Abstract
Context
Novel mobile assessment and intervention capabilities are changing the face of physical activity (PA) research. A comprehensive systematic review of how mobile technology has been used for measuring PA and promoting PA behavior change is needed.
Evidence acquisition
Article collection was conducted using six databases from February to June 2012 with search terms related to mobile technology and PA. Articles that described the use of mobile technologies for PA assessment, sedentary behavior assessment, and/or interventions for PA behavior change were included. Articles were screened for inclusion and study information was extracted.
Evidence synthesis
Analyses were conducted from June to September 2012. Mobile phone–based journals and questionnaires, short message service (SMS) prompts, and on-body PA sensing systems were the mobile technologies most utilized. Results indicate that mobile journals and questionnaires are effective PA self-report measurement tools. Intervention studies that reported successful promotion of PA behavior change employed SMS communication, mobile journaling, or both SMS and mobile journaling.
Conclusions
mHealth technologies are increasingly being employed to assess and intervene on PA in clinical, epidemiologic, and intervention research. The wide variations in technologies used and outcomes measured limit comparability across studies, and hamper identification of the most promising technologies. Further, the pace of technologic advancement currently outstrips that of scientific inquiry. New adaptive, sequential research designs that take advantage of ongoing technology development are needed. At the same time, scientific norms must shift to accept “smart,” adaptive, iterative, evidence-based assessment and intervention technologies that will, by nature, improve during implementation.
Context
Increasing physical activity (PA) and decreasing sedentary behavior is protective for a number of conditions, including obesity,1 diabetes,2 heart disease,3 depression,4 and some cancers.5 However, recent studies show conclusively that most young people and adults in the U.S. do not meet the recommended PA guidelines.6 Further, extensive amounts of time spent in sedentary behavior poses multiple threats to health.7 The success of traditional interventions to improve PA and decrease sedentary behavior has been inconsistent,8 and most interventions do not scale.9
Mobile health (mHealth) has emerged as an important field for disease management, health behavior assessment, and health behavior interventions. Mobile and connected technologies have been adopted for these purposes because they offer novel approaches to measurement and intervention methodologies. Moreover, mobile phones are used ubiquitously across age groups and populations, suggesting that mobile technologies might offer cost-effective and acceptable implementation tools for health behavior change and maintenance.
More than 85% of U.S. adults own mobile phones.10 Additionally, 77% of youth aged 12–17 years own mobile phones,11 an increase from 45% in 2004.12 The pervasive nature of mobile technology lends mHealth tools the ability to fit seamlessly into people’s everyday lives, providing avenues for novel ways to assess behavior in free-living settings. Coupled with on-body sensing devices, mobile phones can collect and transmit objective, real-time behavioral and biofeedback data.13,14 These rich data can provide insight into people’s behaviors in a context-specific manner. mHealth offers novel ways for interventionists, researchers, and healthcare providers to communicate directly with individuals, opening up the potential to provide constant reminders and immediate feedback in an adaptive, just-in-time manner.15–19
Further, mHealth assessments and interventions can implement features that are not only acceptable but also enjoyable for individuals to use, including mobile applications, mobile games, SMS messaging, and self-monitoring tools.20 These features enable mHealth to move care and intervention programs toward implementation and adoption for long-term behavior change maintenance, which is crucial in the face of the low levels of PA and high levels of sedentary behavior in the U.S. populations, the related epidemic of obesity and chronic conditions,21–23 and the resulting economic burden on healthcare systems.24,25 mHealth technologies are poised to address the shortcomings of current assessment and intervention techniques.
The current review focuses on studies that use mobile technology for activity assessment and activity promotion. Previous reviews have focused on computer- and Internet-based interventions for PA26–30; eHealth (e-mail, website, and SMS-based) interventions for PA31,32 and/or dietary behavior change33; and active video games to increase PA in youth.34 Additionally, two reviews35,36 provide overviews of the use of mobile technology for various health outcomes. One review to date has focused on mobile technology used specifically for PA interventions, emphasizing efficacy of and user satisfaction with text message–based interventions.37 It focuses largely on interventions for weight management, and includes seven articles that were published between January 2005 and August 2010. A recent meta-analysis of 11 studies examined the efficacy of mobile devices to influence PA behavior.38 No reviews to date have included mobile technologies for PA and sedentary behavior assessment as well as interventions.
