Abstract
Objective
The goal of this meta-analysis was to examine whether long-term physical exercise could be a potential effective treatment for substance use disorders (SUD).
Methods
The PubMed, Web of Science, Elsevier, CNKI and China Info were searched for randomized controlled trials (RCT) studies in regards to the effects of physical exercise on SUD between the years 1990 and 2013. Four main outcome measures including abstinence rate, withdrawal symptoms, anxiety, and depression were evaluated.
Results
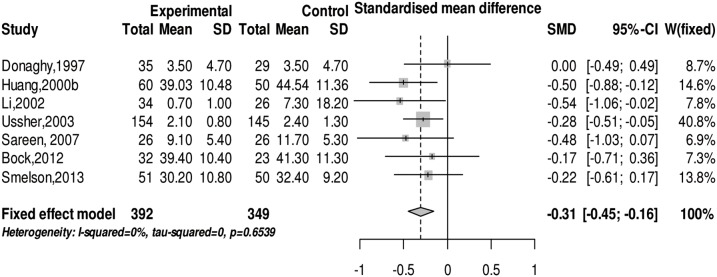
Twenty-two studies were integrated in the meta-analysis. The results indicated that physical exercise can effectively increase the abstinence rate (OR = 1.69 (95% CI: 1.44, 1.99), z = 6.33, p<0.001), ease withdrawal symptoms (SMD = −1.24 (95% CI: −2.46, −0.02), z = −2, p<0.05), and reduce anxiety (SMD = −0.31 (95% CI: −0.45, −0.16), z = −4.12, p<0.001) and depression (SMD = −0.47 (95% CI: −0.80, −0.14), z = −2.76, p<0.01). The physical exercise can more ease the depression symptoms on alcohol and illicit drug abusers than nicotine abusers, and more improve the abstinence rate on illicit drug abusers than the others. Similar treatment effects were found in three categories: exercise intensity, types of exercise, and follow-up periods.
Conclusions
The moderate and high-intensity aerobic exercises, designed according to the Guidelines of American College of Sports Medicine, and the mind-body exercises can be an effective and persistent treatment for those with SUD.
Introduction
Substance abuse, such as alcohol, nicotine, and illicit drugs, is one of the largest public health issues in the world. Figures from the World Health Organization (WHO) show that 2.5 million people die from alcohol abuse each year, and at least 15.3 million people have substance use disorders (SUD). Moreover, 120 countries have reported cases of HIV infection in drug addicts [1]. Substance abuse also increases the risk of spreading HIV and is an overall detriment to society, family, and individuals [2]–[4]. Currently, one of the most commonly used treatments for substance addiction is drug replacement therapy, using substances such as methadone or buprenorphine. Both methadone and buprenorphine are long-acting opioid agonists and used to treat opioid addiction, such as heroin, by reducing and/or eliminating the use of substances, relieving craving behavior, suppressing abstinence symptoms, and decreasing substance abuse-associated infective diseases transmission [5], [6]. However, like all opioids, both methadone and buprenorphine have risk of addiction and often have potential of drug-drug interactions [7]. Opioid substitutes are also linked to diabetes, nicotine addiction, and premature death [8]–[10]. Therefore, there is a strong interest in finding alternative treatments for SUD.
In general, physical exercise is characterized as a planned, organized, and repeated body movement that aims to promote or maintain physical fitness [11]–[13]. The most common physical exercises include aerobics (brisk walking and running) and mind-body exercises (Tai Chi Quan, Qigong, and Yoga). Compared to methadone and buprenorphine drug-replacement therapies, physical exercise has been recognized as a potential add-on treatment for SUD. For example, studies showed that subjects with regular physical exercise showed lower rates of SUD compared to people with less exercise [14], and regular physical exercise in adolescence provided a preventive effect on alcohol and illicit drug use in adulthood [15]. Furthermore, exercise training caused a significant reduction in daily use and craving for cannabis in marijuana-dependent adults [16], and enhanced the healing effect on SUD [17]–[19]. The positive effects of physical exercise on SUD have also been confirmed in animal experiments. For example, wheel-running can ease withdrawal behavior in mice with morphine-addiction [20], while voluntary treadmill exercise [21], [22] and mandatory treadmill exercise [23] can reduce cocaine, morphine, nicotine, and alcohol intake in various mouse models [22], [24], [25].
However, some contradictory findings were reported, such as exercise providing no significant effects on substance abusers. For example, one study reported that a 3- week regiment of aerobic exercise and strength training failed to increase the abstinence rate of alcohol abusers [26], and another study found that a 10-week physical exercise program caused no change in the abstinence rate of smokers or relief for emotional symptoms related to smoking [27]. As there is no clear answer for these controversial findings, more comprehensive analyses of physical exercise, such as the intensity and duration of exercise applied, are needed.
In the past two years, a number of articles reviewed whether physical exercise could be considered as a potential method for treating SUD [13], [18], [28]–[35]. These articles included preclinical and clinical literature of physical exercise-induced protective effects on the different transitional phases of SUD. These include the initiation of drug use, the progression from use to addiction, the drug withdrawal and relapse period [29] in alcohol, nicotine and illicit drug use disorders [32], and the improvement of mood and overall life quality of those with SUD [13]. A few articles also reviewed the relationship between various type of physical exercises as promising complementary therapies for SUD [33], [34]. To further understand the relationship between physical exercise intervention and SUD, several statistical review articles have analyzed the effects of acute exercise on nicotine addiction. For example, Ussher et al. found that physical exercise can effectively intervene in symptoms related to smoking (RR: 0.97–4.96) using meta-analyses on thirteen [36] and fifteen [37] original research articles, while others reported similar results using analyses of individual participant data (IPD) or the systematic review method [38]. Together, these studies provide the support for using physical exercise as a treatment for SUD. However, there is a shortage of important evidence in previously published meta-analyses of physical exercise as treatments in SUD, such as the effect of mind-body exercise or chronic physical exercise on substance addiction with one or polydrugs, as well as a systematic evaluation of randomized controlled trials (RCT). A recent study reported that Yoga, a typical mind-body exercise, may improve mood status and quality of life for women undergoing detoxification for heroin dependence [39]. In addition, subjects who are addicted to more than one drug often develop more complicated symptoms related to the synergistic effect of drug-drug interaction on brain structures and functions [40]. It is known that acute exercise produces different effects on brain function, such as cognition, than long-term routing exercises, which can lead to improvement of object recognition memory and reduction of perceived stress [41]. Indeed, both acute and chronic aerobic exercises have been extensively used to treat SUD. The changes induced by acute exercise can be viewed as a transitory modulation of the arousal physiology [42], while effects of chronic physical exercise are generally explained by structural and durable changes in the organism, such as angiogenesis [43] and neurogenesis [44]. All of these may help to explain the contradictory findings on exercise intervention in SUD.
The aim of this meta-analysis is to verify the treatment effects of chronic physical exercise on various SUD by analyzing the current RCT studies. The abstinence rate, withdrawal symptoms, anxiety levels, and depression levels are included in this meta-analysis as outcomes of treatment. Furthermore, we also included the analyses of exercise intensities, exercise types, and lasting effects of physical exercise on SUD. Lastly, we performed sub-group analyses to provide details of potential optimal physical exercise therapies for specific drug addictions.
Methods
This meta-analysis followed the PRISMA guidelines [45] for conducting and reporting systematic reviews.
Search strategy
We conducted a search for relevant literature in the following electronic databases: PubMed, Web of Science, Elsevier, China National Knowledge Infrastructure (CNKI), and China Info. The key search words included exercise, physical activity, qigong, tai chi, yoga, heroin, morphine, opioid, opiate, cocaine, methadone, marijuana, cannabis, alcohol, drinker, cigarette, smoke, nicotine, drug abuse, drug dependence, and substance use. The search was limited to Chinese and English literature studying adults (≥18 years old) published from January 1990 to August 2013.
Study selection and quality assessment
During reviewing relevant papers, data extraction and analysis complied in accordance to the following standards: (1) The selected papers were studying physical exercise intervention’s effect on drug abuse, excluding preventive studies. (2) All research use RCT. (3) Objects of the study were adults over 18 years old who were assessed as alcohol, nicotine, and illicit drug abusers through the DSM-III(R)/IV. (4) Excluding the studies on acute exercise, we selected results from chronic physical exercise experimental studies. (5) The primary outcome measures in the study included the rate of abstinence from drug addiction, withdrawal symptoms, the level of depression, and anxiety. (6) The baseline of the primary outcome measures in the study and descriptive statistical data after intervention must be obtainable.
