Abstract
Background
In Germany, it is recommended that the surgical treatment of an undescended testis should be carried out between the ages of 6 months and 1 year to lower the risks of subfertility and testicular carcinoma. Although this recommendation has appeared in the German guidelines from 2007 onward, orchidopexy is still frequently performed at later ages.
Method
We retrospectively analyzed data from seven pediatric surgical services in the German state of Baden-Württemberg on all boys who underwent orchidopexy from 2009 to 2012. We classified the timing of surgery as Age Group I (before the first birthday), Age Group II (between the first and second birthdays), and Age Group III (after the second birthday). We determined whether preoperative hormonal treatment was given and distinguished primary from secondary undescended testis.
Results
Among 2213 boys who underwent orchidopexy, 1850 had primary and 363 had secondary undescended testis. Of those with primary undescended testis, the percentages of boys who underwent surgery in Age Groups I, II, and III were (respectively, with 95% confidence intervals): 18.7% (17–20.6%), 24.4% (22.5–26.5%), and 57% (54.6–59.2%). A small percentage of boys in each group also received preoperative hormonal treatment. From 2009 to 2012, there was a secular trend favoring earlier orchidopexy. In 2012, 28 boys (14.2% [9.7–20.0%]) had orchidopexy in outpatient pediatric surgery practices before their first birthday, while 68 did on hospital inpatient services (40.7% [33.2–48.6%]).
Conclusion
Most of the patients studied had surgery at a later age than recommended. Adherence to the guidelines in this respect is nonetheless relatively good in Germany compared to other countries, as studies from abroad have yielded findings that are just as bad or worse.
At birth, 1.8% to 8.4% of boys have a primary undescended testis (1, e1– e9); among premature neonates, the figure is as high as 30% (2, e10). This rate drops to 0.8–1.3% by the third month of life (e11), after which spontaneous descent of the testis is unlikely (e10, e12). An increased incidence of the condition since the 1950s has been described by some, but this observation is disputed (1, e3, e5).
In secondary undescended testis, unlike primary undescended testis, the testicle(s) are initially in the correct, intrascrotal anatomical position and then travel upward because of inadequate longitudinal growth or restraining fibrous portions or the spermatic cord, or other factors (e13).
A much-discussed late sequela of primary undescended testis is the potential impairment of fertility in adulthood. The normal scrotal temperature of around 33°C promotes hormonal changes through which gonocytes mature into adult spermatogonia (Ad spermatogonia); these, in turn, constitute the pool from which spermatocytes later develop (3, e14, e15). If the testis is malpositioned, gonocytes may persist and spermatogonia fail to mature (4). Similar, qualitatively less marked histological changes have also been found in the contralateral, orthotopic testis (e16). In many studies, various findings reflecting this morphological developmental disturbance have been identified as potential markers of impaired fertility:
In a meta-analysis, there was a consistent finding across studies to the effect that early surgery positively affects features that are taken to be markers of fertility (6). It must be pointed out, however, that a Cochrane analysis revealed a markedly lower probability of fathering a child (i.e., direct evidence of fertility) in comparison to the normal population only in men with bilateral undescended testis, and not in those with a single undescended testis (7). As early as 1975, a study found orchidopexy to be beneficial for fertility if performed on boys with unilateral undescended testis before their second birthday (e24). More recent studies have shown a fertility advantage for orchidopexy performed at the age of nine months, as compared to three years (8, e28, e29). A single study showing no advantage from early surgery was based on a small number of cases and may have been inadequately powered (e30).
Along with orchidopexy, some authors recommend preoperative treatment with intranasal gonadotropin-releasing hormone (GnRH) and/or intramuscular human chorionic gonadotropin (hCG) (9). According to some studies, treatment with GnRH analogues improves the fertility index, while hCG can sometimes induce further testicular descent even after the age of 6 months and thereby favorably affect testicular histomorphology (9, 10; e31). However, hormonal treatment is not generally recommended because of its potential side effects, including lasting damage to testicular tissue (11, 12, e32), and the risk of further delay of the necessary operation (13).
In addition to its potentially deleterious effect on fertility, numerous studies have indicated that undescended testis is associated with a higher-than-normal risk of testicular carcinoma. This risk may be due to the persistence of gonocytes with pluripotential stem-cell properties that can give rise to a carcinoma in situ (CIS) (e33). The age-standardized incidence rates of testicular carcinoma in Western populations has been estimated at 3.8 to 7.8 per 100 000 men (e34). This rare tumor thus accounts for only about 1% of cancers in men (e35) but is nonetheless the most common type of cancer in men aged 15 to 34 (e36). A review of pertinent studies revealed that men with a history of undescended testis had a 1.5- to 7.5-fold higher risk of testicular carcinoma in comparison to the normal population (6). When orchidopexy is not performed until the age of 10 years or later, this risk is elevated 2.9- to 32-fold (6, 14). It is currently debated whether orchidopexy before age 10 completely eliminates the excess risk or merely lowers it to a risk that is, at most, 2.6 times that of the normal population (6, 15, 40, e37). In any case, it is clear that only an orthopic position of the testis within the scrotum enables self-examination and facilitates the early detection of testicular tumors (40).
The increasing evidence for potential late sequelae of undescended testis has led to a repeated updating of the national and international treatment recommendations on the timing of surgery. A Cochrane Review is now in preparation (e38). In Germany, the current recommendation is that of the AWMF guideline of 2009, i.e., that the operation should be performed before the child‘s first birthday (e39). In this article, we present the findings of a retrospective, multicenter study of the implementation of the AWMF guideline in pediatric surgical units in the German state of Baden-Württemberg and compare them with the available data from other countries.
Materials and methods
Five pediatric surgical practices performing outpatient surgery (Reutlingen, Stuttgart, Tübingen, Ulm) and two inpatient hospital services of pediatric surgery (Stuttgart, Tübingen) retrospectively evaluated their data on all boys who underwent orchidopexy from 2009 to 2012. Data were obtained on all boys who had been given the specific diagnostic code for undescended testis of the International Statistical Code of Diseases and Related Health Problems, 10th Revision, in its German modification (ICD-10-G), as well as the specific German Operation and Procedure Code (Operationen- und Prozedurenschlüssel, OPS) for the surgical treatment of undescended testis. In the evaluation, it was noted whether each patient had been treated for primary or secondary undescended testis, which side was affected, and whether preoperative hormonal treatment was given (beta-hCG, GnRH analogues, or a combination of the two). As the current guidelines recommend surgery either before the age of 12 months or before the age of 24 months, the patients were classified in one of three groups depending on whether they had been operated on before their first birthday, between the first and second birthdays, or after their second birthday. Ethical approval was given by the state medical association of Baden-Württemberg. The statistical analysis was performed with JMP 10.0.2. Group sizes were expressed as percentages with a 95% confidence interval (95% CI), and trends were calculated with Pearson‘s chi-squared test at a 5% significance level. A logistic regression analysis was performed on the variables “year of surgery” and “inpatient versus outpatient treatment.” The findings were compared with data from other countries on the timing of orchidopexy. Furthermore, a targeted literature search was carried out in the PubMed, World of Science (WoS), and Cochrane Library databases for study reports in English or German, with the key words “orchidopexy” and “cryptorchidism” and/or “undescended testis” and “age” or “timing.” Each retrieved publication was considered in this review if it gave information on the patients‘ age at the time of surgery, and as long as the study involved a cohort of at least 80 patients who were born in 1990 or afterward, and who were studied postoperatively over a well-defined period of time.
