Abstract
Idiopathic hypertrophic spinal pachymeningitis (IHSP) is a chronic, progressive, inflammatory disorder characterized by marked fibrosis of the spinal dura mater with unknown etiology. According to the location of the lesion, it might induce neurologic deficits by compression of spinal cord and nerve root. A 58-year old female with a 3-year history of progressive weakness in both lower extremities was referred to our institute. Spinal computed tomography (CT) scan showed an osteolytic lesion involving base of the C6 spinous process with adjacent epidural mass. Magnetic resonance imaging (MRI) revealed an epidural mass involving dorsal aspect of cervical spinal canal from C5 to C7 level, with low signal intensity on T1 and T2 weighted images and non-enhancement on T1 weighted-enhanced images. We decided to undertake surgical exploration. At the operation field, there was yellow colored, thickened fibrous tissue over the dura mater. The lesion was removed totally, and decompression of spinal cord was achieved. Symptoms improved partially after the operation. Histopathologically, fibrotic pachymeninges with scanty inflammatory cells was revealed, which was compatible with diagnosis of idiopathic hypertrophic pachymeningitis. Six months after operation, motor power grade of both lower extremities was normal on physical examination. However, the patient still complained of mild weakness in the right lower extremity. Although the nature of IHSP is generally indolent, decompressive surgery should be considered for the patient with definite or progressive neurologic symptoms in order to prevent further deterioration. In addition, IHSP can present as an osteolytic lesion. Differential diagnosis with neoplastic disease, including giant cell tumor, is important.
Keywords: Idiopathic hypertrophic spinal pachymeningitis, Osteolytic lesion, Mimicking giant cell tumor, Decompressive surgery, Differential diagnosis
INTRODUCTION
Idiopathic hypertrophic spinal pachymeningitis (IHSP) is a rare clinical disorder characterized by diffuse or localized fibrous thickening of the spinal dura matter with chronic and progressive process13,14,16,25). Several etiologies are related with hypertrophic spinal pachymeningitis, including infection, autoimmune reaction, sarcoidosis and neoplastic process. IHSP is a diagnosis of exclusion after careful exploration for possible etiologies.
Clinical manifestation of IHSP is usually related with compression of the nervous system or vascular structure caused by thickened dura mater. As a result, IHSP might induce various neurologic symptoms depending on the location of the lesion. Cervical and thoracic levels of spine are the most frequently involved among levels17,24).
Typical magnetic resonance imaging (MRI) finding of the IHSP is linear T2 low signal mass involving dura extending over multiple levels with peripheral or nodular enhancement. However, associated osteolytic lesion adjacent to IHSP has barely been described previously.
We report a case of IHSP involving cervical spine with an osteolytic lesion.
CASE REPORT
A 58-year-old female visited our institution with progressive weakness of both lower extremities and clumsiness of both hands. These symptoms had been developed 3 years ago and worsened gradually. The patient received a hysterectomy 10 years ago because of benign myoma and total thyroidectomy 2 years ago because of follicular thyroid carcinoma. There was neither noticeable history of trauma nor contributable family medical history. On physical examination, there was slight motor power weakness (grade 4+/5) in both lower extremities. The deep tendon reflexes were normal and the ankle clonus was absent. There was no fever or leukocytosis. However, the erythrocyte sedimentation rate (ESR) was slightly elevated to 38 mm/hr (reference range : 0-27 mm/hr). Initial computed tomography (CT) scan showed an osteolytic mass-like lesion involving base of the C6 spinous process, which caused spinal canal stenosis. Radiologic report suggested neoplastic disease such as giant cell tumor, which has the characteristics of an osteolytic neoplasm (Fig. 1). MRI was carried out after CT scan and revealed an epidural mass involving the dorsal aspect of cervical spinal canal from C5 to C7 level, with low signal intensity on T1 and T2 weighted images and non-enhancement on T1 weighted-enhanced images. There was abnormally high signal intensity of the spinal cord on T2 weighted image at C6 level, suggesting myelopathy (Fig. 2). The patient underwent surgical exploration, with a complete hemilamiectomy of C5, C6, and C7 with left side approach. There was yellow-colored, thickened fibrous tissue over the dura mater. The mass was grossly totally removed, and decompression of spinal cord was achieved. Dexamethasone was prescribed temporarily to reduce inflammatory reactions. Five days after surgery, patient discharged without complications related with surgery and the symptoms were improved but not completely recovered. Pathologic examination revealed fibrotic pachymeninges with no significant inflammation, and these findings were compatible with diagnosis of IHSP (Fig. 3). Six months after operation, the patients visited an out-patient clinic, and the symptoms were stationary compared with at discharge. A follow-up MRI was conducted and revealed no recurrence of dura mater thickening.
