Abstract
Pulmonary embolism, Deep Vein Thrombosis (DVT) and Disseminated intravascular coagulation (DIC) are important sources of mortality and morbidity in intensive care unit (ICU). And every time D-dimer remains the the commonest investigation. Many times D-dimer is erroneously considered as a diagnostic test in above mentioned conditions. Its interpretation requires cautions. To circumvent this source of error it is necessary to understand D-dimer test and its significance in various disorder. This article review some basic details of D-dimer, condition associated with its increased level and some prognostic value in intracranial hemorrhage and gastrointestinal (GI) bleed.
Keywords: Deep vein thrombosis, Disseminated intravascular coagulation, D-Dimer, pulmonary embolism
INTRODUCTION
The antigen Fibrin D-dimer (DD) is the primary enzymatic degradation product of cross-linked fibrin by plasmin. Systemic values of DD are an index of fibrin turnover in the circulation and a single measurement may be adequate to assess the fibrinolytic status. Despite the implementation of clinical guideline, inappropriate DD testing is a significant problem. It is, consequently, valuable for emergency as well as intensive care physicians to be knowledgeable about the pathophysiological basis and limitations of DD testing to ensure its appropriate clinical use.[1]
PATHOPHYSIOLOGY
Fibrin is the main component of a thrombus. It is formed by the activation of the coagulation system. Its production is followed by activation of the fibrinolytic system, resulting in plasmin generation and subsequent fibrin lysis. Plasmin, the fibrinolytic enzyme, derived from its inactive precursor, plasminogen, by the action of thrombin and plasminogen activator, that is tissue plasminogen activator (TPA) and prourokinase mainly. Plasmin is neutralized by Alfa 2 antiplasmin thereby restricting its fibrinogenolytic activity and localizing the fibrinolysis on the fibrin clot. Under the physiological conditions there is balance of the two opposing processes [Figure 1].[1]
Figure 1.
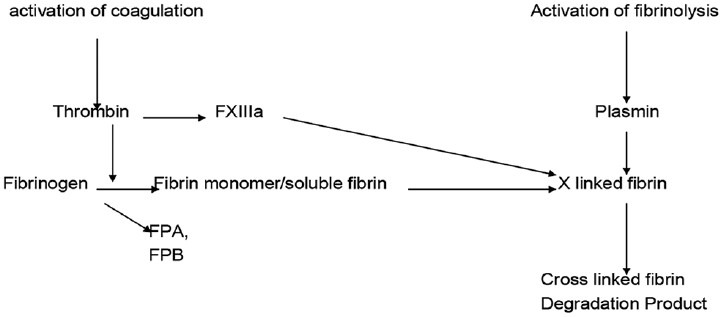
FPA and FPB–Fibrinopeptied A and B. D dimer production (from Wakai et al, 2003
Conditions associated with increased DD titer
Non pathological
Cigarette smoking
Age (healthy elderly patient)
Functional impairment
Race
Pregnancy
Postoperative status.
Pathological
Trauma
Pre-eclampsia
Malignancy
Infection
Disseminated intravascular coagulation
Sickle cell disease
Atrial or venous thromboembolism (VTE)
Atrial fibrillation
Acute coronary syndromes
Stroke
Acute upper gastro intestinal haemorrhage.
Many conditions are associated with raised DD so it has limited specificity. Local fibrin formation and lysis are part of the inflammatory response. Fibrin degradation products (FDP), including DD has been shown to modulate acute phase responses and the production of variety of systemic inflammatory mediator. DD assays especially qualitative latex agglutination assay is not 100% sensitive, limiting their utility as a single screening test.
DD ASSAYS
DD assays detect the presence of D-Dimer in whole blood or plasma of plasmin mediated FDPs that contain cross linked D fragments. Various assays are available.[2]
Manual immunoagglutination assays
Manual immunochromatographic assays
Immuno filtration assays Microplate enzyme linked immunoassay (ELISA) systems
Automated ELISA systems
Latex enhanced photometric immunoassays.
All these assays use a monoclonal antibody against epitopes on the DD fragment that are absent on fibrin, fibrinogen, and non-crosslinked fragment of fibrin. Depending on the degree of the cross linked fibrin a heterogeneous mixture of FDPs of different molecular weight containing the DD moiety may be formed. The reactivity of different DD monoclonal antibodies to these different molecular weight species varies, causing variable results with different assays within individual patients. In addition, some monoclonal antibodies may cross react with non cross linked degradation products of fibrin or fibrinogen.
