Abstract
Background and Purpose
Ultrasound imaging (USI) has been shown to be a reliable measure for direct assessment of the lumbar multifidi among younger adults. However, given age- and chronic low back pain (CLBP)- related spinal changes, similar studies are needed prior to clinical use of USI among older adults with CLBP. The goals of this study were to evaluate intra- and inter-examiner reliability for USI assessment of multifidi thickness at rest and during a contraction and to determine standard error of measurement values (SEMs) and minimal detectable change values (MDCs) among older adults with CLBP.
Methods
Thirty-one adults, aged 60 to 85 years, with CLBP were recruited. Two examiners performed USI assessments of multifidus thickness at rest and during a contralateral lower extremity lift. Intraclass correlation coefficients (ICCs) were used to estimate inter- and intra-examiner reliability. SEMs and MDCs were calculated.
Results
All USI measurement techniques demonstrated excellent within-day, inter-examiner procedural reliability (ICCs: 0.82–0.85) and good-to-excellent between-days, inter-examiner procedural reliability (ICCs: 0.72–0.79). SEMs ranged from 0.36–0.46 centimeters (cm); MDCs ranged from 1.01–1.26 cm. Regardless of the measurement technique, examiner 1, the more experienced examiner, demonstrated lower SEMs and MDCs than examiner 2.
Discussion
Lower ICCs, greater SEMs, and greater MDCs for USI multifidus thickness assessment in older adults with CLBP when compared to previously published, procedural reliability results for younger adults with and without low back pain, may indicate that imaging is more challenging in this patient population. Factors, such as examiner training and participant anthropometrics, may impact reliability.
Conclusions
Good-to-excellent intra- and inter-examiner USI procedural reliability may provide clinicians a direct assessment technique for clinical evaluation of the lumbar multifidi in older adults with CLBP. SEMs and MDCs may allow for accurate interpretation of USI assessments in this population.
Keywords: chronic low back pain, multifidus, ultrasound imaging
INTRODUCTION
Among community-dwelling older adults, low back pain is associated with reduced health-related quality-of-life and function.1 According to the American Geriatric Society, “pain management is most successful when the underlying cause of pain is identified and treated”.2 Unfortunately, the majority of chronic low back pain (CLBP) in older adults is “non-specific”, defined as tension, soreness, and/or stiffness in the lower back region for which a specific cause of the pain cannot be identified.3 While we may not be able to identify a specific cause of low back pain in older adults, it is possible that concurrent age-related4–6 and CLBP-related changes7,8 of the spinal system may play a role in symptom presentation.9 Therefore, establishment of reliable assessment approaches to evaluate spinal morphology are needed for older adults with CLBP.
Age- and CLBP-related changes may affect posterior trunk muscles, including the erector spinae10 and the lumbar multifidi,4,5 which play a role in dynamic spinal stability.10,11 Specifically, findings of muscle atrophy and increased intramuscular fat both in the presence of aging4–6 and low back pain7,8,12–17 may impact muscle function and physical performance.6,7,18 In the clinical setting, assessments of posterior trunk muscles may focus on extensor strength and/or endurance. Extensor strength, which has been associated with falls19 and quality-of-life20 in older adults, is typically assessed using dynamometry; however, dynamometry may not be optimal for documenting change over time secondary to learning effects.21,22 Greater extensor endurance has been associated with better balance in older adults.23 Extensor endurance may be a means of documenting improvement in adults with CLBP over the course of an intervention.21 Unfortunately, test positions do not allow differentiation of back extensor endurance from hip extensor endurance.24 Thus, clinicians are left without a reliable and responsive clinical measure for direct assessment of the muscles of the posterior trunk.
Ultrasound imaging (USI), which uses reflected sound waves to create gray-scale images,25 is emerging as a safe and cost-effective clinical tool. USI offers practitioners the ability to perform not only direct assessments of posterior trunk muscle function but also assessments of muscle size in the outpatient setting. In younger individuals with and without back pain, USI has been shown to be reliable for assessing multifidus size, i.e. thickness and cross-sectional area and multifidus activity, i.e. change in thickness from a resting to a contracted state.26–32 Assessing the multifidus may be desirable due to the proposed role of the multifidus in spinal stabilization.11 To date, no studies have assessed the reliability of USI for multifidus thickness assessment in adults over the age of 60 years.
