function test using MEA, the CAD patients were categorized into responders and non-responders to clopidogrel. Among 211 patients included in this study, 70 patients (33.2%) were classified as non-responders and 141 patients (66.8%) as responders. There was no significance between the two groups regarding differences in age, BMI, sex, number of vessel diseases, underlying diseases (cardiomyopathy, hypertension, dyslipidemia, stroke, renal impairment, and peripheral disorder), and concurrent medications (p>0.05). However, clopidogrel non-responders had a significantly higher proportion of diabetes (p = 0.002), smokers (p = 0.043), and higher platelet counts (p = 0.033) as shown in Table 1.
Table 1. Baseline characteristics of study participants.
| Total | Non-responders | Responders | ||
| Parameters | (n = 211) | (n = 70) | (n = 141) | p-value* |
| Age | 66.25±11.15 | 64.47±10.51 | 67.13±11.39 | 0.102 |
| BMI (kg/m2) | 25.54±4.08 | 25.59±4.13 | 25.57±4.08 | 0.970 |
| Female (%) | 68 (32.3) | 21 (30.0) | 47 (33.3) | 0.626 |
| Type of CAD | ||||
| - Single vessel disease (%) | 51 (24.1) | 19 (27.1) | 32 (22.7) | 0.477 |
| - Multi vessel disease (%) | 143 (67.8) | 46 (65.7) | 97 (68.8) | 0.757 |
| - Others (%) | 17 (8.1) | 5 (7.1) | 12 (8.5) | 0.731 |
| Cardiomyophaty (%) | 7 (3.3) | 3 (4.3) | 4 (2.8) | 0.580 |
| Diabetes (%) | 97 (46.0) | 43 (61.4) | 54 (38.3) | 0.002* |
| Hypertension (%) | 184 (87.8) | 61 (87.1) | 123 (87.2) | 0.985 |
| Dyslipidemia (%) | 149 (70.6) | 52 (74.3) | 97 (68.8) | 0.410 |
| Stroke (%) | 14 (6.6) | 6 (8.6) | 8 (5.7) | 0.426 |
| Renal impairment (%) | 23 (10.9) | 6 (8.6) | 17 (12.1) | 0.444 |
| Peripheral arterial disorder (%) | 13 (6.2) | 4 (5.7) | 9 (6.4) | 0.849 |
| Smoking (%) | 85 (40.3) | 35 (50.0) | 50 (35.5) | 0.043* |
| Medication | ||||
|
83 (39.3) | 30 (42.9) | 53 (37.6) | 0.461 |
|
67 (31.8) | 22 (31.4) | 45 (31.9) | 0.943 |
|
183 (86.7) | 65 (92.9) | 118 (83.7) | 0.065 |
| Platelet count (×105/mm3) | 2.55±0.76 | 2.73±0.84 | 2.47±0.72 | 0.033* |
| ADP platelet aggregation (U) | 43.98±26.19 | 73.33±18.26 | 28.95±10.42 | <0.001 |
* Variable is significant difference between responders and non-responders at p-value<0.05.
Distribution and allele frequencies of CYP2C19*2, *3 and PON1 Q192R genotypes
The distribution of CYP2C19*2, *3 and PON1 Q192R genotypes in the clopidogrel responsive and non-responsive groups were summarized in Table 2, which indicates consistency with the Hardy-Weinberg equilibrium (p>0.05). There was no homozygous CYP2C19*3 genotype detected in the study population, which is consistent with its very rare frequency in Caucasians, Africans, Americans, Japanese and Koreans. Moreover, the high frequency of PON1 R192 in this study was consistent with the other reports in Asian populations. The frequencies of both *2/*2 and *2/*3 genotypes (17.10, 10.00 vs 2.10, 0.70%) and *2 and *3 alleles (39.29, 7.14 vs 20.92, 1.42%) were significantly higher in clopidogrel non-responders than those in responders (p = 1.6×10−4, p = 2.1×10−3 and p = 6.5×10−5, p = 3.6×10−4, respectively). Similarly, the frequencies of CYP2C19*1 genotype and allele (34.30, 53.57 vs 58.20, 77.66%) were significantly lower in non-responders than those in responders (p = 1.1×10−3 and 4.0×10−7, respectively). There were no significant differences of PON1 Q192R genotypes and alleles between the two groups (p>0.05).
Table 2. Distribution of CYP2C19*2, *3 and PON1 genotypes in clopidogrel responders and non-responders.
| CYP2C19*2 (rs4244285) | ||||
| Non-responders | Responders | Total | ||
| Genotype | (n = 70) | (n = 141) | (n = 211) | p-value* |
| GG (*1/*1) | 27 (38.6%) | 85 (60.3%) | 112 (53.1%) | 2.9×10−3 † |
| GA (*1/*2) | 31 (44.3%) | 53 (37.6%) | 84 (35.8%) | 0.349 |
| AA (*2/*2) | 12 (17.1%) | 3 (2.1%) | 15 (7.1%) | 1.6×10−4 † |
| HWE p-value ‡ | 0.549 | 0.106 | 0.889 | - |
| Allele frequency | ||||
| Allele*2 (95%CI) | 0.39 (0.32–0.48) | 0.21 (0.16–0.26) | 0.27 (0.23–0.31) | 6.3×10−5 † |
* Comparison of genotype and allele frequencies between non-responders and responders.
