Abstract
Esophagogastric varices are the most common complication in patients with portal hypertension, and endoscopy plays an important role in their diagnosis and in the prevention of acute bleeding from these structures. Recently, new modalities such as endoscopic ultrasonography (EUS) and narrow-band imaging have been introduced for the diagnosis of esophagogastric varices. In Japan, endoscopic therapy has become the first choice for the treatment of acutely bleeding esophageal or gastric varices. The two principal methods used to treat esophageal varices are endoscopic injection sclerotherapy (EIS) and endoscopic variceal ligation (EVL). Recently, combinations of EIS plus EVL and EVL plus argon plasma coagulation were reported to be more effective than EVL or EIS alone. Additionally, endoscopic cyanoacrylate injection is superior to EIS and EVL for the treatment of acutely bleeding gastric varices.
Keywords: Endoscopic management, esophagogastric varices, endoscopic injection sclerotherapy (EIS), endoscopic variceal ligation (EVL)
Introduction
Portal hypertension is the primary complication of liver cirrhosis and is defined as a pathological increase in the portal venous pressure or an increase in the hepatic venous pressure gradient (HVPVG) above the normal range (1-5 mmHg).
Portal hypertension induces the development of port-systemic collateral vessels. Of these, esophagogastric varices are the most relevant because their rupture results in variceal hemorrhage, which is among the most common lethal complications of cirrhosis. In patients diagnosed with cirrhosis, esophagogastric variceal development occurs at an annual rate of 5-7% (1). Initial esophagogastric variceal bleeding occurs in approximately 12% of patients within 1 year (5% and 15% of small and large varices, respectively) (2,3). Moreover, patients with advanced liver disease and varices that feature red wale marks have a high risk of variceal hemorrhage (4). These complications are a major cause of death, with a 6-week mortality rate of 15-20%, and are the main indication for liver transplantation in patients with liver cirrhosis (5,6).
Variceal hemorrhage is managed as follows: primary prophylaxis to prevent an initial episode of variceal hemorrhage, treatment of acute bleeding episodes, and secondary prophylaxis to prevent recurrent hemorrhage.
Previously, surgery was the only treatment for esophagogastric varices. Interventional radiology (IVR) was introduced in the 1970s; endoscopic treatment was subsequently developed in the 1980s and led to improved survival rates. Currently, endoscopy plays an important role in the diagnosis and prevention of esophagogastric varices and the treatment of acute variceal bleeding.
In this review, we evaluate the current status of the endoscopic management of esophageal varices.
General rules for recording the endoscopic findings of esophagogastric varices in Japan (Table 1)
Table 1. General rules for recording the endoscopic findings of esophagogastric varices in Japan.
| Location (L) |
| Ls: locus superior |
| Lm: locus medialis |
| Li: locus inferior |
| Lg-c: adjacent to the cardiac orifice |
| Lg-cf: extension from the cardiac orifice to the fornix |
| Lg-f: isolated in the fornix |
| Lg-b: located in the gastric body |
| Lg-a: located in the gastric antrum |
| Form (F) |
| F0: no varicose appearance |
| F1: straight, small-caliber varices |
| F2: moderately enlarged, beady varices |
| F3: markedly enlarged, nodular or tumor-shaped varices |
| Color (C) |
| Cw: white varices |
| Cb: blue varices |
| Cw-Th: thrombosed white varices |
| Cb-Th: thrombosed blue varices |
| Red color signs (RC) |
| RWM: red wale markings |
| CRS: cherry red spots |
| HCS: hematocystic spots |
| Esophageal varices: RC0, RC1, RC2, RC3 |
A precise system for the systemic evaluation and recording of esophagogastric varices is essential to the management of portal hypertension. In Japan, a general system is used to record the endoscopic findings of esophageal varices. This system was initially proposed by the Japanese Research Society for Portal Hypertension in 1980 and was revised in 1991 (7). In this system, esophageal and gastric varices are classified according to the color (white and blue), form (small and straight, F1; nodular, F2; and large or coiled, F3), and red color signs (RC 0-3). Gastric varices are divided into those that involve the cardia (Lg-c), the fundus (Lg-f), or both the cardia and fundus (Lg-cf). Bleeding is classified as gushing, spurting, or oozing. As a result of recent progress in this field, these rules were revised to include the newly recognized findings of portal hypertensive gastropathy (PHG) and a new classification for endoscopic ultrasonographic findings (8).
Utility of endoscopic ultrasonography (EUS) for esophagogastric varices
In principal, endoscopic diagnoses are based on endoscopic findings that have been assessed with the naked eye. However, it is impossible to assess deep collateral vessels in this manner. EUS was introduced to visualize the collateral channels that surround the distal esophagus and upper stomach. On EUS images, esophageal varices appear as an echo-free or hyperechoic lumen in the esophageal submucosa. The technique of EUS is noninvasive and can show high resolution images of the collaterals in close proximity to the gut lumen. Various institutions have reported the utility of EUS for evaluating esophagogastric varix hemodynamics and predicting variceal bleeding (9-11). Irisawa et al. demonstrated that EUS-detected, severe-type peri-esophageal collateral vessels could be significant predictors of esophageal varix recurrence (9). EUS can visualize and evaluate collateral veins around the esophagus with portal hypertension. EUS allows visualization of the left gastric vein. The diameter of the left gastric vein is associated with variceal size (12). Moreover, Iwase et al. showed that color Doppler EUS could also detect left gastric vein and rapid hepatofugal velocity, which might indicate the risk of esophageal varix recurrence (13).