Results
Findings of the present study
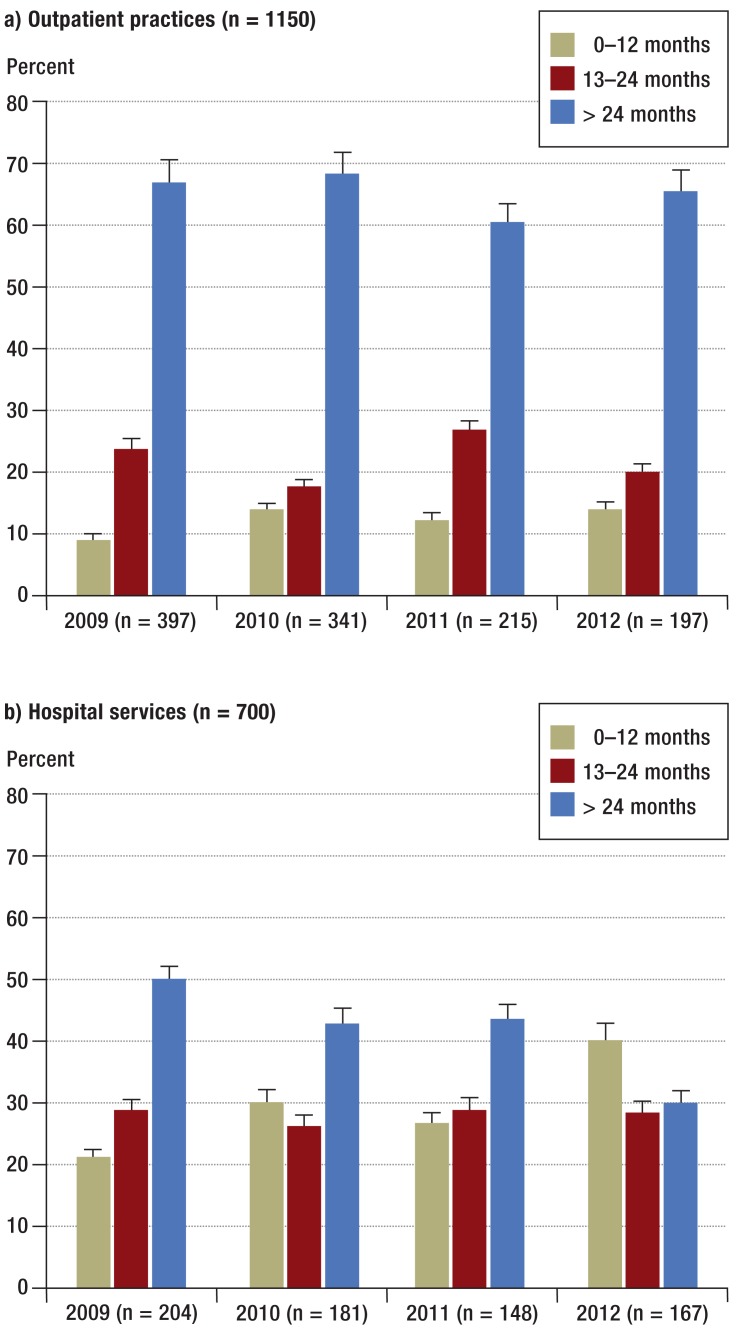
An overview of the findings is provided in Table 1. Over the period of this study, significantly fewer orchidopexies were performed for primary undescended testis (p ≤ 0.001) and significantly more for secondary undescended testis (p ≤ 0.001). The overall trend was for earlier orchidopexy (p ≤ 0.001); this trend was observable both in the inpatient setting (p = 0.0026) and in the outpatient setting (p = 0.05), with a significant difference between the two settings in the chi-squared test (Figure 1). The two settings did not differ significantly with respect to the percentage of patients given hormonal treatment before surgery. The logistic regression analysis on the effect of the calendar year (2009 through 2012) and the effect of inpatient versus outpatient treatment revealed a positive effect of a later calendar year on early surgery (2012 > 2011 > 2010 > 2009, p = 0.0002), as well as a positive effect of inpatient treatment on early surgery (p ≤ 0.0001). Of the 363 boys with secondary undescended testis, 44 (12%, 95% CI 9–15.9%) received preoperative hormonal treatment.
Table 1. Findings of the multicenter study.
| 0–12 months | 12–24 months | > 24 months | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | 95% CI | n | % | 95% CI | n | % | 95% CI | |
| Primary undescended testis | |||||||||
| 2009–2012 n=1850 | 346 | 18.7 | 17.0–20.6 | 452 | 24.4 | 22.5–26.5 | 1053 | 57.0 | 54.6–59.2 |
| 2009 n=601 | 80 | 13.3 | 10.7–16.3 | 154 | 25.6 | 22.2–29.3 | 367 | 61.1 | 57.0–65.0 |
| hCG i.m. | 13 | 2.2 | 1.2–3.7 | 41 | 6.8 | 4.9–9.1 | 26 | 4.3 | 2.9–6.3 |
| GnRH intranasal | 7 | 1.6 | 0.5–2.4 | 14 | 2.3 | 1.3–3.9 | 24 | 4.0 | 2.6–5.9 |
| hCG + GnRH | 16 | 2.7 | 1.5–4.3 | 18 | 2.99 | 1.8–4.7 | 9 | 1.5 | 0.7–2.8 |
| 2010 n=522 | 103 | 19.7 | 16.4–23.4 | 108 | 21.0 | 17.3–24.4 | 311 | 59.6 | 55.2–63.8 |
| hCG i.m. | 8 | 1.5 | 0.7–3.0 | 17 | 3.3 | 1.9–5.2 | 18 | 3.5 | 2.1–5.4 |
| GnRH intranasal | 8 | 1.5 | 0.7–3.0 | 3 | 0.6 | 0.1–1.7 | 11 | 2.1 | 1.1–3.7 |
| hCG + GnRH | 22 | 4.2 | 2.7–6.3 | 25 | 4.8 | 3.1–7.0 | 10 | 1.9 | 0.9–3.4 |
| 2011 n = 363 | 67 | 18.5 | 14.6–22.8 | 101 | 27.8 | 23.3–32.7 | 195 | 53.7 | 48.4–58.9 |
| hCG i.m. | 5 | 1.4 | 0.5–3.2 | 4 | 1.1 | 0.3–2.8 | 4 | 1.1 | 0.3–2.8 |
| GnRH intranasal | 5 | 1.4 | 0.5–3.2 | 3 | 0.8 | 0.2–2.4 | 7 | 1.9 | 0.8–3.9 |
| hCG + GnRH | 12 | 3.3 | 1.7–5.7 | 17 | 4.7 | 2.8–7.4 | 5 | 1.4 | 0.5–3.2 |
| 2012 n = 364 | 96 | 26.4 | 21.9–31.2 | 88 | 24.2 | 19.9–28.9 | 180 | 49.5 | 44.2–54.7 |
| hCG i.m. | 1 | 0.3 | 0.0–1.5 | 7 | 1.9 | 0.8–3.9 | 8 | 2.2 | 1.0–4.3 |
| GnRH intranasal | 9 | 2.5 | 1.1–4.6 | 4 | 1.1 | 0.3–2.8 | 9 | 2.5 | 1.1–4.6 |
| hCG + GnRH | 13 | 3.6 | 1.9–6.0 | 13 | 3.6 | 1.9–6.0 | 5 | 1.4 | 0.5–3.2 |
| Outpatient practices | |||||||||
| 2009 n = 397 | 36 | 9.1 | 6.4–12.3 | 95 | 23.9 | 19.8–28.4 | 266 | 67.0 | 62.4–71.6 |
| 2010 n = 341 | 48 | 14.1 | 10.6–18.2 | 60 | 17.6 | 13.7–22.1 | 233 | 68.3 | 63.1–73.2 |
| 2011 n = 215 | 27 | 12.6 | 8.4–17.7 | 58 | 27.0 | 21.2–33.4 | 130 | 60.5 | 53.6–67.1 |
| 2012 n = 197 | 28 | 14.2 | 9.7–20.0 | 40 | 20.3 | 14.9–26.6 | 129 | 65.5 | 58.4–72.1 |
| Inpatient hospital services | |||||||||
| 2009 n=204 | 44 | 21.6 | 16.127.9 | 59 | 28.9 | 22.8–35.7 | 101 | 49.5 | 42.5–56.6 |
| 2010 n=181 | 55 | 30.4 | 23.8–37.7 | 48 | 26.5 | 20.3–33.6 | 78 | 43.1 | 35.8–50.7 |
| 2011 n=148 | 40 | 27.0 | 20.1–34.9 | 43 | 29.1 | 21.9–37.1 | 65 | 43.9 | 35.8–52.3 |
| 2012 n=167 | 68 | 40.7 | 33.2–48.6 | 48 | 28.7 | 22.0–36.2 | 51 | 30.5 | 23.6–38.1 |
| Secondary undescended testis 2009–2012 n=363 | |||||||||
| 2009 n=36 | 2 | 5.6 | 0.7–18.7 | 11 | 30.6 | 16.6–48.1 | 23 | 63.9 | 46.2–80.2 |
| 2010 n=132 | 3 | 2.3 | 0.5–6.5 | 7 | 5.3 | 2.2–10.6 | 122 | 92.4 | 86.5–96.3 |
| 2011 n=84 | 2 | 2.4 | 0.3–8.3 | 3 | 3.6 | 0.7–10.1 | 79 | 94.1 | 86.7–98.0 |
| 2012 n=111 | 1 | 0.9 | 0.0–4.9 | 4 | 3.6 | 1.0–9.0 | 106 | 95.5 | 90.0–99.0 |
CI, confidence interval; hCG, human chorionic gonadotropin; GnRH, gonadotropin-releasing hormone
Figure 1.
Differences between a) outpatient practices and b) hospital services with respect to the percentage of orchidopexies in each age category
Literature search