Therefore, the aim of the current review was to provide a comprehensive assessment of mobile technologies employed for both of these purposes. Further, this review provides an update of studies published through June 2012 and includes 13 articles that have not been assessed in previous reviews of mobile technologies for PA interventions.39–51 Considering the fast pace with which technology develops and the fact that the mHealth field is quickly expanding, an updated and expanded review is warranted. This systematic review focused on addressing the following questions:
Which mobile technologies have been used for PA and sedentary behavior detection and PA promotion?
Which mobile technologies are effective for PA and sedentary behavior measurement and interventions?
Have mobile technologies been harnessed for their potential to provide real-time feedback in adaptive behavioral interventions?
How feasible are mobile technologies for PA measurement and PA and sedentary behavior interventions?
Evidence Acquisition
Data Sources and Search Strategy
Articles were identified from searches in PubMed, Google Scholar, Web of Knowledge, Ovid Healthstar, and IEEE Xplore databases, as well as from references cited in reviewed articles and searches of relevant journals during February to June 2012. The following search term was used: ((mobile phone OR cell phone OR text message OR SMS OR short message service OR internet OR web OR e-mail OR electronic mail) AND (physical activity OR active OR physical fitness OR exercise OR sedentary OR inactiv*)). The search terms internet, web, e-mail, and electronic mail were included to account for the possibility of studies using these technologies via mobile platforms to measure PA or implement interventions for PA or sedentary behavior. Studies that were published in English as journal articles or conference proceedings; described more than one participant; and described the use of mobile phones for PA assessment, sedentary behavior assessment, and/or PA or sedentary behavior interventions were considered for review.
Inclusion/Exclusion Criteria
To be considered for full review, articles had to include a sample of youth or adults and meet at least one of the following inclusion criteria:
Usability, feasibility, or evaluation studies describing mobile technology for PA or sedentary behavior self-report
Usability, feasibility, evaluation, or intervention studies describing SMS messaging for communication about PA or sedentary behavior
Usability, feasibility, or evaluation studies describing mobile technology for objective PA or sedentary behavior detection
Intervention studies describing mobile technology used to influence PA or sedentary behavior
Articles that described e-mail or website-based PA assessment or promotion that was not implemented using mobile technology were not included because they did not describe how mobile technologies could be utilized to implement the assessment or intervention. Although users may not differentiate between mobile and web-based platforms, this is an important distinction in the sphere of mHealth research. Web-based platforms are not necessarily mobile-accessible to all users, so web-based content delivered via computers could have different characteristics and elicit different user responses than web-based content delivered via mobile devices. Additionally, articles that described only designs or engineering proofs, but not the testing of designs with users, were not considered for review.
Identification of Relevant Studies
Articles were screened and questions about eligibility were discussed and resolved. Potential articles were identified by first screening the title and then the abstract. Articles that were considered potentially relevant from title and abstract screenings were screened in full for final consideration.
Summarizing Study Findings
Analyses were conducted June–September 2012. Information about study characteristics (Appendix A, available online at www.ajpmonline.org) was extracted from the reviewed articles. For PA behavior change outcomes, findings were considered significant if the p-value was <0.05. For studies that did not include PA behavior change as a main outcome, usability, feasibility, or other main findings were reported.
Study Quality Assessment
A critical assessment of the reviewed studies was conducted using the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool.52 This quality-assessment tool has six subscales, including participant selection bias, study design, confounding, blinding, data collection methods, and participant withdrawals and drop-outs. The subscales pertaining to study design, confounding, and blinding are appropriate evaluation metrics for intervention studies but not for non-intervention studies. Therefore, a modified version of the assessment tool excluding these subscales was used for non-intervention studies. Quality scores were assigned to the studies (Appendix A, available online at www.ajpmonline.org).
Evidence Synthesis
Included/Excluded Articles
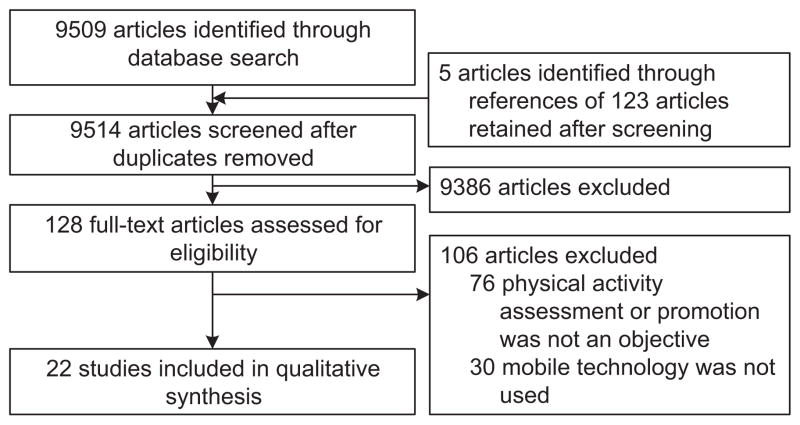
As of June 16, 2012, a total of 9509 articles were returned in the search results. After reviewing the titles and abstracts of the search returns, 128 articles were considered for full review. A final sample of 22 articles that met the inclusion/ exclusion criteria was included in this review (Figure 1).