The Delphi List Criteria was used to [46] assess the quality of each literature included in the meta-analysis. Our literature evaluation criteria included: randomness of grouping, concealment of treatment allocation, homogeneity of baseline data, clarity of various standards, viability of using the blind method for outcome measurement, assessment tools for the main outcome, and intent treatment analysis. In the current research, items 6 and 7 in the Delphi List are not integrated in the assessment. When measuring the effect of physical exercise on SUD, treatment providers need to guide and monitor patients to execute physical exercise intervention, making a blind method impossible.
Data extraction and statistical analysis
We used an Excel spreadsheet to extract the data from the integrated literature. The data included information of participants, intervention of experimental and control groups, types of drug addiction, and primary outcome measurements. We conducted a meta-analysis through the meta package in R software (R 3.0.1 version) [47]. We used the odd ratio (OR) to assess the abstinence rate under two different conditions. Due to different follow-up intervals, we defined follow-up periods of 1–3 months, 4–7 months, and ≥8 months as short, middle, and long term, respectively. We evaluated the treatment effect by measuring abstinence rates at the end of physical exercise and throughout different follow-up periods, and then conducted a sub-group analysis based on different follow-up phases. We also employed the standardized mean difference (SMD) to assess withdrawal symptoms, depression, and anxiety after physical exercise intervention. The confidence interval was set at 95%. A p value less than 0.05 is referred to the level of statistical significance. We used Q-test and I 2-test to assess heterogeneity. If the p value in Q-test was less than 0.05 or if the I 2 index in I 2-test was more than 50%, the data was judged to achieve heterogeneity [48], [49]. If there was heterogeneity, the random effects model was chosen in the meta-analysis; otherwise, the fixed effects model was used. Given the heterogeneity in the study, we rendered sensitivity analysis. We employed the funnel plot visual, Egger’s test, and false safe number (Nfs0.05) to assess publication bias in the meta-analysis including more than ten papers [50]. In addition, we performed sub-group analysis according to certain characteristics of participants in the studies (physical exercise intensity, physical exercise type, addictive type, and follow-up period).
Authors WYQ and WYY completed the screening of the literature, data extraction, quality analysis, and statistical analysis process independently. Meetings were held regularly to minimize the risk of error in each link. In case of conflicts between two authors in any process, the final decision was made by another author.
Results
Included trials
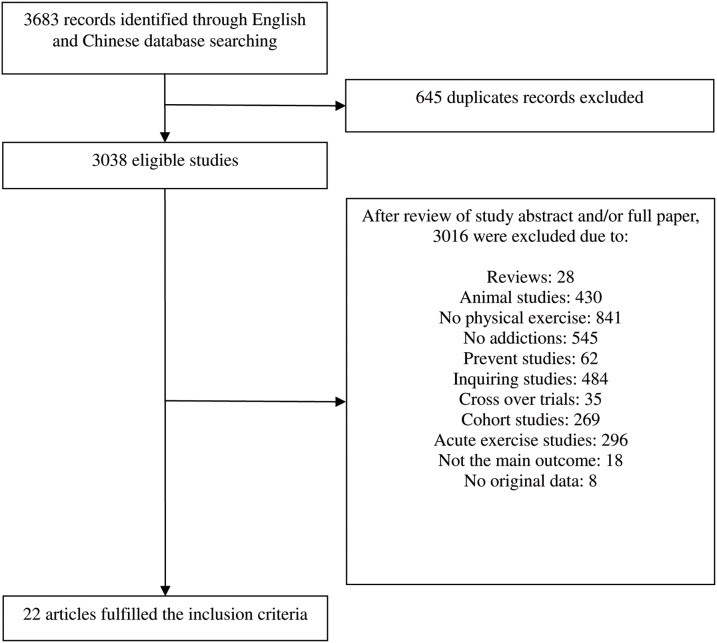
Based on the selection criteria, we derived 22 out of 3683 studies for meta-analysis. The flow diagram of identification, screening and the inclusion of studies was shown (see Figure 1). One doctoral dissertation was selected [26], and the original data of one study was provided by contacting the author [51]. Five papers from 22 studies investigated the treatment effects of physical exercise on illicit drug abusers [39], [51]–[54], eleven on nicotine abusers [27], [55]–[64], three on alcohol abusers [26], [65], [66], and four on polydrug abusers of alcohol, nicotine, and illicit drugs [26], [67]–[69]. Table 1 shows the specific characteristics of the included studies. Among all the studies, abstinence rate was regarded as the primary outcome measure with four reporting only the abstinence rate or abstinence population after physical exercise intervention [52], [53], [64], [67]. Other papers reported abstinence conditions immediately after intervention and in different follow-up periods. Moreover, five papers reported withdrawal symptoms [51]–[54], [57], seven papers described changes in anxiety levels before and after physical exercise intervention [26], [51], [53], [57], [63], [66], [69], and nine present variety in depression levels before and after physical exercise intervention [26], [27], [39], [53], [54], [63], [65], [66], [69].
Figure 1. Flow chart of trials used in the study.
Table 1. Characteristics of included studies.
| Article | Substance | Group | N | Age | Gender | Race | Physical Exercise | Outcomemeasure | ||||
| Type | Intensity | Duration | Frequency | Each time | ||||||||
| Burling (1992)[67] | Illicit drug,alcohol | Exp | 34 | 38.8 | 2.9%F | 50%Black;41%Caucasian | Softball | NR | 30 day | 1/Wks | NR | Abstinent ratea |
| Ctrl | 61 | NR | NR | NR | No Exercise | NR | 30 day | NR | NR | |||
| Marcus (1995)[55] | Nicotine | Exp | 10 | 39 | F | NR | Walking,rowing, cycleergometry | 70–85%HR max | 12 week | 3/Wks | 30–45 min | Abstinent ratea |
| Ctrl | 10 | 36 | F | NR | Educationmeeting | NR | 12 week | 1/Wks | 30–45 min | |||
| Donaghy (1997)[26] | Alcoholic, | Exp | 80 | 41.3 | 25%F | NR | Aerobicexercise,strengthening | NR | 3 week | 3/Wks | 30 min | Abstinent ratea; BDI; STAI(state) |
| Ctrl | 78 | 41.7 | 25%F | NR | Breathing | NR | 3 week | 3/Wks | 30 min | |||
| Martin (1997)[68] | Nicotine,alcohol,illicit drug | Exp | 72 | 40.5 | 43%F | 90.4%Caucasian | Walking | Moderate | 8 week | 3/Wks | 15–45 min | Abstinent ratea |
| Ctrl | 70 | 41.5 | 46%F | 95.7%Caucasian | Standardtreatment | NR | 8 week | NR | 60–70 min | |||
| Marcus (1999)[56] | Nicotine | Exp | 134 | 40.7 | F | NR | Walking,rowing, cycleergometry | 69–85%HR max | 12 week | 3/Wks | 40 min | Abstinent ratea |
| Ctrl | 147 | 39.7 | F | NR | Educationmeeting | NR | 12 week | 1/Wks | 30 min | |||
| Huang (2000a)[52] | Heroin | Exp | 60 | NR | 30%F | Asia/Chinese | Jogging | 40–70%VO2 max | 10 day | 3/Wks | 40–60 min | Withdrawal symptomsc; Abstinent ratea |
| Ctrl | 60 | NR | 33%F | Asia/Chinese | Daily life | 7–8 Borgb | 10 day | NR | NR | |||
| Huang (2000b)[53] | Heroin | Exp | 60 | 27.0 | 30%F | Asia/Chinese | Brisk walking | 50–60%VO2 max | 6 month | 3/Wks | 40–60 min | Withdrawal symptomsc; Abstinent ratea; SAS; SDS |
| Ctrl | 50 | 28.2 | 27%F | Asia/Chinese | Daily life | 9–10 Borgc | 6 month | NR | NR | |||
| Li (2002) [51] | Heroin | Exp | 34 | 33.3 | M | Asia/Chinese | Qi Gong | NR | 10 day | 4–5/D | 25–30 min | Withdrawal symptomsc; HAS |
