Abstract
Biomarker science brings great promise to clinical medicine. This is especially true in the era of technology miniaturization, rapid dissemination of knowledge, and point-of-care (POC) implementation of novel diagnostics. Despite this tremendous progress, the journey from a candidate biomarker to a scientifically validated biomarker continues to be an arduous one. In addition to substantial financial resources, biomarker research requires considerable expertise and a multidisciplinary approach. Investigational designs must also be taken into account, with the randomized controlled trial remaining the “gold standard”. The authors present a condensed overview of biomarker science and associated investigational methods, followed by specific examples from clinical areas where biomarker development and/or implementation resulted in tangible enhancements in patient care. This manuscript also serves as a call to arms for the establishment of a truly global, well-coordinated infrastructure dedicated to biomarker research and development, with focus on delivery of the latest discoveries directly to the patient via point-of-care technology.
Keywords: Biomarker research, global approach, point-of-care testing, patient-centered approach
The term “biomarker” was introduced as a Medical Subject Hesading (MeSH) in 1989 and was defined as, “measurable and quantifiable biological parameter (e.g. specific enzyme concentration, specific hormone concentration, specific gene phenotype distribution in a population, presence of biological substances) which serves as an index for health- and physiology-related assessments, such as disease risk, psychiatric disorders, environmental exposure and its effects, disease diagnosis, metabolic processes, substance abuse, pregnancy, cell line development, epidemiologic studies, etc.”[1] By 2001 the term was further standardized as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathologic processes, or pharmacologic responses to a therapeutic intervention”.[2]
Biomarkers have a defining characteristic or property that is objectively measured and evaluated as an indicator of normal biological, pathologic, or pharmacologic processes/responses to a therapeutic intervention.[2,3,4] The general purpose of biomarkers includes identification of disease risk, diagnosis of disease, estimation of disease severity, guiding interventions, and monitoring patients’ therapeutic responses.[2,4,5] When utilized clinically, biomarkers should assist in the determination of whether a drug or an intervention is safe and effective, and optimally can decrease the time and cost required to identify and/or treat the disease.
The emergence of biomarkers promised improved diagnosis, but only a small number of clinical disciplines saw tangible benefits from biomarker research. While modern technological advances resulted in more than 150,000 scientific reports documenting thousands of potential biomarkers, only about 100 have been validated.[6] George Poste in his Nature commentary argues that, “…the dismal patchwork of fragmented research on disease-associated biomarkers should be replaced by a coordinated big science approach”.[6] Standardized methodologies and large sample sizes are needed to bridge the science of biomarkers and that of people's health. There are also challenges involving scientific culture and analytical technologies in academia, where much of the biomarker research occurs. Consequently, Poste's point regarding the need for large collaborative networks that include industry as well as academia is well taken, and will be the optimal approach to reduce research costs, health care expenditures, and deliver usable and sustainable results.[6]
A perfect biomarker should be readily obtainable, and the corresponding results should be available instantaneously or near-instantaneously. In addition, the most optimal delivery platform would be portable, that is, point-of-care (POC) testing.[7,8,9] Of course, high sensitivity and specificity would be desirable. In an idealized world, a “perfect biomarker” would approach 100% sensitivity and specificity for its diagnostic indication.
MEASUREMENT AND METHODOLOGICAL CONSIDERATIONS
In measuring and reporting biomarkers, there are multiple factors to consider. Biomarkers are often reflected using surrogate end points, which mirror “clinical end points” of interest. For example, lactic acidosis is the clinical surrogate for determination of ongoing limb ischemia, while a clinical end point would be a trait or variable that reflects how a patient feels, functions or survives. Although most biomarkers are far from perfect, they should all ideally possess certain basic characteristics, including reliability (that is, be accurate and reproducible) and validity (measuring what they are supposed to measure). Sensitivity and specificity are key parameters in this regard, as are likelihood ratios, which further define the probability that a biomarker is actually tied to disease outcomes through POC testing.[10]
In addition, there are fundamental biomarker classifications and uses. Prognostic biomarkers are associated with outcomes and allow risk assessment in relation to treatment decisions. In contrast, predictive biomarkers are associated with determining or predicting treatment response, and are helpful in individualizing therapy. In both instances, researchers must determine whether the biomarker of interest is: (a) a true risk factor; (b) a confounding variable (or is affected by other confounders); or (c) involved in an interaction with another variable. All of these factors will impact precise assessment of the biomarker's relationship to pertinent outcomes.
If a biomarker is a true risk factor, it is present within the causal pathway (s) leading to disease. More specifically, it is correlated with the disease statistically, although it is not always linked causally (e.g., the APOE-ε4 allele is considered a risk factor for Alzheimer's disease, but many patients without this allele develop Alzheimer's disease). However, if the biomarker's measurement is affected by one or more confounding variables-and if these confounding variables are not controlled-the biomarker's actual relationship to the disease outcome is “muddied” by those other sources of bias (e.g. age and/or exercise habits may confound accurate measurement of HDL-C in determining ischemic stroke risk). On the other hand, a biomarker could be part of an interaction effect, or effect modification profile, meaning its impact on the disease outcome depends on the presence or absence of another factor (e.g. older patients might have a different biomarker profile than younger patients as it relates to their disease expression). In the latter case, it is essential to detect and estimate this interaction effect, rather than control for it, since the interaction represents a real phenomenon and not simply “background noise”.[11,12] Statistical regression techniques (e.g. multivariate linear and logistic models) are commonly used to determine the degree to which biomarkers represent true risk factors after adjusting for confounding variable effects and accounting for any interaction or effect modification relationships.[11,13]
When investigating novel biomarkers in particular, the randomized controlled trial remains the “gold standard” for research design, although retrospective designs are still useful in identifying biomarker candidates. In the case of prognostic biomarkers, a relationship between either the biomarker's baseline value, or biomarker temporal variability, and the outcome of interest must be demonstrated. This relationship must be established apart from any treatment effects. For predictive biomarkers, the values at baseline and/or changes over time must demonstrate their ability to predict the effectiveness of treatment or safety based on a predefined outcome of interest. For both prognostic and predictive biomarkers, repeated studies in diverse clinical situations should replicate original findings in order to conclude the validity of the biomarker in question.[13]
Another scientific approach is the biomarker by treatment interaction design, whereby biomarker classification is used as a stratification variable (that is, dividing a sample into subgroups based on biomarker status) in order to substantiate the effect of treatment. Patients in each biomarker subgroup are then randomly assigned to treatment groups.[13] The biomarker-strategy design is intended to assess a biomarker's clinical value. As described by Gosho, et al., “First, all patients are randomly assigned to an experimental arm (‘biomarker-based strategy’ arm) that uses the biomarker to determine treatment, or to a control arm (‘non-biomarker-based strategy’ arm) that does not. Next, if the patients allocated to the biomarker-based strategy arm are diagnosed as biomarker positive, they are allowed to proceed to the test treatment. On the other hand, if the patients allocated to the biomarker-based strategy arm are biomarker negative, they then proceed to the standard treatment”.[13] Other design types include: (a) enrichment design; (b) adaptive signature design; (c) biomarker-adaptive threshold design; (d) adaptive accrual design; and (e) Bayesian adaptive design.[13] Details of these methodologies are beyond the scope of the current discussion. Thus the reader is encouraged to consult the sources referenced above for further information.