Fig. 1.
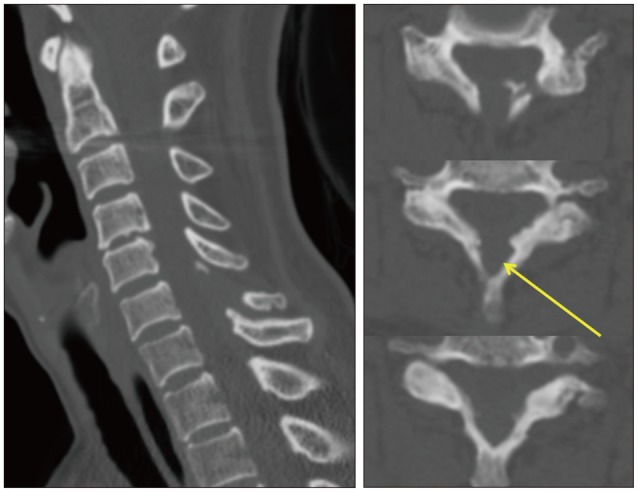
Computed tomography scan revealed an osteolytic lesion involving base of the C6 spinous process.
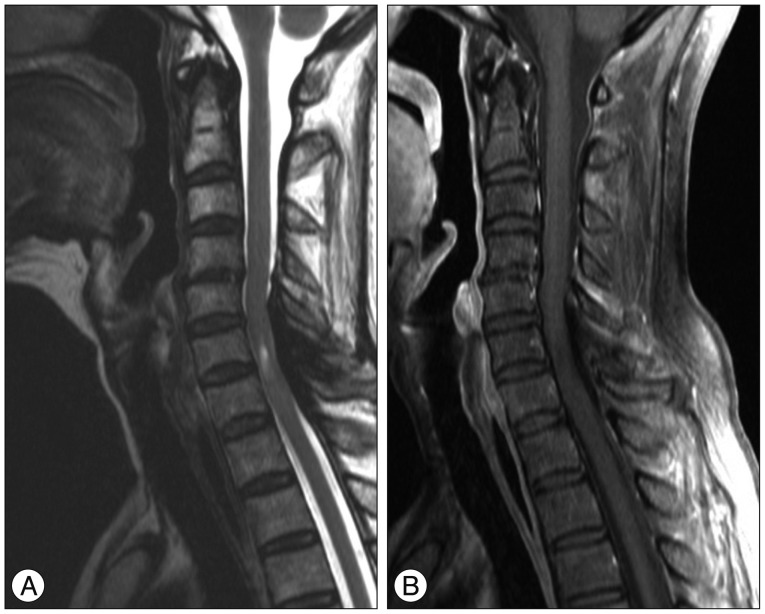
Fig. 2.
Magnetic resonance imaging revealed an epidural mass involving the dorsal aspect of cervical spinal canal from C5 to C7 level, with low signal intensity on T2 weighted image (A) and non-enhancement on T1 weighted-enhanced image (B).
Fig. 3.