Among them, a whole blood manual immunoagglutination test that gives qualitative results within 2 minutes (SimpliRED) and more recent immunochromatographic test gives semi quantitative results in 10 minutes. Rapid ELISA assay requires 35 minutes to give quantitative results.
SimpliRED has disadvantage of having visual interpretation so chances of interobserver variation are high, whereas rapid ELISA is highly sensitive but is too cumbersome for emergency use.
New turbidimetric immunoassay may be equal in sensitivity and slightly better specificity in ED department. Also it is less cumbersome to perform than ELISA.
D DIMER AND PULMONARY EMBOLISM
DD can be detected in serum using variety of different assay [Table 1].
Table 1.
D DIMER testing techniques
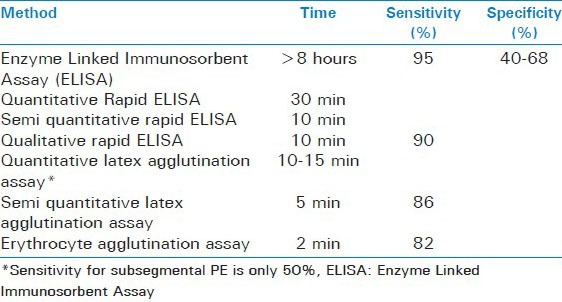
Different assays, turn around time, sensitivity and specificity for PE have been tabulated in above table.[3]
Hospitalized patients especially with malignancy or rectal surgery, severe renal dysfunction (GFR < 60 ml/min)[4] and increased age[5] lead to high DD level. That is the reason for low specificity.
NEGATIVE PREDICTIVE VALUE IN PE: D DIMER PLUS PRETEST PROBABILITY
Ability of normal or negative DD to exclude acute PE depends on both the type of D dimer assay and clinical pretest probability. Evidence indicates that a DD level < 500 ng/ml by quantitative ELISA or semiquantitative latex agglutination is sufficient to rule out PE with low pretest probability of PE. A negative DD by erythrocyte agglutination is only sufficient to exclude PE in patient with low pretest probability.[3,6,7,8,9]
D dimer in DVT
Duplex scanning, the present method of choice for the diagnosis of Deep Vein Thrombosis (DVT), is comparatively time consuming and expensive. In addition, the majority of imaging studies for patients with suspected DVT, up to 98% in one study, are negative. A highly sensitive and simple test used for initial screening and ruling out DVT in substantial proportion of subjects, might be cost effective. More specific ultrasound sonography (USG) test would then be applied only in patients presenting with a DD concentration above the appropriate cut-off point. Wells et al., in 2003 demonstrated that with the use of DD there was significant reduction in USG for DVT. (Up to 40%).[10]
A meta analysis of 11 studies pooling 1337 patients revealed a negative predictive value of DD assays of 94% when DD were les then 500 ng/ml.[11] The likelihood of VTE remained < 10% even when pretest probabilities were as high as 55%.[12]
D dimer in atrial fibrillation
A best Bets review (updated in 2007) suggests that a negative DD test may be able to rival echocardiography (ECG) in ruling out an atrial thrombus in atrial fibrillation (negative predictive value of 98%), thus allowing cardioversion to be safely performed in the emergency department without need for further investigation. However many of the studies included were in Japanese language and only English language abstract were appraised. A large well designed study is needed to confirm these promising finding.[13]
D dimer in aortic dissection
The systemic review of 10 studies by Sutherland et al. (2008) showed that DD cannot be used as a sole screening tool for acute aortic dissection.[14]
D dimer in elderly patient
It is known that DD concentrations increase with age and specificity of DD test is decreased in older patients, making the test less useful for excluding VTE. A recent retrospective study by Douma et al., (2010) suggests that higher cut off value (age × 10 μg/L) can be safely used in patient over 50 years of age.[15]
D dimer in pregnancy
Increased level of DD in pregnancy has been confirmed in various studies. DD result is always positive in third trimester. A negative DD test in a patient with low pretest probability still rules out VTE.[16]
Coronary Ischaemia