An overview of the available data from a total of 17 other studies is shown in Table 2 (15– 31). The following variables relating to the treatment of undescended testis are displayed:
Table 2. Age at time of orchidopexy: an international comparison.
| Source | Country | Number of orchidopexies | Distinction between primary and secondary undescended testis? (indirect signs) | Time period | Mean age on diagnosis (months) | Mean age at surgery (months) | <12 months (%) (x/n) | <24 months (%) (x/n) | Variables: earlier surgery | Variables: later surgery | Trend toward earlier surgery 1: year, mean age at surgery (mo.) 2: year, percentage younger than x mo. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies based on nationwide databases | |||||||||||
| McCabe JE, 2008 (22) |
GB | 36847 | no (2nd peak at ages 7 to 9) |
1997– 2005 |
– | – | 23.8 (8770/ 34847) |
operation by pediatric surgeon | operation by general surgeon or urologist | trend (descriptive): 2: 1997, 16 <24 2: 2005, 29 <24 |
|
| Kokorowski PJ, 2010 (20) |
USA | 28204 | no | 1999– 2008 |
– | 52.8 | 18 (5031/28204) |
43 (12165/28204) |
ethnic origin, non-Hispanic white; private health insurance | ethnic origin, black or Hispanic; government health insurance | no trend 2: 1999, 40 <24 2: 2003, 44 <24 2: 2008, 42 <24 |
| Capello SA, 2006 (17) |
USA | 26575 | no | 1984– 2002 |
– | – | – | – | – | – | trend (descriptive): 2: 1984–88, 20 <24 2: 1998–93, 28 <24 2: 1994–98, 32 <24 2: 1999–02, 38 <24 |
| Springer A, 2013 (25) |
A | 19998 | no (2nd peak at ages 6 to 10) |
1993– 2009 |
– | 62.4 | 2.7 (539/19998) |
22.89 (4573/19998) |
treatment in the Tyrol (Austrian state) | – | trend (significant): 1: 1993, 72.0 1: 2004, 51.6 2: 1993, 15.2 <24 2: 2004, 26 <24 |
| Pettersson A, 2007 (15) |
S | 16983 | no | 1964– 1999 |
– | 103.2 | – | 4.2 | – | – | trend (descriptive): 2: 1964–69, 27 > 156 2: 1970–74, 15 > 156 2: 1975–79, 11 > 156 2: 1980–84, 7 > 156 2: 1985–89, 5 > 156 |
| Jensen MS, 2011 (19) |
DK | 5473 | no | 1995– 2009 |
trend: 1995–1997, 40 1998–2000, 37 2001–2003, 35 |
– | – | – | – | – | trend (significant): 1: 1995–1997, 46 1: 1998–2000, 43 1: 2001–2003, 40 |
| Yiee JH, 2012 (28) |
USA | 1365 | no (patients over age 5 yr were excluded) |
2002– 2007 |
8.2 | – | – | 87 (<18 months) n |
private health insurance, frequent check-ups, referral by a pediatrician, availabllity of a laparoscopy unit | – | – |
| Chen YF, 2013 (18) |
CN | 547 | no | 1997– 2009 |
12 | 44.7 | 20.08 (110/547) |
– | early diagnosis, urban rather than rural setting | frequent medical visits, youger diagnosing physician, older surgeon | no trend |
| Single-center studies | |||||||||||
| Bayne AP, 2011 (16) |
USA | 677 | no | 2002– 2009 |
45.2 | 50.4 | – | – | earlier surgery if genital anomaly or abdominal testis | – | – |
| Nah SA, 2014 (24) |
SGP | 513 | yes (2nd peak at age 6 yr) |
2007– 2011 |
(13.2 median) | (19.2 median) |
23 (120/513) |
58 (297/513) |
association with urogenital malformations | – | – |
| Upadhyay V, 2001 (27) |
NZ | 325 | no | 1996– 1998 |
45.2 | 52.2 | – | – | – | ||
| Moslemi MK, 2013 (23) |
IR | 252 | no | 2005– 2009 |
– | 53.3 | 17 | – | – | – | |
| Zöller G, 2005 (29) | D | 127 | yes | 2002– 2004 |
– | – | – | 13.4 | – | – | no trend: 2: 1990–94, 17 <24 2: 1995–99, 20 <24 2: 2000–04, 13 <24 |
| Lim KT, 2003 (30) |
IRL | 97 | no | 1996– 1999 |
80.4 | 67.2 | – | 28.9 (28/97) |
– | – | – |
| Multicenter studies | |||||||||||
| Marchetti F, 2012 (21) |
I | 88 | no | 2002– 2004 |
– | 22.8 | 13 (12/88) |
64 (56/88) |
– | – | – |
| Steckler RE, 1995 (26) |
USA | 329 | no | 1991– 1993 |
– | 51.6 | 17 (56/329) |
44 (145/329) |
– | – | – |
| Bruijnen CJP, 2008 (31) |
NZ | 788 | no | 1997– 2007 |
54.3 | – | – | 42.5 (335/788) |
– | – | no trend |
| Present study, 2014 | D | 1850 | yes | 2009– 2012 |
– | – | 18.6 (346/1850) |
43 (797/1850) |
Surgery in hospital providing maximal care | Surgery in pediatric surgical outpatient practice | trend: 2:2009, 13 <12 2: 2010, 20 <12 2: 2011, 18 <12 2: 2012, 26 <12 |
yr, year
GB, United Kingdom; USA, United States of America; A, Austria; S, Sweden; DK, Denmark; CN, People‘s Republic of China; SGP, Singapore; NZ, New Zealand; RIL, Republic of Ireland; I, Italy; D, Germany.