Statistically significant difference at p<0.05.
p-value of Hardy-Weinberg equilibrium.
Association of CYP2C19 and PON1 Q192R gene polymorphisms and clopidogrel responsiveness
The results of a simple logistic regression model demonstrated that having one copy of CYP2C19*3 was significantly associated with a 5.71 fold higher risk of clopidogrel resistance (95% CI, 1.72–18.93; p = 0.004) as compared with wild type CYP2C19 (*1/*1). Although one copy of CYP2C19*2 was not significantly associated with clopidogrel resistance (p = 0.053), two copy of CYP2C19 (*2/*2) was associated with 12.59 times higher risk of clopidogrel resistance (95%CI, 3.31–47.96; p<0.001). The combined effect of CYP2C19*2 and *3 estimated that both *2/*2 and *2/*3 genotypes significantly increased the risk of clopidogrel resistances with an unadjusted OR of 13.67 (95%CI, 3.56–52.43; p<0.001) and 23.92 (95%CI, 2.80–204.11; p = 0.004), respectively. After adjusting for the co-dominant effects of *2 and *3 alleles, comparing to *1 allele, *2 was associated with 2.63 times higher risk of clopidogrel resistance (95%CI, 1.62–4.27; p<0.001), and *3 was associated with 6.18 times higher risk of clopidogrel resistance (95%CI, 1.80–21.17; p = 0.004). In contrast, the PON1 Q192R, both genotypes (QQ/QR) and Q allele, did not significantly associate with clopidogrel resistance (p>0.05).
From multivariable logistic regression analysis, assuming a co-dominant allele effect, having one copy of CYP2C19*2 (*1/*2) was associated with 2.30 times higher risk than *1/*1 (95%CI, 1.14–4.66); p<0.021), after adjusted for age, sex, and all variables that differed between responders and non-responders (from Table 1). Similarly, one copy of CYP2C19*3 (*1/*3) was associated with 10.59 times higher risk of clopidogrel resistance compared with *1/*1 (95%CI, 2.39–46.85; p = 0.002). Two copy of CYP2C19*2 (*2/*2) was associated with 13.23 times higher risk of clopidogrel resistance compared with *1/*1 (95%CI, 2.87–60.88; p = 0.001).
The combined effects of CYP2C19*2 and *3, after controlling for additional covariates, compared with *1/*1, CYP2C19*2/*3 was associated with 84.06 times higher risk of clopidogrel resistance (95%CI, 6.89–1026.24; p = 0.001); homozygous CYP2C19*2 (*2/*2) was associated with 13.09 times higher risk of clopidogrel resistance (95%CI, 2.83–60.57; p = 0.001).
For allelic association, after adjusting for the co-dominant effect of *3 allele, *2 allele carrier was associated with 2.94 times higher risk of clopidogrel resistance compared with *1 allele (95%CI, 1.65–5.26; p<0.001). After adjusting for the effects of *2 allele, *3 allele was associated with 11.26 times higher risk of clopidogrel resistance compared with *1 (95%CI, 2.47–51.40; p = 0.002). In contrast, PON1 QR and QQ genotypes and Q allele showed no association with clopidogrel resistance compared with either RR genotype or R allele as references (Table 3).
Table 3. Association between CYP2C19*2, *3, PON1 Q192R and clopidogrel resistance.
| CYP2C19*2 (rs4244285) | ||||
| Genotype | Crude OR (95%CI) | p-value | Adjusted OR (95%CI)† | p-value |
| GG (*1/*1) | 1 | - | 1 | - |
| GA (*1/*2) | 1.84 (0.99–3.42) | 0.053 | 2.30 (1.14–4.66) | 0.021 |
| AA (*2/*2) | 12.59 (3.31–47.96) | <0.001* | 13.23 (2.87–60.88) | 0.001* |
| Allele A (*2) | 2.57 (1.59–4.14) | <0.001* | 2.86 (1.63–5.03) | <0.001* |
* Risk is statistical significant when compared to the reference genotype at p-value<0.017.
Adjusted for diabetes, age, sex, history of smoking and platelet count.
Adjusted for concurrent *2 or *3 allele and covariates (diabetes, age, sex, history of smoking, and platelet count).
The estimated effects of *1, *2, and *3 genotypes, combined with smoking, diabetes status, and increase in platelet count using *1/*1 as a reference genotype, markedly increase the risk of clopidogrel resistance in linear trend as summarized in Table 4.