| Ctrl | 26 | 31.7 | M | Asia/Chinese | NR | NR | 10 day | NR | NR | |||
| Ussher (2003)[57] | Nicotine | Exp | 154 | 41.5 | 53%F | 87.9%Caucasian | ‘Life-style’or morestructuredexercise | 40% HRmax | 6 week | 5/Wks | 5–30 min | Withdrawal symptomsd; Abstinent ratea MPSS |
| Ctrl | 145 | 44.4 | 53%F | 87.9%Caucasian | Healtheducation | NR | 6 week | 1/Wks | 5–30 min | |||
| Marcus (2005)[58] | Nicotine | Exp | 109 | 42.5 | F | 82.5%Caucasian; 6.9%Black | Aerobictraining | 50–69%HR max | 8 week | 4/Wks | 30–45 min | Abstinent ratea |
| Ctrl | 108 | 43.0 | F | 82.5%Caucasian; 6.9%Black | Healtheducation | NR | 8 week | NR | 30–45 min | |||
| Vedamurthachar (2006) [65] | Alcohol | Exp | 30 | 35.6 | M | NR | Sudarshana Kriya Yoga | NR | 2 week | NR | 60 min | BDI |
| Ctrl | 30 | 37.7 | M | NR | No intervention | NR | 2 week | NR | NR | |||
| Sareen (2007)[66] | Alcohol | Exp | 26 | 50 | 14%F | NR | Iyengar Yoga | NR | 12 week | 2/Wks | 60 min | POMS |
| Ctrl | 26 | 50 | 14%F | NR | Usual care | NR | 12 week | NR | NR | |||
| Prapavessis(2007) [59] | Nicotine | Exp | 76 | 37.9 | F | NR | Walking, rowing,cycle ergometry | 60–75%HR max | 12 week | 3/Wks | 45 min | Abstinent ratea |
| Ctrl | 66 | 38.2 | NR | NR | Cognitivebehavior therapy | NR | 12 week | NR | NR | |||
| Ussher (2007)[60] | Nicotine | Exp | 154 | 41.5 | 53%F | 87.9%Caucasian | ‘Life-style’ ormore structuredexercise | 40% HRmax | 6 week | 5/Wks | 5–30 min | Abstinent ratea |
| Ctrl | 145 | 44.4 | 53%F | 87.9%Caucasian | Health education | NR | 6 week | 1/Wks | 5–30 min | |||
| Kinnunen (2008)[61] | Nicotine | Exp | 92 | 38.3 | F | 81.5%Caucasian | Treadmill | 60–80%HR max | 19 week | 1–2/Wks | 30 min | Abstinent ratea |
| Ctrl | 34 | 39.9 | F | 75.8%Caucasian | Standard treatment | NR | 19 week | NR | 30 min | |||
| Vickers (2009)[27] | Nicotine | Exp | 30 | 41.8 | F | Caucasian | Exercise | NR | 10 week | 5/Wks | 30 min | Abstinent ratea; HRSD |
| Ctrl | 30 | 40.9 | F | 97%Caucasian | Health counseling | NR | 10 week | 1/Wks | 30 min | |||
| Williams (2010)[62] | Nicotine | Exp | 29 | 41.5 | F | 83.3%Caucasian | Treadmill | 70% HRmax | 8 week | 3/Wks | 50 min | Abstinent ratea |
| Ctrl | 30 | 43.3 | F | 86.7%Caucasian | Wellness videos | NR | 8 week | 3/Wks | 30 min | |||
| Bock (2012)[63] | Nicotine | Exp | 32 | 43.8 | F | 88%Caucasian | Yoga | NR | 8 week | 2/Wks | 60 min | Abstinent ratea; STAIT; CESD |
| Ctrl | 23 | 48.1 | F | 74%Caucasian | Wellness sessions | NR | 8 week | NR | NR | |||
| Whiteley (2012)[64] | Nicotine | Exp | 166 | 44.1 | F | NR | Aerobic &resistance training | 77–85%HR max | 12 week | 1/Wks | 40–60 min | Abstinent ratea |
| Ctrl | 164 | 42.9 | F | NR | Wellness session | NR | 12 week | NR | NR | |||
| Li (2013) [54] | Heroin | Exp | 17 | 30.3 | F | Asia/Chinese | Tai Chi | NR | 150 day | 1–2/D | 60 min | Withdrawal symptomsc; HRSD |
| Ctrl | 16 | 29.6 | F | Asia/Chinese | Daily life | NR | 150 day | NR | NR | |||
| Smelson (2013)[69] | Cocaine, alcohol | Exp | 51 | 30.6 | 4%F | 60%Caucasian; 35%Black | Qi Gong | NR | 14 day | 2–3/Wks | 15 min | SAIS(state); BDI |
| Ctrl | 50 | 40.4 | 4%F | 60%Caucasian; 35%Black | Sham Qi Gong | NR | 14 day | NR | 15 min | |||
| Zhuang (2013)[39] | Heroin | Exp | 37 | 29.1 | F | Asia/Chinese | Yoga | NR | 6 month | 5/Wks | 50 min | POMS(depression) |
| Ctrl | 38 | 27.8 | F | Asia/Chinese | Hospital routinecare | NR | 6 month | NR | NR | |||
Exp: Experimental; Ctrl: Control; F: Female subjects; NR: No Reported; HR: Heart Rate; VO2 max: maximal oxygen consumption; BDI: Beck Depression Inventory; SAIS: State-Trait Anxiety Inventory-State; TAIS: Trait Anxiety Inventory-State; SAS: Self-Rating Anxiety Scale; SDS: Self-rating depression scale; HAS: Hamilton Anxiety Scores; MPSS: Mood and Physical Symptoms Scale-anxiety; HRSD: Hamilton Rating Scale for Depression; CESD: Center for Epidemiologic Studies Depression Scale; POMS: Profile of Mood States.
Continual abstinence;
Borg index;
Rating scale of heroin withdrawal symptoms;
Tobacco withdrawal symptoms.
Methodological Quality of Included Studies
Delphi List Criteria, which assesses the quality of RCT methodology [46], was used for quality assessment of all studies. Scores of quality ranged from 4 to 7 (see Table 2), which indicated that the bias of the study was relatively low. Some authors did not clearly report the experimental information such as whether the assessment of outcome adopted the blind method, or if sufficient concealment was made in the allocation of participants.
Table 2. Assessment of Methodological Quality of Included Studies.
| Randomizationa | Similar atbaselineb | Criteriaspecifiedc | Assessorblindedd | Allocationconcealmente | Variabilityoutcomef | ITAg | Totalscore | |
| Burling (1992)[67] | Unknown | YES | YES | Unknown | YES | YES | YES | 5 |
| Marcus (1995)[55] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Donaghy (1997)[26] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Martin (1997)[68] | YES | YES | YES | Unknown | YES | YES | NO | 5 |
| Marcus (1999)[56] | YES | YES | YES | YES | Unknown | YES | YES | 6 |
| Huang (2000a)[52] | YES | YES | YES | YES | Unknown | YES | NO | 5 |
| Huang (2000b)[53] | YES | YES | YES | YES | Unknown | YES | YES | 6 |
| Li (2002) [51] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Ussher (2003)[57] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Marcus (2005)[58] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Char (2006)[65] | YES | YES | YES | YES | Unknown | YES | YES | 6 |
| Sareen (2007) [66] | YES | YES | YES | NO | Unknown | YES | YES | 5 |
| Prapavessis (2007)[59] | YES | YES | YES | YES | Unknown | YES | YES | 6 |
| Ussher (2007)[60] | YES | YES | YES | YES | YES | YES | YES | 7 |
| Kinnunen (2008)[61] | YES | YES | YES | Unknown | YES | YES | NO | 5 |
| Vickers (2009)[27] | YES | YES | YES | Unknown | YES | YES | NO | 5 |
| Williams (2010)[62] | YES | YES | YES | Unknown | Unknown | YES | NO | 4 |
| Bock (2012)[63] | YES | YES | YES | Unknown | Unknown | YES | YES | 5 |
| Whiteley (2012)[64] | YES | YES | YES | Unknown | YES | YES | YES | 6 |
| Li (2013)[54] | YES | YES | YES | Unknown | YES | YES | NO | 5 |
| Smelson (2013)[69] | YES | YES | YES | Unknown | Unknown | YES | NO | 4 |
| Zhuang (2013)[39] | YES | YES | YES | Unknown | YES | YES | NO | 5 |
Was randomization performed?