DD is positively associated with coronary heart disease incidence[17,18] or recurrence.[19] Bayes et al., have recently demonstrated that plasma DD values are significantly higher in patients with acute ischemic events [myocardial infarction (MI) and unstable angina] than in non ischemic patients. DD concentration > 500 μg/l has an independent diagnostic value for MI and increases the diagnostic sensitivity of ECG and history from 73-92%.[20]
Plasma DD value is a potentially useful marker of coronary artery disease (CHD) risk[17,18], an addition to clinical diagnostic models for MI detection in erectile dysfunction (ED) patients with acute cardiogenic chest pain and may identify acute coronary syndrome (ACS) patients who may benefit from more aggressive antithrombotic therapy.[21] Currently the use of DD testing in ACS is limited by the inherent lack of specificity of most assays for the detection of coronary thrombosis. This limitation may at least be partially obviated using diagnostic strategies incorporating other more established markers of myocardial damage such as cardiac specific troponins.[21]
DD AS AN ED PROGNOSTIC MARKER
Increased plasma DD is associated with adverse clinical out come in acute upper GI bleed and Intracerebral hemorrhage (ICH). DD values may be an indicator of the need of emergency laparotomy in acute bowel ischaemia and emergency endoscopy in upper GI bleed. DD values may indicate the etiology of cerebral infarction Cardio-embolic and atherothrombotic strokes are associated with higher DD value compared to lacunar strokes.[1]
Clinical applicability of current data regarding the prognostic role of DD suffer from several limitations including studies that are retrospective, have small sample sizes and use of qualitative rather than quantitative DD assays.[1]
SUMMARY
Summary Following are the key points[22]
The DD test is a marker of blood clotting activity and it can be useful in various medical conditions to rule out diagnosis or improve diagnostic yield in shorter time and with reduced expenses
When used appropriately the DD test helps “rule out” VTE if the test is negative and the chance of the patient having a VTE is relatively low (pretest probability)
If the DD test is positive further investigation may or may not be necessary depending on the likely cause of the elevated DD result, of which there are many
Diagnosis of VTE is based on pretest clinical probabilities and balances the risks of further investigation against the risk of missing the diagnosis. No investigation can reduce the chance of having VTE to “absolute zero”
DD negative patients can still develop VTE and should be advised to return if symptoms worsen or new symptoms develop (e.g. worsening of leg pain and swelling, shortness of breath, chest pain or collapse).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Wakai A, Gleeson A, Winter D. Role of fibrin d-dimer testing in emergency medicine. Emerg Med J. 2003;20:319–25. doi: 10.1136/emj.20.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Monyé W, Sanson BJ, Mac Gillavry MR, Pattynama PM, Büller HR, van den Berg-Huysmans AA, et al. ANTELOPE-Study Group. Embolus location affects the sensitivity of a rapid quantitative D-dimer assay in the diagnosis of pulmonary embolism. Am J Respir Crit Care Med. 2002;165:345–8. doi: 10.1164/ajrccm.165.3.2104099. [DOI] [PubMed] [Google Scholar]
- 3.Stein PD, Hull RD, Patel KC, Olson RE, Ghali WA, Brant R, et al. D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: A systematic review. Ann Intern Med. 2004;140:589–602. doi: 10.7326/0003-4819-140-8-200404200-00005. [DOI] [PubMed] [Google Scholar]
- 4.Karami-Djurabi R, Klok FA, Kooiman J, Velthuis SI, Nijkeuter M, Huisman MV. D-dimer testing in patients with suspected pulmonary embolism and impaired renal function. Am J Med. 2009;122:1050–3. doi: 10.1016/j.amjmed.2009.03.032. [DOI] [PubMed] [Google Scholar]
- 5.Righini M, Goehring C, Bounameaux H, Perrier A. Effects of age on the performance of common diagnostic tests for pulmonary embolism. Am J Med. 2000;109:357–61. doi: 10.1016/s0002-9343(00)00493-9. [DOI] [PubMed] [Google Scholar]