POINT-OF-CARE TESTING
Historically, health care was literally delivered in a POC fashion, with the practitioner tending for the sick directly at the bedside by providing house visits.[14] During the 20th Century, gradual centralization of medical facilities occurred around the globe, with increasingly large medical institutions and networks providing centralized care and diagnostic services. It was not until recently that technological developments including the introduction of highly specialized, portable, miniaturized diagnostic equipment created a new opportunity for the shift away from large-scale, centralized facilities back to the patient's bedside. Benefits of modern POC testing are many, the most prominent of which include: (a) the ability to shift toward early detection and prevention of disease; (b) the capacity to provide immediate diagnostic results and eliminate unnecessary delays; (c) potential to reduce health care costs; and (d) provide much needed diagnostic services where no services were previously available (that is, rural areas, regions with limited resources and/or access).[14,15]
There are several general types of POC testing devices. The simplest classification includes the degree to which the equipment is mobile, beginning with bench-top (semi-moveable units such as thromboelastography analyzers)[16,17] devices, proceeding through portable devices (wheeled platform-based ultrasound),[18] to purely hand-held devices (smart phone-sized ultrasound units, rapid pregnancy tests, or pupillary assessment devices).[19,20] Of course, with one defined set of benefits come certain disadvantages. More specifically, controversy continues regarding the accuracy and reliability of POC devices.[21,22,23] Another potential drawback is the need for standardized staff training, device calibration, standardization of results, and routine equipment maintenance.[24,25,26] It is likely that with the emergence of new, improved devices some of these concerns may be alleviated. However, it is unlikely that completely “error-proof,” POC diagnostic devices will emerge any time soon.
In the subsequent sections, we will discuss selected clinical areas where biomarker research resulted in the most tangible benefits to the patient. It is important to note that neither the list of biomarkers listed below, nor the examples of research programs (or disciplines) provided are meant to be comprehensive. Such an undertaking alone would require an entire textbook. Rather, we chose to focus on concrete steps taken by biomarker investigators in order to successfully implement collaborative research programs capable of initiating and conducting large-scale, clinically relevant biomarker discovery efforts.
CARDIOLOGY AND CARDIOVASCULAR DISEASES
In view of Professor Poste's comments outlined in the introductory paragraphs of this manuscript,[6] the question of not only the need for better technologies in regard to acquisition of clinically usable, reliable biomarkers, but also of the political will to follow through in such undertaking must be asked. This can be answered in the affirmative regarding cardiac biomarkers. In 2013, the Global Cardiovascular Disease Taskforce released a scientific statement titled Moving from political declaration to action in reducing the global burden of cardiovascular diseases.[27] In this document the GCDT, comprised of the World Heart Federation, American Heart Association, American College of Cardiology Foundation, European Heart Network and the European Society of Cardiology (including representation from the World's emerging economies) assessed and defined metrics that needed to be met by 2025. This included the ambitious plan to reduce the mortality of premature non-communicable disease by 25% by 2025 (the “25-by-25” plan).
Addona et al.,[28] performed novel work inspired by the fact that very few protein biomarkers identified using proteomics had been introduced clinically.[28] They contended that there was no organized strategy to transition candidate biomarkers from the discovery phase to clinical validation. Therefore, they developed a “pipeline” to integrate proteomic technologies used for discovery through the verification stages of plasma biomarker identification. Their experimental model utilizes proteomics/liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS) paradigm wherein biological samples are obtained from patients undergoing planned treatment for hypertrophic cardiomyopathy. Actual sampling occurs before, during, and after a controlled myocardial infarction, thus ensuring a “target-rich” environment and allowing participating patients to serve as “internal controls” without introducing risks beyond those of the planned therapy.[28] Addona et al., identified 121 highly expressed proteins and over 100 new candidate proteins. These newly discovered candidates were then qualified by peripheral blood screening from the femoral vein (using accurate inclusion mass screening, or AIMS) and verified by stable isotope dilution and multiple reaction monitoring.[28] This, in fact, was a proof-of-concept for the creation of a coherent sampling, discovery, qualification, and verification “assembly line” for potential biomarkers. The above design exemplifies the synergies created when political will, practical technological methodology, and team determination are simultaneously present.
Bone marrow-derived endothelial progenitor cells (EPCs) are robust indicators (high counts may herald pathologic change) of cardiovascular disease (CVD) and may represent a novel new biomarker for CVD and even serve as a mode of therapy.[29] MicroRNAs (miRNA) are short segments of RNA that are posttranscriptional regulators of gene expression and are not translated into proteins; they have been associated with CVD.[30] MiRNAs are stable in the circulation and lipoproteins may act as carriers, or transporters. Current evidence relating miRNA to CVD follows a logical path[31]: (a) Type II diabetes has the most dramatic impact on circulating miRNAs[32]; (b) An miRNA signature of only three miRNAs (miR-126, miR-223, and miR-197) was implicated in the Framingham study[33]; (c) adverse outcomes and these three miRNAs were associated[33]; and (d) miR-126, miR-223, and miR-197 were associated with miR-21 and miR-24, which as a cluster, were highly expressed on platelets.[33]
In patients with advanced heart failure, growth-differentiation factor 15, high-sensitivity C-reactive protein (CRP), and high sensitivity troponin-T, all from the N-terminal portion of the natriuretic peptide (NT-proBNP) have been implicated in predicting long-term mortality. Growth-differentiation factor 15 was an even stronger marker than NT-proBNP. Other novel biomarkers have been discovered for new-onset cardiovascular disease, cardiovascular stress, and ventricular hypertrophy.[34,35] However, their clinical utility is limited because the lack of credentialing and validation, as mentioned above. In another example, a new generation of cardiac Troponin assays may improve the identification of non-ST-segment elevation acute coronary syndrome (NSTE-ACS).[36] O’Malley et al. have recently reported on the importance of copeptin, midregional proadrenomedullin (MR-proADM), and midregional proatrial natriuretic peptide (MR-proANP) in a large study of patients with moderate to high risk for NSTE-ACS.[37] All three biomarkers were associated with death or heart failure at 12 months. Adding these three biomarkers to clinical symptomatology and other previously known biomarkers increased the ability to perform more accurate predictive modeling.