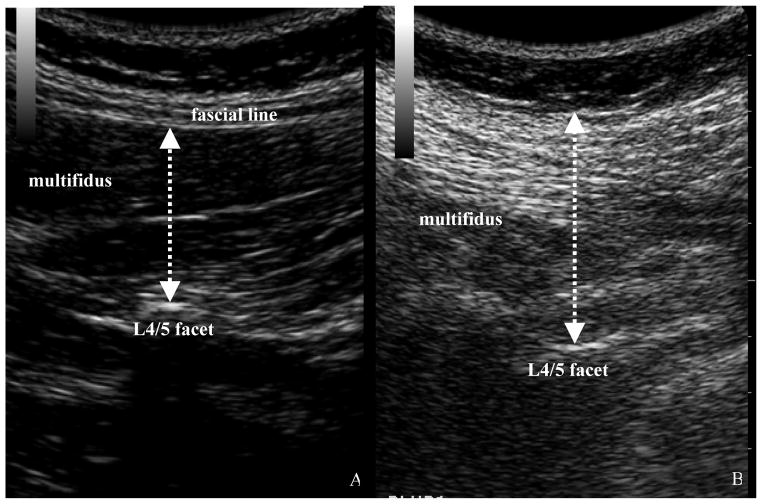
During an USI assessment of the multifidus, two techniques may be employed: parasagittal and/or transverse imaging.25,29,33 Parasagittal imaging is used to assess multifidus thickness and activity,27,29 while transverse imaging is used to assess multifidus cross-sectional area.26,32 USI measurement techniques rely on the ability to accurately identify multifidi fascial lines, which are hyperechoic (appear bright white) when compared to adjacent muscle tissue, which is more hypoechoic (appears darker). In the presence of increased intramuscular fat secondary to aging4,5 and low back pain,12,13 fascial line differentiation may be challenging (FIGURE 1). Therefore, the reliability of standard US measurement techniques should be evaluated in older adults with low back pain, prior to utilization of USI in clinical practice and skeletal muscle research in this population. Alternative measurement techniques that include the multifidus fascial line (FIGURE 1) may be more reliable in older individuals with CLBP who have increased intramuscular fat, eliminating the need to differentiate the multifidus from its fascia.
FIGURE 1. Parasagittal Ultrasound Imaging: Younger versus Older Adult.
Image of the L4/5 multifidus at rest in a younger adult (A) and an older adult with chronic low back pain (B). In the standard measurement technique (A), the measurement is taken from the L4/5 facet joint to the last dark pixel before the multifidus fascial line. In the alternative technique (B), the measurement is taken from the L4/5 facet joint up to and including the fascial layer given the difficulty of determining the fascial line.
Implementation of USI assessments for older adults with CLBP in the clinical setting may be dependent on two types of reliability: (1) procedural, which may be defined as the ability of examiners to perform the entire imaging process, i.e. location of the level of interest, image acquisition, and measurements of the images, in a consistent, repeatable fashion and (2) measurement reliability, which may be defined as the ability of examiners to perform measurements of muscle morphology from previously attained images in a consistent, repeatable fashion. While establishing between-days procedural reliability may allow for documentation of muscle changes across the course of treatment, establishing inter-examiner measurement reliability may allow for image processing to be delegated to trained support staff. Determination of minimal detectable change values (MDCs) for USI measurements in older adults with low back pain may allow researchers and clinicians to decide post-treatment when muscle changes surpass procedural and measurement error.34
The objectives of this measurement study were to (1) evaluate inter-examiner measurement reliability for assessments of multifidi resting and contracted thicknesses, (2) to evaluate intra-examiner and inter-examiner procedural reliability for USI assessments of multifidi resting and contracted thicknesses, and (3) to determine USI standard error of measurement values (SEMs) and MDCs for multifidi thicknesses in older adults with CLBP. We hypothesized that USI inter-examiner measurement reliability for USI would be excellent and that intra-examiner and inter-examiner procedural reliability would be excellent in older adults with CLBP. We hypothesized that an alternative thickness measurement technique that included the fascial line would have better reliability than the standard measurement technique in older adults with CLBP.
METHODS
Participants
Thirty-one cognitively intact, English-speaking and English-reading, community-dwelling older adults, aged 60 to 85 years with CLBP, defined as low back pain of at least 3 months duration, were recruited. Participants were excluded if they had (1) a history of low back surgery; (2) received treatment for low back pain within the past 6 months; (3) symptoms of non-mechanical low back pain, including unrelenting night pain, sensation changes in the groin region, or bowel and bladder disturbances; (4) a diagnosis of scoliosis; (5) experienced a recent traumatic event; (6) to use an assistive device greater than a cane for community-mobility; (7) a neurological disorder; (8) an acute or terminal illness; or (9) difficulty lying prone for USI imaging. Individuals who rated their current pain intensity as less than 3/10 on the Facial Pain Scale-Revised35 or scored less than 14% on the modified Oswestry Low Back Pain Questionnaire, an internationally-known measure of low back pain-related disability with established reliability and validity,36–38 were also excluded to increase the likelihood that participants would be representative of persons with significant CLBP-related disability who might seek outpatient services.