- 6.Ginsberg JS, Wells PS, Kearon C, nderson D, Crowther M, Weitz JI, et al. Sensitivity and specificity of a rapid whole-blood assay for D-dimer in the diagnosis of pulmonary embolism. Ann Intern Med. 1998;129:1006–11. doi: 10.7326/0003-4819-129-12-199812150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Kearon C, Ginsberg JS, Douketis J, Turpie AG, Bates SM, Lee AY, et al. Canadian Pulmonary Embolism Diagnosis Study (CANPEDS) Group. An evaluation of D-dimer in the diagnosis of pulmonary embolism: A randomized trial. Ann Intern Med. 2006;144:812–21. doi: 10.7326/0003-4819-144-11-200606060-00007. [DOI] [PubMed] [Google Scholar]
- 8.Sox HC. Commentary. Ann Intern Med. 2004;140:602–18. [Google Scholar]
- 9.Stein PD, Woodard PK, Weg JG, Wakefield TW, Tapson VF, Sostman HD, et al. Diagnostic pathways in acute pulmonary embolism: Recommendations of the PIOPED II investigators. Am J Med. 2006;119:1048–55. doi: 10.1016/j.amjmed.2006.05.060. [DOI] [PubMed] [Google Scholar]
- 10.Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349:1227–35. doi: 10.1056/NEJMoa023153. [DOI] [PubMed] [Google Scholar]
- 11.Bounameaux H, de Moerloose P, Perrier A, Reber G. Plasma measurement of D-dimer as diagnostic aid in suspected venous thromboembolism: An overview. Thromb Haemost. 1994;71:1–6. [PubMed] [Google Scholar]
- 12.Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, et al. Application of a diagnostic clinical model for the management of hospitalized patients with suspected deep-vein thrombosis. Thromb Haemost. 1999;81:493–7. [PubMed] [Google Scholar]
- 13.Body R, Allie B. Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. Negative D-dimer may allow safe early cardioversion of atrial fibrillation. Emerg Med J. 2007;24:432–5. doi: 10.1136/emj.2007.049510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sutherland A, Escano J, Coon TP. D-Dimer as the sole screening test for acute aortic dissection: A review of literature. Ann Emerg Med. 2008;52:339–43. doi: 10.1016/j.annemergmed.2007.12.026. [DOI] [PubMed] [Google Scholar]
- 15.Douma RA, le Gal G, Söhne M, Righini M, Kamphuisen PW, Perrier A, et al. Potential of an age adjusted D-dimer cut-off value to improve the exclusion of pulmonary embolism in older patients: A retrospective analysis of three large cohorts. BMJ. 2010;340:C1475. doi: 10.1136/bmj.c1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan WS, Chunilal S, Lee A, Crowther M, Rodger M, Ginsberg JS. A red blood cell agglutination D-dimer test to exclude deep venous thrombosis in pregnancy. Ann Intern Med. 2007;147:165. doi: 10.7326/0003-4819-147-3-200708070-00005. [DOI] [PubMed] [Google Scholar]
- 17.Folsom AR, Alecsic N, Park E, Salomaa V, Juneja H, Wu KK. Prospective study of fibrinolytic factors and incident coronary heart disease: The Atherosclerosis Risk in Communities (ARIC) study. Arterioscler Thromb Vasc Biol. 2001;21:611–7. doi: 10.1161/01.atv.21.4.611. [DOI] [PubMed] [Google Scholar]
- 18.Lowe GD, Yarnell JW, Rumbley A, Bainton D, Sweetnam PM. C-reactive protein, fibrin D-dimer and incident ischaemic heart disease in the Speedwell study: Are inflammation and fibrin turnover linked in pathogenesis? Arterioscler Thromb Vasc Biol. 2001;21:603–10. doi: 10.1161/01.atv.21.4.603. [DOI] [PubMed] [Google Scholar]
- 19.Moss AJ, Goldstein RE, Marder VJ, Sparks CE, Oakes D, Greenberg H, et al. Thrombogenic factors and recurrent coronary events. Circulation. 1999;99:2517–22. doi: 10.1161/01.cir.99.19.2517. [DOI] [PubMed] [Google Scholar]
- 20.Bayes-Genis A, Mateo J, Santalo M, Oliver A, Guindo J, Badimon L, et al. D dimer is an early diagnostic marker of coronary ischaemia in patients with chest pain. Am Heart J. 2000;140:379–84. doi: 10.1067/mhj.2000.108823. [DOI] [PubMed] [Google Scholar]
- 21.Ottani F, Galvani M. Prognostic role of hemostatic markers in acute coronary syndrome patients. Clin Chim Acta. 2001;311:33–9. doi: 10.1016/s0009-8981(01)00555-1. [DOI] [PubMed] [Google Scholar]
- 22. [Last accessed on 2014 Sep 12]. Available from: http://lifeinthefastlane.com/hematology-hoodwinker-001/