Were the groups similar at baseline regarding important prognostic indicators?
Were the eligibility criteria specified?
Was the outcome assessor blinded?
Was allocation concealment adequate?
Were point estimates and measures of variability presented for the primary outcome measures?
Did the analysis include an intention to treat analysis?
Effect of physical exercise on abstinence rate
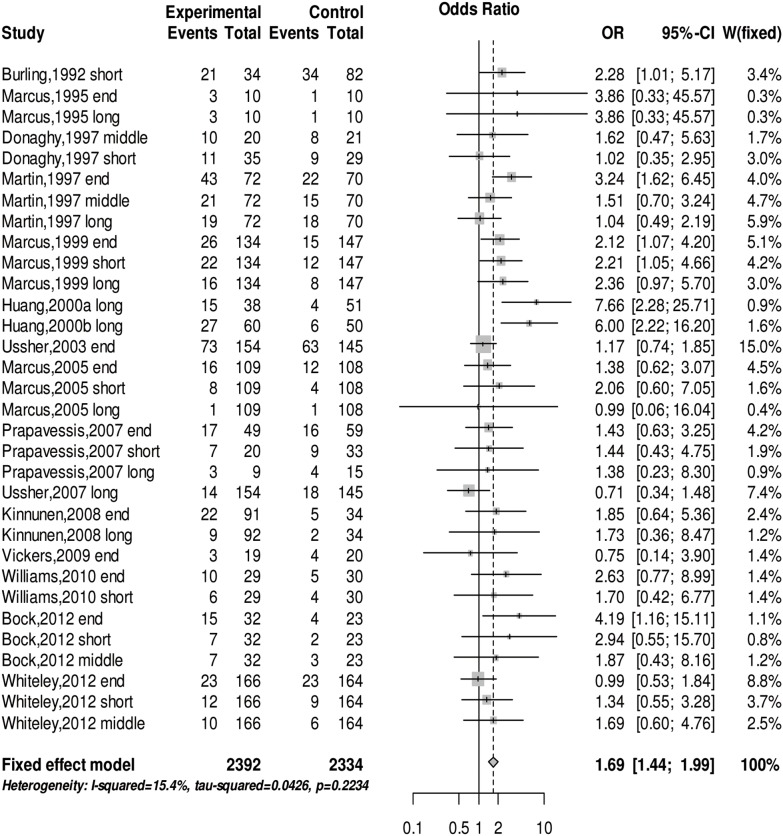
We conducted a meta-analysis of the abstinence rate for SUD at the end of the physical exercise treatment, the short-term (≤3 months), middle-term (4–7 months) and long-term (≥8 months) follow-up periods after the intervention. The Q test (Q(31) = 36.64, p = 0.22) and I2 test (I2 = 15.4%) revealed no heterogeneity in any of the studies. The meta-analysis of the fixed effects model shows that physical exercise can significantly increase the abstinence rate in subjects with SUD (OR = 1.69 (95% CI: 1.44, 1.99), z = 6.33, p<0.001) (see Figure 2). There was no evidence of publication bias upon using Egger’s test (z = 1.02, p = 0.31) and a false safe number (Nfs0.05 = 351). Table 3 shows the result of sub-group analysis indicating the effect of physical exercise intervention on the abstinence rate in various follow-up periods having no significant difference. The effect of physical exercise intensity and type of physical exercise on abstinence rate is not significantly different. However, there is strong evidence indicating the special effect of physical exercise on various addictive drugs. The treatment effect of physical exercise on drug abusers is better than its effect on alcohol and nicotine abusers (see Table 3).
Figure 2. The forest plot about the effect of physical exercise on abstinence rate.
The abstinence rate of past physical exercise treat, and differences follow-up periods were used odds ratio analysis.
Table 3. Sub-group analysis results.
| Sample size | N ofstudies | Meta-analytic effect size | Heterogeneity | ||||||
| (Exp/Ctrl) | SMD/OR(95%-CI) | Q(d.f.) | p | I2 | Q | ||||
| Abstinence rate | |||||||||
| Intensity type | |||||||||
| low | 96/69 | 3 | 2.96(1.29,6.83) | 1.91(2) | 0.3841 | 0% | 0.66 | ||
| moderate | 1193/1244 | 19 | 1.62(1.32,1.98) | 36.8% | 28.49 | ||||
| high | 1103/1021 | 10 | 1.71(1.28,2.29) | 0% | 5.47 | ||||
| Physical exercise type | |||||||||
| aerobic Ex | 2296/2265 | 29 | 1.65(1.40,1.95) | 1.82(1) | 0.177 | 17.9% | 34.10 | ||
| mind-body Ex | 96/69 | 3 | 2.96(1.29,6.83) | 0% | 0.66 | ||||
| Follow-up period | |||||||||
| end | 865/810 | 11 | 1.60(1.26,2.02) | 0.57(3) | 0.9027 | 23.8% | 13.12 | ||
| short-term | 559/616 | 8 | 1.79(1.25,2.56) | 0% | 2.65 | ||||
| middle-term | 290/278 | 4 | 1.62(0.96,2.71) | 0% | 0.07 | ||||
| long-term | 678/630 | 9 | 1.84(1.30,2.59) | 60.9% | 20.45 | ||||
| Addict type | |||||||||
| alcohol | 271/260 | 5 | 1.65(1.14,2.39) | 11.51(2) | 0.0032** | 33.1% | 5.98 | ||
| illicit drug | 132/183 | 3 | 4.13(2.39,7.14) | 43.9% | 3.56 | ||||
| nicotine | 1989/1891 | 24 | 1.51(1.24,1.83) | 0% | 16.40 | ||||
| Withdrawal symptoms | |||||||||
| Physical exercise type | |||||||||
| aerobic Ex | 274/255 | 3 | −1.67(−3.51, 0.17) | 0.71 (1) | 0.399 | 98.5% | 2.59 | ||
| mind-body Ex | 51/42 | 2 | −0.61(−2.25,1.03) | 92.6% | 1.30 | ||||
| Anxiety | |||||||||
| Addict type | |||||||||
| alcohol | 61/55 | 2 | −0.21(−0.58, 0.16) | 1.03(2) | 0.5975 | 37.9% | 1.61 | ||
| illicit drug | 145/126 | 3 | −0.40(−0.64, −0.16) | 0% | 1.41 | ||||
| nicotine | 186/168 | 2 | −0.26(−0.47, −0.05) | 0% | 0.13 | ||||
| Physical exercise type | |||||||||
| aerobic Ex | 249/224 | 3 | −0.29(−0.47, −0.11) | 0.06(1) | 0.8065 | 21.1% | 2.54 | ||
| mind-body Ex | 143/125 | 4 | −0.33(−0.57, −0.09) | 0% | 1.57 | ||||
| Depression | |||||||||
| Physical exercise type | |||||||||
| aerobic Ex | 132/117 | 3 | −0.43(−0.84, −0.03) | 0.04(1) | 0.838 | 59.4% | 4.93 | ||
| mind-body Ex | 186/175 | 6 | −0.50(−1.00, −0.01) | 81.5% | 27.03 | ||||
| Addict type | |||||||||
| alcohol | 91/85 | 3 | −0.77(−1.73,0.19) | 8.21(2) | 0.0165* | 89.2% | 18.52 | ||
| illicit drug | 165/154 | 4 | −0.51(−0.73, −0.28) | 0% | 2.81 | ||||
| nicotine | 62/53 | 2 | 0.10(−0.27, 0.46) | 0% | 0.01 | ||||
Exp: Experimental; Ctrl: Control; Ex: Exercise; SMD: Standardized Mean Difference; OR: Odds Ratio; CI: Confidence Interval.