Data Collections
This study was approved by the Institutional Review Board for Human Subjects Research at the University of Delaware. Eligible participants, after completing the informed consent and a demographics questionnaire, underwent body anthropometric assessments, including height and weight.
USI Procedures
Participants were seen for 2 USI sessions scheduled 2 to 9 days apart. Two licensed physical therapists performed independent USI, with random determination of examiner and examination order. Both examiners received USI training through continuing education courses. Examiner 1 conducted about 75 posterior trunk muscle USI examinations in individuals ages 18 to 85 years prior to the start of the study, while examiner 2 conducted 10 USI sessions with examiner 1 and performed 10 USI sessions in older adults independently prior to the study (approximately 20 hours of hands-on training). Participants were requested to avoid trunk muscle exercises between sessions.
Images were obtained with a Mylab 25 portable ultrasonography unit (Biosound Esaote Inc., Indianapolis, IN) using brightness mode. Since trunk extension results in increased erector spinae thickness,39 participants were placed prone in 0–5 degrees of extension, as measured with an inclinometer placed at the L4/5 interspinous space.29 Three right and 3 left parasagittal images, using the split screen function to assess resting and contracted multifidus thickness side-by-side were obtained. A 3.5–7.0 MHz curvilinear transducer32 was used, with slight counter-pressure during active images to match muscle contraction pressure. Gain was adjusted for each image for optimal fascial line delineation and the transducer was removed from the skin between images.
During USI, the transducer was placed longitudinally and angled medially to capture the L4/5 facet joint (FIGURE 2A).33 Parasagittal images were taken at rest and during a contralateral, isometric straight leg raise26 of approximately 5 centimeters following 2 practice trials per limb (FIGURE 2B). Transducer locations were established using palpation, skin markings, and ultrasound verification using the sacrum as a reference point as described by Wallwork et al.29 Skin markings were removed between examiners to ensure that each examiner independently established transducer positions.29 Examiners were not able to observe one another during imaging; image acquisition took less than 15 minutes per examiner. Prior to USI during session 2, participants answered the question, “Since the last USI session, have you participated in exercises targeting your belly or back regions?” If the participant answered “yes” to this question, further participation was terminated.
FIGURE 2. Parasagittal Ultrasound Imaging Technique and Resultant Images.
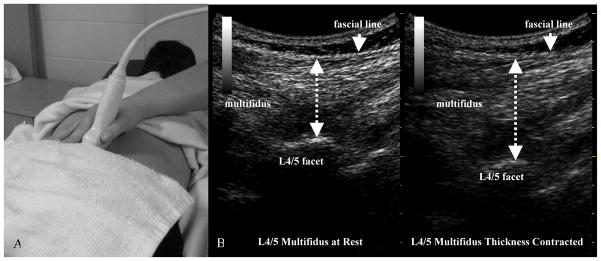
(A) Shown in the picture is the transducer placement for parasagittal imaging of L4/5 multifidus thickness. (B) Parasagittal images in an older adult for both the multifidus at rest and during a contralateral lower extremity lift are provided; standard measurements of multifidus thickness are shown for both images.
USI Data Analysis
All images were analyzed using MyLab software independently by each examiner (authors JMS and TOV); examiners were masked to measurement outputs. To allow determination of inter-examiner measurement reliability, examiner 2 took measurements of all images captured by examiner 1 from session 1. To allow determination of intra-examiner and inter-examiner, within-day and between-days USI procedural reliabilities, examiners 1 and 2 took measurements of their images obtained from both sessions 1 and 2. Measurements of multifidus thickness were taken using the standard technique, where a linear measurement is taken from the L4/5 facet joint to the last dark pixel before the multifidus fascial line27,29. Examiners also used the alternative measurement technique where a linear measurement was taken from the L4/5 facet joint up to and including the fascial layer. Each set of measurements took less than 10 minutes. Measurements were entered into a spreadsheet by a third member of the research team.
Statistical Analysis
PASW Statistics 18 (SPSS, Inc., Chicago, IL) was used to calculate ICCs with 95% CIs to estimate reliability. Between-days intra-examiner procedural reliability was determined using model (3,3). Within-day inter-examiner measurement, within-day inter-examiner procedural, and between-days inter-examiner procedural reliabilities were determined using model (2,3). Based on proposed ICC cut-offs by Fleiss, ICCs greater than 0.75 were considered excellent; 0.40 to 0.75 were considered fair-to-good.40 ICCs between standard and alternative ultrasound measurement techniques were compared to determine whether one technique was superior, i.e. more reliable, for assessing multifidus thickness. SEMs and MDCs were calculated.41,42
RESULTS
A total of 31 individuals met the inclusion and exclusion criteria and opted to participate in the study. Descriptive statistics are provided in Table 1. Only 1 participant did not return for session 2.