Table 4. Estimated risk of clopidogrel resistance in patients with at least one of the following risk factors: CYP2C19*2, CYP2C19*3, smoking, diabetes mellitus, increase in platelet count adjusted for age and sex.
| Risk Factors | Adjusted OR* | 95% CI | p-value† |
| *1/*1 | 1 | - | - |
| *1/*1+Smoking | 3.52 | 1.53–8.09 | 0.003 |
| *1/*1+DM | 3.33 | 1.62–6.85 | 0.001 |
| *1/*1+Platelet | 1.05 | 1.00–1.10 | 0.034 |
| *1/*1+DM+Smoking | 7.78 | 2.68–22.53 | <0.001 |
| *1/*1+DM+Platelet | 3.26 | 1.65–6.45 | 0.001 |
| *1/*1+DM+Smoking+Platelet | 8.12 | 2.82–23.73 | <0.001 |
| *1/*2 | 2.94 | 1.65–5.26 | <0.001 |
| *2/*2 | 8.78 | 3.00–25.71 | <0.001 |
| *1/*3 | 11.26 | 2.47–51.41 | 0.002 |
| *2/*3 | 33.15 | 7.01–156.72 | <0.001 |
| *1/*2+Smoking | 7.43 | 2.76–20.05 | <0.001 |
| *2/*2+Smoking | 22.03 | 5.44–89.17 | <0.001 |
| *1/*3+Smoking | 28.06 | 4.84–162.83 | <0.001 |
| *2/*3+Smoking | 83.16 | 12.51–552.97 | <0.001 |
| *1/*2+DM | 9.19 | 3.59–23.52 | <0.001 |
| *2/*2+DM | 27.23 | 6.90–107.37 | <0.001 |
| *1/*3+DM | 34.68 | 6.75–178.06 | <0.001 |
| *2/*3+DM | 102.77 | 17.16–615.29 | <0.001 |
| *1/*2+Platelet count | 3.12 | 1.82–5.34 | <0.001 |
| *2/*2+Platelet count | 9.23 | 3.15–27.03 | <0.001 |
| *1/*3+Platelet count | 11.76 | 2.81–49.29 | <0.001 |
| *2/*3+Platelet count | 34.86 | 7.30–166.45 | <0.001 |
| *1/*2+Smoking+DM | 23.05 | 6.36–83.56 | <0.001 |
| *2/*2+Smoking+DM | 68.3 | 12.96–360.05 | <0.001 |
| *1/*3+Smoking+DM | 86.99 | 12.30–615.28 | <0.001 |
| *2/*3+Smoking+DM | 257.79 | 31.21–2129.62 | <0.001 |
| *1/*2+Smoking+DM+Platelet | 24.23 | 6.67–87.95 | <0.001 |
| *2/*2+Smoking+DM+Platelet | 71.82 | 13.62–378.77 | <0.001 |
| *1/*3+Smoking+DM+Platelet | 91.47 | 12.82–652.52 | <0.001 |
| *2/*3+Smoking+DM+Platelet | 271.07 | 32.56–2256.56 | <0.001 |
*Estimated OR for each risk factor category compared to men with no CYP2C19 mutation (wild type), with average age (66.25 year-old), average platelet count (255,900 platelets/mm3), who do not smoke and do not have diabetes. Platelet variable is calculated per ×1,000 platelet increased. Log odds for clopidogrel resistance were calculated using multivariate logistic regression as a function of CYP2C19*2+CYP2C19*3+Smoking+Diabetic Status+increased Platelet Count.
Risk is statistically significant when compared to the reference genotype at p-value<0.05.
CYP2C19*2, *3 and PON1 Q192R genotypes and platelet aggregation
The ADP-induced platelet aggregation values across CYP2C19*2 and *3 genotypes were shown in Table 5. For CYP2C19*2 genotypes, ADP-induced platelet aggregation significantly differed across genotype groups (p = 2.98×10−5). In the patients who were carriers of at least one *2 allele (*1/*2 or *2/*2), ADP induced-platelet aggregation was also significantly different when compared with *1/*1 genotype (p = 0.004). For CYP2C19*3 genotypes, the ADP-induced platelet aggregation did not differ across genotype groups (p = 0.069). However, when combining CYP2C19*2 and *3, the ADP-induced platelet aggregations across genotypes were significantly different (p = 1.98×10−6). For PON1 Q192R genotypes, the ADP-induced platelet aggregation did not differ across genotype groups (p = 0.359).
Table 5. ADP induced platelet aggregation level by CYP2C19*2, *3 and PON1 Q192R polymorphisms in clopidogrel treated patients with coronary artery disease.
| Genotypes | n | Platelet Aggregation Level | |
| CYP2C19 *2 | GG (*1/*1) | 112 | 39.16±23.28 |
| (rs4244285; 681G>A) | GA (*1/*2) | 84 | 45.20±23.62 |
| AA (*2/*2) | 15 | 73.07±39.77 | |
| p-value | 2.98×10−5 | ||
| CYP2C19 *3 | GG (*1/*1) | 197 | 43.10±26.36 |
| (rs4986893; 636G>A) | GA (*1/*3) | 14 | 56.29±20.69 |
| AA (*3/*3) | 0 | - | |
| p-value | 0.069 | ||
| CYP2C19 *2 | *1/*1 | 106 | 38.90±23.49 |
| & CYP2C19 *3 | *1/*2 | 76 | 43.36±23.28 |
| *1/*3 | 6 | 47.67±19.14 | |
| *2/*3 | 8 | 62.75±20.54 | |
| *2/*2 | 15 | 73.07±39.77 | |
| p-value | 1.98×10−6 | ||
| PON1 | GG (RR) | 105 | 42.14±25.43 |
| (rs662; 575A>G) | AG (QR) | 84 | 45.77±27.30 |
| AA (QQ) | 22 | 45.86±26.08 | |
| p-value | 0.359 |
p-values assuming additive genetic model represent the association between genotype and ADP-induced platelet aggregation (U) at p-value<0.05.