*p<0.05, **p<0.01
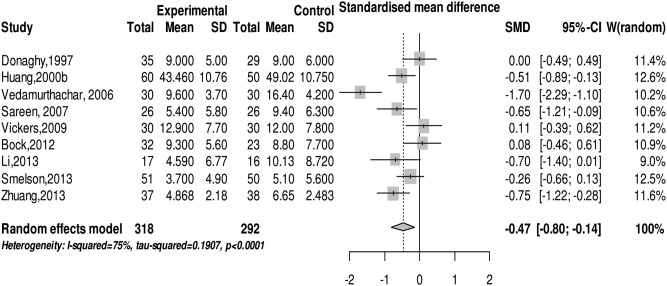
Effect of physical exercise on withdrawal symptoms
We conducted a meta-analysis on withdrawal symptoms in drug abusers after physical exercise intervention. The Q test (Q(4) = 151.4, p<0.001) and I2 test (I2 = 97.4%) showed heterogeneity in the included studies. We chose the random effects model in meta-analysis and the result indicates that exercise can significantly ease withdrawal symptoms in subjects with SUD (SMD = −1.24 (95% CI: −2.46, −0.02), z = −2.00, p<0.05) (see Figure 3). The sub-group analysis finds that different types of physical exercise affect withdrawal symptoms of SUD differently (see Table 3).
Figure 3. The forest plot about the effect of physical exercise on withdrawal symptoms.
Effect of physical exercise on anxiety levels in subjects with SUD
We employed a meta-analysis on anxiety levels in subjects with SUD after physical exercise intervention. No evidence of heterogeneity was found based on the result of the Q test (Q(6) = 4.17, p = 0.65) and I2 test (I2 = 0%). The meta-analysis of the fixed effects model showed that physical exercise can significantly attenuate anxiety symptoms in subjects with SUD (SMD = −0.31 (95% CI: −0.45, −0.16), z = −4.11, p<0.001) (see Figure 4). The sub-group analysis finds that different types of physical exercise do not have significantly different effects on anxiety symptoms of addicts, and physical exercise does not differently influence the anxiety symptoms of all kinds of SUD (see Table 3).
Figure 4. The forest plot about the effect of physical exercise on anxiety status.
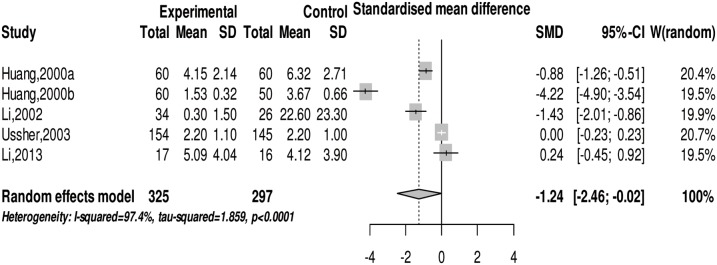
Effect of physical exercise on depression levels in subjects with SUD
We conducted a meta-analysis on the depression level in SUD after physical exercise intervention. There was moderate heterogeneity exhibited in the studies demonstrated by the Q test (Q(8) = 31.99, p<0.001) and I2 test (I2 = 75%). The random effects model meta-analysis showed that physical exercise can significantly relieve depression symptoms in SUD (SMD = −0.47 (95% CI: −0.80, −0.14), z = −2.76, p<0.01) (see Figure 5). The sub-group analysis indicated that the effect of physical exercise on the depression symptoms of SUD is not significantly different. However, physical exercise does have a significant relief effect on depression symptoms in alcohol and illicit drug abusers (see Table 3).
Figure 5. The forest plot about the effect of physical exercise on depression status.
Discussion
Summary of main results
Based on our knowledge, our statistical review of physical exercise in SUD is the first meta-analysis article on the treatment effects of chronic physical exercise on alcohol, nicotine, and illicit drugs in human studies. Our meta-analysis assesses the effects of various forms of physical exercises on SUD in the following four aspects: abstinence rate, withdrawal symptoms, anxiety, and depression level. Compared to the treatment effects on alcohol and nicotine abusers, chronic physical exercises can better increase the abstinence rate in illicit drugs abusers. Meanwhile, physical exercise (aerobic exercise and mind-body exercise) can effectively attenuate withdrawal symptoms and ease anxiety symptoms in alcohol, nicotine and illicit drug addictions, while physical exercise-induced improvement of depression symptoms was only observed in illicit drug abusers. Furthermore, there are no significant differences in exercise-induced treatment on SUD between exercise types (aerobics vs. mind-body exercise), nor among different levels of physical exercise intensities (low, moderate, and high intensity). Overall, physical exercise can effectively assist abusers with withdrawing from addictive drugs. The result of this meta-analysis is not only consistent with the previous meta-analysis results from a single acute physical exercise treatment for SUD [38], [70], but it also complies with the result of several review articles [18], [29], [32].
Specificity of physical exercise on different addictive drugs
There are three types of addictive substances included in this analysis. They are alcohol, nicotine, and illicit drugs that induce strong dependence in human beings and could result in abuse. Since the different addictive mechanisms of these three substances may be involved, we performed sub-group analyses on each addictive substance independently. Indeed, we found that exercise affects the abstinence rate of illicit drugs more than that of alcohol and nicotine abuse. The possible cause for this result may be the difference in addictive mechanisms for each of the three addictive substances. For example, opioid drugs (morphine, heroin, etc.) take effect through β-endorphin neurotransmitters activating the µ and δ opium receptors [71]. Alcohol takes effect through promoting the reaction of the GABAA receptor [72] and increasing stimulation to the dopamine and opiate receptor [73], [74]. Nicotine takes effect through acetylcholine neurotransmitters activating the α2β4nACh receptor [75]–[77].
Physical exercise intensity for effectively treating drug abuse
The sub-group analysis indicated no significant difference in the abstinence rate among low-, moderate-, and high-intensity long-term physical exercise. It is mean that all three exercise intensities induce similar levels of abstinence rate reduction in alcohol, nicotine and illicit drug abusers. Correspondingly, non-RCT studies presented that long-term treadmill exercise at moderate-intensity (55–69% HR max) can effectively ease the craving for cannabis [16] and increase abstinence rate of other drugs in SUD [17]. And non-RCT studies also show that high- and moderate-intensity long-term physical exercise can significantly treat alcohol abuse. A pilot study on the treatment effects of aerobics on alcohol abusers [78] reported that 35 minutes of moderate- (HR = 50–60% VO2max) to high-intensity (HR = 80–90% VO2max) physical exercise for six weeks, can significantly reduce depression symptoms in alcohol abusers. Another cross-over design study showed that moderate-intensity fast walking can significantly enhance self-management techniques in alcohol abusers [79], [80]. The results of the above-mentioned study further proved the findings of our meta-analysis. While the mechanisms underlying these results remain unclear, moderate- and high-intensity aerobic exercises have significant effects on SUD. Mind-body exercises are included as low-intensity physical exercise in this meta-analysis. Due to the different nature of mind-body exercises compared to classical running and walking, we have included the analyses of mind-body exercises in SUD independently in the sections below.
Persistency of treatment effects of physical exercise on SUD
To investigate the long lasting effects of exercise on SUD, we conducted a sub-group analysis to evaluate the treatment effects of physical exercise in different follow-up periods. As shown in Table 3, there is no significant difference in exercise-induced reduction of the abstinence rate among the different follow-up periods,suggesting that physical exercise leaves a long lasting treatment effect on SUD. The results of two meta-analyses [36], [37] studies have also shown obvious treatment effects in 3 and 12 months follow-up periods. These results are likely due to the long lasting effect of physical exercise on changes in brain structure and function. For instance,studies showed that physical exercise can regulate the gene transcription of endogenous opium brain-derived neurotrophic factor (BDNF) by activating the cyclic AMP response element-binding (CREB) protein [81] and synaptic plasticity [82], [83], which is critical for rehabilitation for patients with SUD via promoting repair of drug-induced neuronal damage [84] and improving corresponding brain functions [85]. This neuronal structural change induced by exercises might contribute a long lasting effect on SUD.
Different effects of various forms of physical exercises
In addition to aerobic exercises, mind-body exercises are also acceptable and easy to apply in treatment for drug abuse. The sub-group analysis showed that mind-body exercises and aerobic exercises induce similar beneficial effects on the abstinence rate, withdrawal symptoms, anxiety, and depression levels in subjects with SUD (see Table 3). The outcome from our analysis is consistent with previously published literatures, suggesting that mind-body exercises can also effectively facilitate the treatment of drug addiction [35].