TABLE 1.
Demographics
| Variables | Older Adults with CLBP (n=31) |
|---|---|
| n (% of sample) | |
|
| |
| Female | 15 (48.4%) |
| Caucasian | 29 (93.5%) |
| Right Hand Dominance | 28 (90.3%) |
|
| |
| mean (SD) | |
|
| |
| Age (years) | 71.5 (6.4) |
| BMI (kg/m2) | 29.7 (5.0) |
| Pain Intensity (0–10)a | 3.3 (1.4) |
| Oswestry (%) | 29.3 (10.3) |
Abbreviations: CLBP, chronic low back pain; %, percentage; standard deviation, SD; BMI, body mass index; kg, kilograms.
Pain intensity is the composite of current, best, and worst pain in the past 24 hours.
Table 2 summarizes within day reliability. Regardless of the measurement technique used, ICCs indicated excellent inter-examiner measurement reliability (ICCs: 0.97–0.98). Both USI measurement techniques demonstrated excellent within-day, inter-examiner procedural reliability for both resting and contracted thicknesses (ICCs: 0.82–0.85). Within-day ICCs, SEMs, and MDCs did not indicate superiority of the alternative measurement technique when compared to the standard technique.
TABLE 2.
Inter-Examiner, Within-Days Reliability
| Older Adults with CLBP (n=31) | Measurement Reliability | Procedural Reliability | |||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | ICC (95% CI) | SEM | MDC | ICC (95% CI) | SEM | MDC | |
| LM thickness at rest (cm)a | 3.59 (0.95) | 0.98 (0.96, 0.99) | 0.13 | 0.35 | 0.84 (0.67, 0.92) | 0.38 | 1.06 |
| LM thickness contracted (cm)a | 4.04 (0.87) | 0.98 (0.96, 0.99) | 0.12 | 0.34 | 0.82 (0.63, 0.91) | 0.40 | 1.10 |
| LM thickness at rest ALT (cm)a | 3.98 (0.96) | 0.97 (0.94, 0.98) | 0.15 | 0.42 | 0.85 (0.70, 0.93) | 0.36 | 1.01 |
| LM thickness contracted ALT (cm)a | 4.48 (0.91) | 0.97 (0.95, 0.99) | 0.13 | 0.37 | 0.85 (0.69, 0.92) | 0.37 | 1.02 |
Abbreviations: CLBP, chronic low back pain; SD, standard deviation; ICC, intraclass correlation coefficient; CI, confidence interval; SEM, standard error of measurement; MDC, minimal detectable change; LM, lumbar multifidus; cm, centimeters; ALT, alternative.
Measurements are provided for the left L4/5 multifidi.
Table 3 summarizes between day reliability. Regardless of the measurement technique used to assess thickness, i.e. standard or alternative, both examiners demonstrated excellent intra-examiner, between-days, procedural reliability (ICCs: 0.90–0.93). The alternative measurement technique for multifidus thickness assessment had similar intra-examiner reliability when compared to the standard technique based on overlapping 95% confidence intervals. Examination of SEMs and MDCs indicates that examiner 1 consistently demonstrated lower SEMs and MDCs than examiner 2.
TABLE 3.
Between-Days Procedural Reliability
| Older Adults with CLBP (n=30) | Intra-Examiner
|
Inter-Examiner | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Examiner 1 | Examiner 2 | ||||||||
|
| |||||||||
| ICC (95% CI) | SEM | MDC | ICC (95% CI) | SEM | MDC | ICC (95% CI) | SEM | MDC | |
| LM thickness at rest (cm)a | 0.92 (0.84, 0.96) | 0.23 | 0.64 | 0.92 (0.83, 0.96) | 0.25 | 0.70 | 0.78 (0.55, 0.89) | 0.41 | 1.13 |
| LM thickness contracted (cm)a | 0.91 (0.82, 0.96) | 0.24 | 0.66 | 0.90 (0.78, 0.95) | 0.30 | 0.82 | 0.72 (0.43, 0.86) | 0.46 | 1.26 |
| LM thickness at rest ALT (cm)a | 0.93 (0.87, 0.97) | 0.21 | 0.60 | 0.93 (0.85, 0.96) | 0.24 | 0.67 | 0.79 (0.55, 0.90) | 0.41 | 1.13 |
| LM thickness contracted ALT (cm)a | 0.92 (0.84, 0.96) | 0.23 | 0.64 | 0.90 (0.80, 0.95) | 0.27 | 0.74 | 0.76 (0.51, 0.88) | 0.42 | 1.18 |
Abbreviations: CLBP, chronic low back pain; ICC, intraclass correlation coefficient; CI, confidence interval; SEM, standard error of measurement; MDC, minimal detectable change; LM, lumbar multifidus; cm, centimeters; ALT, alternative.