Interaction between PON1 Q192R polymorphisms and ADP-induced platelet aggregation level after stratification by CYP2C19*2 and CYP2C19*3
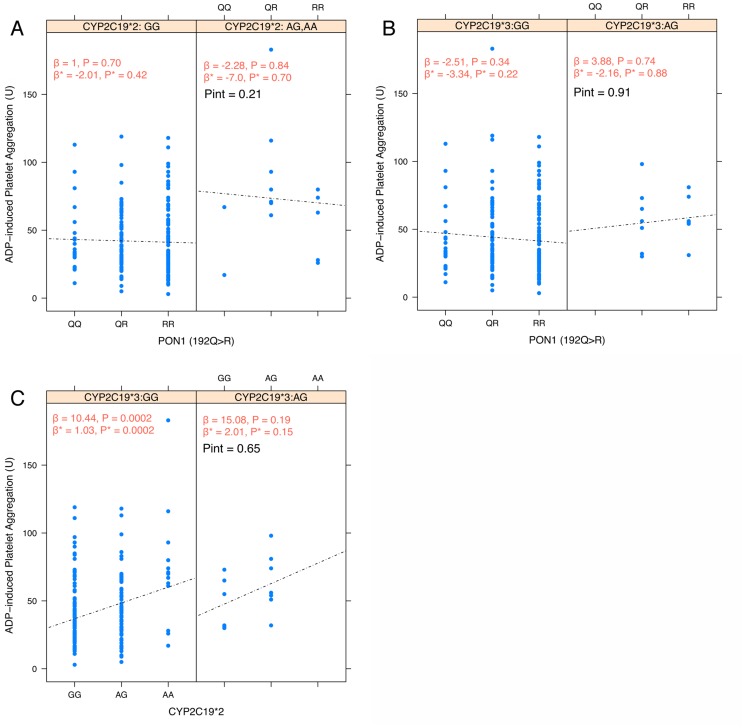
Since both CYP2C19 and PON1 involve in activation of clopidogrel prodrug as suggested by Bouman et al. [20], the interaction effects between CYP2C19 (*2, *3) and PON1 (Q192R) on ADP-induced platelet aggregation were investigated. After stratification by CYP2C19*2 (Figure 1A) and *3 genotypes (Figure 1B), the effects of PON1 (Q192R) polymorphism on ADP-induced platelet aggregation were not modified by neither CYP2C19*2 nor CYP2C19*3 allele. Cordell's test for epistatic interaction showed no statistically significant interaction between CYP2C19*2 or *3 with PON1 Q192R polymorphisms (pint = 0.21 and 0.91, respectively). Similarly, CYP2C19*3 did not modify the effects of CYP2C19*2 on ADP-induced platelet aggregation (pint = 0.65, Figure 1C). To examine the extent of linkage disequilibrium (LD) in these study samples, standardized LD coefficient (D′) and correlation coefficient (r) were calculated for all pairs of polymorphisms. Table 6 shows the LD matrix generated using D′ and r. No evidence of LD was observed among these three polymorphisms (D′ and r<0.5).
Figure 1. Interaction among polymorphisms in CYP2C19*2, *3 and PON1 Q192R and the effects on ADP-induced platelet aggregation.
A) Effects of PON1 Q192R polymorphism on platelet aggregation stratified by CYP2C19*2 genotype; B) Effects of PON1 Q192R polymorphism on platelet aggregation stratified by CYP2C19*3 genotype; C) Effects of CYP2C19*2 on platelet aggregation stratified by CYP2C19*3 genotype
Table 6. Standardized linkage disequilibrium coefficient (D′) and correlation coefficient (r) among three polymorphisms in CYP2C19 and PON1.
| D′ r | PON1 Q192R | CYP2C19*3 | CYP2C19*2 |
| PON1 Q192R | - | −0.0276 | 0.0089 |
| CYP2C19 *3 | 0.2258 | - | 0.0223 |
| CYP2C19 *2 | 0.0097 | 0.0731 | - |
D′ values are shown in the lower triangle, and r values are shown in the upper triangle.
Discussion
Bouman et al's study [20] is the first report to identify that PON1 Q192R is a major determinant of clopidogrel efficacy using in vitro metabolomic profiling techniques. The PON1 activity was significantly reduced in subjects with homozygous wild type allele (PON1 QQ192) compared with carriers of the mutant allele. In addition, in a group of patients with stent thrombosis and matched controls without stent thrombosis, PON1 QQ192 was associated with decreased platelet inhibition by clopidogrel and decreased plasma active thiol metabolite after given a 600 mg clopidogrel loading dose. In addition, PON1 QQ192 was also associated with an OR of 3.3 for the occurrence of stent thrombosis as compared with QR192 or RR192 genotypes. Later, however, other studies could not document the influence of PON1 Q192R genotype on clopidogrel antiplatelet aggregation since the publication of the study by Bouman et al [21]–[23]. In this study, we evaluated the effects of CYP2C19 and PON1 genetic polymorphisms on clopidogrel antiplatelet function in Thai population. Similar to the findings from other investigators in African-American and Caucasian populations [21], [22], our results have shown that only CYP2C19*2 and *3 genotypes, but not the PON1 Q192R genotypes, modified the effect of clopidogrel. The mean aggregation values increased by a strong genetic effect across CYP2C19 genotype groups in individuals treated with clopidogrel. Also, only CYP2C19*2 and *3 genotypes but not the PON1 Q192R genotypes were found to be associated with a higher risk of clopidogrel resistance in CAD patients during treatment with clopidogrel.