In terms of exercise intensity, some studies have shown that the intensity of Tai Chi Quan is about 52–63% HR max [86], which is similar to low- or moderate-intensity aerobic exercises [87]–[89]. Meanwhile, Qigong [90] and Yoga [91], [92] are also regarded as low- and moderate-intensity physical exercises. Therefore, both mind-body exercise and aerobic exercise show similar beneficial effects on drug addiction when administered at low- or moderate-intensities as shown in Table 3. In addition to exercise intensity, the particular characteristics of mind-body exercise, namely meditation and breathing exercises, may be the key reasons for producing significant exercise effectiveness [93], [94].
Physical exercise inducing emotional improvement in SUD
The meta-analysis indicates that physical exercise can effectively ease anxiety and depression symptoms in subjects with SUD. The sub-group analysis shows that physical exercises reduce anxiety symptoms in nicotine, alcohol and illicit drug abusers, while significant exercise-induced improvement on depression symptoms was only found in alcohol and illicit drug abusers (see Table 3). Our findings are consistent with previously published review articles which also found that physical exercise can effectively ease anxiety symptoms in subjects with SUD [29], [32], [95].
However, we also included three studies that reported that physical exercise did not reduce depression symptoms in nicotine and alcohol abusers [27], [63]. As the number of the RCT studies included in our meta-analysis is limited, it is insufficient to make a valid conclusion of whether exercise reduces depression symptoms in subjects with SUD. However, some review articles claim that physical exercise could attenuate depression symptoms in alcohol and nicotine abusers based on non-RCT studies [32], [70]. Hence, subsequent studies are needed for further evidence of the effect of exercise on altering depression symptoms in SUD.
Limitations
There are some limitations that need to be considered in the current meta-analysis: (1) Addictive drugs involved in the studies often include participants with polydrug use disorders. Therefore, the specific treatment of exercise on a single drug abuse is difficult to analyze. Because there are insufficient RCT studies on exercise as an intervention for alcohol and drug abuse, the results in the present meta-analysis study may need further investigation. (2) Due to the limitation of available studies, only published RCT studies from 1990 to 2013 were included. There were no unpublished papers and dissertations found. These limitations in the literature collection may cause publishing bias. (3) Some papers lack clear explanations on the study information. Such limitation affected the quality of study and the assessment of clinic-relevant data. (4) In the research, some studies comprised of mostly female participants, whereas male participants accounted for only a small part. We were unable to evaluate the differences in gender through a statistical method due to difficulty in obtaining individual data. Accordingly, compared with males, female participants have more difficulty in giving up drug addiction [95]. (5) The main outcome indices in meta-analysis include abstinence rate, withdrawal symptoms, anxiety, and depression levels; the assessment tools in the literature also varied. (6) The included studies have some risk of bias. Lacking of assessor blinding and allocation concealment was the most frequent shortcoming of these studies (See Table 2). Other limitations included the small sample size of two studies [54], [55]. Although we adopted some methods (e.g., continuous variable adopts standardization mean difference method) for the assessment, certain biases listed above still exist.
Conclusions
The current meta-analysis provides strong evidence that physical exercise can be an effective adjunct treatment method for abstinence from alcohol, nicotine, and illicit drugs in abusers. Physical exercise not only increases the abstinence rate in subjects with SUD, but also eases withdrawal symptoms, anxiety, and depression symptoms. The treatment effects of physical exercise in these four aspects verify that physical exercise guidance by the American College of Sports Medicine (ACSM) [12] is an effective means for drug abstinence. Additionally, mind-body exercises (including Tai Chi Quan, Qigong, and Yoga) have similar treatment effects as to aerobic exercise. Although physical exercise has been proven effective in facilitating drug abstinence, its effects on alcohol, nicotine and illicit drug abusers are different. From the results of the meta-analysis, the effects of physical exercise on illicit drugs abusers are significantly greater compared to the others. Given the limitation of materials, these issues require further investigation.
Supporting Information
PRISMA Checklist.
(DOC)
Acknowledgments
The authors would like to thank all of the other authors for the research in which this meta-analysis was based upon; especially PhD Kevin Chen for original data resources support.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the Supporting Information files.
Funding Statement
This work was supported by the ISP grant (No. 13490503600) from Scientific and Technological Commission of Shanghai, National Science Foundation of China (No. 31171004), and the Project of Scientific and Technological Innovation grant (No. yjscx201324) from Shanghai University of Sport. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.WHO (2013) Management of substance abuse. World Health Organization.
- 2.CNNCC (2013) Annual Report on Drug Control in China 2013. Beijing: Ministry of Public Security.
- 3.UNODC (2012) World Drug Report 2012. United Nations Publication.
- 4. Deng Q, Tang Q, Schottenfeld RS, Hao W, Chawarski MC (2012) Drug use in rural China: a preliminary investigation in Hunan Province. Addiction 107: 610–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Joseph H, Stancliff S, Langrod J (2000) Methadone Maintenance Treatment (MMT):A Review of Historical and Clinical Issues. The Mount Sinai Journal of Medicine 67: 347–364. [PubMed] [Google Scholar]
- 6.Mattick RP, Kimber J, Breen C, Davoli M (2014) Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane database of systematic reviews.
- 7. Fischer B, Rehm J, Rgen U, Kim G, Kirst M (2004) Eyes wide shut?–A conceptual and empirical critique of methadone maintenance treatment. European addiction research 11: 1–14. [DOI] [PubMed] [Google Scholar]
- 8. Maruyama A, Macdonald S, Borycki E, Zhao J (2013) Hypertension, chronic obstructive pulmonary disease, diabetes and depression among older methadone maintenance patients in British Columbia. Drug and alcohol review 32: 412–418. [DOI] [PubMed] [Google Scholar]
- 9. Fareed A, Casarella J, Amar R, Vayalapalli S, Drexler K (2009) Benefits of retention in methadone maintenance and chronic medical conditions as risk factors for premature death among older heroin addicts. Journal of Psychiatric Practice 15: 227–234. [DOI] [PubMed] [Google Scholar]
- 10. Wapf V, Schaub M, Klaeusler B, Boesch L, Stohler R, et al. (2008) The barriers to smoking cessation in Swiss methadone and buprenorphine-maintained patients. Harm reduction journal 5: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Corbin CB, Pangrazi RP, Franks BD (2000) Definitions: Health, Fitness, and Physical Activity. President's Council on Physical Fitness and Sports Research Digest.
- 12.Thompson WR, Gordon NF, Pescatello LS (2009) ACSM's guidelines for exercise testing and prescription: Hubsta Ltd. [DOI] [PubMed]
- 13. Weinstock J, Wadeson HK, VanHeest JL (2012) Exercise as an adjunct treatment for opiate agonist treatment: review of the current research and implementation strategies. Substance Abuse 33: 350–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ströhle A, Höfler M, Pfister H, Müller AG, Hoyer J, et al. (2007) Physical activity and prevalence and incidence of mental disorders in adolescents and young adults. Psychological medicine 37: 1657–1666. [DOI] [PubMed] [Google Scholar]
- 15. Korhonen T, Kujala UM, Rose RJ, Kaprio J (2009) Physical activity in adolescence as a predictor of alcohol and illicit drug use in early adulthood: a longitudinal population-based twin study. Twin Research and Human Genetics 12: 261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Buchowski MS, Meade NN, Charboneau E, Park S, Dietrich MS, et al. (2011) Aerobic exercise training reduces cannabis craving and use in non-treatment seeking cannabis-dependent adults. PLoS One 6: e17465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, et al. (2010) A pilot study of aerobic exercise as an adjunctive treatment for drug dependence. Mental health and physical activity 3: 27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sarah EL, Joseph TC, Michael U, Bess HM (2013) Exercise-based smoking cessation interventions among women. Women's Health 9: 69–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Brown RA, Abrantes AM, Read JP, Marcus BH, Jakicic J, et al. (2009) Aerobic Exercise for Alcohol Recovery: Rationale, Program Description, and Preliminary Findings. Behavior modification 33: 220–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Miladi GH, Rashidy PA, Fathollahi Y (2012) Anxiety profile in morphine-dependent and withdrawn rats: effect of voluntary exercise. Physiology & behavior 105: 195–202. [DOI] [PubMed] [Google Scholar]
- 21. Lynch WJ, Piehl KB, Acosta G, Peterson AB, Hemby SE (2010) Aerobic exercise attenuates reinstatement of cocaine-seeking behavior and associated neuroadaptations in the prefrontal cortex. Biol Psychiatry 68: 774–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sanchez V, Moore C, Brunzell D, Lynch W (2013) Effect of wheel-running during abstinence on subsequent nicotine-seeking in rats. Psychopharmacology 227: 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Thanos PK, Stamos J, Robison LS, Heyman G, Tucci A, et al. (2013) Daily treadmill exercise attenuates cocaine cue-induced reinstatement and cocaine induced locomotor response but increases cocaine-primed reinstatement. Behav Brain Res 239: 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Engelmann AJ, Aparicio MB, Kim A, Sobieraj JC, Yuan CJ, et al. (2013) Chronic wheel running reduces maladaptive patterns of methamphetamine intake: regulation by attenuation of methamphetamine-induced neuronal nitric oxide synthase. Brain Structure and Function 219: 657–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hashemi Nosrat Abadi T, Vaghef L, Babri S, Mahmood AM, Beirami M (2013) Effects of different exercise protocols on ethanol-induced spatial memory impairment in adult male rats. Alcohol 47: 309–316. [DOI] [PubMed] [Google Scholar]
- 26.Donaghy ME (1997) The investigation of exercise as an adjunct to the treatment and rehabilitation of the problem drinker: University of Glasgow.