Measurements are provided for the left L4/5 multifidi.
Inter-examiner procedural reliability was acceptable for all measurements (ICCs: 0.72–0.79). There was not a clear advantage to the alternative measurement technique for assessing resting thickness over the standard measurement technique, although a lower SEM and a lower MDC were found for the alternative measurement for multifidus contracted thickness. Comparisons of within-day to between-days inter-examiner reliability indicated a decrease in reliability point estimates but overlapping confidence intervals (TABLES 2 and 3). SEMs and MDCs for all measurements were larger for between-days assessments, when compared to within-days (TABLES 2 and 3).
DISCUSSION
Results of this study indicate excellent measurement and procedural reliability, both within-day and between-days, is possible for assessments of multifidus thickness in older adults, aged 60 to 85 years, with CLBP. There is not a clear advantage to using the alternative measurement technique over the standard technique when assessing multifidi thickness in older adults with CLBP who may have increased intramuscular fat. However, the proposed alternative technique that includes the fascial line may be reliably used when the fascial line is indistinguishable from the multifidus muscle. Comparisons of intra- versus inter-examiner reliability indicate that re-evaluations should be conducted by the same examiner when possible, which may result in an improved ability to detect changes in muscle size and function.
Assessments of multifidus thickness at rest and during contralateral limb lift tasks are used to calculate thickness change (percent thickness change = [contracted thickness-resting thickness]/resting thickness*100), which has been correlated to electromyographic muscle activity for low level contractions.33 Calculations of multifidi thickness from ultrasound images may allow clinicians to directly evaluate and monitor multifidus function over the course of an intervention. Our between-days, procedural reliability results among older adults with CLBP, while lower than those previously published among younger adults with non-specific low back pain,27 suggest that USI may be reliable tool for assessment of multifidi function in older adults with back pain. For standard measurements, procedural reliability SEMs (0.23–0.46 cm) and MDCs (0.64–1.26 cm) were also larger than previously reported (0.02–0.21 cm and 0.07–0.58 cm respectively) among younger adults with and without low back pain.27,29–31 Lower reliability, greater SEMs, and greater MDCs may support the hypothesis that USI is more challenging among older adults with CLBP due to age- and CLBP-related muscle changes, although examiner training differences could also be responsible. Greater imaging challenges in older adults may be supported by the fact that examiner 2, the more novice examiner, received similar or greater hands-on training when compared to ‘novices’ in other studies.27,29–31 We acknowledge that our older adults with CLBP had greater body mass indices (BMIs) than participants in previously published USI reliability studies,27,29–31 but our sample was similar in BMI (29.7 kg/m2) to older individuals with CLBP (29.0 kg/m2) in a study by Rudy et al.43 Further, due to age-related changes there are inherent issues with using BMI to assess body fatness in older adults,44 and thus, it may not be appropriate to compare BMI between age groups. For measurement reliability, comparison of our parasagittal imaging results to those previously published among younger adults with and without low back pain,27,33 indicate that despite aging, CLBP, and participant anthropometrics, measurements of multifidi function may be delegated to trained staff.
Our SEMs provide information on measurement precision and are used to calculate MDCs.41,42 MDCs allow researchers and clinicians to determine when ‘true change’ has occurred pre-to-post treatment.34 Based on multifidus thickness MDCs obtained in this study, it may be easier to detect changes in multifidus thickness and function in an older adult with CLBP within a single-session rather than over time. Within-session assessment of multifidus thickness may be helpful to determine if a given treatment is effective at improving multifidus activity, (calculated from the resting and contracted thickness measurements), but further research is needed. Lower MDCs for examiner 1, who was more experienced in USI when compared to examiner 2, support previous ultrasound findings in younger adults of greater precision for experienced examiners.29
Our study has several limitations. While we believe that our sample is representative of older adults who might seek clinical services for their CLBP as they reported at least minimal disability per the modified Oswestry Low Back Pain Questionnaire, we are unable to say with certainty. We acknowledge that providing USI reliability data from a group of older adults without CLBP for comparison would have expanded the breadth of this study. As USI procedural reliability for multifidi thickness assessment takes into account the ability to determine the target level, capture optimal images at rest and during a contraction, and perform accurate measurements, examiner training is critical. Examiner 1 and 2 not only attended continuing education courses in USI, specific to the posterior trunk that focused on capturing optimal images and taking measurements but also participated in ‘in-depth’ anatomy education, including cadaveric dissection that focused on spinal level identification. Examiners with differing educational backgrounds may or may not be able to attain similar reliability. USI assessments were conducted by examiners whose USI training included older adults; training specificity cannot be discounted. Increased imaging experience may enable detection of smaller pre-to-post treatment multifidus changes; therefore, it is possible that years-of-experience may enhance reliability. Further, while examiners were reliable at level L4/5, we acknowledge that these results may not translate to adjacent levels, i.e. L3/4 or L5/S1.