Additionally, the association of biomarkers with ethnicity was demonstrated recently.[38] Specific associations between C-reactive protein, fibrinogen, interleukin-6, D-dimer and plasmin-antiplasmin complex in a number of different populations have been made with cardiovascular events.[38] The need for demographic-based risk stratification in relation to new biomarkers was emphasized. Also, the question regarding a role for novel biomarkers in cardiovascular risk prediction for women arises.[39] As previously mentioned, an organized “pipeline,” that also involves industry, must be put into place to credential and validate novel biomarkers in large prospective, randomized trials.
INFECTIOUS DISEASES AND SEPSIS
Traditional biomarkers in sepsis include a variety of microbiologic, laboratory, and clinical tools. However, these tend to be unreliable, can be readily biased by concurrent antibiotic use and other confounders, and may be expensive. Erythrocyte sedimentation rate (ESR) and (CRP) were popular in the 1980s and 1990s, but have fallen into disfavor due to their low specificity for both sepsis and infection in general.[40,41,42,43,44,45] Additional potential biomarkers in the setting of sepsis include the so-called pancreatic stone protein,[46,47] protein C,[48,49] and urinary L-type fatty acid-binding protein.[50] Currently, there are over 100 biomarker candidates for sepsis, with the ongoing amount of scientific work reaching unprecedented new levels.
In the setting of sepsis or septic shock, detection of causative organism or pathogen-related markers in combination with clinical signs and symptoms remain the mainstay of diagnosis. However, there is increasing interest in host biomarkers for early diagnosis, identification of latent infections, monitoring of disease progression, and assessing response to treatment. Procalcitonin (PCT) has been used as biomarker for respiratory tract infections, to distinguish between bacterial and viral etiologies, and to guide therapy.[51] Plasmodial lactate dehydrogenase and histidine-rich protein II are biomarkers that show promise in rapid reliable diagnosis of malaria.[52] Interleukin-2 appears to be a useful biomarker for identifying latent tuberculosis.[53] In patients suffering from invasive candidiasis (1, 3)-β-D-Glucan may be a prognostic marker of treatment response.[54]
Although biomarker analysis has gained considerable attention for infection-induced changes in human hosts, many of these markers may not be specific for individual disease. These markers may involve non-specific host responses to a variety of infections, and numerous biomarkers thought to have an association with individual infections are awaiting validation as diagnostic or prognostic tools.[55]
ACUTE KIDNEY INJURY
Acute kidney injury (AKI) is a complex physiological and biochemical messaging process that that involves many “signals” that are essentially biological markers. These biomarkers are invaluable in caring for critically ill patients because they provide clinicians with an armamentarium to diagnose, treat, and prognosticate. Technologies that provide “early warning” of AKI may allow accurate diagnostic and effective therapeutic planning in regards to the prevention or amelioration of this pathologic state. Accurate AKI biomarkers may also have positive social, political, and economic implications. This is because AKI is a very costly hospital complication associated with increased lengths of stay, prolonged intensive care unit (ICU) stays, invasive hemodynamic monitoring, renal replacement therapy, readmission, and/or mortality.[56,57] Moreover, patients with AKI are at risk for chronic kidney disease and end-stage renal disease. Traditionally urine output, serial serum creatinine measurements, blood urea nitrogen, and urinalysis are followed when there is concern for AKI. However, renal failure is a gradual process, and can be assessed by using criteria such as those of the Acute Kidney Injury Network (AKIN); the Risk, Injury, Failure, End-Stage Kidney Disease (RIFLE), and Kidney Disease Improving Global Outcomes (KDIGO).[58]
All injured biological organs produce quantifiable proteins, and the kidney is no different.[59] Renal damage can occur with sepsis, prolonged ischemia, shock, and toxic agents (e.g. aminoglycosides). McCullough et al., reported that biomarkers are produced by renal tubular cells because filtered proteins are not reabsorbed (proximal tubules) and become measurable, or by upregulation by messenger RNA and synthesis of proteins.[56,60] Biomarkers signaling impending AKI (within 24–48 hours) include tubular cell-cycle arrest markers (insulin-like growth factor-binding protein 7 [IGFBP7]) and metalloproteinases-2 (TIMP-2) tissue inhibitor.[61] Fulminant AKI is suggested by steep increases in neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule-1 (KIM-1), L-type fatty acid-binding protein (L-FABP), α-glutathione S-transferase (α-GST), π-GST and interleukin-18. Of interest, these biomarkers may become elevated before the serum creatinine,[62] and even in the absence of elevated serum creatinine.[63] Particularly in regard to sepsis-related AKI, IL-18, NGAL, and KIM-1 are strongly associated.[64]
OBSTETRICS AND GYNECOLOGY
As a discipline, obstetrics is one of the early adopters of widespread POC testing. One of the best examples of successful translation of biomarker research into clinical practice is the introduction of the rapid urine test for beta-human chorionic gonadotropin (β-hCG) in pregnancy testing.[65] In addition to providing qualitative information regarding pregnancy status, β-hCG levels also change during the pregnancy,[66] thus allowing for quantitative assessment into the expected versus observed progression of the pregnancy. Without a significant research effort in the 1970s and the 1980s, this simple test taken for granted by many would not have been possible today.[67]
Another topic of active biomarker research in obstetrics is the area of amniotic fluid embolism (AFE).[68] This devastating pathophysiologic entity continues to be a diagnosis of exclusion, with sepsis, pulmonary embolism, and other acute cardio-pulmonary disorders competing for the bedside clinician's attention.[69] Development of a sensitive and specific biomarker for AFE may provide an opportunity not only for early diagnosis, but much more importantly for earlier and more effective clinical intervention.[68]
Ovarian and uterine cancer are among the most feared gynecologic malignancies. When detected and treated early, their mortality is relatively low. Yet, ovarian cancer is known for its ability to elude early diagnosis, with significant proportion of patients presenting in advanced disease stages.[70] Among potential biomarkers of ovarian cancer, inherited gene mutations, epigenetic changes, gene expression, metabolomics and microRNA detection all may play a role in developing an inexpensive, reliable, and widely available POC test.[70]
Cervical cancer accounts for a significant proportion of potentially preventable cancer deaths in the female population, especially in areas where routine screening programs are not readily available.[71,72,73] Active biomarker research in this area focuses on the human papilloma virus (HPV) oncogenes.[74] Among promising biomarkers for cervical cancer are: (a) p16(INK4a)/Ki-67 dual-stain cytology; (b) promoter region methylation of the cell adhesion molecule 1 (CADM1) gene; (c) repression of the T-lymphocyte maturation associated protein (MAL) gene by promoter methylation; and (d) viral integration.[75,76,77,78,79] Despite encouraging early results, it is not known how accurately these biomarkers will help predict and/or modify patient outcomes.[75]
ONCOLOGY
Cancer caused over 8 million deaths in 2012 and over 14 million new cases were diagnosed.[80] Most deaths are due to the lack of early diagnosis and detection. Consequently, improved ability to classify and assess cancer-specific biomarkers represents an active area of opportunity for improvement.[81,82] Biological markers are indicators of pathologic processes, normal processes, or even responses to pharmaceutical therapies.[83] Prognostic and predictive oncologic biomarkers offer immense potential for future development of patient-centered, personalized therapies.[84] Prognostic biomarkers predict outcome (survival or tumor reduction) and involve individual traits or characteristics that independently predict such outcome regardless of treatment. Predictive biomarkers foretell a patient's response to treatment. Patient cohort outcomes are needed for prognostication and involve the documentation of similar treatments and of adequate follow-ups.[84] Phase II or III clinical trials are required, with storage of patient samples that can be reviewed and retrieved at some point in the future, to validate and confirm treatment responses and/or benefits.[84] Oncologic biomarkers must demonstrate a definite clinical utility, and require the requisite credentialing and validation. In cancer therapy there have been few well-designed prospective trials for biomarker validation and robust evidence-based associations are still lacking.