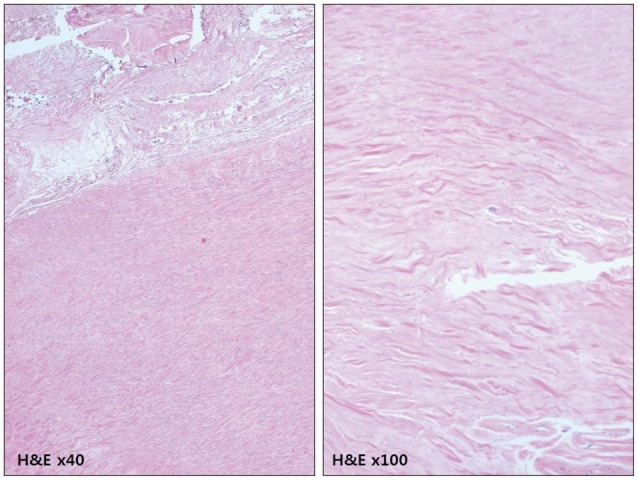
Photomicrograph of a section of the excised dura mater showed fibrotic pachymeninges with no significant inflammation, which was more apparent at the higher magnification view (Hematoxylin and eosin staining).
DISCUSSION
IHSP is a rare condition, but possibly under-recognized because of its indolent nature and non-specific symptoms. Since accessibility of the diagnostic imaging technique including spinal MRI has improved recently, IHSP has been diagnosed and reported more frequently.
According to etiology of the disease, hypertrophic pachymeningitis is classified as idiopathic and secondary. Some infectious diseases including syphilis, and diseases caused by HTLV-1, mycobacterium, and fungi are reportedly associated with hypertrophic pachymeningitis2,10,18,27,29). Various autoimmune disorders, such as rheumatoid arthritis, Wegener's granulomatosis, multifocal fibrosclerosis, sclerosing cholangitis, and sarcoidosis are also regarded as etiologic factors in particular cases3,4,5,7,15,17,19,22,24,26). The diagnosis of IHSP depends on exclusion of these possible causative factors. In this case, we tried to reveal possible causative factors but failed. Although ESR was slightly increased, it was normalized 2 months after the operation and seemed to be a non-specific finding rather than sign of hidden inflammatory disease.
Clinical manifestations of IHSP vary according to location and size. In the early stage of the disease, the patient may experience only localized pain, However, as the lesion grows, it may lead to radiculopathy or compressive myelopathy.8) Typically, the symptoms caused by IHSP have an indolent nature with a chronic course5,9).
Histopathologically, IHSP is characterized by fibrosis and infiltration of inflammatory cells, such as lymphocytes, plasma cells, polymorphonuclear cells, eosinophils and macrophages, without necrotic change. However, in cases of secondary hypertrophic pachymeningitis, specific histopathologic findings might be different according to the nature of the underlying causative disease. In the present case, there were only scanty inflammatory cells and no evidence of active inflammation. These pathologic findings correspond to MRI findings. Typically, IHSP showed peripheral or nodular enhancement pattern and it represent to zone of inflammation.6) Nevertheless, in this case, MRI showed no enhanced portion. Less inflammatory reaction, more fibrosis, and no enhanced portion are related to worse response to steroid therapy23).
Because of the lack of long-term follow-up studies, there is insufficient clinical information on the natural history and clinical course of the disease to establish an optimal management plan for patients with IHSP. However, it seems to progress without treatment. Decompressive surgery for the patient with definite or progressive neurologic symptoms should be considered for preventing further deterioration. Surgical management is the only treatment option that offers the prospect of cure. In addition, some authors suggest subsequent steroid therapy after surgery to reduce inflammatory reactions12), though the efficacy of this remains debatable. Alternative clinical trial including chemotherapy with azathioprine, cyclophosphamide and methotrexate, or radiation therapy in selected patients has been reported, but these treatments showed limited efficacy1,5,11,16,20,21).
There has been no previous report describing a case of IHSP with osteolytic lesion to our knowledge. In the present case, pre-operative CT showed definite osteolytic lesion on the adjacent spinous process. The reason of osteolysis is not clear, but it might be a vestige of inflammatory reaction. Although there was no evidence of active inflammatory reaction according to histopathologic findings, it is hard to exclude the possibility of a change in activity of inflammation with time course. The clinical importance of IHSP with osteolytic lesion is that it must be distinguished from osteolytic neoplasm including giant cell tumor.
Most reports of IHSP have been limited to short-term follow-up after the initial treatment. According to previous reports, with long term follow-up exceeding 5 years, recurrence was noted in three of five cases28). In this regard, repeated follow ups are desirable in patient with IHSP even after successful treatment.