The present study was strengthened by testing the influence of these SNPs on platelet aggregation in parallel as measured by MEA assay. Only CYP2C19*2 and *3 polymorphisms have been demonstrated to be a strong determinant of reduced active clopidogrel metabolite formation corresponding to the studies in Caucasians [14], [17], [42]–[52]. Nevertheless, the influence of PON1 on the level of platelet aggregation had a trend towards higher values in QR192 and QQ192 patients (Table 5). This suggested that PON1 polymorphism may be associated with small differences in platelet inhibition as suggested by the finding of Bouman et al [20]. The small effects of PON1 Q192R could explain why several reports were unable to confirm this association between PON1 polymorphism and platelet aggregation in patients who were treated with clopidogrel [21]–[23],[53]–[57]. Concerning the clinical outcome of patients treated with clopidogrel, our results reported here are in agreement with a number of prior studies and confirm the pivotal role of CYP2C19*2 and *3 as genetic markers for platelet aggregation and clopidogrel response. This present study also demonstrated no association and linkage disequilibrium between CYP2C19 and PON1 polymorphisms, which supports the evidence that CYP2C19 locus, located on chromosome 10, was the only locus which was significantly associated with clopidogrel treatment efficacy in a genome-wide association study (GWAS) [42]. The GWAS did not find evidence for association between SNPs located on or near the PON1 gene on chromosome 7 and variation in platelet inhibition by clopidogrel [42]. In addition, in a meta-analysis investigating the effect of CYP2C19 alleles on recurrent stenosis in patients receiving clopidogrel after coronary stenting, the presence of one reduced-function allele was associated with a HR of 2.67, and the presence of two reduced-function alleles was associated with a HR of 3.97 for the recurrence of thrombosis [46]. This study also confirms that the presence of one reduced-function allele of CYP2C19 was associated with adjusted ORs of 2.94 and 11.26 for *2 and *3, respectively. The presence of two reduced-function alleles was associated with adjusted ORs of 13.09 and 84.06 for *2/*2 and *2/*3, respectively. These findings support the clinical importance of the reduced-function CYP2C19 polymorphism and clopidogrel resistance on recurrent ischemic events and restenosis after coronary stenting.
In this study, smoking status, diabetes mellitus, and increase in platelet count were shown to be the three major contributing factors that could promote the development of platelet aggregation in CAD patients (Table 4). These conditions have been known to be associated with high oxidative stress, suggesting a possible link between high oxidative stress and response to clopidogrel treatment. This study suggested that not only genetic polymorphisms but also oxidative stress can enhance platelet aggregation to clopidogrel responsiveness in CAD patients.
Limitations of the study include a relatively small sample size, which might contribute to the inability to detect weaker effects of PON1 on clopidogrel response, as compared with the stronger effects of CYP2C19. Although plasma levels of the active metabolite of clopidogrel and PON1 enzyme activity were not measured to confirm the lower level of enzyme activity associated with Q allele, these parameters could be used to indirectly assess the platelet function test as measured by ADP-induced platelet aggregation. Finally, platelet function testing was done with only one single device (Multiplate anslyser), using ADP-induced platelet aggregation, therefore, we could not exclude the possibility that other mechanisms might also explain the clopidogrel resistance as measured by the Multiplate analyser.
Conclusions
This study confirms the impact of CYP2C19*2 and *3 polymorphisms on antiplatelet effects of clopidogrel in Thai population similar to the results found in Caucasian populations with different genetic background. PON1 Q192R appeared to have a little modification of efficacy and safety of clopidogrel in CAD patients. A larger study may be needed to confirm the association of the PON1 Q192 allele with adverse ischemic events in patients receiving clopidogrel treatment. Our results are only relevant to clopidogrel-treated patients; however, knowing the genotypes of CYP2C19 should aid in selection of antiplatelet therapy. In the future, pharmacogenetic studies may be needed to introduce newer antiplatelet drugs that do not require CYP2C19 activation and may reduce the overall impact of clopidogrel resistance in patients with CAD.
Acknowledgments
The authors would like to thank Dr. William M. Honsa for English language editorial support. Some parts of this work have been presented in a local meeting at the 39th Congress on Science and Technology of Thailand.
Data Availability
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Due to ethical concerns over the nature of clinical and genetic data, access to the data will be approved only to researchers who meet the criteria for access to confidential data, as reviewed by Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University. Requests for data can be made to the corresponding author.