Figure 1.
Flow diagram of selection process of articles for inclusion in the review
Types of Mobile Technologies Utilized
Seventeen (77%) of the reviewed studies described mobile technologies for PA promotion.39,41,42,45–49,51,53–60 Twelve of these used mobile technologies to implement PA interventions42,46,48,49,51,53,55–60; others39,41,45,47,54 aimed to evaluate usability and feasibility of PA-promoting mobile systems. The remaining five40,43,44,50,61 of the reviewed studies tested mobile technologies for PA assessment.
Mobile journals or questionnaires, featured in 11 (50%) studies,40,42,43,46,47,49–51,53,57,61 were the most commonly used mobile technologies. They were tested for both PA measurement40,43,50,61 and PA behavior change through self-monitoring.42,46,47,49,51,53,57 Mobile journals were followed by SMS messaging, which was used in eight (36%) studies.46,48,51,55,56,58–60 SMS messaging was used in these studies to encourage PA behavior change with automated messages46,51,56,58–60 or personalized SMS messages.48,55 None of the reviewed studies used SMS for PA measurement. On-body activity-sensing systems were described in five (23%) studies.39,41,44,45,54 (The number of studies in these categories does not equal 22, as seven studies40,41,45,46,50,51,61 [32%] employed more than one mobile technology.)
Study Quality Assessment
Of the 22 studies reviewed, seven39,41,45,50,51,59,61 received weak quality ratings, nine42,44,46,47,53–55,57,60 received moderate quality ratings, and six40,43,48,49,56,58 received strong quality ratings.
Of the 12 studies that used mobile technologies for PA interventions, two51,59 had weak quality, six42,46,53,55,57,60 had moderate quality, and four48,49,56,58 had strong quality. Of the five studies that aimed to evaluate usability and feasibility of PA-promoting mobile systems, three39,41,45 received weak quality ratings and two47,54 received moderate quality ratings. Two50,61 of the five studies that tested mobile technologies for PA assessment had weak quality, whereas one had moderate quality44 and two had strong quality.40,43
Efficacy of Mobile Technologies for Physical Activity and Sedentary Behavior Measurement
Six studies (27%), four40,43,46,50 that used mobile journals or questionnaires and two44,54 that used mobile on-body sensing systems, assessed whether the mobile technologies they used were suitable for PA and sedentary behavior measurement. Each of the studies40,43,46,50 that evaluated mobile PA journals or questionnaires compared data collected via these methods with data collected by validated PA measurement tools. According to the results from these comparisons, self-report of PA and sedentary behavior using mobile journals or questionnaires agreed with validated assessment tools.
Of the two studies44,54 that tested the efficacy of on-body sensing systems, one44 tested the ability of the system to accurately detect real-time PA states, and one54 tested the ability of the system to correctly infer activities in real time. The study44 that used a system to detect PA states found that the system was 94% accurate in PA state detection compared to in-lab activity observations. The study54 that used a system to infer activities found that 61% of activities recorded by participants were correctly inferred by the on-body sensing system.
Efficacy of Mobile Technologies for Physical Activity and Sedentary Behavior Change
Of the 12 studies that used mobile technologies to influence PA behavior, nine (75%) reported significant changes in PA42,46,53,55–58,60 or sedentary behavior.49 These studies employed SMS communication to promote PA,55,56,58,60 PA self-monitoring through mobile journaling,42,49,53,57 or both SMS and journaling.46
Intervention tailoring using mobile technologies was featured in six of the interventions.48,49,51,53,55,59 Tailoring strategies included displays of personal PA data and progress toward PA goals,51,53 personally tailored SMS messages,48,55 and personalized feedback to self-reported data.48,49,59 PA behavior change results from interventions that used tailoring techniques were mixed. Three of these studies49,53,55 reported behavior change outcomes. Two studies48,59 reported no changes in PA behaviors, and one51 did not report statistical results. Although four studies39,41,45,54 described on-body mobile systems that provided real-time feedback about PA behavior to users, which could be used to implement personalized, adaptive interventions, none of the studies tested these mobile systems for efficacy of PA or sedentary behavior change.