CONCLUSION
IHSP is a rare condition, but possibly under-recognized because of its indolent nature and non-specific symptoms. Decompressive surgery should be considered for the patient with definite or progressive neurologic symptoms in order to prevent further deterioration. After the surgical treatment, scheduled follow up is mandatory because IHSP can be recurrent. In addition, IHSP can present as an osteolytic lesion. Differential diagnosis with neoplastic disease, including giant cell tumor, is important.
References
- 1.Adler JR, Sheridan W, Kosek J, Linder S. Pachymeningitis associated with a pulmonary nodule. Neurosurgery. 1991;29:283–287. doi: 10.1097/00006123-199108000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Agdal N, Hagdrup HK, Wantzin GL. Pachymeningitis cervicalis hypertrophica syphilitica. Acta Derm Venereol. 1980;60:184–186. [PubMed] [Google Scholar]
- 3.Astrom KE, Lidholm SO. Extensive intracranial lesions in a case of orbital non-specific granuloma combined with polyarteritis nodosa. J Clin Pathol. 1963;16:137–143. doi: 10.1136/jcp.16.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bucy PC, Freeman LW. Hypertrophic spinal pachymeningitis with special reference to appropriate surgical treatment. J Neurosurg. 1952;9:564–578. doi: 10.3171/jns.1952.9.6.0564. [DOI] [PubMed] [Google Scholar]
- 5.Dumont AS, Clark AW, Sevick RJ, Myles ST. Idiopathic hypertrophic pachymeningitis : a report of two patients and review of the literature. Can J Neurol Sci. 2000;27:333–340. doi: 10.1017/s0317167100001116. [DOI] [PubMed] [Google Scholar]
- 6.Friedman D, Flanders A, Tartaglino L. Contrast-enhanced MR imaging of idiopathic hypertrophic craniospinal pachymeningitis. AJR Am J Roentgenol. 1993;160:900–901. doi: 10.2214/ajr.160.4.8456697. [DOI] [PubMed] [Google Scholar]
- 7.Guidetti B, La Torre E. Hypertrophic spinal pachymeningitis. J Neurosurg. 1967;26:496–503. doi: 10.3171/jns.1967.26.5.0496. [DOI] [PubMed] [Google Scholar]
- 8.Ito Z, Osawa Y, Matsuyama Y, Aoki T, Harada A, Ishiguro N. Recurrence of hypertrophic spinal pachymeningitis. Report of two cases and review of the literature. J Neurosurg Spine. 2006;4:509–513. doi: 10.3171/spi.2006.4.6.509. [DOI] [PubMed] [Google Scholar]
- 9.Kao KP, Huang CI, Shan DE, Ho JT, Chang T, Chu FL. Non-obstructive idiopathic pachymeningitis cervicalis hypertrophica. J Neurol Neurosurg Psychiatry. 1986;49:1441–1444. doi: 10.1136/jnnp.49.12.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawano Y, Kira J. Chronic hypertrophic cranial pachymeningitis associated with HTLV-I infection. J Neurol Neurosurg Psychiatry. 1995;59:435–437. doi: 10.1136/jnnp.59.4.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khadilkar SV, Menezes K, Parekh HN, Ursekar M, Bhagwati SN. Idiopathic hypertrophic cervical pachymeningitis : a case report with 5 year follow up. J Assoc Physicians India. 2003;51:391–393. [PubMed] [Google Scholar]
- 12.Kim JH, Chin DK. Idiopathic hypertrophic spinal pachymeningitis : report of two cases and review of the literature. J Korean Neurosurg Soc. 2011;50:392–395. doi: 10.3340/jkns.2011.50.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kupersmith MJ, Martin V, Heller G, Shah A, Mitnick HJ. Idiopathic hypertrophic pachymeningitis. Neurology. 2004;62:686–694. doi: 10.1212/01.wnl.0000113748.53023.b7. [DOI] [PubMed] [Google Scholar]