- 27. Vickers KS, Patten CA, Lewis BA, Clark MM, Ussher M, et al. (2009) Feasibility of an exercise counseling intervention for depressed women smokers. Nicotine & tobacco research 11: 985–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hillman CH, Drobes DJ (2012) Physical Activity and Cognitive Control: Implications for Drug Abuse. Child Development Perspectives 6: 367–373. [Google Scholar]
- 29. Lynch WJ, Peterson AB, Sanchez V, Abel J, Smith MA (2013) Exercise as a novel treatment for drug addiction: A neurobiological and stage-dependent hypothesis. Neuroscience & Biobehavioral Reviews 37: 1622–1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pareja GH, Sanchis GF, Mayero S (2013) Exercise as an adjuvant intervention in opiate dependence. Substance Abuse 34: 87–88. [DOI] [PubMed] [Google Scholar]
- 31. Smith MA, Lynch WJ (2012) Exercise as a potential treatment for drug abuse: evidence from preclinical studies. Frontiers in Psychiatry 2: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zschucke E, Heinz A, Strohle A (2012) Exercise and physical activity in the therapy of substance use disorders. ScientificWorldJournal 2012: 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khanna S, Greeson JM (2013) A narrative review of yoga and mindfulness as complementary therapies for addiction. Complementary therapies in medicine 21: 244–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Posadzki P, Choi J, Lee MS, Ernst E (2014) Yoga for addictions: a systematic review of randomised clinical trials. Focus on Alternative and Complementary Therapies 19: 1–8. [Google Scholar]
- 35. Carim TL, Mitchell SH, Oken BS (2013) Mind–body practices: An alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug and alcohol dependence 132: 399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ussher M H TA, Faulkner G (2008) Exercise interventions for smoking cessation. Cochrane Database of Systematic Reviews. [DOI] [PubMed]
- 37. Ussher MH, Taylor A, Faulkner G (2012) Exercise interventions for smoking cessation. Cochrane Database Syst Rev 1: 1–50. [DOI] [PubMed] [Google Scholar]
- 38. Haasova M, Warren F, Ussher M, VanRensberg K, Faulkner GC, et al. (2013) The acute effects of physical activity on cigarette cravings Systematic review and meta-analysis with individual participant data (IPD). Addiction 108: 26–37. [DOI] [PubMed] [Google Scholar]
- 39. Zhuang SM, An SH, Zhao Y (2013) Yoga Effects on Mood and Quality of Life in Chinese Women Undergoing Heroin Detoxification, a Randomized Controlled Trial Nursing Research. 62: 260–268. [DOI] [PubMed] [Google Scholar]
- 40.Pattison LP, McIntosh S, Sexton T, Childers SR, Hemby SE (2014) Changes in dopamine transporter binding in nucleus accumbens following chronic self-administration cocaine: Heroin combinations. Synapse. [DOI] [PMC free article] [PubMed]
- 41. Hopkins ME, Davis FC, Vantieghem MR, Whalen PJ, Bucci DJ (2012) Differential effects of acute and regular physical exercise on cognition and affect. Neuroscience 215: 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McMorris T, Graydon J (2000) The effect of incremental exercise on cognitive performance. International Journal of Sport Psychology 31: 66–81. [Google Scholar]
- 43. Swain RA, Harris AB, Wiener EC, Dutka MV, Morris HD, et al. (2003) Prolonged exercise induces angiogenesis and increases cerebral blood volume in primary motor cortex of the rat. Neuroscience 117: 1037–1046. [DOI] [PubMed] [Google Scholar]
- 44. van Praag H (2008) Neurogenesis and exercise: past and future directions. Neuromolecular medicine 10: 128–140. [DOI] [PubMed] [Google Scholar]
- 45. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 46. Verhagen AP, de Vet HC, de Bie RA, Kessels AG, Boers M, et al. (1998) The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of clinical epidemiology 51: 1235–1241. [DOI] [PubMed] [Google Scholar]
- 47.Team RC (2013) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing.
- 48. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ: British Medical Journal 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Higgins J, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Statistics in medicine 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 50. Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. Bmj 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Li M, Chen K, Mo Z (2002) Use of qigong therapy in the detoxification of heroin addicts. Alternative Therapies in Health and Medicine 8: 50–59. [PubMed] [Google Scholar]
- 52. Huang H, Yang F, Yang SS, Xiao DS, Nie AH, et al. (2000) Influence of aerobic training on recovery of herion sddicts. Chinese Journal of Physical Therapy 23: 267–270. [Google Scholar]
- 53. Huang H, Yang F (2000) Exercise therapy adjuvant treatment of herion dependence on clinical observation. Chinese Journal of Drug Abuse Prevention and Treatment 26: 30–31. [Google Scholar]
- 54. Li DX, Zhuang XY, Zhang YP, Guo H, Wang Z, et al. (2013) Effects of Tai Chi on the Protracted Abstinence Syndrome: A Time Trial Analysis. The American journal of Chinese medicine 41: 43–57. [DOI] [PubMed] [Google Scholar]
- 55. Marcus BH, Albrecht AE, Niaura RS, Taylor ER, Simkin LR, et al. (1995) Exercise enhances the maintenance of smoking cessation in women. Addictive Behaviors 20: 87–92. [DOI] [PubMed] [Google Scholar]
- 56. Marcus BH, Albrecht AE, King TK, Parisi AF, Pinto BM, et al. (1999) The efficacy of exercise as an aid for smoking cessation in women: a randomized controlled trial. Archives of Internal Medicine 159: 1229–1235. [DOI] [PubMed] [Google Scholar]
- 57. Ussher M, West R, McEwen A, Taylor A, Steptoe A (2003) Efficacy of exercise counselling as an aid for smoking cessation: a randomized controlled trial. Addiction 98: 523–532. [DOI] [PubMed] [Google Scholar]
- 58. Marcus BH, Lewis BA, Hogan J, King TK, Albrecht AE, et al. (2005) The efficacy of moderate-intensity exercise as an aid for smoking cessation in women: a randomized controlled trial. Nicotine Tob Res 7: 871–880. [DOI] [PubMed] [Google Scholar]
- 59. Prapavessis H, Cameron L, Baldi JC, Robinson S, Borrie K, et al. (2007) The effects of exercise and nicotine replacement therapy on smoking rates in women. Addict Behav 32: 1416–1432. [DOI] [PubMed] [Google Scholar]
- 60. Ussher M, West R, McEwen A, Taylor A, Steptoe A (2007) Randomized controlled trial of physical activity counseling as an aid to smoking cessation: 12 month follow-up. Addict Behav 32: 3060–3064. [DOI] [PubMed] [Google Scholar]
- 61. Kinnunen T, Leeman RF, Korhonen T, Quiles ZN, Terwal DM, et al. (2008) Exercise as an adjunct to nicotine gum in treating tobacco dependence among women. Nicotine & Tobacco Research 10: 689–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Williams DM, Whiteley JA, Dunsiger S, Jennings EG, Albrecht AE, et al. (2010) Moderate intensity exercise as an adjunct to standard smoking cessation treatment for women: a pilot study. Psychology of Addictive Behaviors 24: 349–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bock BC, Fava JL, Gaskins R, Morrow KM, Williams DM, et al. (2012) Yoga as a complementary treatment for smoking cessation in women. J Womens Health (Larchmt) 21: 240–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Whiteley JA, Williams DM, Dunsiger S, Jennings EG, Ciccolo JT, et al. (2012) YMCA commit to quit: randomized trial outcomes. Am J Prev Med 43: 256–262. [DOI] [PubMed] [Google Scholar]