Usability, Acceptability, and Feasibility Outcomes
The majority of the reviewed studies aimed to determine directions for future work through evaluation outcomes related to usability, feasibility, or acceptability. One or more of these outcomes was featured in 14 (64%) studies.39–43,45,47,48,54,55,57,59–61 Usability and acceptability were assessed through participant interviews,39,48,54 questionnaires,41,57,61 and tasks to test participant performance with the mobile technology.45 Responses for usability were mixed, varying from 58% of participants agreeing that a mobile journal was easy to use61 to all participants agreeing that an on-body sensing system was easy to use.39 The studies that reported acceptability assessment outcomes revealed that on-body sensing systems,54 mobile journals,43,47 and SMS messaging48,59 received positive acceptability ratings from participants.
The results of feasibility assessments demonstrate that mobile platforms for journals and SMS messaging can be feasible for PA measurement and for implementation of PA interventions. Two studies assessed the feasibility of mobile journals for PA measurement.40,43 They found positive feasibility outcomes for use of mobile journals to collect self-reported PA compared to energy expenditure estimated by doubly labeled water and indirect calorimetry40 and PA measured by accelerometer.43 Additionally, one study42 that used a mobile journal and three studies48,55,60 that used SMS messaging determined that these mobile technologies are feasible ways to deliver PA interventions. None of the studies that employed on-body sensing systems assessed feasibility, so the literature does not provide evidence of the feasibility of on-body systems for PA measurement or interventions.
Discussion
A variety of mobile technologies have been used in mHealth PA assessment and promotion studies, including mobile journaling, SMS messaging, and on-body sensing systems. Positive feasibility findings from studies that measured these outcomes indicate that mobile journals and SMS messaging are viable measurement and intervention tools. However, on-body sensing systems lack evidence for feasibility of PA measurement and intervention delivery, so research is needed to determine how viable mobile on-body sensing systems are for these purposes. The fact that usability of mobile technologies across modalities received mixed results from study participants indicates that research is also necessary to determine the features of mobile PA measurement and intervention technologies that are functional for users.
The literature demonstrates that mobile technologies have largely been adopted as isolated components and have not yet been integrated into comprehensive systems for use in interventions. However, mHealth PA research has demonstrated some efficacy for measuring PA and for influencing PA behavior and sedentary behavior change. Mobile journals and questionnaires were found to be effective for PA measurement compared to validated PA measurement tools.40,43,46,50 Of the six studies that tested these mobile technologies for PA measurement efficacy, five received strong40,43 or moderate44,46,54 quality ratings, which lends support to these findings. However, only two of the studies that described mobile on-body sensing systems tested the systems for accuracy of PA and sedentary behavior detection.44,54
The mixed results from these studies indicate that more research is needed to understand how on-body sensing technologies can be used for accurate PA and sedentary behavior measurement. Additionally, SMS,55,56,58,60 mobile journaling,42,49,53,57 or both SMS and journaling46 were used to deliver several successful interventions. All of the studies that reported significant PA or sedentary behavior changes received strong49,56,58 or moderate42,46,53,55,57,60 quality ratings. The qualities and outcomes of these studies suggest that SMS and mobile journaling can be used to implement effective PA interventions.
Although evidence62 suggests that tailoring may strengthen the efficacy of behavior change interventions, few of the interventions used these technologies to deliver personalized interventions or real-time feedback. Moreover, behavior change outcomes from PA interventions that used tailoring strategies were mixed. This may have been due in part to the variable quality of studies that employed tailored interventions, as the studies that had positive behavioral outcomes were strong49 or moderate,54,55 whereas those that did not had weak quality ratings.50,59 Tailoring of mHealth PA interventions using real-time feedback could provide context-specific, just-in-time support for behavior change. Evidence from the education literature supports the benefits of immediate feedback; studies63,64 have demonstrated that immediate feedback can enhance learning and improve behavioral outcomes. Because mobile technologies have the capabilities for real-time feedback, this tailoring strategy should be explored as a way to potentially improve mHealth PA intervention efficacy.