Examples of where important biomarker development work is produced and catalogued will now follow. Drake and Kislinger have delved into signaling pathways of prostate cancer through work on exosomes secreted by the prostate, urine, seminal fluid, and blood.[85] Cremona et al., have attacked clear cell renal carcinoma through characterization of cell signaling into either cycle and proliferation, or cell death and survival.[86] Gasparini et al., reported that four miRNAs (miR-155, miR-493, mirR-30e, and miR-27a) form a novel diagnostic and prognostic pattern in Triple Negative Breast Cancers.[87] Others have reviewed candidate biomarkers for cervical cancer treatment in regard to the neoplasm's sensitivity to anticancer agents, prediction of radiosensitivity, presence in the peripheral blood, and prognostic utility.[88] Furthermore, “molecular imaging” (e.g. PET imaging of estrogen receptor expression) can be used in prediction of cancer diagnosis, therapy, and outcome.[89]
Biomarkers in cancer treatment and prognostication suffer from shortcomings similar to those of biomarkers in other clinical fields, including lack of evidence-based therapy, lack of industry involvement, lack of “pipeline” credentialing and validation (including liquid chromatography, mass spectrometry, multiple reaction monitoring, and accurate inclusion mass screening).
TRAUMA AND CRITICAL CARE
A number of potential biomarkers have been explored in the general area of critical illness, trauma and burn injury. Among the most commonly used, but at the same time more “crude” biomarkers are anion gap, base deficit and the urine output.[90,91,92] Other biomarker candidates in the setting of trauma are heat shock proteins,[93] cytokines,[94] fibrin degradation products,[95] and matrix metalloproteinases.[96]
More recently, new biomarker discoveries emerged in the area of traumatic brain injury (TBI). Sodjin et al., studied cerebral spinal fluid to look for candidate biomarkers using hexapeptide ligand libraries (HLL) and identified neuron specific enolase, glial fibrillary acidic protein, myelin basic protein, creatine kinase B-type and S-100β as potential biomarker candidates.[97] Their findings support the use of HLL as a “biomarker screening tool”. Neselius et al., have studied Olympic boxers and found that levels of T-tau, neurofilament light protein (NFL), glial fibrillary acidic protein (GFAP), and S-100β were increased in 80% of the boxers indicating that repetitive brain trauma may induce changes in potential CSF biomarkers and help diagnose central nervous system injury. The lack of normalization of NFL and GFAP after resting in subgroup of boxers may be an indication of ongoing, more chronic degenerative injury.[98] Svetlov et al., presented a strategy to study molecular signatures of blast injury-related neurotrauma and to develop a pathway/network map for novel biomarker discovery.[99] They postulate that such a biomarker discovery pathway/network may be effective for triaging and managing both combat and civilian causalities.
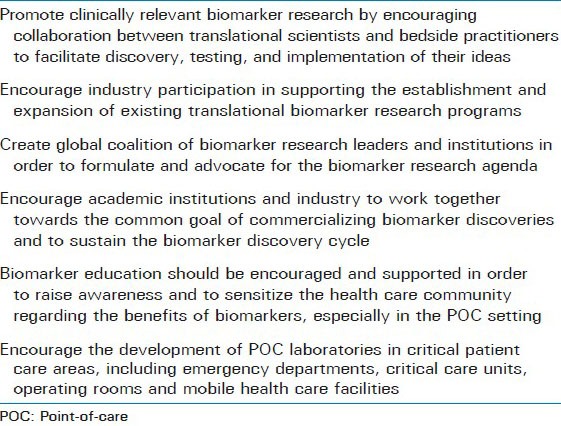
Genet et al. looked at biomarkers related to coagulopathy and endothelial damage in TBI versus non-TBI patients.[100] Other examples of biomarker research in trauma and critical care include the work of Rayner et al.,[101] in identifying biomarkers (urinary and transfusion-related) of systemic oxidative injury and activation of platelets in trauma, and that of Teng et al.,[96] in examining matrix metalloproteinase-9 (MP-9) as a new biomarker of multi-organ system failure in trauma and infection. Despite continued progress, a reliable biomarker for universal use in critical illness and injury has not yet been identified. A list of strategic elements required for the creation and maintenance of a sustainable network for biomarker discovery is presented in Table 1.
Table 1.
Building a sustainable network for biomarker discovery and research: Key strategic goals
CONCLUSIONS
There is an urgency to better organize and formalize the framework for biomarker validation and qualification. The only real solution is a global collaborative effort involving industry, academia and national/trans-national regulatory agencies. Necessary for successful implementation of such global biomarker evaluation and validation is the standardization and harmonization of biomarker and surrogate end point definitions and approval criteria. Regulatory agencies, in addition to ensuring compliance should expand their guidance to both industry and academia so that the evolution of the biomarker evaluation system can be guided towards greater transparency, more collaborative culture, and synergistic utilization of existing resources. Although the path to scientific and regulatory approval for new biomarkers seems convoluted, the benefits of accurate disease identification and prediction far outweigh the risks (and monetary investments) involved in completing the lengthy process of research, development, and its implementation. Most importantly, all new discoveries should be geared toward simplified implementation, rapid deployment, wide accessibility, and patient-centered POC application.
Footnotes
Source of Support: Nil
Conflict of Interest: No.
REFERENCES
- 1.Vasan RS. Biomarkers of cardiovascular disease: Molecular basis and practical considerations. Circulation. 2006;113:2335–62. doi: 10.1161/CIRCULATIONAHA.104.482570. [DOI] [PubMed] [Google Scholar]
- 2.Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 3.Fuentes-Arderiu X. What is a biomarker? It's time for a renewed definition. Clin Chem Lab Med. 2013;51:1689–90. doi: 10.1515/cclm-2013-0240. [DOI] [PubMed] [Google Scholar]
- 4.Shaw A. Emerging biomarkers of acute kidney injury. [Last accessed date on 2014 Jul 09]. Available from: https://scahq.org/sca3/events/2012/annual/syllabus/submissions/tue/Emerging%20Biomarkers%20for%20Periop%20Acute%20Kidney%20Injury%20-%20Shaw.pdf .