Endoscopic therapy is difficult to perform on acutely bleeding gastric varices; however, an EUS-guided cyanoacrylate adhesive treatment for gastric variceal bleeding was recently reported (14,15).
Endoscopic management of esophageal varices (Figure 1)
Figure 1.
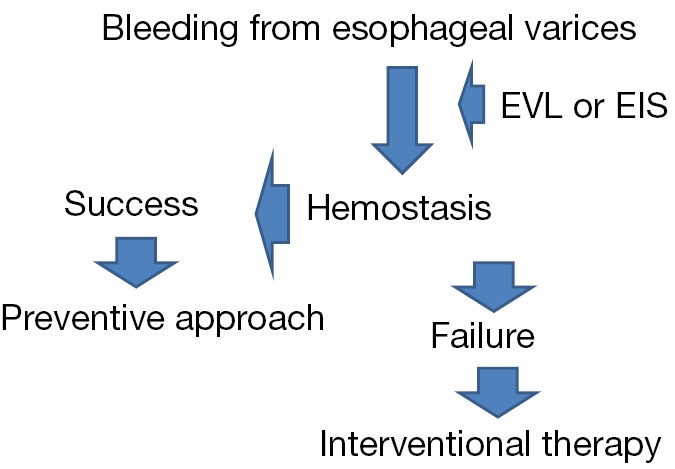
Endoscopic treatment of acute esophageal varices. EVL, endoscopic variceal ligation; EIS, endoscopic injection sclerotherapy.
Endoscopic techniques are considered optimal treatments for acutely bleeding varices and are also well suited for long-term management to prevent recurrences. Therefore, endoscopic therapy is considered a first-line treatment for bleeding esophageal varices and is also used to prevent initial variceal hemorrhage and to provide secondary prophylaxis.
In Japan, F2 (nodular, moderately enlarged) and F3 (markedly enlarged) esophageal varices with RC sighs is high risk sign of bleeding. Therefore, this high risk group is performed prophylactic endoscopic treatment.
Endoscopic injection sclerotherapy (EIS) and endoscopic variceal ligation (EVL) are the two primary endoscopic methods used to prevent the initial episodes of variceal hemorrhage or to treat acutely bleeding esophageal varices.
Endoscopic injection sclerotherapy (EIS)
For many years, EIS has been used to treat esophageal varices. Flexible endoscopic sclerotherapy was introduced in the 1980s, and has been widely used since then, resulting in an improved survival rate for these patients.
This technique was introduced in Japan in 1980s and was reported to be an efficacious therapy.
Some sclerosants such as sodium nitrate, podicocanol, ethanolamine, alcohol, and sodium tetradecyl sulfate have been widely used for EIS (16,17). In Japan, ethanolamine oleate (EO) is the most commonly used sclerosant. Injection of EO causes an acute, dose-related inflammatory reaction of the intimal endothelium of the vein. This leads to scarring and possible occlusion of the vein. However, EO is hemolytic, and the resultant free hemoglobin can cause renal failure, Therefore, haptogloblin are used as preventive (18). In other countries, its complications and lack of experience with EO has made its use infrequent.
EIS comprises an injection into the variceal lumen or area adjacent to the varix to induce vessel thrombosis. With repeated sessions, the vascular wall inflammation promotes fibrosis and subsequent variceal obliteration. There are some technical variations associated with EIS, including the device used and the type and concentration of the sclerosant (19). Some endoscopists perform this technique in a free-hand manner, whereas others incorporate a balloon placed on the end of the endoscope to compress the varices following the injections.
The sclerosant can be injected either intravariceally or paravariceally. Paravariceal injections, when administered immediately adjacent and slightly distal to the bleeding site, form a protective fibrotic layer around the varices. In contrast, intravariceal injections directly induce variceal thrombosis.
EIS is inexpensive, easily performed, and effective. However, there are several complications associated with this technique. Minor complications such as a low-grade fever, chest pain, and dysphagia can occur within the first 24-48-hrs after the procedure and do not require treatment (20,21).
Local complications such as esophageal ulcers, ulcer-related bleeding, and esophageal strictures are also associated with EIS. Most of these complications are induced by incorrect injections or high sclerosant concentrations (20) and usually heal with omeprazole treatment. Esophageal stenosis occurs in 2-10% of cases.
Sclerotherapy-related mortalities have been reported in 2% of treated patients; these often result from major complications such as recurrent bleeding, perforation, sepsis, and respiratory disease (22).
Endoscopic variceal ligation (EVL)
In 1989, Stiegmannand and Golf reported the use of EVL for the treatment of esophageal varices (23). EIS chemically occludes the variceal walls, whereas EVL obliterates varices via mechanical strictures induced by rubber bands.