mean age at presentation with undescended testis (4 studies) (16, 19, 27, 28)
mean age at orchidopexy (11 studies) (15, 16, 18, 20, 23, 25– 27, 30, 31)
data on trends toward earlier surgery (9 studies) (15, 17– 20, 22, 25, 29, 31)
percentages of patients who underwent surgery before their first birthday (6 studies) or before their second birthday (12 studies) (15, 20– 26, 28– 31)
correlations with variables that seem linked to earlier or later surgery (7 studies) (16, 18, 20, 22, 24, 25, 28)
percentages of patients that received hormonal treatment (2 studies) (21, 29)
14 studies did not distinguish primary from secondary undescended testis. More common orchidopexies between the ages of about 6 to 10 years were described in three studies (22, 24, 25). One study indirectly excluded cases of secondary undescended testis by not including orchidopexies performed on boys over the age of five years (28). One study report provided only the median (not the mean) age of patients at the times of presentation and orchidopexy and therefore could not be fully considered in the evaluation (24).
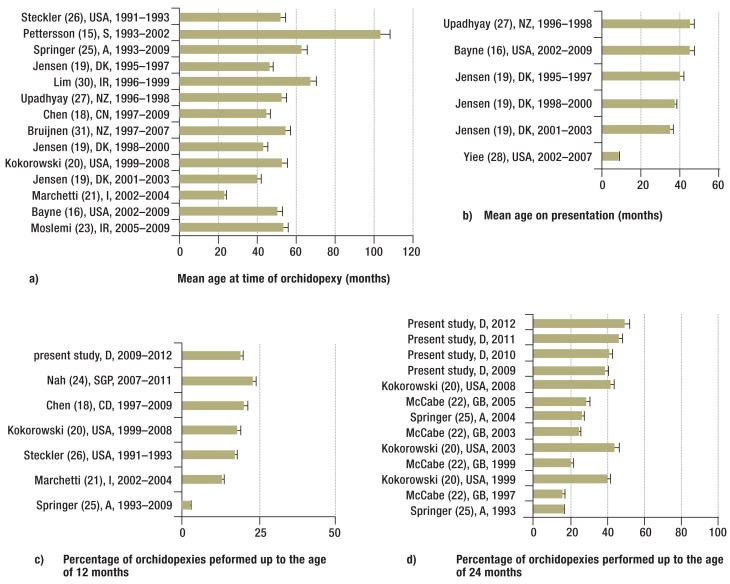
In most studies (Figure 2a), the mean age at orchidopexy ranged from 42 to 67 months (16, 18– 20, 23, 25– 27, 30, 31), with markedly better results reported in a study from Italy (21). In three of four studies, the mean age at presentation was very late (16, 19, 27, 28). A comparison of the studies that included data on the percentages of orchidopexies done under the age of 24 months and under the age of 12 months (Figures 2c and d) reveals a trend toward earlier surgery.
Figure 2.
International comparison with respect to mean age at time of orchidopexy (a), mean age on presentation (b), and the percentage of orchidopexies performed up to the age of 12 (c) or 24 (d) months.
GB, United Kingdom; USA, United States of America; A, Austria; S, Sweden; DK, Denmark; CN, People‘s Republic of China; SGP, Singapore; NZ, New Zealand; RIL, Republic of Ireland; I, Italy; D, Germany.
Hormonal treatment was given to 40 of 127 patients (31%) in one study (21), 35 of 127 patients (27.5%) in another (29), and 21.0% of the patients in the present study (95% CI, 19.3–22.8%), with the mean age at the start of hormonal treatment considerably older than 12 months. The variables potentially linked to early or late surgery are listed in Table 2.
Discussion
Over the past few decades, the recommended age for orchidopexy has been consistently lowered in all pertinent medical recommendations. In 1975, the American Academy of Pediatrics (AAP) still recommended surgery at the age of four to six years for primary undescended testis (32). Once it became clear that the histological changes in testicular tissue associated with this condition are not congenital, but in fact develop from the age of six months onward (33), the AAP in its recommendations of 1996 favored performing orchidopexy at around one year of age (34). Comparable modifications in European recommendations were seen somewhat later: the first AWMF guideline recommending orchidopexy before the second birthday appeared in 1999 (e40), and the European Association of Urologists followed suit in 2001 (35). In 2007, the Nordic Consensus recommendations were updated to favor orchidopexy between the ages of 6 and 12 months (36). The AWMF guidelines were also modified to this effect, beginning in 2007: the earliest indication of a recommendation for orchidopexy from 6 to 12 months appeared in an unofficial, preliminary version of the 2008 guidelines (e44), and the recommendation was officially accepted by the German specialty societies and published in 2009 (e39).
Multiple articles appeared on this subject in Germany as early as 2005, with reference to the AAP recommendations of 1996 (2, e41– e43). Further publications in Deutsches Ärzteblatt and regional medical periodicals were intended to raise consciousness of the need for early surgical treatment among physicians in all of the affected specialties (29, e24, e44– e55).
The implementation of these recommendations has been analyzed in studies around the world. The German data available before the present report, which were derived from a retrospective single-center study for the years 2002 to 2004, showed surgery being performed after the second birthday in more than 80% of patients (29). That study, however, was considered too small to be representative (e54). Our current findings, from the years 2009 to 2012, are somewhat more encouraging, with 18.7% of patients (95% CI, 17–20.6%) undergoing orchidopexy before their first birthday in conformity with the guidelines, although 57% (1053 of 1850 patients; 95% CI, 54.6–59.2%) still underwent orchidopexy after their second birthday. Treatment in an inpatient setting was positively associated with earlier orchidopexy. A possible and reasonable explanation for this may be that younger children are preferentially referred for inpatient treatment because of the better pediatric anesthesiological infrastructure available in hospitals as opposed to ambulatory surgical practices.
The available data from other countries reveal a marked increase in the percentages of orchidopexies being carried out under the ages of 24 months and 12 months (Figures 2c and d). Of all studies, the present one showed the highest percentage of boys undergoing orchidopexy under the age of 12 months, possibly because the analysis distinguished primary from secondary undescended testis. Yet the percentage of boys undergoing surgery in their first year is still very low in all studies, without exception.
In eight studies that were carried out in comparable periods of time, the mean age at orchidopexy ranged from 45 to 62 months (16, 18– 20, 23, 25– 27); a relatively low mean age of 22.8 months was only reported in a single study (21). This may be due to a bias in data collection, as the data in that study were taken from questionnaires voluntarily filled out by pediatricians in private practice, rather than being obtained from a representative patient cohort over a given period of time. Another study with better-than-average results showed that 87% of all orchidopexies (in 1192 of 1365 patients) had been carried out under the age of 18 months. The data that led to this conclusion were derived from a private health-insurance carrier, with the exclusion of patients with low birth weight, premature birth, and orchidopexy after the age of five years (among others); thus, there was no representative overall cohort in this study either (28). Various factors seemingly linked to early surgery (Table 2) were inconsistent across studies. Above all, improved care is to be achieved through a change in the treating physicians‘ behavior.
Only two studies included an evaluation of whether hormonal treatment was provided. As in the present study, many children were only given hormonal treatment after their first birthday, or postoperatively (21, 29). This reflects the low importance attached to hormonal treatment in clinical practice. Preoperative hormonal treatment is no longer recommended in the Nordic Consensus (36), the Swiss guidelines (e56), or other international recommendations (37, e60), but it was recommended as a complement to orchidopexy by the European Association of Urologists (2001) and in the AWMF guidelines of 1999 and 2007 (35, e39, e40). In the current, 2013 version of these guidelines, hormonal treatment is described as an option alongside surgery, but there is an explicit recommendation against giving hormonal treatment after the child‘s first birthday (38).
It is now well known that the mere knowledge that a particular recommendation is contained in a medical guideline does not automatically lead to its implementation (39, e57). From the present data, we can only speculate on the disease-specific reservations that physicians might have regarding the treatment of undescended testis. To alleviate concern about potential surgical complications, physicians should be made aware that the complications of orchidopexy (anesthesia-related incidents, hemorrhage, wound infection, recurrent undescended testis, testicular atrophy, injury to the vas deferens) are no more common when the procedure is performed in the child‘s first year than when it is peformed later, as long as it takes place in a unit with the requisite experience in pediatric surgery and pediatric urology (5, e58). The rare reported cases of spontaneous testicular descent after the age of six months should not be cited to support a general policy of watchful waiting. Such observations are likely to be based on a lack of differential diagnostic clarity, with a missed distinction between retractile and undescended testis (e59).
Limitations
One limitation of the present study is that it was restricted to a group of pediatric surgical units that are located near one another in a relatively small geographical area within a single German state. No comparable data are available for other pediatric surgical units in Baden-Württemberg, or for the other German states. The findings of the present study are, however, comparable with those of other studies from outside Germany.
This study does not include any information on orchidopexies performed by urologists or general surgeons. Interestingly, a British study found that boys operated on by pediatric surgeons were significantly younger than those operated on by urologists or general surgeons (22).
A further limitation of this study is that the patients‘ age at presentation was not determined. In four of the five studies containing data of this type, the mean age at presentation ranged from 35 to 45 months (16, 19, 27), and 57.6% of all patients (310 of 547 patients) were already past their first birthday at the time of presentation (18) (Figure 2b). We cannot exclude late presentation as a possible cause of delayed surgical treatment among the patients in the present study. This limitation is a consequence of retrospective data acquisition.
Overview
Even though early orchidopexy for primary undescended testis is now widely advocated in Germany and other countries, and even though the AWMF guideline of 2009 contains a recommendation for orchidopexy between the ages of 6 and 12 months, only 18.7% of the patients in this study actually underwent orchidopexy in the recommended age range. Studies from abroad show comparably inadequate implementation of the existing guidelines.
We conclude that the AWMF guideline on undescended testis clearly needs to be more intensively disseminated and more consistently implemented.
Key Messages.
It is recommended in the AWMF guideline that orchidopexy for primary undescended testis should be performed between the ages of 6 and 12 months. The same recommendation is found in the guidelines of the American Academy of Pediatrics (AAP) and the Nordic Consensus.
Only 18.7% of the boys in this study underwent orchidopexy at age 6–12 months as recommended in the guidelines.
The findings of comparable studies in other countries are just as bad.
Little importance is attached to hormonal treatment in clinical practice.
The AWMF guideline should be more consistently implemented.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
The authors state that they have no conflict of interest.
References
- 1.Toledano MB, Hansell AL, Jarup L, Quinn M, Jick S, Elliott P. Temporal trends in orchidopexy, Great Britain, 1992-1998. Environ Health Perspect. 2003;111:129–132. doi: 10.1289/ehp.5446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rokitansky AM. Chirurgische Therapie des Hodenhochstand. Monatsschr Kinderheilkd. 2005;153:444–450. [Google Scholar]
- 3.Virtanen HE, Cortes D, Rajpert-De Meyts E, et al. Development and descent of the testis in relation to cryptorchidism. Acta Paediatr. 2007;96:622–627. doi: 10.1111/j.1651-2227.2007.00244.x. [DOI] [PubMed] [Google Scholar]
- 4.Hutson JM, Li R, Southwell BR, Petersen BL, Thorup J, Cortes D. Germ cell development in the postnatal testis: the key to prevent malignancy in cryptorchidism? Front Endocrinol. 2012;3 doi: 10.3389/fendo.2012.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kogan SJ, Tennenbaum S, Gill B, Reda E, Levitt SB. Efficacy of orchiopexy by patient age 1 year for cryptorchidism. J Urol. 1990;144:508–509. doi: 10.1016/s0022-5347(17)39505-8. [DOI] [PubMed] [Google Scholar]
- 6.Chan E, Wayne C, Nasr A. Ideal timing of orchiopexy: a systematic review. Pediatric surgery international. 2014;30:87–97. doi: 10.1007/s00383-013-3429-y. [DOI] [PubMed] [Google Scholar]
- 7.Lee PA, O‘Leary LA, Songer NJ, Bellinger MF, LaPorte RE. Paternity after cryptorchidism: lack of correlation with age at orchidopexy. Br J Urol. 1995;75:704–707. doi: 10.1111/j.1464-410x.1995.tb07375.x. [DOI] [PubMed] [Google Scholar]
- 8.Kollin C, Stukenborg JB, Nurmio M, et al. Boys with undescended testes: endocrine, volumetric and morphometric studies on testicular function before and after orchidopexy at nine months or three years of age. J Clin Endocrinol Metab. 2012;97:4588–4595. doi: 10.1210/jc.2012-2325. [DOI] [PubMed] [Google Scholar]
- 9.Kucharski P, Niedzielski J. Neoadjuvant human Chorionic Gonadotropin (hCG) therapy may improve the position of undescended testis: a preliminary report. Cent European J Urol. 2013;66:224–228. doi: 10.5173/ceju.2013.02.art29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henna MR, Del Nero RG, Sampaio CZ, et al. Hormonal cryptorchidism therapy: systematic review with metanalysis of randomized clinical trials. Ped Surg Int. 2004;20:357–359. doi: 10.1007/s00383-004-1198-3. [DOI] [PubMed] [Google Scholar]
- 11.Cortes D, Thorup J, Visfeldt J. Hormonal treatment may harm the germ cells in 1 to 3-year-old boys with cryptorchidism. J Urol. 2000;163:1290–1292. [PubMed] [Google Scholar]
- 12.Ludwikowski B, Gonzalez R. The controversy regarding the need for hormonal treatment in boys with unilateral cryptorchidism goes on: a review of the literature. Eur J Pediatr. 2013;172:5–8. doi: 10.1007/s00431-012-1711-y. [DOI] [PubMed] [Google Scholar]
- 13.Ritzen EM. Undescended testes: a consensus on management. Eur J Endocrinol. 2008;159:87–90. doi: 10.1530/EJE-08-0181. [DOI] [PubMed] [Google Scholar]
- 14.Walsh TJ, Dall‘Era MA, Croughan MS, Carroll PR, Turek PJ. Prepubertal orchiopexy for cryptorchidism may be associated with lower risk of testicular cancer. J Urol. 2007;178:1440–1446. doi: 10.1016/j.juro.2007.05.166. [DOI] [PubMed] [Google Scholar]
- 15.Pettersson A, Richiardi L, Nordenskjold A, Kaijser M, Akre O. Age at surgery for undescended testis and risk of testicular cancer. N Engl J Med. 2007;356:1835–1841. doi: 10.1056/NEJMoa067588. [DOI] [PubMed] [Google Scholar]
- 16.Bayne AP, Alonzo DG, Hsieh MH, Roth DR. Impact of anatomical and socioeconomic factors on timing of urological consultation for boys with cryptorchidism. J Urol. 2011;186:1601–1605. doi: 10.1016/j.juro.2011.03.102. [DOI] [PubMed] [Google Scholar]
- 17.Capello SA, Giorgi LJ, Jr., Kogan BA. Orchiopexy practice patterns in New York State from 1984 to 2002. J Urol. 2006;176:1180–1183. doi: 10.1016/j.juro.2006.04.052. [DOI] [PubMed] [Google Scholar]
- 18.Chen YF, Huang WY, Huang KH, Hsieh JT, Lan CF, Chang HC. Factors related to the time to cryptorchidism surgery-A nationwide, population-based study in Taiwan. J Formos Med Assoc. 2013 doi: 10.1016/j.jfma.2013.06.001. dx.doi.org/10.1016/j.jfma.2013.06.001 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 19.Jensen MS, Olsen LH, Thulstrup AM, Bonde JP, Olsen J, Henriksen TB. Age at cryptorchidism diagnosis and orchiopexy in Denmark: a population based study of 508,964 boys born from 1995 to 2009. J Urol. 2011;186:1595–1600. doi: 10.1016/j.juro.2011.03.070. [DOI] [PubMed] [Google Scholar]
- 20.Kokorowski PJ, Routh JC, Graham DA, Nelson CP. Variations in timing of surgery among boys who underwent orchidopexy for cryptorchidism. Pediatrics. 2010;126:e576–e582. doi: 10.1542/peds.2010-0747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marchetti F, Bua J, Tornese G, Piras G, Toffol G, Ronfani L. Management of cryptorchidism: a survey of clinical practice in Italy. BMC Pediatr. 2012;12 doi: 10.1186/1471-2431-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCabe JE, Kenny SE. Orchidopexy for undescended testis in England: is it evidence based? J Ped Surg. 2008;43:353–357. doi: 10.1016/j.jpedsurg.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 23.Moslemi MK. Evaluation of orchiopexy practice patterns in patients with cryptorchidism: A single-centre study. J Pediatr Urol. 2014,;10:230–232. doi: 10.1016/j.jpurol.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Nah SA, Yeo CS, How GY, et al. Undescended testis: 513 patients‘ characteristics, age at orchidopexy and patterns of referral. Arch Dis Child. 2014;99:401–406. doi: 10.1136/archdischild-2013-305225. [DOI] [PubMed] [Google Scholar]
- 25.Springer A, Subramaniam R, Krall C, Fulop G. Orchidopexy patterns in Austria from 1993 to 2009. J Pediatr Urol. 2013;9:535–541. doi: 10.1016/j.jpurol.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Steckler RE, Zaontz MR, Skoog SJ, Rushton HG., Jr. Cryptorchidism pediatricians, and family practitioners: patterns of practice and referral. J Pediatr. 1995;127:948–951. doi: 10.1016/s0022-3476(95)70034-x. [DOI] [PubMed] [Google Scholar]
- 27.Upadhyay V, Kothari M, Manoharan M. The referral pattern for undescended testes in Auckland. N Z Med J. 2001;114:310–311. [PubMed] [Google Scholar]
- 28.Yiee JH, Saigal CS, Lai J, Copp HL, Churchill BM, Litwin MS. Timing of orchiopexy in the United States: a quality-of-care indicator. Urology. 2012;80:1121–1126. doi: 10.1016/j.urology.2012.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zöller G, Ringert RH. Hodenhochstand im Kindesalter - oft zu spät behandelt. Dtsch Arztebl. 2005;102:1750–1752. [Google Scholar]
- 30.Lim KT, Casey RG, Lennon F, Gillen P, Stokes M. Cryptorchidism: a general surgical perspective. Ir J Med Sci. 2003;172:139–140. doi: 10.1007/BF02914500. [DOI] [PubMed] [Google Scholar]
- 31.Bruijnen CJ, Vogels HD, Beasley SW. Review of the extent to which orchidopexy is performed at the optimal age: implications for health services. ANZ Journal of Surgery. 2008;78:1006–1009. doi: 10.1111/j.1445-2197.2008.04745.x. [DOI] [PubMed] [Google Scholar]
- 32.Kelalis P, Bunge R, Barkin M, et al. The timing of elective surgery on the genitalia of male children with particular reference to undescended testes and hypospadias. Pediatrics. 1975;56:479–483. [PubMed] [Google Scholar]
- 33.Hadziselimovic F, Herzog B, Buser M. Development of cryptorchid testes. Eur J Pediatr. 1987;146:8–12. doi: 10.1007/BF00452859. [DOI] [PubMed] [Google Scholar]
- 34.American Academy of Pediatrics. Timing of elective surgery on the genitalia of male children with particular reference to the risks, benefits, and psychological effects of surgery and anesthesia. Pediatrics. 1996;97:590–594. [PubMed] [Google Scholar]
- 35.Riedmiller H, Androulakakis P, Beurton D, Kocvara R, Gerharz E. EAU guidelines on paediatric urology. Eur Urol. 2001;40:589–599. doi: 10.1159/000049841. [DOI] [PubMed] [Google Scholar]
- 36.Ritzen EM, Bergh A, Bjerknes R, et al. Nordic consensus on treatment of undescended testes. Acta Paediatr. 2007;96:638–643. doi: 10.1111/j.1651-2227.2006.00159.x. [DOI] [PubMed] [Google Scholar]
- 37.Callaghan P. Undescended testis. Pediatr Rev. 2000;21 [PubMed] [Google Scholar]
- 38.Deutsche Gesellschaft für Kinderchirurgie, der Deutsche Gesellschaft für Urologie, der Deutsche Gesellschaft für Kinder- und Jugendmedizin, vertreten durch die Arbeitsgemeinschaft für pädiatrische Endokrinologie (APE) www.awmf.org/leitlinien/detail/ll/006-022.html. AWMF-Leitlinie Nr. 006/022, 2k, Hodenhochstand - Maldeszensus testis 2013. (last accessed on 23 July 2014) [Google Scholar]
- 39.Karbach U, Schubert I, Hagemeister J, Ernstmann N, Pfaff H, Hopp HW. Physicians‘ knowledge of and compliance with guidelines: an exploratory study in cardiovascular diseases. Dtsch Arztebl Int. 2011;108:61–69. doi: 10.3238/arztebl.2011.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ilic D, Misso ML. Screening for testicular cancer. The Cochrane Database of Systematic Reviews. 2011: doi: 10.1002/14651858.CD007853.pub2. Cd007853. [DOI] [PubMed] [Google Scholar]
- e1.Virtanen HE, Bjerknes R, Cortes D, et al. Cryptorchidism: classification, prevalence and long-term consequences. Acta Paediatr. 2007;96:611–616. doi: 10.1111/j.1651-2227.2007.00241.x. [DOI] [PubMed] [Google Scholar]
- e2.Chilvers C, Pike MC, Forman D, Fogelman K, Wadsworth ME. Apparent doubling of frequency of undescended testis in England and Wales in 1962-81. Lancet. 1984;2:330–332. doi: 10.1016/s0140-6736(84)92697-7. [DOI] [PubMed] [Google Scholar]
- e3.Cortes D, Kjellberg EM, Breddam M, Thorup J. The true incidence of cryptorchidism in Denmark. J Urol. 2008;179:314–318. doi: 10.1016/j.juro.2007.08.158. [DOI] [PubMed] [Google Scholar]
- e4.Berkowitz GS, Lapinski RH, Dolgin SE, Gazella JG, Bodian CA, Holzman IR. Prevalence and natural history of cryptorchidism. Pediatrics. 1993;92:44–49. [PubMed] [Google Scholar]
- e5.Boisen KA, Kaleva M, Main KM, et al. Difference in prevalence of congenital cryptorchidism in infants between two Nordic countries. Lancet. 2004;363:1264–1269. doi: 10.1016/S0140-6736(04)15998-9. [DOI] [PubMed] [Google Scholar]
- e6.Ghirri P, Ciulli C, Vuerich M, et al. Incidence at birth and natural history of cryptorchidism: a study of 10 730 consecutive male infants. J Endocrinol Invest. 2002;25:709–715. doi: 10.1007/BF03345105. [DOI] [PubMed] [Google Scholar]
- e7.Preiksa RT, Zilaitiene B, Matulevicius V, et al. Higher than expected prevalence of congenital cryptorchidism in Lithuania: a study of 1 204 boys at birth and 1 year follow-up. Hum Reprod. 2005;20:1928–1932. doi: 10.1093/humrep/deh887. [DOI] [PubMed] [Google Scholar]
- e8.Scorer CG. The Descent of the Testis. Arch Dis Child. 1964;39:605–609. doi: 10.1136/adc.39.208.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e9.Thong M, Lim C, Fatimah H. Undescended testes: incidence in 1 002 consecutive male infants and outcome at 1 year of age. Ped Surg Int. 1998;13:37–41. doi: 10.1007/s003830050239. [DOI] [PubMed] [Google Scholar]
- e10.Virtanen HE, Toppari J. Epidemiology and pathogenesis of cryptorchidism. Hum Reprod Update. 2008;14:49–58. doi: 10.1093/humupd/dmm027. [DOI] [PubMed] [Google Scholar]
- e11.Hutson JM. Undescended testis: the underlying mechanisms and the effects on germ cells that cause infertility and cancer. J Ped Surg. 2013;48:903–908. doi: 10.1016/j.jpedsurg.2013.02.001. [DOI] [PubMed] [Google Scholar]
- e12.Hamza AF, Elrahim M, Elnagar, Maaty SA, Bassiouny E, Jehannin B. Testicular descent: when to interfere? Eur J Pediatr Surg. 2001;11:173–176. doi: 10.1055/s-2001-15484. [DOI] [PubMed] [Google Scholar]
- e13.Hack WW, Goede J, van der Voort-Doedens LM, Meijer RW. Acquired undescended testis: putting the pieces together. Int J Androl. 2012;35:41–45. doi: 10.1111/j.1365-2605.2011.01155.x. [DOI] [PubMed] [Google Scholar]
- e14.Hadziselimovic F, Herzog B. The importance of both an early orchidopexy and germ cell maturation for fertility. Lancet. 2001;358:1156–1157. doi: 10.1016/S0140-6736(01)06274-2. [DOI] [PubMed] [Google Scholar]
- e15.Huff DS, Fenig DM, Canning DA, Carr MG, Zderic SA, Snyder HM., 3rd Abnormal germ cell development in cryptorchidism. Horm Res. 2001;55:11–17. doi: 10.1159/000049957. [DOI] [PubMed] [Google Scholar]
- e16.Huff DS, Hadziselimovic F, Snyder HM, 3rd, Blythe B, Ducket JW. Histologic maldevelopment of unilaterally cryptorchid testes and their descended partners. Eur J Pediatr. 1993;152:11–4. [PubMed] [Google Scholar]
- e17.Taskinen S, Wikstrom S. Effect of age at operation, location of testis and preoperative hormonal treatment on testicular growth after cryptorchidism. J Urol. 1997;158:471–473. [PubMed] [Google Scholar]
- e18.Nagar H, Haddad R. Impact of early orchidopexy on testicular growth. Brit J Urol. 1997;80:334–335. doi: 10.1046/j.1464-410x.1997.t01-1-00301.x. [DOI] [PubMed] [Google Scholar]
- e19.Riebel T, Herrmann C, Wit J, Sellin S. Ultrasonographic late results after surgically treated cryptorchidism. Pediatr Radiol. 2000;30:151–155. doi: 10.1007/s002470050034. [DOI] [PubMed] [Google Scholar]
- e20.Park KH, Lee JH, Han JJ, Lee SD, Song SY. Histological evidences suggest recommending orchiopexy within the first year of life for children with unilateral inguinal cryptorchid testis. Int J Urol. 2007;14:616–621. doi: 10.1111/j.1442-2042.2007.01788.x. [DOI] [PubMed] [Google Scholar]
- e21.Tasian GE, Hittelman AB, Kim GE, DiSandro MJ, Baskin LS. Age at orchiopexy and testis palpability predict germ and Leydig cell loss: clinical predictors of adverse histological features of cryptorchidism. J Urol. 2009;182:704–709. doi: 10.1016/j.juro.2009.04.032. [DOI] [PubMed] [Google Scholar]
- e22.Cortes D, Thorup JM, Visfeldt J. Cryptorchidism: aspects of fertility and neoplasms. A study including data of 1335 consecutive boys who underwent testicular biopsy simultaneously with surgery for cryptorchidism. Horm Res. 2001;55:21–27. doi: 10.1159/000049959. [DOI] [PubMed] [Google Scholar]
- e23.Wojciechowski K. Long-term results of undescended testicle operative treatment. Progr Pediatr Surg. 1977;10:296–304. [PubMed] [Google Scholar]
- e24.Ludwig G, Potempa J. Optimal time for treating cryptorchism (author‘s transl) Dtsch Med Wochenschr. 1975;100:680–683. doi: 10.1055/s-0028-1106278. [DOI] [PubMed] [Google Scholar]
- e25.Knorr D. Sex differentiation disorders. Internist (Berl) 1979;20:85–94. [PubMed] [Google Scholar]
- e26.Hortling H, Chapelle A, Johansson CJ, Niemi M, Sulamaa M. An endocrinologic follow-up study of operated cases of cryptorchism. J Clin Endocrinol Metab. 1967;27:120–129. doi: 10.1210/jcem-27-1-120. [DOI] [PubMed] [Google Scholar]
- e27.Chilvers C, Dudley NE, Gough MH, Jackson MB, Pike MC. Undescended testis: the effect of treatment on subsequent risk of subfertility and malignancy. J Pediatr Surg. 1986;21:691–696. doi: 10.1016/s0022-3468(86)80389-x. [DOI] [PubMed] [Google Scholar]
- e28.Kollin C, Hesser U, Ritzen EM, Karpe B. Testicular growth from birth to two years of age, and the effect of orchidopexy at age nine months: a randomized, controlled study. Acta Paediatr. 2006;95:318–324. doi: 10.1080/08035250500423812. [DOI] [PubMed] [Google Scholar]
- e29.Kollin C, Karpe B, Hesser U, Granholm T, Ritzen EM. Surgical treatment of unilaterally undescended testes: testicular growth after randomization to orchiopexy at age 9 months or 3 years. J Urol. 2007;178:1589–1593. doi: 10.1016/j.juro.2007.03.173. [DOI] [PubMed] [Google Scholar]
- e30.van Brakel J, Kranse R, de Muinck Keizer-Schrama SM, et al. Fertility potential in men with a history of congenital undescended testes: a long-term follow-up study. Andrology. 2013;1:100–108. doi: 10.1111/j.2047-2927.2012.00024.x. [DOI] [PubMed] [Google Scholar]
- e31.Pyorala S, Huttunen NP, Uhari M. A review and meta-analysis of hormonal treatment of cryptorchidism. J Clin Endocrinol Metab. 1995;80:2795–2799. doi: 10.1210/jcem.80.9.7673426. [DOI] [PubMed] [Google Scholar]
- e32.Dunkel L, Taskinen S, Hovatta O, Tilly JL, Wikstrom S. Germ cell apoptosis after treatment of cryptorchidism with human chorionic gonadotropin is associated with impaired reproductive function in the adult. J Clin Invest. 1997;100:2341–2346. doi: 10.1172/JCI119773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e33.Hutson JM, Li R, Southwell BR, Petersen BL, Thorup J, Cortes D. Germ cell development in the postnatal testis: the key to prevent malignancy in cryptorchidism? Front Endocrinol (Lausanne) 2012;3 doi: 10.3389/fendo.2012.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e34.Shanmugalingam T, Soultati A, Chowdhury S, Rudman S, Van Hemelrijck M. Global incidence and outcome of testicular cancer. Clin Epidemiol. 2013;5:417–427. doi: 10.2147/CLEP.S34430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e35.Liu S, Wen SW, Mao Y, Mery L, Rouleau J. Birth cohort effects underlying the increasing testicular cancer incidence in Canada. Can J Public Health. 1999;90:176–180. doi: 10.1007/BF03404502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e36.Ferguson L, Agoulnik AI. Testicular cancer and cryptorchidism. Front Endocrinol. 2013;4 doi: 10.3389/fendo.2013.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e37.Strader CH, Weiss NS, Daling JR, Karagas MR, McKnight B. Cryptorchism, orchiopexy, and the risk of testicular cancer. Am J Epidemiol. 1988;127:1013–1018. doi: 10.1093/oxfordjournals.aje.a114877. [DOI] [PubMed] [Google Scholar]
- e38.Deshpande AV, Michail P, Smith GH. Interventions for undescended testes in children. Cochrane Database of Systematic Reviews. 2014 DOI: 10.1002/14651858.CD010978. [Google Scholar]
- e39.Deutsche Gesellschaft für Kinderchirurgie, Deutsche Gesellschaft für Urologie, Deutsche Gesellschaft für Kinder- und Jugendmedizin, vertreten durch die Arbeitsgemeinschaft für pädiatrische Endokrinologie (APE) www.awmf-online.de/e40. AWMF-Leitlinie Nr. 006/022, 2k, Hodenhochstand - Maldeszensus testis, 2009, https://web.archive.org/web/20100131230738/ . (last accessed on 23 July 2014) [Google Scholar]
- e40.Deutsche Gesellschaft für Kinderchirurgie. https://web.archive.org/web/20010331105838/http://awmf.org/ AWMF-Leitlinie Nr. 006/022, 1, Hodenhochstand, 1999. (last accessed on 23 July 2014) [Google Scholar]
- e41.Grüters A. Entwicklung und Entwicklungsstörungen der Hoden. Monatsschr Kinderheilkd. 2005;153:424–429. [Google Scholar]
- e42.Hiort O, Wünsch L, Holterhus PM. Differentialdiagnostische Überlegungen beim Hodenhochstand. Monatsschr Kinderheilkd. 2005;153:430–435. [Google Scholar]
- e43.Rieger C, Schulte-Wissermann H. Hodenhochstand. Trainingsprogramm für die Weiterbildung zum Kinderarzt. Monatsschr Kinderheilkd. 2005;153:451–452. [Google Scholar]
- e44.Mathers MJ, Sperling H, Rubben H, Roth S. The undescended testis: diagnosis, treatment and long-term consequences. Dtsch Arztebl Int. 2009;106:527–532. doi: 10.3238/arztebl.2009.0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e45.Haß HJ, Krause H, Liehr UB, Rißmann A. Aktuelle Therapierichtlinien zur Behandlung des Hodenhochstands. Ärzteblatt Sachsen-Anhalt. 2010;21:23–54. [Google Scholar]
- e46.Cortes D, Brandt B, Thorup J. Direct mixed antiglobulin reaction (MAR) test in semen at follow-up after testicular biopsy of maldescended testes operated in puberty. Z Kinderchir. 1990;45:227–228. doi: 10.1055/s-2008-1042587. [DOI] [PubMed] [Google Scholar]
- e47.Lentze MJ. Hodenhochstand. Monatsschr Kinderheilkd. 2005;153 [Google Scholar]
- e48.Albers N. Konservative Therapie des Hodenhochstandes. Monatsschr Kinderheilkd. 2005;153:436–443. [Google Scholar]
- e49.Hadziselimovic F, Hoecht B. Testicular histology related to fertility outcome and postpubertal hormone status in cryptorchidism. Klin Padiatr. 2008;220:302–307. doi: 10.1055/s-2007-993194. [DOI] [PubMed] [Google Scholar]
- e50.Butenandt O, Knorr D. Maldescensus testis, therapy and prognosis. Fortschr Med. 1979;97:1453–1455. [PubMed] [Google Scholar]
- e51.Städtler F. Morphological findings. Dtsch Arztebl Int. 2010;107 doi: 10.3238/arztebl.2010.0073b. Correspondence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e52.Becker K. Clinical remarks. Dtsch Arztebl Int. 2010;107 doi: 10.3238/arztebl.2010.0073a. Correspondence. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e53.Zöller G. Hodenhochstand im Kindesalter - oft zu spät behandelt: Schlusswort. Dtsch Arztebl. 2006;103 [Google Scholar]
- e54.Schwarzt HP, Dietz, HG. Hodenhochstand im Kindesalter - oft zu spät behandelt: Zahlen nicht repräsentativ. Dtsch Arztebl. 2006;103 [Google Scholar]
- e55.Richter J. Hodenhochstand im Kindesalter - oft zu spät behandelt: Präventionsgesetz ist zu fordern. Dtsch Arztebl. 2006;103 [Google Scholar]
- e56.Fanconi S, Reinberg O, Gapany C, et al. Pediatrics. Rev Med Suisse. 2008;4:61–66. [PubMed] [Google Scholar]
- e57.Kunz U. Leitlinien in der Medizin: Anwendung, Einstellung und Barrieren - Eine Befragung Berliner Hausärzte. äzq Schriftenreihe. 2006;27:1–72. [Google Scholar]
- e58.Hart Prieto MC, Jones PA. Are general paediatric surgery outcomes comparable between district general hospital and regional referral centres? Ann R Coll Surg Engl. 2011;93:548–550. doi: 10.1308/147870811X13137608454894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e59.Goh DW, Hutson JM. The retractile testis: time for a reappraisal. J Paediatri Child Health. 1993;29:407–408. doi: 10.1111/j.1440-1754.1993.tb03008.x. [DOI] [PubMed] [Google Scholar]
- e60.Kolon TF, Herndon CDA, Baker LA, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol. 2014 doi: 10.1016/j.juro.2014.05.005. doi: 10.1016/j.juro.2014.05.005 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]