- 5.He P. Identifying cut points for biomarker defined subset effects in clinical trials with survival endpoints. Contemp Clin Trials. 2014;38:333–7. doi: 10.1016/j.cct.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Poste G. Bring on the biomarkers. Nature. 2011;469:156–7. doi: 10.1038/469156a. [DOI] [PubMed] [Google Scholar]
- 7.Poehling KA, Zhu Y, Tang YW, Edwards K. Accuracy and impact of a point-of-care rapid influenza test in young children with respiratory illnesses. Arch Pediatr Adolesc Med. 2006;160:713–8. doi: 10.1001/archpedi.160.7.713. [DOI] [PubMed] [Google Scholar]
- 8.Grossman HB, Messing E, Soloway M, Tomera K, Katz G, Berger Y, et al. Detection of bladder cancer using a point-of-care proteomic assay. JAMA. 2005;293:810–6. doi: 10.1001/jama.293.7.810. [DOI] [PubMed] [Google Scholar]
- 9.Singer AJ, Ardise J, Gulla J, Cangro J. Point-of-care testing reduces length of stay in emergency department chest pain patients. Ann Emerg Med. 2005;45:587–91. doi: 10.1016/j.annemergmed.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 10.Sackett DL, Straus S.E, Richardson W.S, Rosenberg W, Haynes R.B. London: Churchill Livingstone; 2000. Evidence-based medicine: How to teach and practice. [Google Scholar]
- 11.Hosmer DW, Lemeshow S. Wiley series in probability and statistics. Texts and references section. 2nd ed. xii. New York: Wiley; 2000. Applied logistic regression; p. 373. [Google Scholar]
- 12.Mayeux R. Biomarkers: Potential uses and limitations. NeuroRx. 2004;1:182–8. doi: 10.1602/neurorx.1.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gosho M, Nagashima K, Sato Y. Study designs and statistical analyses for biomarker research. Sensors (Basel) 2012;12:8966–86. doi: 10.3390/s120708966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NIH. Point-of-care diagnostic testing. [Last accessed date on 2014 Jul 20]. Available from: http://report.nih.gov/nihfactsheets/ViewFactSheet.aspx?csid=112 .
- 15.Stawicki SP, Howard JM, Pryor JP, Bahner DP, Whitmill ML, Dean AJ. Portable ultrasonography in mass casualty incidents: The CAVEAT examination. World J Orthop. 2010;1:10–9. doi: 10.5312/wjo.v1.i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Price CP. Point of care testing. BMJ. 2001;322:1285–8. doi: 10.1136/bmj.322.7297.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stammers AH, Bruda NL, Gonano C, Hartmann T. Point-of-care coagulation monitoring: Applications of the thromboelastography. Anaesthesia. 1998;53(Suppl 2):58–9. doi: 10.1111/j.1365-2044.1998.tb15159.x. [DOI] [PubMed] [Google Scholar]
- 18.Behnia M, Powell S, Fallen L, Tamaddon H, Behnia M. Correlation of Stroke Volume Measurement between Sonosite Portable Echocardiogram and Edwards Flotrac Sensor-Vigileo Monitor in an Intensive Care Unit. Clin Med Insights Circ Respir Pulm Med. 2013;7:45–51. doi: 10.4137/CCRPM.S12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bercich R, Bernhard J, Larson K, Lindsey J. Hand-held plasma isolation device for point-of-care testing. IEEE Trans Biomed Eng. 2011;58:759–62. doi: 10.1109/TBME.2010.2095419. [DOI] [PubMed] [Google Scholar]
- 20.Gault MH, Harding CE, Duffett S, Longerich L. i-STAT hand-held point-of-care analyzer for dialysis units. Nephron. 1998;80:344–8. doi: 10.1159/000045196. [DOI] [PubMed] [Google Scholar]
- 21.Martinez Lomakin F, Tobar C. Accuracy of point-of-care serum creatinine devices for detecting patients at risk of contrast-induced nephropathy: A critical overview. Crit Rev Clin Lab Sci. 2014:1–12. doi: 10.3109/10408363.2014.937794. [DOI] [PubMed] [Google Scholar]
- 22.Sobieraj-Teague M, Daniel D, Farrelly B, Coghlan D, Gallus A. Accuracy and clinical usefulness of the CoaguChek S and XS Point of Care devices when starting warfarin in a hospital outreach setting. Thromb Res. 2009;123:909–13. doi: 10.1016/j.thromres.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 23.Wood WG. Problems with the external quality assessment of accuracy of point of care devices (POCD) for blood glucose are independent of sample composition. Clin Lab. 2006;52:345–51. [PubMed] [Google Scholar]
- 24.Buchegger P, Sauer U, Toth-Székély H, Preininger C. Miniaturized protein microarray with internal calibration as point-of-care device for diagnosis of neonatal sepsis. Sensors (Basel) 2012;12:1494–508. doi: 10.3390/s120201494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shermock KM, Clarke W, Streiff MB. A superior method to report clinically relevant quality information about the point-of-care INR device performance compared with the International Organization for Standardization guidelines. Clin Chim Acta. 2010;411:1756–60. doi: 10.1016/j.cca.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 26.Campbell S, Howanitz PJ. Resident training in point-of-care testing. Clin Lab Med. 2007;27:397–410. doi: 10.1016/j.cll.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Smith SC, Jr, Chen D, Collins A, Harold JG, Jessup M, Josephson S, et al. Moving from political declaration to action on reducing the global burden of cardiovascular diseases: A statement from the Global Cardiovascular Disease Taskforce. J Am Coll Cardiol. 2013;62:2151–3. doi: 10.1016/j.jacc.2013.08.722. [DOI] [PubMed] [Google Scholar]
- 28.Addona TA, Shi X, Keshishian H, Mani DR, Burgess M, Gillette MA, et al. A pipeline that integrates the discovery and verification of plasma protein biomarkers reveals candidate markers for cardiovascular disease. Nat Biotechnol. 2011;29:635–43. doi: 10.1038/nbt.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sen S, McDonald SP, Coates PT, Bonder CS. Endothelial progenitor cells: Novel biomarker and promising cell therapy for cardiovascular disease. Clin Sci (Lond) 2011;120:263–83. doi: 10.1042/CS20100429. [DOI] [PubMed] [Google Scholar]
- 30.Mayr M, Zampetaki A, Willeit P, Willeit J, Kiechl S. MicroRNAs within the continuum of postgenomics biomarker discovery. Arterioscler Thromb Vasc Biol. 2013;33:206–14. doi: 10.1161/ATVBAHA.112.300141. [DOI] [PubMed] [Google Scholar]