Funding Statement
This study was partly supported by Graduate Thesis Scholarship grant from Faculty of Medicine Siriraj Hospital, Mahidol University to RK. AL and BS were supported by “Chalermphrakiat” grant, Faculty of Medicine Siriraj Hospital, Mahidol University. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Moleerergpoom W, Kanjanavanit R, Jintapakorn W, Sritara P (2007) Costs of payment in Thai acute coronary syndrome patients. J Med Assoc Thai 90 Suppl 121–31. [PubMed] [Google Scholar]
- 2. Syed FA, Bett J, Walters DL (2011) Anti-platelet therapy for Acute Coronary Syndrome: A review of currently available agents and what the future holds. Cardiovasc Hematol Disord Drug Targets [DOI] [PubMed] [Google Scholar]
- 3. Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, et al. (2006) ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention-Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J Am Coll Cardiol 47: 216–235. [DOI] [PubMed] [Google Scholar]
- 4. Gurbel PA, Tantry US (2006) Drug insight: Clopidogrel nonresponsiveness. Nat Clin Pract Cardiovasc Med 3: 387–395. [DOI] [PubMed] [Google Scholar]
- 5. Gurbel PA, Bliden KP, Hiatt BL, O'Connor CM (2003) Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation 107: 2908–2913. [DOI] [PubMed] [Google Scholar]
- 6. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Alfonso F, Macaya C, et al. (2007) Variability in individual responsiveness to clopidogrel: clinical implications, management, and future perspectives. J Am Coll Cardiol 49: 1505–1516. [DOI] [PubMed] [Google Scholar]
- 7. Jaremo P, Lindahl TL, Fransson SG, Richter A (2002) Individual variations of platelet inhibition after loading doses of clopidogrel. J Intern Med 252: 233–238. [DOI] [PubMed] [Google Scholar]
- 8. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Ramirez C, Sabate M, et al. (2005) Platelet function profiles in patients with type 2 diabetes and coronary artery disease on combined aspirin and clopidogrel treatment. Diabetes 54: 2430–2435. [DOI] [PubMed] [Google Scholar]
- 9. Muller I, Besta F, Schulz C, Massberg S, Schonig A, et al. (2003) Prevalence of clopidogrel non-responders among patients with stable angina pectoris scheduled for elective coronary stent placement. Thromb Haemost 89: 783–787. [PubMed] [Google Scholar]
- 10. Mobley JE, Bresee SJ, Wortham DC, Craft RM, Snider CC, et al. (2004) Frequency of nonresponse antiplatelet activity of clopidogrel during pretreatment for cardiac catheterization. Am J Cardiol 93: 456–458. [DOI] [PubMed] [Google Scholar]
- 11. Matetzky S, Shenkman B, Guetta V, Shechter M, Beinart R, et al. (2004) Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation 109: 3171–3175. [DOI] [PubMed] [Google Scholar]
- 12. Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Ramirez C, Barrera-Ramirez C, et al. (2005) Identification of low responders to a 300-mg clopidogrel loading dose in patients undergoing coronary stenting. Thromb Res 115: 101–108. [DOI] [PubMed] [Google Scholar]
- 13. Kazui M, Nishiya Y, Ishizuka T, Hagihara K, Farid NA, et al. (2010) Identification of the human cytochrome P450 enzymes involved in the two oxidative steps in the bioactivation of clopidogrel to its pharmacologically active metabolite. Drug Metab Dispos 38: 92–99. [DOI] [PubMed] [Google Scholar]
- 14. Hulot JS, Bura A, Villard E, Azizi M, Remones V, et al. (2006) Cytochrome P450 2C19 loss-of-function polymorphism is a major determinant of clopidogrel responsiveness in healthy subjects. Blood 108: 2244–2247. [DOI] [PubMed] [Google Scholar]
- 15. Brandt JT, Close SL, Iturria SJ, Payne CD, Farid NA, et al. (2007) Common polymorphisms of CYP2C19 and CYP2C9 affect the pharmacokinetic and pharmacodynamic response to clopidogrel but not prasugrel. J Thromb Haemost 5: 2429–2436. [DOI] [PubMed] [Google Scholar]
- 16. Umemura K, Furuta T, Kondo K (2008) The common gene variants of CYP2C19 affect pharmacokinetics and pharmacodynamics in an active metabolite of clopidogrel in healthy subjects. J Thromb Haemost 6: 1439–1441. [DOI] [PubMed] [Google Scholar]
- 17. Simon T, Verstuyft C, Mary-Krause M, Quteineh L, Drouet E, et al. (2009) Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med 360: 363–375. [DOI] [PubMed] [Google Scholar]
- 18. Sibbing D, Braun S, Morath T, Mehilli J, Vogt W, et al. (2009) Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent thrombosis. J Am Coll Cardiol 53: 849–856. [DOI] [PubMed] [Google Scholar]
- 19. Bonello L, Tantry US, Marcucci R, Blindt R, Angiolillo DJ, et al. (2010) Consensus and future directions on the definition of high on-treatment platelet reactivity to adenosine diphosphate. J Am Coll Cardiol 56: 919–933. [DOI] [PubMed] [Google Scholar]
- 20. Bouman HJ, Schomig E, van Werkum JW, Velder J, Hackeng CM, et al. (2011) Paraoxonase-1 is a major determinant of clopidogrel efficacy. Nat Med 17: 110–116. [DOI] [PubMed] [Google Scholar]