Gaps can be identified between current implementations and utilizing mHealth technologies to their full potential for measuring activities in real time and providing personalized, adaptive feedback to users. Mobile on-body sensing was the most seldom-used mobile technology. Despite the increasing capability of mobile on-body sensors to facilitate real-time, personalized feedback to users in adaptive interventions, none of the studies in this review used this mobile technology to change PA or sedentary behavior.
The studies that did describe mobile on-body sensing technologies tested the systems with small sample sizes for usability and feasibility and did not include PA behavior change as a main outcome.39,41,44,45,54 Future mobile technology use in this field should integrate various components (SMS messaging, self-reported diaries, on-body sensors, real-time data exchange, integrative technologies for incorporating sensor data, ecologic momentary assessment, and geospatial data, for example) for adaptive and iterative interventions that can provide personalized, real- or near-time feedback to users based on situational and behavioral contexts.
The potential for integrated mHealth systems for PA and sedentary behavior measurement and promotion is promising, but is in need of further research and development. mHealth research does not yet provide the evidence base to indicate how fully integrated mobile systems that incorporate sensing capabilities and real-time or near-time data transmission can be utilized to influence PA behavior and sedentary behavior change. Additionally, the lack of pervasive use of personalization and real-time feedback in mHealth studies creates difficulty in determining how these components can be most successfully used in mHealth interventions to influence behavior change.
Further, the lag time between the fast pace of technology development and the slow pace of research funding and designs such as the RCT needs to be closed by developing and implementing innovative funding scaffolding and research designs that promote rapid turnaround. Adaptive experimental designs such as the Multiphase Optimization Strategy (MOST) and the Sequential Multiple Assignment Randomized Trial (SMART) could provide study design and evaluation methods that are suited to the iterative development and evaluation of mHealth interventions.65 Utilization of innovative study design could improve understanding of the mobile technologies that are most effective for PA and sedentary behavior measurement and interventions.
Limitations
There are limitations to this review, some of which are inherent to the nascent field of mHealth. For instance, there is a lack of consensus on the types of PA targeted and the implementation of mobile technologies. It is therefore difficult to compare studies or to derive a definitive understanding of “best practices” in mobile technology implementation for behavior change.
Additionally, most studies were conducted over short periods of time. The lack of longitudinal examination in the reviewed studies also renders it impossible to determine whether these technologies are feasible for long-term PA behavior change maintenance in free-living settings. Moreover, most of the studies reviewed focus only on PA and not on sedentary behavior. Decreased sedentary behavior is categorically different from increased PA, as these two activity patterns are not necessarily reciprocal.66,67 Research has shown that too much sedentary behavior, even when one achieves recommended PA, has adverse health consequences.7 There is increasing evidence that sedentary behavior should be targeted for health interventions, so this is an outcome that requires attention in future mHealth research.1
Conclusion
The objectives of this literature review were to determine how mobile technologies have been used for PA and sedentary behavior detection and PA promotion, whether these technologies have been harnessed for their potential to provide real-time feedback in adaptive behavioral interventions, and whether mobile technologies have been successfully utilized to change PA and sedentary behavior. This review found that the mobile technologies utilized to develop mHealth PA and sedentary behavior assessment and promotion systems have included: mobile phone-based journals and questionnaires, SMS correspondence for self-monitoring of PA or communication about activities, and on-body activity sensing systems for PA detection and promotion. Several studies have shown that mobile PA journals and questionnaires are effective tools for measuring self-reported PA.
Additionally, there is a lack of evidence of the efficacy of on-body mobile sensing systems for accurate PA measurement. Several studies have demonstrated that use of SMS-based and mobile journal–based interventions can positively affect PA and sedentary behavior. However, these technologies have been predominantly utilized in isolation. mHealth systems that integrate mobile technologies to provide real-time feedback, user-and health-provider-in-the-loop, personalized, and adaptive interventions need to be developed and tested for efficacy in order to take full advantage of mobile and connected capabilities.
Supplementary Material
Acknowledgments
The authors thank Ariel Hart for her assistance in the preliminary phases of this literature review. Funding for this study was received from NCMHD (supplement to P60 MD002254-01).
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version at, http://dx.doi.org/10.1016/j.amepre.2013.05.012.
Footnotes
No financial disclosures were reported by the authors of this paper.
References
- 1.Jakicic JM. The effect of physical activity on body weight. Obesity. 2012;17(S3):S34–S38. doi: 10.1038/oby.2009.386. [DOI] [PubMed] [Google Scholar]
- 2.Jeon CY, Lokken RP, Hu FB, Van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30(3):744–52. doi: 10.2337/dc06-1842. [DOI] [PubMed] [Google Scholar]
- 3.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: an updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008;15(3):247–57. doi: 10.1097/HJR.0b013e3282f232ac. [DOI] [PubMed] [Google Scholar]
- 4.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Prev Med. 2008;46(5):397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Steindorf K, Leitzmann MF, Friedenreich CM. Physical activity and primary cancer prevention. In: Ulrich CM, et al., editors. Exercise, energy balance, and cancer. Vol. 6. New York: Springer; 2012. pp. 83–106. [Google Scholar]
- 6.Physical Activity Guidelines Advisory Committee report, 2008. To the secretary of Health and Human Services, Part A: executive summary. Nutr Rev. 2009;67(2):114–20. doi: 10.1111/j.1753-4887.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- 7.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobiac LJ, Vos T, Barendregt JJ. Cost-effectiveness of interventions to promote physical activity: a modelling study. PLoS Med. 2009;6(7):e1000110. doi: 10.1371/journal.pmed.1000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Estabrooks PA, Gyurcsik NC. Evaluating the impact of behavioral interventions that target physical activity: issues of generalizability and public health. Psychol Sport Exerc. 2003;4(1):41–55. [Google Scholar]
- 10.Pew Internet and American Life Project. Trend data (adults) 2012 pewinternet.org/Trend-Data-(Adults)/Device-Ownership.aspx.
- 11.Pew Internet and American Life Project. Trend data (teens) 2011 pewinternet.org/Static-Pages/Trend-Data-(Teens)/Teen-Gadget-Ownership.aspx.
- 12.Pew Internet and American Life Project. Teens and mobile phones. 2010 pewinternet.org/Reports/2010/Teens-and-Mobile-Phones/Summary-of-findings.aspx.
- 13.Patrick K, Griswold W, Raab F, Intille S. Health and the mobile phone. Am J Prev Med. 2008;35(2):177–81. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atienza AA, Patrick K. Mobile health: the killer app for cyber infrastructure and consumer health. Am J Prev Med. 2011;40(5S2):S151–S153. doi: 10.1016/j.amepre.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Bickmore T, Gruber A, Intille S. Just-in-time automated counseling for physical activity promotion. AMIA Annu Symp Proc. 2008:880. [PubMed] [Google Scholar]
- 16.Intille SS. Ubiquitous computing technology for just-in-time motivation of behavior change. Stud Health Technol Inform. 2004;107(Pt 2):1434–7. [PubMed] [Google Scholar]
- 17.Intille SS, Kukla C, Farzanfar R, Bakr W. Just-in-time technology to encourage incremental, dietary behavior change. AMIA Annu Symp Proc. 2003:874. [PMC free article] [PubMed] [Google Scholar]
- 18.Intille SS, Larson K, Kukla C. Just-in-time context-sensitive questioning for preventative health care. Proceedings of the AAAI 2002 Workshop on Automation as Caregiver: The Role of Intelligent Technology in Elder Care; 2002. [Google Scholar]
- 19.Intille SS, Kukla C, Farzanfar R, Bakr W. Just-in-time technology to encourage incremental, dietary behavior change. AMIA Annual Symposium Proceedings; American Medical Informatics Association; 2003; p. 874. [PMC free article] [PubMed] [Google Scholar]
- 20.Gotsis M, Hua Wang H, Spruijit-Metz D, Jordan-Marsh M, Valente T. Wellness partners: the design and evaluation of a web-based physical activity diary with social gaming features for adults. JMIR Res Protoc. 2013;2(1):e10. doi: 10.2196/resprot.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long term weight control. Obes Res. 2012;12(S12):151S–162S. doi: 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- 22.Ewbank PP, Darga LL, Lucas CP. Physical activity as a predictor of weight maintenance in previously obese subjects. Obes Res. 2012;3(3):257–63. doi: 10.1002/j.1550-8528.1995.tb00146.x. [DOI] [PubMed] [Google Scholar]