- 31.Engelhardt S. Small RNA biomarkers come of age. J Am Coll Cardiol. 2012;60:300–3. doi: 10.1016/j.jacc.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 32.Zampetaki A, Kiechl S, Drozdov I, Willeit P, Mayr U, Prokopi M, et al. Plasma microRNA profiling reveals loss of endothelial miR-126 and other microRNAs in type 2 diabetes. Circ Res. 2010;107:810–7. doi: 10.1161/CIRCRESAHA.110.226357. [DOI] [PubMed] [Google Scholar]
- 33.Zampetaki A, Willeit P, Tilling L, Drozdov I, Prokopi M, Renard JM, et al. Prospective study on circulating MicroRNAs and risk of myocardial infarction. J Am Coll Cardiol. 2012;60:290–9. doi: 10.1016/j.jacc.2012.03.056. [DOI] [PubMed] [Google Scholar]
- 34.Yin X, Subramanian S, Hwang SJ, O’Donnell CJ, Fox CS, Courchesne P, et al. Protein biomarkers of new-onset cardiovascular disease: Prospective study from the systems approach to biomarker research in cardiovascular disease initiative. Arterioscler Thromb Vasc Biol. 2014;34:939–45. doi: 10.1161/ATVBAHA.113.302918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xanthakis V, Larson MG, Wollert KC, Aragam J, Cheng S, Ho J, et al. Association of novel biomarkers of cardiovascular stress with left ventricular hypertrophy and dysfunction: Implications for screening. J Am Heart Assoc. 2013;2:e000399. doi: 10.1161/JAHA.113.000399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Filippatos G, Farmakis D, Parissis J. Novel biomarkers in acute coronary syndromes: New molecules, new concepts, but what about new treatment strategies? J Am Coll Cardiol. 2014;63:1654–6. doi: 10.1016/j.jacc.2013.11.055. [DOI] [PubMed] [Google Scholar]
- 37.O’Malley RG, Bonaca MP, Scirica BM, Murphy SA, Jarolim P, Sabatine MS, et al. Prognostic performance of multiple biomarkers in patients with non-ST-segment elevation acute coronary syndrome: Analysis from the MERLIN-TIMI 36 trial (Metabolic Efficiency With Ranolazine for Less Ischemia in Non-ST-Elevation Acute Coronary Syndromes-Thrombolysis In Myocardial Infarction 36) J Am Coll Cardiol. 2014;63:1644–53. doi: 10.1016/j.jacc.2013.12.034. [DOI] [PubMed] [Google Scholar]
- 38.Veeranna V, Zalawadiya SK, Niraj A, Kumar A, Ference B, Afonso L. Association of novel biomarkers with future cardiovascular events is influenced by ethnicity: Results from a multi-ethnic cohort. Int J Cardiol. 2013;166:487–93. doi: 10.1016/j.ijcard.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 39.Paynter NP, Everett BM, Cook NR. Cardiovascular disease risk prediction in women: Is there a role for novel biomarkers? Clin Chem. 2014;60:88–97. doi: 10.1373/clinchem.2013.202796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vyas PK, Patel MP, Sheth KR, Shah RC. C-reactive protein in early diagnosis of neonatal sepsis. J Indian Med Assoc. 1985;83:408–10. [PubMed] [Google Scholar]
- 41.Schentag JJ, O’Keeffe D, Marmion M, Wels PB. C-reactive protein as an indicator of infection relapse in patients with abdominal sepsis. Arch Surg. 1984;119:300–4. doi: 10.1001/archsurg.1984.01390150040010. [DOI] [PubMed] [Google Scholar]
- 42.Jeon JH, Namgung R, Park MS, Park KI, Lee C. Positive maternal C-reactive protein predicts neonatal sepsis. Yonsei Med J. 2014;55:113–7. doi: 10.3349/ymj.2014.55.1.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang HE, Shapiro NI, Safford MM, Griffin R, Judd S, Rodgers JB, et al. High-sensitivity C-reactive protein and risk of sepsis. PLoS One. 2013;8:e69232. doi: 10.1371/journal.pone.0069232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walliullah SM, Islam MN, Siddika M, Hossain MA, Chowdhury AK. Role of micro-ESR and I/T ratio in the early diagnosis of neonatal sepsis. Mymensingh Med J. 2009;18:56–61. [PubMed] [Google Scholar]
- 45.Trevisanuto D, Dani C, Chiodin E, Cantarutti F, Zanardo V. The micro-ESR with the capillary tube inclined to 45 degrees in the “sepsis screen” of neonatal infection due to beta-hemolytic B-group Streptococcus. Pediatr Med Chir. 1992;14:507–8. [PubMed] [Google Scholar]
- 46.Que YA, Delodder F, Guessous I, Graf R, Bain M, Calandra T, et al. Pancreatic stone protein as an early biomarker predicting mortality in a prospective cohort of patients with sepsis requiring ICU management. Crit Care. 2012;16:R114. doi: 10.1186/cc11406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jiří Ž, Kýr M, Vavřina M, Fedora M. Pancreatic stone protein-a possible biomarker of multiorgan failure and mortality in children sepsis. Cytokine. 2014;66:106–11. doi: 10.1016/j.cyto.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 48.Gutovitz S, Papa L, Jimenez E, Falk J, Wieman L, Sawyer S, et al. Protein C as an early biomarker to distinguish pneumonia from sepsis. J Crit Care. 2011;26:330e9–12. doi: 10.1016/j.jcrc.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 49.Shorr AF, Nelson DR, Wyncoll DL, Reinhart K, Brunkhorst F, Vail GM, et al. Protein C: A potential biomarker in severe sepsis and a possible tool for monitoring treatment with drotrecogin alfa (activated) Crit Care. 2008;12:R45. doi: 10.1186/cc6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doi K1, Noiri E, Maeda-Mamiya R, Ishii T, Negishi K, Hamasaki Y, et al. Urinary L-type fatty acid-binding protein as a new biomarker of sepsis complicated with acute kidney injury. Crit Care Med. 2010;38:2037–42. doi: 10.1097/CCM.0b013e3181eedac0. [DOI] [PubMed] [Google Scholar]
- 51.Gilbert DN. Procalcitonin as a biomarker in respiratory tract infection. Clin Infect Dis. 2011;52(Suppl 4):S346–50. doi: 10.1093/cid/cir050. [DOI] [PubMed] [Google Scholar]
- 52.Jain P, Chakma B, Patra S, Goswami P. Potential biomarkers and their applications for rapid and reliable detection of malaria. Biomed Res Int 2014. 2014:852645. doi: 10.1155/2014/852645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mamishi S, Pourakbari B, Teymuri M, Rubbo PA, Tuaillon E, Keshtkar AA, et al. Diagnostic accuracy of IL-2 for the diagnosis of latent tuberculosis: A systematic review and meta-analysis. Eur J Clin Microbiol Infect Dis. 2014 doi: 10.1007/s10096-014-2190-z. [DOI] [PubMed] [Google Scholar]