- 14.Lee YC, Chueng YC, Hsu SW, Lui CC. Idiopathic hypertrophic cranial pachymeningitis : case report with 7 years of imaging follow-up. AJNR Am J Neuroradiol. 2003;24:119–123. [PMC free article] [PubMed] [Google Scholar]
- 15.Levine MR, Kaye L, Mair S, Bates J. Multifocal fibrosclerosis. Report of a case of bilateral idiopathic sclerosing pseudotumor and retroperitoneal fibrosis. Arch Ophthalmol. 1993;111:841–843. doi: 10.1001/archopht.1993.01090060129037. [DOI] [PubMed] [Google Scholar]
- 16.Martin N, Masson C, Henin D, Mompoint D, Marsault C, Nahum H. Hypertrophic cranial pachymeningitis : assessment with CT and MR imaging. AJNR Am J Neuroradiol. 1989;10:477–484. [PMC free article] [PubMed] [Google Scholar]
- 17.Mikawa Y, Watanabe R, Hino Y, Hirano K. Hypertrophic spinal pachymeningitis. Spine (Phila Pa 1976) 1994;19:620–625. doi: 10.1097/00007632-199403000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Moore AP, Rolfe EB, Jones EL. Pachymeningitis cranialis hypertrophica. J Neurol Neurosurg Psychiatry. 1985;48:942–944. doi: 10.1136/jnnp.48.9.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naffziger HC, Stern WE. Chronic pachymeningitis; report of a case and review of the literature. Arch Neurol Psychiatry. 1949;62:383–411. [PubMed] [Google Scholar]
- 20.Nishino H, Rubino FA, Parisi JE. The spectrum of neurologic involvement in Wegener's granulomatosis. Neurology. 1993;43:1334–1337. doi: 10.1212/wnl.43.7.1334. [DOI] [PubMed] [Google Scholar]
- 21.Nishizaki T, Iwamoto F, Uesugi S, Akimura T, Yamashita K, Ito H. Idiopathic cranial pachymeningoencephalitis focally affecting the parietal dura mater and adjacent brain parenchyma : case report. Neurosurgery. 1997;40:840–843. doi: 10.1097/00006123-199704000-00037. discussion 843. [DOI] [PubMed] [Google Scholar]
- 22.Noble SC, Chandler WF, Lloyd RV. Intracranial extension of orbital pseudotumor : a case report. Neurosurgery. 1986;18:798–801. doi: 10.1227/00006123-198606000-00023. [DOI] [PubMed] [Google Scholar]
- 23.Pai S, Welsh CT, Patel S, Rumboldt Z. Idiopathic hypertrophic spinal pachymeningitis : report of two cases with typical MR imaging findings. AJNR Am J Neuroradiol. 2007;28:590–592. [PMC free article] [PubMed] [Google Scholar]
- 24.Park SH, Whang CJ, Sohn M, Oh YC, Lee CH, Whang YJ. Idiopathic hypertrophic spinal pachymeningitis : a case report. J Korean Med Sci. 2001;16:683–688. doi: 10.3346/jkms.2001.16.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Riku S, Kato S. Idiopathic hypertrophic pachymeningitis. Neuropathology. 2003;23:335–344. doi: 10.1046/j.1440-1789.2003.00520.x. [DOI] [PubMed] [Google Scholar]
- 26.Rosenfeld JV, Kaye AH, Davis S, Gonzales M. Pachymeningitis cervicalis hypertrophica. Case report. J Neurosurg. 1987;66:137–139. doi: 10.3171/jns.1987.66.1.0137. [DOI] [PubMed] [Google Scholar]
- 27.Schiess RJ, Coscia MF, McClellan GA. Petriellidium boydii pachymeningitis treated with miconazole and ketoconazole. Neurosurgery. 1984;14:220–224. doi: 10.1227/00006123-198402000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Tsutsui M, Yasuda T, Kanamori M, Hori T, Kimura T. Long-term outcome of idiopathic hypertrophic thoracic pachymeningitis. Eur Spine J. 2012;21(Suppl 4):S404–S407. doi: 10.1007/s00586-011-1848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamashita K, Suzuki Y, Yoshizumi H, Takahashi JB, Nogawa T. Tuberculous hypertrophic pachymeningitis involving the posterior fossa and high cervical region--case report. Neurol Med Chir (Tokyo) 1994;34:100–103. doi: 10.2176/nmc.34.100. [DOI] [PubMed] [Google Scholar]