- 65. Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna D, et al. (2006) Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. Journal of affective disorders 94: 249–253. [DOI] [PubMed] [Google Scholar]
- 66. Sareen S, Kumari V, Gajebasia KS, Gajebasia NK (2007) Yoga: a tool for improving the quality of life in chronic pancreatitis. World Journal of Gastroenterology 13: 391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Burling TA, Seidner AL, Robbins-Sisco D, Krinsky A, Hanser SB (1992) Batter up! Relapse prevention for homeless veteran substance abusers via softball team participation. Journal of Substance Abuse 4: 407–413. [DOI] [PubMed] [Google Scholar]
- 68. Martin JE, Calfas KJ, Patten CA, Polarek M, Hofstetter CR, et al. (1997) Prospective evaluation of three smoking interventions in 205 recovering alcoholics: One-year results of Project SCRAP-Tobacco. Journal of Consulting and Clinical Psychology 65: 190–194. [DOI] [PubMed] [Google Scholar]
- 69. Smelson D, Chen KW, Ziedonis D, Andes K, Lennox A, et al. (2013) A Pilot Study of Qigong for Reducing Cocaine Craving Early in Recovery. The Journal of Alternative and Complementary Medicine 19: 97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Roberts V, Maddison R, Simpson C, Bullen C, Prapavessis H (2012) The acute effects of exercise on cigarette cravings, withdrawal symptoms, affect, and smoking behaviour: systematic review update and meta-analysis. Psychopharmacology (Berl) 222: 1–15. [DOI] [PubMed] [Google Scholar]
- 71. Sarkar DK, Sengupta A, Zhang C, Boyadjieva N, Murugan S (2012) Opiate antagonist prevents µ-and δ-opiate receptor dimerization to facilitate ability of agonist to control ethanol-altered natural killer cell functions and mammary tumor growth. Journal of Biological Chemistry 287: 16734–16747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Silveri MM (2014) GABAergic contributions to alcohol responsivity during adolescence: Insights from preclinical and clinical studies. Pharmacology & Therapeutics 143: 197–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Gilman JM, Ramchandani VA, Davis MB, Bjork JM, Hommer DW (2008) Why we like to drink: a functional magnetic resonance imaging study of the rewarding and anxiolytic effects of alcohol. The Journal of Neuroscience 28: 4583–4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Berrettini W (2013) Opioid pharmacogenetics of alcohol addiction. Alcohol: Science, Policy and Public Health 3: 97–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Dajas-Bailador F, Wonnacott S (2004) Nicotinic acetylcholine receptors and the regulation of neuronal signalling. Trends in pharmacological sciences 25: 317–324. [DOI] [PubMed] [Google Scholar]
- 76. Coe JW, Brooks PR, Vetelino MG, Wirtz MC, Arnold EP, et al. (2005) Varenicline: an α4β2 nicotinic receptor partial agonist for smoking cessation. Journal of medicinal chemistry 48: 3474–3477. [DOI] [PubMed] [Google Scholar]
- 77. Sala M, Braida D, Pucci L, Manfredi I, Marks MJ, et al. (2013) CC4, a dimer of cytisine, is a selective partial agonist at α4β2/α6β2 nAChR with improved selectivity for tobacco smoking cessation. British journal of pharmacology 168: 835–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Roessler KK, Bilberg R, Jensen K, Kjaergaard A-S, Dervisevic A, et al. (2013) Exercise as Treatment for Alcohol Dependence. Sport Science Review 22: 205–216. [Google Scholar]
- 79. Taylor AH, Oh H, Cullen S (2013) Acute effect of exercise on alcohol urges and attentional bias towards alcohol related images in high alcohol consumers. Mental Health and Physical Activity 6: 220–226. [Google Scholar]
- 80. Karoly HC, Stevens CJ, Thayer RE, Magnan RE, Bryan AD, et al. (2013) Aerobic Exercise Moderates the Effect of Heavy Alcohol Consumption on White Matter Damage. Alcoholism: Clinical and Experimental Research 37: 1508–1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Koo JW, Mazei-Robison MS, Chaudhury D, Juarez B, LaPlant Q, et al. (2012) BDNF is a negative modulator of morphine action. science 338: 124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Gomez PF, Hillman C (2013) The Influence of Exercise on Cognitive Abilities. Comprehensive Physiology 3: 403–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Coelho FG, Gobbi S, Andreatto CA, Corazza DI, Pedroso RV, et al. (2013) Physical exercise modulates peripheral levels of brain-derived neurotrophic factor (BDNF): a systematic review of experimental studies in the elderly. Arch Gerontol Geriatr 56: 10–15. [DOI] [PubMed] [Google Scholar]
- 84. Thomas AG, Dennis A, Bandettini PA, Johansen-Berg H (2012) The effects of aerobic activity on brain structure. Frontiers in psychology 3: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Lin TW, Kuo YM (2013) Exercise Benefits Brain Function: The Monoamine Connection. Brain Sciences 3: 39–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lan C, Lai JS, Chen SY, Wong MK (1998) 12-month Tai Chi training in the elderly: its effect on health fitness. Medicine and Science in Sports and Exercise 30: 345–351. [DOI] [PubMed] [Google Scholar]
- 87. Ahn S, Song R (2012) Effects of Tai Chi Exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. The Journal of Alternative and Complementary Medicine 18: 1172–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Wu Y, Wang Y, Burgess EO, Wu J (2013) The effects of Tai Chi exercise on cognitive function in older adults: A meta-analysis. Journal of Sport and Health Science 2: 193–203. [Google Scholar]
- 89. Pan L, Yan J, Guo Y, Yan J (2013) Effects of Tai Chi training on exercise capacity and quality of life in patients with chronic heart failure: a meta-analysis. European journal of heart failure 15: 316–323. [DOI] [PubMed] [Google Scholar]
- 90. Kjos V, Etnier JL (2006) Pilot study comparing physical and psychological responses in medical qigong and walking. Journal of aging and physical activity 14: 241–253. [DOI] [PubMed] [Google Scholar]
- 91. DiPietro L, Seeman TE, Stachenfeld NS, Katz LD, Nadel ER (1998) Moderate-intensity aerobic training improves glucose tolerance in aging independent of abdominal adiposity. Journal of the American Geriatrics Society 46: 875–879. [DOI] [PubMed] [Google Scholar]
- 92. Ward S, McCluney N, Bosch P (2013) Heart Rate Response to Vinyasa Yoga in Healthy Adults. J Yoga Phys Ther 3: 1–15. [Google Scholar]
- 93. Khalsa SBS, Khalsa GS, Khalsa HK, Khalsa MK (2008) Evaluation of a residential Kundalini yoga lifestyle pilot program for addiction in India. Journal of ethnicity in substance abuse 7: 67–79. [DOI] [PubMed] [Google Scholar]
- 94. Elibero A, Janse Van Rensburg K, Drobes DJ (2011) Acute effects of aerobic exercise and Hatha yoga on craving to smoke. Nicotine Tob Res 13: 1140–1148. [DOI] [PubMed] [Google Scholar]
- 95. Kinnunen TH, Korhonen T, Craft LL, Perna FM (2010) Treating tobacco dependence in women with exercise: Review on effectiveness and mechanisms. International Journal of Sport and Exercise Psychology 8: 48–60. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA Checklist.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the Supporting Information files.