- 54.Jaijakul S, Vazquez JA, Swanson RN, Ostrosky-Zeichner L. (1,3)-beta-D-glucan as a prognostic marker of treatment response in invasive candidiasis. Clin Infect Dis. 2012;55:521–6. doi: 10.1093/cid/cis456. [DOI] [PubMed] [Google Scholar]
- 55.Ray S, Patel SK, Kumar V, Damahe J, Srivastava S. Differential expression of serum/plasma proteins in various infectious diseases: Specific or nonspecific signatures. Proteomics Clin Appl. 2014;8:53–72. doi: 10.1002/prca.201300074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McCullough PA, Bouchard J, Waikar SS, Siew ED, Endre ZH, Goldstein SL, et al. Implementation of novel biomarkers in the diagnosis, prognosis, and management of acute kidney injury: Executive summary from the tenth consensus conference of the Acute Dialysis Quality Initiative (ADQI) Contrib Nephrol. 2013;182:5–12. doi: 10.1159/000349962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stawicki SP, Gracias VH, Lorenzo M. Surgical critical care: From old boundaries to new frontiers. Scand J Surg. 2007;96:17–25. doi: 10.1177/145749690709600104. [DOI] [PubMed] [Google Scholar]
- 58.KDIGO. Clinical practice guidline for acute kidney injury. Kidney Int Suppl. 2012;2:1–138. [Google Scholar]
- 59.Boudonck KJ, Rose DJ, Karoly ED, Lee DP, Lawton KA, Lapinskas PJ. Metabolomics for early detection of drug-induced kidney injury: Review of the current status. Bioanalysis. 2009;1:1645–63. doi: 10.4155/bio.09.142. [DOI] [PubMed] [Google Scholar]
- 60.McCullough PA, Shaw AD, Haase M, Bouchard J, Waikar SS, Siew ED, et al. Diagnosis of acute kidney injury using functional and injury biomarkers: Workgroup statements from the tenth Acute Dialysis Quality Initiative Consensus Conference. Contrib Nephrol. 2013;182:13–29. doi: 10.1159/000349963. [DOI] [PubMed] [Google Scholar]
- 61.Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25. doi: 10.1186/cc12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Doi K, Negishi K, Ishizu T, Katagiri D, Fujita T, Matsubara T, et al. Evaluation of new acute kidney injury biomarkers in a mixed intensive care unit. Crit Care Med. 2011;39:2464–9. doi: 10.1097/CCM.0b013e318225761a. [DOI] [PubMed] [Google Scholar]
- 63.Prowle JR, Liu YL, Licari E, Bagshaw SM, Egi M, Haase M, et al. Oliguria as predictive biomarker of acute kidney injury in critically ill patients. Crit Care. 2011;15:R172. doi: 10.1186/cc10318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Srisawat N, Kellum JA. Acute kidney injury: Definition, epidemiology, and outcome. Curr Opin Crit Care. 2011;17:548–55. doi: 10.1097/MCC.0b013e32834cd349. [DOI] [PubMed] [Google Scholar]
- 65.Canfield RE, O’Connor JF, Birken S, Krichevsky A, Wilcox AJ. Development of an assay for a biomarker of pregnancy and early fetal loss. Environ Health Perspect. 1987;74:57–66. doi: 10.1289/ehp.877457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Braunstein GD, Rasor J, Danzer H, Adler D, Wade ME. Serum human chorionic gonadotropin levels throughout normal pregnancy. Am J Obstet Gynecol. 1976;126:678–81. doi: 10.1016/0002-9378(76)90518-4. [DOI] [PubMed] [Google Scholar]
- 67.VMC. Pregnancy test. [Last accessed date on 2014 Jul 21]. Available from: http://www.myvmc.com/investigations/pregnancy-test/#c7 .
- 68.Stawicki SP, Papadimos TJ. Challenges in managing amniotic fluid Embolism: An up-to-date perspective on diagnostic testing with focus on novel biomarkers and avenues for future research. Curr Pharm Biotechnol. 2014;14:1168–78. doi: 10.2174/1389201015666140430163921. [DOI] [PubMed] [Google Scholar]
- 69.Thongrong C, Kasemsiri P, Hofmann JP, Bergese SD, Papadimos TJ, Gracias VH, et al. Amniotic fluid embolism. Int J Crit Illn Inj Sci. 2013;3:51–7. doi: 10.4103/2229-5151.109422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang B, Cai FF, Zhong XY. An overview of biomarkers for the ovarian cancer diagnosis. Eur J Obstet Gynecol Reprod Biol. 2011;158:119–23. doi: 10.1016/j.ejogrb.2011.04.023. [DOI] [PubMed] [Google Scholar]
- 71.Nour NM. Cervical cancer: A preventable death. Rev Obstet Gynecol. 2009;2:240–4. [PMC free article] [PubMed] [Google Scholar]
- 72.Saraiya UB. Preventable but not prevented: The reality of cervical cancer. J Obstet Gynaecol Res. 2003;29:351–9. doi: 10.1046/j.1341-8076.2003.00126.x. [DOI] [PubMed] [Google Scholar]
- 73.Black PA. Cervical cancer: A preventable problem. Prof Nurse. 1989;4:338–42. [PubMed] [Google Scholar]
- 74.Wentzensen N, von Knebel Doeberitz M. Biomarkers in cervical cancer screening. Dis Markers. 2007;23:315–30. doi: 10.1155/2007/678793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Litjens RJ, Hopman AH, van de Vijver KK, Ramaekers FC, Kruitwagen RF, Kruse AJ. Molecular biomarkers in cervical cancer diagnosis: A critical appraisal. Expert Opin Med Diagn. 2013;7:365–77. doi: 10.1517/17530059.2013.808621. [DOI] [PubMed] [Google Scholar]
- 76.Schmidt D, Bergeron C, Denton KJ, Ridder R European CINtec Cytology Study Group. p16/ki-67 dual-stain cytology in the triage of ASCUS and LSIL papanicolaou cytology: Results from the European equivocal or mildly abnormal Papanicolaou cytology study. Cancer Cytopathol. 2011;119:158–66. doi: 10.1002/cncy.20140. [DOI] [PubMed] [Google Scholar]
- 77.Overmeer RM, Henken FE, Snijders PJ, Claassen-Kramer D, Berkhof J, Helmerhorst TJ, et al. Association between dense CADM1 promoter methylation and reduced protein expression in high-grade CIN and cervical SCC. J Pathol. 2008;215:388–97. doi: 10.1002/path.2367. [DOI] [PubMed] [Google Scholar]
- 78.Overmeer RM, Henken FE, Bierkens M, Wilting SM, Timmerman I, Meijer CJ, et al. Repression of MAL tumour suppressor activity by promoter methylation during cervical carcinogenesis. J Pathol. 2009;219:327–36. doi: 10.1002/path.2598. [DOI] [PubMed] [Google Scholar]
- 79.Peitsaro P, Johansson B, Syrjänen S. Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol. 2002;40:886–91. doi: 10.1128/JCM.40.3.886-891.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.WHO. International Agency for Research on Cancer: Latest world statistics. [Last accessed date on 2014 Jul 09]. Available from: http://www.iarc.fr/en/media-centre/pr/2013/pdfs/pr223_E.pdf .