When the fascial line is indistinguishable from the multifidus muscle and the examiner opts to use the alternative measurement technique, the examiner should be cognizant that the fascial layer can be thickened and disorganized in those with CLBP.45 Further, fascia may respond to exercises prescribed for CLBP.46 Therefore, changes in fascia pre-to-post treatment are possible. While these factors may not affect within-day reliability of the measurement, between-days reliability may be affected.
CONCLUSIONS
In conclusion, findings of excellent intra- and inter-examiner USI procedural reliability among older adults with CLBP may provide clinicians a direct assessment technique for clinical evaluation of lumbar multifidus. Use of the standard USI measurement technique for multifidus thickness assessment is recommended. Provided SEMs and MDCs may allow for interpretation of USI assessments in this patient population. Among older adults with CLBP, the use of USI as an adjunct to standard clinical measures may allow detection of small muscular changes resulting in large functional improvements. Future research exploring relationships between USI findings and clinical measures, including those assessing the psychosocial domain, may help clinicians to better understand the etiology of CLBP and develop more effective interventions.
Acknowledgments
The work of Dr. Sions is supported in part by the Foundation for Physical Therapy PODS I/II, the University of Delaware’s Office of Graduate Studies, R21 HD057274 (NICHD), and 1R01AG041202-01(NIA). The work of Teonette Velasco and Dr. Hicks is supported in part by R21 HD057274 (NICHD) and R01AG041202-01(NIA).
Footnotes
Conflicts of Interest: None
Disclaimer: The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of the U.S. Army Medical Research and Materiel Command, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense, or the U.S. Government.
A portion of this manuscript was presented in poster format at the 2011 Orthopedic Research Society meeting in Long Beach, California.
Contributor Information
J. Megan Sions, Email: megsions@udel.edu.
Teonette O. Velasco, Email: teonette@udel.edu.
Deydre S. Teyhen, Email: dteyhen@gmail.com.
Gregory E. Hicks, Email: ghicks@udel.edu.
References
- 1.Hicks GE, Gaines JM, Shardell M, Simonsick EM. Associations of back and leg pain with health status and functional capacity of older adults: findings from the retirement community back pain study. Arthritis Rheum. 2008;59(9):1306–1313. doi: 10.1002/art.24006. [DOI] [PubMed] [Google Scholar]
- 2.American Geriatrics Society releases persistent pain management guideline. J Pain Palliat Care Pharmacother. 2002;16(4):127–129. [PubMed] [Google Scholar]
- 3.Savigny P, Watson P, Underwood M. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ. 2009;338:b1805. doi: 10.1136/bmj.b1805. [DOI] [PubMed] [Google Scholar]
- 4.Taaffe DR, Henwood TR, Nalls MA, Walker DG, Lang TF, Harris TB. Alterations in muscle attenuation following detraining and retraining in resistance-trained older adults. Gerontology. 2009;55(2):217–223. doi: 10.1159/000182084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadar H, Gadoth N, Heifetz M. Fatty replacement of lower paraspinal muscles: normal and neuromuscular disorders. AJR Am J Roentgenol. 1983;141(5):895–898. doi: 10.2214/ajr.141.5.895. [DOI] [PubMed] [Google Scholar]
- 6.Burton LA, Sumukadas D. Optimal management of sarcopenia. Clin Interv Aging. 2010;5:217–228. doi: 10.2147/cia.s11473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamaz M, Kiresi D, Oguz H, Emlik D, Levendoglu F. CT measurement of trunk muscle areas in patients with chronic low back pain. Diagn Interv Radiol. 2007;13(3):144–148. [PubMed] [Google Scholar]
- 8.Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol. 2000;55(2):145–149. doi: 10.1053/crad.1999.0340. [DOI] [PubMed] [Google Scholar]