First, the endoscope is introduced along with a flexible sheath for EVL. Next, the endoscope is removed to allow the attachment of an EVL device. As each varix is drawn into the cap of the endoscope tip, air is injected into the tube to stricture the varix. During the first EVL session, the varices are ligated on the oral side of the gastroesophageal junction. Varix eradication usually requires 2 or 3 sessions.
For actively bleeding esophageal varices, the rubber band should be introduced at the bleeding point. If the bleeding point cannot be identified, varices should be ligated at the oral side of the gastroesophageal junction.
Varix eradication is achieved in approximately 90% of patients, although recurrence is not rare (24). However, recurrence after EVL does not carry a high risk of recurrent bleeding.
Recurrent varices can usually be treated with repeated ligation. Yoshida et al. reported a lower recurrence rate when EVL was performed once every 2 months versus every 2 weeks (25).
Both EIS and EVL are reportedly effective for acute variceal bleeding; however, EVL is the first-choice therapy because of its safety and ease of use. The complications associated with EVL include esophageal laceration or perforation, transient dysphagia, chest pain, esophageal stricture, and ulcer-related bleeding (26). The reported incidence of bacteremia and infection was higher after EIS than after EVL. Some meta-analyses have shown that EVL was well suited for the treatment of acute bleeding and was associated with fewer adverse events and improved mortality when compared with EIS (27).
Currently, EVL is considered the gold standard for variceal eradication. However, EVL is plagued by a high recurrence rate after variceal eradication because it does not obliterate the deeper varices and perforating veins (28,29), whereas the chemical effect of EIS reaches deeper varices and perforating veins. Therefore, the combinations of EIS plus EVL are reportedly more effective than EVL alone (30). Likewise, EVL plus argon plasma laser induce fibrosis of the esophageal mucosa; result in suppression of variceal recurrence (31). A meta-analysis revealed that, compared with drug therapy alone, a combination of endoscopy and drug therapy further reduced the incidence of overall and variceal bleeding (32). Therefore, combined therapy is required to reduce the recurrence rate.
Endoscopic management of acutely bleeding gastric varices (Figure 2)
Figure 2.
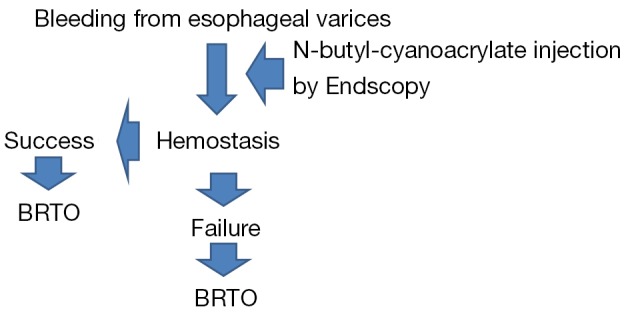
Endoscopic treatment of acute gastric varices.
Unlike esophageal varices, EIS and EVL do not efficiently treat gastric varices. Regarding EIS, the higher volume of blood flow in gastric varices leads to the rapid flushing of the sclerosant from the blood stream. EIS for gastric varices requires larger volumes of sclerosants than those required for esophageal varices and consequently induces more side effects (33).
High recurrent bleeding rates (up to 90%) have been reported with EIS for gastric varices (33,34). Although EVL is generally safe, its ability to control gastric variceal bleeding is limited (35-37). Some case series initially demonstrated the safety and efficacy of EVL for the treatment of acute gastric variceal bleeding. The reported 3-year re-bleeding rate associated with EVL for gastric variceal bleeding was 72% (37).
Obstruction resulting from the injection of a tissue adhesive such as N-butyl-cyanoacrylate (Histoacryl®) was found to be more effective than sclerotherapy for the treatment of acute gastric variceal bleeding (38,39). The re-bleeding rate associated with gastric variceal obstruction ranges from 22-37% (38,40-43). Prospective and randomized controlled studies designed to evaluate the optimal management of bleeding from gastric varices (44) demonstrated that gastric variceal obstruction resulted in improved clinical benefit compared to EIS and EVL.
Kumar et al. reported that undiluted Histoacryl was effective in achieving initial hemostasis in case of actively bleeding gastric varices and not associated with embolic complications (45). However, in many Japanese institutions, Histoacryl is diluted with lipiodol, a radiopaque contrast agent to (1) prevention of polymerization of Histoacryl so that it may be injected easily into varices and (2) to enable radiographic visualization of obliterated varices (46).
Some of the common complications associated with gastric variceal obstruction include pyrexia and abdominal pain/discomfort; severe complications include systemic thromboembolic phenomena such as cerebral, pulmonary, portal vein, and splenic infarction (47-49).
Taken together, gastric variceal obstruction is recommended as the treatment of choice for acute gastric variceal bleeding because of its high efficacy as a treatment for acute bleeding and its association with a lower re-bleeding rate relative to EIS and EVL.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med 2005;353:2254-61. [DOI] [PubMed] [Google Scholar]
- 2.Merli M, