Abstract
Background:
Ketamine is used as a general anesthetic for short-term surgical procedures. The aim of this study is to compare the effect of intravenous (IV) ketamine and intramuscular (IM) ketamine in children admitted to the emergency department (ED).
Materials and Methods:
This is a clinical trial on 60 patients who were randomly classified into two groups. The first group received IV ketamine (1 mg/kg) and the second received IM ketamine (4 mg/kg). Data were collected before, during, and after the procedure. Time to reach sedation, severity of the sedation, and complications of the drug until discharge were studied.
Results:
In this study, 60 patients were evaluated. The average length of the procedures was similar in both groups (P > 0.05). According to this study, sedation levels in the two groups in 5, 10, and 15 minutes did not show significant differences (P > 0.05), but there was a significant difference in sedation levels of patients in 30, 35, 40, and 45 minutes during sedation (P = 0.03, P = 0.04, P = 0.03 and P = 0.05). There was no significant difference in the incidence of complications between the two groups.
Dicussion:
There was no significant difference in complications and level of sedation in both groups, but sedation was longer in the IM group; so, IV ketamine is the desirable approach for orthopedic procedures in sedating children.
Keywords: Children sedation, intramuscular ketamine, intravenous ketamine, orthopedic procedures
INTRODUCTION
Painful diagnostic and therapeutic procedures performed in the emergency department (ED) for children is a routine action. Today, the number of therapeutic and diagnostic techniques that are used in the ED has increased;[1,2,3,4,5,6,7] so, the use of sedation for painful procedures in emergency care for children with a standard diet and various medical regimens has special benefits.[8,9,10,11,12] However, different drugs that are used for children have various dangerous side effects.[13,14] There are several ways to achieve adequate sedation.[9,10,14,15] One of the most important effective sedative methods is using ketamine as an anesthetic drug.[11,12,16] Ketamine is now commonly used in the pediatric ED for sedation and can be administrated intramuscularly (IM) and/or intravenously (IV).[10,11] Comparison of IV with IM ketamine may assist in selecting the most effective and safest procedure for medical care in the ED. The aim of this study is to compare effects of IV ketamine with IM ketamine in children who were admitted to the ED and were in need of sedation for therapeutic procedures.
MATERIALS AND METHODS
This is a single-blind, clinical trial on 60 pediatric patients who were referred to the ED during 2010. All patients were enrolled after informed consent was obtained from their parents. There was no added cost for the patients due to this study. All the patients were alert, hemodynamically stable, and less than five years old. They were randomized by an allocation software to two groups that received IV ketamine (1 mg/kg) and IM ketamine (4 mg/kg). Information about the patients during and after the procedure, time to reach sedation, severity of sedation, and complications of the drug until discharge were obtained. All drugs had been prepared in 5 mL syringes in the ED and also contained 0.02 mg/kg atropin and 0.05 mg/kg midazolam. All injections were administered under the supervision of the Professor of Emergency Medicine. Exclusion criteria were: (1) Age less than 12 months, (2) age over 5 years, (3) history of known allergy to the drugs, (4) patients with open globe injury, (5) patients with traumatic brain injury, (6) patients with a history of psychiatric disorders, and (7) patients with memory impairment or cognitive impairment. The Ramsay sedation scale was used to assess the level of sedation.
Ramsay sedation scale:
Patient is co-operative, oriented, and tranquil
Patient is anxious and agitated or restless, or both
Patient responds to commands only
Patient exhibits brisk response to light glabellar tap or loud auditory stimulus
Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus
Patient exhibits no response.
Recovery time was calculated from the last dose of drug adminstrated up to the time patients achieved discharge criteria.
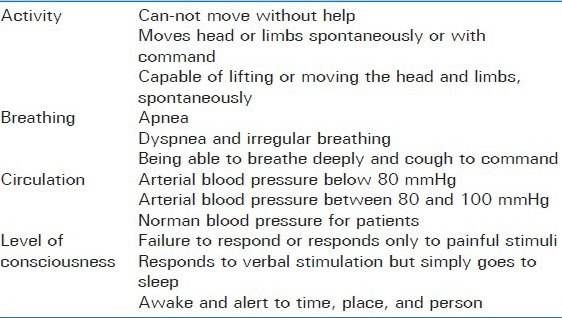
Patients with scores equal to or more than 7 were considered safe for discharge [Table 1].
Table 1.
Discharge criteria consistings of for parts
Sedation levels and side effects based on data collection forms at 5, 10, 15, 20, 30, 45, 50, 55, and 60 minutes after injection were measured. After collecting data, SPSS software version 15 descriptive and inferential analysis was used for analysis; P < 0.05 was considered significant.
RESULTS
In this study, 60 patients were evaluated; 18 patients (30%) were famale and 42 patients (70%) were male. Mean age of the group who received 1 mg/kg ketamine IV was 2.4 ± 7.9 years and for patients who recivied 4 mg/kg ketamine IM, it was 2.7 ± 7.3 years.
Average length of time from receiving sedation medication up to the child awakening in ketamine IV and ketamine IM groups was 36.2 ± 0.5 and 56.5 ± 0.6 minutes, respectively. All children were awake and conscious during the first hour after the adminstaration of the drug. Continued evaluation of all children up to three hours after sedation was done to control side effects such as convulsions, increased salivation, rash, apnea, airway manangement such as the need for intubation, incidence of delirium, hypotension, hypoxia, and tachycardia, but no cases experienced such side effects.
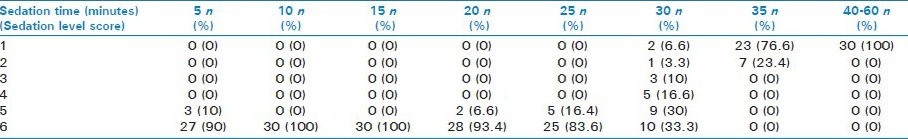
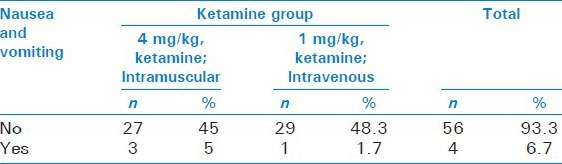
The only side effect observed in our study was the incidence of nausea and vomiting in both groups. All cases experienced vomiting in the late phase of recovery after sedation, but its incidence according to the age of the patients showed no significant difference (P = 0.07). The average length of procedures was similar in both groups (P > 0.05). Sedation levels in the two groups at 5, 10, and 15 minutes did not show significant differences (P > 0.05), but the study at 30, 35, 40, and 45 minutes showed a significant difference in sedation levels (P = 0.03, P = 0.04, P = 0.03, and P = 0.05). All the patients were awake after 50 minutes in both groups [Tables 2 and 3].
Table 2.
Sedation time and sedation level scores in patients who received 4 mg/kg intramuscular ketamine
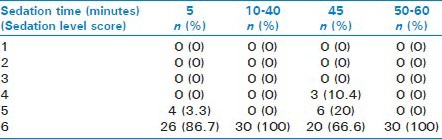
Table 3.
Sedation time and sedation level scores in patients who received 1 mg/kg intravenous ketamine
There were no significant differences between the two groups in the incidence of vomiting (P > 0.05) [Table 4]. Also, there was no significant difference between the two groups in the incidence of other disorders or complications related to the adminstaration of IV and IM ketamine. The mean of duration of sedation differed significantly between the two groups (P = 0.05) and children in the IM ketamine group experienced longer sedation than the other group.
Table 4.
Complications of treatment
DISCUSSION
In this study, 60 children were studied to compare the effects of IV and IM ketamine in pediatric sedation for orthopedic procedures. Shorter duration of sedation in patients who received IV ketamine was the most important finding that led to earlier return of consciousness and discharge of the patiens. This finding may lower the anxiety of parents.
According to a study by Joe E. Wathen et al. about the usage of IV ketamine for pediatric sedation (1 mg/kg IV) in the emergency department, it was seen that the incidence of pulmonary complications was 4.5%, vomiting 18.7%, and 7.1% incidence of hallucinations and delusions in patients who received ketamine.
In another study in 2006 by Roback MG, et al., the effects of IM and IV sedation using ketamine in children admitted to the ED with orthopedic trauma were compared. The results show that the incidence of nausea was higher (11.9%) in the group who received IM ketamine.[4]
Our study showed the incidence of vomiting (5 vs. 1.7%) in the ketamine IM group and ketamine IV group. The incidence of vomiting was higher in the patients who received IM ketamine.
Roback MG et al. in a study reported that the duration of sedation by IM ketamine was more than in the IV route; this is similar to our results (36.2 ± 0.5 minutes in the IV group vs. 56.5 ± 0.6 minutes in IM ketamine group). All the children were awake and conscious during the first hour after adminstration of the drug. Other side effects during evaluation were not observed.
Considering better control of the sedation of patients and lack of side effects, ketamine is more effective and safer in both IV and IM adminstration. IV administration of ketamine, due to faster results and quicker healing and awakening (shorter-term sedation), can have a relatively better prognosis. It requires minimum serious intervention and is recommended for pediatric sedation, but exact control of the duration of sedation and careful examination of the side effects in patients is necessary and should be scrutinizingly evaluated. No significant difference was seen in vomiting complications between the two groups. On the other hand, the recovery time did not differ neither did the risk of aspiration.
CONCLUSION
There was no significant difference in complications between the two groups, but a longer duration of sedation was observed in the IM ketamine group which makes IV ketamine more desirable. We recommend that in future studies, the clinical status of patients and its alteration be evaluated precisely to determine the most efficient method of pediatric sedation.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Chudnofsky CR, Lozon MM. Procedural Sedation and Analgesia. In: Marx JA, Hockberger RS, Walls RM, editors. Rosen's emergency medicine: Concepts and clinical practice. 6th ed. Philadelphia PA: Mosby; 2006. pp. 2938–55. [Google Scholar]
- 2.Shah RK, Singh RP, Prasad N. Sedation with ketamine: A Safe and effective anaesthetic agent for children in the developing world. Nepal Med Coll J. 2003;5:9–13. [PubMed] [Google Scholar]
- 3.Karapinar B, Yilmaz D, Demirağ K, Kantar M. Sedation with ketamine and midazolam for painful procedures in children. Pediatr Int. 2006;48:146–51. doi: 10.1111/j.1442-200X.2006.02186.x. [DOI] [PubMed] [Google Scholar]
- 4.Roback MG, Wathen JE, Mackenzie T, Bajaj L. A Randomized, Controlled trial of IV versos IM Ketamine for Sedation of pediatric receiving emergency department Orthopedic procedures. Ann Emerg Med. 2006;48:605–12. doi: 10.1016/j.annemergmed.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Green SM, Johnson NE. Ketamine sedation for pediatric procedures: Part 2, Review and implications. Ann Emerg Med. 1990;19:1033–46. doi: 10.1016/s0196-0644(05)82569-7. [DOI] [PubMed] [Google Scholar]
- 6.Green SM, Hummel CB, Wittlake WA, Rothrock SG, Hopkins GA, Garrett W. What is the optimal dose of intramuscular ketamine for pediatric sedation. Acad Emerg Med. 1999;6:21–6. doi: 10.1111/j.1553-2712.1999.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 7.Walls R, Murphy MF. Philadelphia, PA: Lippincott Williams and Wilkins; 2004. Manual of emergency airway management. [Google Scholar]
- 8.Qureshi FA, Mellis PT, McFadden MA. Efficacy of oral ketamine for providing sedation and analgesia to children requiring laceration repair. Pediatr Emerg Care. 1995;11:93–7. doi: 10.1097/00006565-199504000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Horiuchi T, Kawaguchi M, Kurehara K, Kawaraguchi Y, Sasaoka N, Furuya H. Evaluation of relatively low dose oforal transmucosal ketamine premedication in children: A comparison with oral midazolam. Paediatr Anaesth. 2005;15:643–7. doi: 10.1111/j.1460-9592.2004.01513.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller R, Fleisher L, Roger A. Miller's Anesthesia. 6th ed. Vol. 1. New York: Churchill livingstone; 2005. General anesthesia; pp. 379–410. [Google Scholar]
- 11.White PF, Way WL, Trevor AJ. Ketamine: Its pharmacology and therapeutic uses. Anesthesiology. 1982;56:119–36. doi: 10.1097/00000542-198202000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Hall J, Collyer T. Ketamine sedation in children. Emerg Nurse. 2007;15:24–7. doi: 10.7748/en2007.09.15.5.24.c4251. [DOI] [PubMed] [Google Scholar]
- 13.Cravero JP, Blike GT. Review of pediatric sedation. Anesth Analg. 2004;99:1355–64. doi: 10.1213/01.ANE.0000134810.60270.E8. [DOI] [PubMed] [Google Scholar]
- 14.Melzack R, McGill T. Major properties and scoring methods of pain. Pain. 1995;1:277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 15.Finkel JC, Pestieau SR, Quezado ZM. Ketamine as an adjuvant for treatment of cancer pain in children and adolescents. Pain. 2007;8:515–21. doi: 10.1016/j.jpain.2007.02.429. [DOI] [PubMed] [Google Scholar]
- 16.Neil S. Morton MBChB, FRCA, FRCPCH Ketamine for procedural sedation and analgesia in pediatric emergency medicine: A UK perspective Pediatric Anesthesia. 2007;18(1):25–9. doi: 10.1111/j.1460-9592.2007.02395.x. [DOI] [PubMed] [Google Scholar]