- 9.Hicks GE, Morone N, Weiner DK. Degenerative lumbar disc and facet disease in older adults: prevalence and clinical correlates. Spine (Phila Pa 1976) 2009;34(12):1301–1306. doi: 10.1097/BRS.0b013e3181a18263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Briggs AM, Greig AM, Wark JD, Fazzalari NL, Bennell KL. A review of anatomical and mechanical factors affecting vertebral body integrity. Int J Med Sci. 2004;1(3):170–180. doi: 10.7150/ijms.1.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moseley GL, Hodges PW, Gandevia SC. Deep and superficial fibers of the lumbar multifidus muscle are differentially active during voluntary arm movements. Spine (Phila Pa 1976) 2002;27(2):E29–36. doi: 10.1097/00007632-200201150-00013. [DOI] [PubMed] [Google Scholar]
- 12.Kjaer P, Bendix T, Sorensen JS, Korsholm L, Leboeuf-Yde C. Are MRI-defined fat infiltrations in the multifidus muscles associated with low back pain? BMC Med. 2007;5:2. doi: 10.1186/1741-7015-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hultman G, Nordin M, Saraste H, Ohlsen H. Body composition, endurance, strength, cross-sectional area, and density of MM erector spinae in men with and without low back pain. J Spinal Disord. 1993;6(2):114–123. [PubMed] [Google Scholar]
- 14.Hicks GE, Simonsick EM, Harris TB, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2005;60(7):882–887. doi: 10.1093/gerona/60.7.882. [DOI] [PubMed] [Google Scholar]
- 15.Demoulin C, Crielaard JM, Vanderthommen M. Spinal muscle evaluation in healthy individuals and low-back-pain patients: a literature review. Joint Bone Spine. 2007;74(1):9–13. doi: 10.1016/j.jbspin.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976) 1994;19(2):165–172. doi: 10.1097/00007632-199401001-00009. [DOI] [PubMed] [Google Scholar]
- 17.Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146(2):116–127. doi: 10.7326/0003-4819-146-2-200701160-00006. [DOI] [PubMed] [Google Scholar]
- 18.Hicks GE, Simonsick EM, Harris TB, et al. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol A Biol Sci Med Sci. 2005;60(11):1420–1424. doi: 10.1093/gerona/60.11.1420. [DOI] [PubMed] [Google Scholar]
- 19.Kasukawa Y, Miyakoshi N, Hongo M, et al. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J Bone Miner Metab. 2010;28(1):82–87. doi: 10.1007/s00774-009-0107-1. [DOI] [PubMed] [Google Scholar]
- 20.Miyakoshi N, Hongo M, Maekawa S, Ishikawa Y, Shimada Y, Itoi E. Back extensor strength and lumbar spinal mobility are predictors of quality of life in patients with postmenopausal osteoporosis. Osteoporos Int. 2007;18(10):1397–1403. doi: 10.1007/s00198-007-0383-3. [DOI] [PubMed] [Google Scholar]
- 21.Gruther W, Wick F, Paul B, et al. Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J Rehabil Med. 2009;41(8):613–619. doi: 10.2340/16501977-0391. [DOI] [PubMed] [Google Scholar]
- 22.Keller A, Hellesnes J, Brox JI. Reliability of the isokinetic trunk extensor test, Biering-Sorensen test, and Astrand bicycle test: assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine (Phila Pa 1976) 2001;26(7):771–777. doi: 10.1097/00007632-200104010-00017. [DOI] [PubMed] [Google Scholar]
- 23.Suri P, Kiely DK, Leveille SG, Frontera WR, Bean JF. Increased trunk extension endurance is associated with meaningful improvement in balance among older adults with mobility problems. Arch Phys Med Rehabil. 2011;92(7):1038–1043. doi: 10.1016/j.apmr.2010.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moreau CE, Green BN, Johnson CD, Moreau SR. Isometric back extension endurance tests: a review of the literature. J Manipulative Physiol Ther. 2001;24(2):110–122. doi: 10.1067/mmt.2001.112563. [DOI] [PubMed] [Google Scholar]
- 25.Whittaker JL, Teyhen DS, Elliott JM, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007;37(8):434–449. doi: 10.2519/jospt.2007.2350. [DOI] [PubMed] [Google Scholar]
- 26.Pressler JF, Heiss DG, Buford JA, Chidley JV. Between-day repeatability and symmetry of multifidus cross-sectional area measured using ultrasound imaging. J Orthop Sports Phys Ther. 2006;36(1):10–18. doi: 10.2519/jospt.2006.36.1.10. [DOI] [PubMed] [Google Scholar]
- 27.Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, Magel JS. Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil. 2009;90(1):87–94. doi: 10.1016/j.apmr.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 28.Van K, Hides JA, Richardson CA. The use of real-time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther. 2006;36(12):920–925. doi: 10.2519/jospt.2006.2304. [DOI] [PubMed] [Google Scholar]