- 23.Haskell WL, Blair SN, Hill JO. Physical activity: health outcomes and importance for public health policy. Prev Med. 2009;49(4):280–2. doi: 10.1016/j.ypmed.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Obesity outranks both smoking and drinking in its deleterious effects on health and health costs. Health Aff. 2002;21(2):245–53. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 25.Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–41. doi: 10.1111/j.1467-789X.2009.00712.x. [DOI] [PubMed] [Google Scholar]
- 26.Hamel LM, Robbins LB, Wilbur J. Computer- and web-based interventions to increase preadolescent and adolescent physical activity: a systematic review. J Adv Nurs. 2011;67(2):251–68. doi: 10.1111/j.1365-2648.2010.05493.x. [DOI] [PubMed] [Google Scholar]
- 27.Marcus BH, Ciccolo JT, Sciamanna CN. Using electronic/computer interventions to promote physical activity. Br J Sports Med. 2009;43(2):102–5. doi: 10.1136/bjsm.2008.053744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsai HM, Chee W, Im EO. Internet methods in the study of women’s physical activity. Stud Health Technol Inform. 2006;122:396–400. [PubMed] [Google Scholar]
- 29.van den Berg MH, Schoones JW, Vliet Vlieland TP. Internet-based physical activity interventions: a systematic review of the literature. J Med Internet Res. 2007;9(3):e26. doi: 10.2196/jmir.9.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vandelanotte C, Spathonis KM, Eakin EG, Owen N. Website-delivered physical activity interventions a review of the literature. Am J Prev Med. 2007;33(1):54–64. doi: 10.1016/j.amepre.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 31.Laplante C, Peng W. A systematic review of e-health interventions for physical activity: an analysis of study design, intervention characteristics, and outcomes. Telemed J E Health. 2011;17(7):509–23. doi: 10.1089/tmj.2011.0013. [DOI] [PubMed] [Google Scholar]
- 32.Lau PW, Lau EY, Wong del P, Ransdell L. A systematic review of information and communication technology-based interventions for promoting physical activity behavior change in children and adolescents. J Med Internet Res. 2011;13(3):e48. doi: 10.2196/jmir.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med. 2007;33(4):336–45. doi: 10.1016/j.amepre.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Foley L, Maddison R. Use of active video games to increase physical activity in children: a (virtual) reality? Pediatr Exerc Sci. 2010;22(1):7–20. doi: 10.1123/pes.22.1.7. [DOI] [PubMed] [Google Scholar]
- 35.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–98. doi: 10.1016/j.jbi.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–40. doi: 10.1089/tmj.2008.0099. [DOI] [PubMed] [Google Scholar]
- 37.Stephens J, Allen J. Mobile phone interventions to increase physical activity and reduce weight: a systematic review. J Cardiovasc Nurs. 2013;28(4):320–9. doi: 10.1097/JCN.0b013e318250a3e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fanning J, Mullen PS, McAuley E. Increasing physical activity with mobile devices: a meta-analysis. J Med Internet Res. 2012;14(6):e161. doi: 10.2196/jmir.2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Anderson I, Maitland J, Sherwood S, et al. Shakra: tracking and sharing daily activity levels with unaugmented mobile phones. Mobile Networks Appl. 2007;12(2–3):185–99. [Google Scholar]
- 40.Bexelius C, Löf M, Sandin S, Lagerros YT, Forsum E, Litton JE. Measures of physical activity using cell phones: validation using criterion methods. J Med Internet Res. 2010;12(1):e2. doi: 10.2196/jmir.1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buttussi F, Chittaro L. Smarter phones for healthier lifestyles: an adaptive fitness game. IEEE Pervasive Comput. 2010;9(4):51–7. [Google Scholar]
- 42.David P, Buckworth J, Pennell ML, Katz ML, DeGraffinreid CR, Paskett ED. A walking intervention for postmenopausal women using mobile phones and Interactive Voice Response. J Telemed Telecare. 2012;18(1):20–5. doi: 10.1258/jtt.2011.110311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dunton GF, Liao Y, Intille SS, Spruijt-Metz D, Pentz M. Investigating children’s physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity (Silver Spring) 2011;19(6):1205–12. doi: 10.1038/oby.2010.302. [DOI] [PubMed] [Google Scholar]
- 44.Emken BA, Li M, Thatte G, et al. Recognition of physical activities in overweight Hispanic youth using KNOWME Networks. J Phys Act Health. 2012;9(3):432–41. doi: 10.1123/jpah.9.3.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fujiki Y, Kazakos K, Puri C, Buddharaju P, Pavlidis I, Levine J. NEAT-o-Games: blending physical activity and fun in the daily routine. Comput Entertain (CIE) 2008;6(2):21. [Google Scholar]