- 21. Kreutz RP, Nystrom P, Kreutz Y, Miao J, Desta Z, et al. (2012) Influence of paraoxonase-1 Q192R and cytochrome P450 2C19 polymorphisms on clopidogrel response. Clin Pharmacol 4: 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sibbing D, Koch W, Massberg S, Byrne RA, Mehilli J, et al. (2011) No association of paraoxonase-1 Q192R genotypes with platelet response to clopidogrel and risk of stent thrombosis after coronary stenting. Eur Heart J 32: 1605–1613. [DOI] [PubMed] [Google Scholar]
- 23. Pare G, Ross S, Mehta SR, Yusuf S, Anand SS, et al. (2012) Effect of PON1 Q192R genetic polymorphism on clopidogrel efficacy and cardiovascular events in the Clopidogrel in the Unstable Angina to Prevent Recurrent Events trial and the Atrial Fibrillation Clopidogrel Trial with Irbesartan for Prevention of Vascular Events. Circ Cardiovasc Genet 5: 250–256. [DOI] [PubMed] [Google Scholar]
- 24. Marsillach J, Aragones G, Beltran R, Caballeria J, Pedro-Botet J, et al. (2009) The measurement of the lactonase activity of paraoxonase-1 in the clinical evaluation of patients with chronic liver impairment. Clin Biochem 42: 91–98. [DOI] [PubMed] [Google Scholar]
- 25. Bhattacharyya T, Nicholls SJ, Topol EJ, Zhang R, Yang X, et al. (2008) Relationship of paraoxonase 1 (PON1) gene polymorphisms and functional activity with systemic oxidative stress and cardiovascular risk. JAMA 299: 1265–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mackness MI, Arrol S, Mackness B, Durrington PN (1997) Alloenzymes of paraoxonase and effectiveness of high-density lipoproteins in protecting low-density lipoprotein against lipid peroxidation. Lancet 349: 851–852. [DOI] [PubMed] [Google Scholar]
- 27. Lawlor DA, Day IN, Gaunt TR, Hinks LJ, Briggs PJ, et al. (2004) The association of the PON1 Q192R polymorphism with coronary heart disease: findings from the British Women's Heart and Health cohort study and a meta-analysis. BMC Genet 5: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Regieli JJ, Jukema JW, Doevendans PA, Zwinderman AH, Kastelein JJ, et al. (2009) Paraoxonase variants relate to 10-year risk in coronary artery disease: impact of a high-density lipoprotein-bound antioxidant in secondary prevention. J Am Coll Cardiol 54: 1238–1245. [DOI] [PubMed] [Google Scholar]
- 29. Likidlilid A, Akrawinthawong K, Poldee S, Sriratanasathavorn C (2010) Paraoxonase 1 polymorphisms as the risk factor of coronary heart disease in a Thai population. Acta Cardiol 65: 681–691. [DOI] [PubMed] [Google Scholar]
- 30. Ko YL, Ko YS, Wang SM, Hsu LA, Chang CJ, et al. (1998) The Gln-Arg 191 polymorphism of the human paraoxonase gene is not associated with the risk of coronary artery disease among Chinese in Taiwan. Atherosclerosis 141: 259–264. [DOI] [PubMed] [Google Scholar]
- 31. Imai Y, Morita H, Kurihara H, Sugiyama T, Kato N, et al. (2000) Evidence for association between paraoxonase gene polymorphisms and atherosclerotic diseases. Atherosclerosis 149: 435–442. [DOI] [PubMed] [Google Scholar]
- 32. Ferre N, Tous M, Paul A, Zamora A, Vendrell JJ, et al. (2002) Paraoxonase Gln-Arg(192) and Leu-Met(55) gene polymorphisms and enzyme activity in a population with a low rate of coronary heart disease. Clin Biochem 35: 197–203. [DOI] [PubMed] [Google Scholar]
- 33. Goldstein JA (2001) Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol 52: 349–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sibbing D, Braun S, Jawansky S, Vogt W, Mehilli J, et al. (2008) Assessment of ADP-induced platelet aggregation with light transmission aggregometry and multiple electrode platelet aggregometry before and after clopidogrel treatment. Thromb Haemost 99: 121–126. [DOI] [PubMed] [Google Scholar]
- 35. Gerotziafas GT, Zarifis J, Bandi A, Mossialos L, Galea V, et al. (2012) Description of response to aspirin and clopidogrel in outpatients with coronary artery disease using multiple electrode impedance aggregometry. Clin Appl Thromb Hemost 18: 356–363. [DOI] [PubMed] [Google Scholar]
- 36. de Morais SM, Wilkinson GR, Blaisdell J, Nakamura K, Meyer UA, et al. (1994) The major genetic defect responsible for the polymorphism of S-mephenytoin metabolism in humans. J Biol Chem 269: 15419–15422. [PubMed] [Google Scholar]
- 37. De Morais SM, Wilkinson GR, Blaisdell J, Meyer UA, Nakamura K, et al. (1994) Identification of a new genetic defect responsible for the polymorphism of (S)-mephenytoin metabolism in Japanese. Mol Pharmacol 46: 594–598. [PubMed] [Google Scholar]
- 38. Campo S, Sardo MA, Trimarchi G, Bonaiuto M, Fontana L, et al. (2004) Association between serum paraoxonase (PON1) gene promoter T(-107)C polymorphism, PON1 activity and HDL levels in healthy Sicilian octogenarians. Exp Gerontol 39: 1089–1094. [DOI] [PubMed] [Google Scholar]