- 29.Wallwork TL, Hides JA, Stanton WR. Intrarater and interrater reliability of assessment of lumbar multifidus muscle thickness using rehabilitative ultrasound imaging. J Orthop Sports Phys Ther. 2007;37(10):608–612. doi: 10.2519/jospt.2007.2418. [DOI] [PubMed] [Google Scholar]
- 30.Wong AY, Parent EC, Kawchuk GN. Reliability of Two Ultrasonic Imaging Analysis Methods in Quantifying Lumbar Multifidus Thickness. J Orthop Sports Phys Ther. 2013;43(4):251–262. doi: 10.2519/jospt.2013.4478. [DOI] [PubMed] [Google Scholar]
- 31.Teyhen DS, George SZ, Dugan JL, Williamson J, Neilson BD, Childs JD. Inter-rater reliability of ultrasound imaging of the trunk musculature among novice raters. J Ultrasound Med. 2011;30(3):347–356. doi: 10.7863/jum.2011.30.3.347. [DOI] [PubMed] [Google Scholar]
- 32.Stokes M, Rankin G, Newham DJ. Ultrasound imaging of lumbar multifidus muscle: normal reference ranges for measurements and practical guidance on the technique. Man Ther. 2005;10(2):116–126. doi: 10.1016/j.math.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 33.Kiesel KB, Uhl TL, Underwood FB, Rodd DW, Nitz AJ. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther. 2007;12(2):161–166. doi: 10.1016/j.math.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 34.de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes. 2006;4:54. doi: 10.1186/1477-7525-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hadjistavropoulos T, Martin RR, Sharpe D, Lints AC, McCreary DR, Asmundson GJ. A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community-dwelling older adults. J Aging Health. 2007;19(6):965–984. doi: 10.1177/0898264307308611. [DOI] [PubMed] [Google Scholar]
- 36.Hicks GE, Manal TJ. Psychometric properties of commonly used low back disability questionnaires: are they useful for older adults with low back pain? Pain Med. 2009;10(1):85–94. doi: 10.1111/j.1526-4637.2008.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calmels P, Bethoux F, Condemine A, Fayolle-Minon I. Low back pain disability assessment tools. Ann Readapt Med Phys. 2005;48(6):288–297. doi: 10.1016/j.annrmp.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 38.Vianin M. Psychometric properties and clinical usefulness of the Oswestry Disability Index. J Chiropr Med. 2008;7(4):161–163. doi: 10.1016/j.jcm.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watanabe K, Miyamoto K, Masuda T, Shimizu K. Use of ultrasonography to evaluate thickness of the erector spinae muscle in maximum flexion and extension of the lumbar spine. Spine (Phila Pa 1976) 2004;29(13):1472–1477. doi: 10.1097/01.brs.0000128755.84693.10. [DOI] [PubMed] [Google Scholar]
- 40.Fleiss JL. The Design and Analysis of Clinical Experiments. New York: Wiley; 1999. [Google Scholar]
- 41.Eliasziw M, Young SL, Woodbury MG, Fryday-Field K. Statistical methodology for the concurrent assessment of interrater and intrarater reliability: using goniometric measurements as an example. Phys Ther. 1994;74(8):777–788. doi: 10.1093/ptj/74.8.777. [DOI] [PubMed] [Google Scholar]
- 42.Roebroeck ME, Harlaar J, Lankhorst GJ. The application of generalizability theory to reliability assessment: an illustration using isometric force measurements. Phys Ther. 1993;73(6):386–395. doi: 10.1093/ptj/73.6.386. discussion 396–401. [DOI] [PubMed] [Google Scholar]
- 43.Rudy TE, Weiner DK, Lieber SJ, Slaboda J, Boston JR. The impact of chronic low back pain on older adults: a comparative study of patients and controls. Pain. 2007;131(3):293–301. doi: 10.1016/j.pain.2007.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Villareal DT, Apovian CM, Kushner RF, Klein S. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Obes Res. 2005;13(11):1849–1863. doi: 10.1038/oby.2005.228. [DOI] [PubMed] [Google Scholar]
- 45.Langevin HM, Stevens-Tuttle D, Fox JR, et al. Ultrasound evidence of altered lumbar connective tissue structure in human subjects with chronic low back pain. BMC Musculoskelet Disord. 2009;10:151. doi: 10.1186/1471-2474-10-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schleip R, Muller DG. Training principles for fascial connective tissues: scientific foundation and suggested practical applications. J Bodyw Mov Ther. 2013;17(1):103–115. doi: 10.1016/j.jbmt.2012.06.007. [DOI] [PubMed] [Google Scholar]