- 81.Gupta S, Venkatesh A, Ray S, Srivastava S. Challenges and prospects for biomarker research: A current perspective from the developing world. Biochim Biophys Acta. 2014;1844:899–908. doi: 10.1016/j.bbapap.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 82.Smith RA, Brooks D, Cokkinides V, Saslow D, Brawley OW. Cancer screening in the United States, 2013: A review of current American Cancer Society guidelines, current issues in cancer screening, and new guidance on cervical cancer screening and lung cancer screening. CA Cancer J Clin. 2013;63:88–105. doi: 10.3322/caac.21174. [DOI] [PubMed] [Google Scholar]
- 83.Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL. Human breast cancer: Correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science. 1987;235:177–82. doi: 10.1126/science.3798106. [DOI] [PubMed] [Google Scholar]
- 84.Chung C, Christianson M. Predictive and prognostic biomarkers with therapeutic targets in breast, colorectal, and non-small cell lung cancers: A systemic review of current development, evidence, and recommendation. J Oncol Pharm Pract. 2014;20:11–28. doi: 10.1177/1078155212474047. [DOI] [PubMed] [Google Scholar]
- 85.Drake RR, Kislinger T. The proteomics of prostate cancer exosomes. Expert Rev Proteomics. 2014;11:167–77. doi: 10.1586/14789450.2014.890894. [DOI] [PubMed] [Google Scholar]
- 86.Cremona M, Espina V, Caccia D, Veneroni S, Colecchia M, Pierobon M, et al. Stratification of clear cell renal cell carcinoma by signaling pathway analysis. Expert Rev Proteomics. 2014;11:237–49. doi: 10.1586/14789450.2014.893193. [DOI] [PubMed] [Google Scholar]
- 87.Gasparini P, Cascione L, Fassan M, Lovat F, Guler G, Balci S, et al. microRNA expression profiling identifies a four microRNA signature as a novel diagnostic and prognostic biomarker in triple negative breast cancers. Oncotarget. 2014;5:1174–84. doi: 10.18632/oncotarget.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Iida M, Banno K, Yanokura M, Nakamura K, Adachi M, Nogami Y, et al. Candidate biomarkers for cervical cancer treatment: Potential for clinical practice. Mol Clin Oncol. 2014;2:647–55. doi: 10.3892/mco.2014.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mankoff DA, Pryma DA, Clark AS. Molecular imaging biomarkers for oncology clinical trials. J Nucl Med. 2014;55:525–8. doi: 10.2967/jnumed.113.126128. [DOI] [PubMed] [Google Scholar]
- 90.Jeng JC, Lee K, Jablonski K, Jordan MH. Serum lactate and base deficit suggest inadequate resuscitation of patients with burn injuries: Application of a point-of-care laboratory instrument. J Burn Care Rehabil. 1997;18:402–5. doi: 10.1097/00004630-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 91.Leskovan JJ, Justiniano CF, Bach JA, Cook CH, Lindsey DE, Eiferman DS, et al. Anion gap as a predictor of trauma outcomes in the older trauma population: Correlations with injury severity and mortality. Am Surg. 2013;79:1203–6. [PubMed] [Google Scholar]
- 92.Paratz JD, Stockton K, Paratz ED, Blot S, Muller M, Lipman J, et al. Burn resuscitation-hourly urine output vs alternative endpoints: A systematic review. Shock. 2014 doi: 10.1097/SHK.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 93.Welch WJ. Heat shock proteins as biomarkers for stroke and trauma. Am J Med. 2001;111:669–70. doi: 10.1016/s0002-9343(01)01046-4. [DOI] [PubMed] [Google Scholar]
- 94.Volpin G, Cohen M, Assaf M, Meir T, Katz R, Pollack S. Cytokine levels (IL-4, IL-6, IL-8 and TGFbeta) as potential biomarkers of systemic inflammatory response in trauma patients. Int Orthop. 2014;38:1303–9. doi: 10.1007/s00264-013-2261-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hagiwara S, Oshima K, Aoki M, Murata M, Ishihara K, Kaneko M, et al. Usefulness of fibrin degradation products and d-dimer levels as biomarkers that reflect the severity of trauma. J Trauma Acute Care Surg. 2013;74:1275–8. doi: 10.1097/TA.0b013e31828cc967. [DOI] [PubMed] [Google Scholar]
- 96.Teng L, Yu M, Li JM, Tang H, Yu J, Mo LH, et al. Matrix metalloproteinase-9 as new biomarkers of severity in multiple organ dysfunction syndrome caused by trauma and infection. Mol Cell Biochem. 2012;360:271–7. doi: 10.1007/s11010-011-1066-0. [DOI] [PubMed] [Google Scholar]
- 97.Sjödin MO, Bergquist J, Wetterhall M. Mining ventricular cerebrospinal fluid from patients with traumatic brain injury using hexapeptide ligand libraries to search for trauma biomarkers. J Chromatogr B Analyt Technol Biomed Life Sci. 2010;878:2003–12. doi: 10.1016/j.jchromb.2010.05.036. [DOI] [PubMed] [Google Scholar]
- 98.Neselius S, Brisby H, Theodorsson A, Blennow K, Zetterberg H, Marcusson J. CSF-biomarkers in Olympic boxing: Diagnosis and effects of repetitive head trauma. PLoS One. 2012;7:e33606. doi: 10.1371/journal.pone.0033606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Svetlov SI, Larner SF, Kirk DR, Atkinson J, Hayes RL, Wang KK. Biomarkers of blast-induced neurotrauma: Profiling molecular and cellular mechanisms of blast brain injury. J Neurotrauma. 2009;26:913–21. doi: 10.1089/neu.2008.0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Genét GF, Johansson PI, Meyer MA, Sølbeck S, Sørensen AM, Larsen CF, et al. Trauma-induced coagulopathy: Standard coagulation tests, biomarkers of coagulopathy, and endothelial damage in patients with traumatic brain injury. J Neurotrauma. 2013;30:301–6. doi: 10.1089/neu.2012.2612. [DOI] [PubMed] [Google Scholar]
- 101.Van den Eckart E, Tran E, Caldwell E, Fu X, Watkins T.R, Rayner S.G. Transfusion and urinary biomarkers of systemic oxidative injury and platelet activation in trauma patients. Am J Respir Crit Care Med. 2013;187:A1239. [Google Scholar]