- 39. Cordell HJ (2002) Epistasis: what it means, what it doesn't mean, and statistical methods to detect it in humans. Hum Mol Genet 11: 2463–2468. [DOI] [PubMed] [Google Scholar]
- 40. Schwender H, Fritsch A (2013) scrime: Analysis of High-Dimensional Categorical Data such as SNP Data. Available: http://CRAN.R-project.org/package=scrime. [Google Scholar]
- 41.R Core Team (2013) R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Available: http://www.R-project.org. [Google Scholar]
- 42. Shuldiner AR, O'Connell JR, Bliden KP, Gandhi A, Ryan K, et al. (2009) Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA 302: 849–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sibbing D, Gebhard D, Koch W, Braun S, Stegherr J, et al. (2010) Isolated and interactive impact of common CYP2C19 genetic variants on the antiplatelet effect of chronic clopidogrel therapy. J Thromb Haemost 8: 1685–1693. [DOI] [PubMed] [Google Scholar]
- 44. Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, et al. (2009) Cytochrome P450 genetic polymorphisms and the response to prasugrel: relationship to pharmacokinetic, pharmacodynamic, and clinical outcomes. Circulation 119: 2553–2560. [DOI] [PubMed] [Google Scholar]
- 45. Mega JL, Close SL, Wiviott SD, Shen L, Walker JR, et al. (2010) Genetic variants in ABCB1 and CYP2C19 and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial: a pharmacogenetic analysis. Lancet 376: 1312–1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mega JL, Simon T, Collet JP, Anderson JL, Antman EM, et al. (2010) Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA 304: 1821–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hochholzer W, Trenk D, Fromm MF, Valina CM, Stratz C, et al. (2010) Impact of cytochrome P450 2C19 loss-of-function polymorphism and of major demographic characteristics on residual platelet function after loading and maintenance treatment with clopidogrel in patients undergoing elective coronary stent placement. J Am Coll Cardiol 55: 2427–2434. [DOI] [PubMed] [Google Scholar]
- 48. Trenk D, Hochholzer W, Fromm MF, Chialda LE, Pahl A, et al. (2008) Cytochrome P450 2C19 681G>A polymorphism and high on-clopidogrel platelet reactivity associated with adverse 1-year clinical outcome of elective percutaneous coronary intervention with drug-eluting or bare-metal stents. J Am Coll Cardiol 51: 1925–1934. [DOI] [PubMed] [Google Scholar]
- 49. Sibbing D, Stegherr J, Latz W, Koch W, Mehilli J, et al. (2009) Cytochrome P450 2C19 loss-of-function polymorphism and stent thrombosis following percutaneous coronary intervention. Eur Heart J 30: 916–922. [DOI] [PubMed] [Google Scholar]
- 50. Collet JP, Hulot JS, Pena A, Villard E, Esteve JB, et al. (2009) Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study. Lancet 373: 309–317. [DOI] [PubMed] [Google Scholar]
- 51. Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, et al. (2009) Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 360: 354–362. [DOI] [PubMed] [Google Scholar]
- 52. Harmsze AM, van Werkum JW, Ten Berg JM, Zwart B, Bouman HJ, et al. (2010) CYP2C19*2 and CYP2C9*3 alleles are associated with stent thrombosis: a case-control study. Eur Heart J 31: 3046–3053. [DOI] [PubMed] [Google Scholar]
- 53. Simon T, Steg PG, Becquemont L, Verstuyft C, Kotti S, et al. (2011) Effect of paraoxonase-1 polymorphism on clinical outcomes in patients treated with clopidogrel after an acute myocardial infarction. Clin Pharmacol Ther 90: 561–567. [DOI] [PubMed] [Google Scholar]
- 54. Trenk D, Hochholzer W, Fromm MF, Zolk O, Valina CM, et al. (2011) Paraoxonase-1 Q192R polymorphism and antiplatelet effects of clopidogrel in patients undergoing elective coronary stent placement. Circ Cardiovasc Genet 4: 429–436. [DOI] [PubMed] [Google Scholar]
- 55. Fontana P, James R, Barazer I, Berdague P, Schved JF, et al. (2011) Relationship between paraoxonase-1 activity, its Q192R genetic variant and clopidogrel responsiveness in the ADRIE study. J Thromb Haemost 9: 1664–1666. [DOI] [PubMed] [Google Scholar]
- 56. Rideg O, Komocsi A, Magyarlaki T, Tokes-Fuzesi M, Miseta A, et al. (2011) Impact of genetic variants on post-clopidogrel platelet reactivity in patients after elective percutaneous coronary intervention. Pharmacogenomics 12: 1269–1280. [DOI] [PubMed] [Google Scholar]
- 57. Lewis JP, Fisch AS, Ryan K, O'Connell JR, Gibson Q, et al. (2011) Paraoxonase 1 (PON1) gene variants are not associated with clopidogrel response. Clin Pharmacol Ther 90: 568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Due to ethical concerns over the nature of clinical and genetic data, access to the data will be approved only to researchers who meet the criteria for access to confidential data, as reviewed by Siriraj Institutional Review Board, Faculty of Medicine Siriraj Hospital, Mahidol University. Requests for data can be made to the corresponding author.