- 46.Fukuoka Y, Kamitani E, Dracup K, Jong SS. New insights into compliance with a mobile phone diary and pedometer use in sedentary women. J Phys Act Health. 2011;8(3):398–403. doi: 10.1123/jpah.8.3.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mattila E, Parkka J, Hermersdorf M, et al. Mobile diary for wellness management‚ results on usage and usability in two user studies. IEEE Trans Inf Technol Biomed. 2008;12(4):501–12. doi: 10.1109/TITB.2007.908237. [DOI] [PubMed] [Google Scholar]
- 48.Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 49.Spring B, Schneider K, McFadden HG, et al. Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology. Arch Intern Med. 2012;172(10):789–96. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sternfeld B, Jiang SF, Picchi T, Chasan-Taber L, Ainsworth B, Quesenberry CP., Jr Evaluation of a cell phone-based physical activity diary. Med Sci Sports Exerc. 2012;44(3):487–95. doi: 10.1249/MSS.0b013e3182325f45. [DOI] [PubMed] [Google Scholar]
- 51.Toscos T, Faber A, An S, Gandhi M. Chick clique: persuasive technology to motivate teenage girls to exercise. CHI Conf Proc. 2006 [Google Scholar]
- 52.Effective Public Health Practice Project. Effective public health practice quality assessment tool. 2004 www.city.hamilton.on.ca/phcs/EPHPP/
- 53.Consolvo S, Everitt K, Smith I, Landay JA. Design requirements for technologies that encourage physical activity. CHI Conf Proc; Montréal, Canada. April 22–27; 2006. pp. 457–66. [Google Scholar]
- 54.Consolvo S, Mcdonald D, Toscos T, et al. Activity sensing in the wild: a field trial of UbiFit garden. CHI Conf Proc; 2008. [Google Scholar]
- 55.Fjeldsoe BS, Miller YD, Marshall AL. MobileMums: a randomized controlled trial of an SMS-based physical activity intervention. Ann Behav Med. 2010;39(2):101–11. doi: 10.1007/s12160-010-9170-z. [DOI] [PubMed] [Google Scholar]
- 56.Hurling R, Catt M, Boni MD, et al. Using internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res. 2007;9(2):e7. doi: 10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kirwan M, Duncan MJ, Vandelanotte C, Mummery WK. Using smart-phone technology to monitor physical activity in the 10,000 Steps program: a matched case-control trial. J Med Internet Res. 2012;14(2):e55. doi: 10.2196/jmir.1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Prestwich A, Perugini M, Hurling R. Can implementation intentions and text messages promote brisk walking? A randomized trial. Health Psychol. 2010;29(1):40. doi: 10.1037/a0016993. [DOI] [PubMed] [Google Scholar]
- 59.Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008;40(6):385–91. doi: 10.1016/j.jneb.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sirriyeh R, Lawton R, Ward J. Physical activity and adolescents: an exploratory randomized controlled trial investigating the influence of affective and instrumental text messages. Br J Health Psychol. 2010;15 (4):825–40. doi: 10.1348/135910710X486889. [DOI] [PubMed] [Google Scholar]
- 61.Lee W, Chae YM, Kim S, Ho SH, Choi I. Evaluation of a mobile phone-based diet game for weight control. J Telemed Telecare. 2010;16(5):270–5. doi: 10.1258/jtt.2010.090913. [DOI] [PubMed] [Google Scholar]
- 62.Krebs P, Prochaska JO, Rossi JS. A meta-analysis of computer-tailored interventions for health behavior change. Prev Med. 2010;51(3):214–21. doi: 10.1016/j.ypmed.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Boyce BA, Markos NJ, Jenkins DW, Loftus JR. How should feedback be delivered? J Phys Educ Recreat Dance. 1996;67(1):18–22. [Google Scholar]
- 64.Butler DL, Winne PH. Feedback and self-regulated learning: a theoretical synthesis. Rev Educ Res. 1995;65(3):245–81. [Google Scholar]
- 65.Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5S):S112–S118. doi: 10.1016/j.amepre.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. Int J Obes (Lond) 2005;29(S2):S84–S96. doi: 10.1038/sj.ijo.0803064. [DOI] [PubMed] [Google Scholar]
- 67.Reilly JJ, McDowell ZC. Physical activity interventions in the prevention and treatment of paediatric obesity: systematic review and critical appraisal. Proc Nutr Soc. 2003;62(3):611–9. doi: 10.1079/PNS2003265. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.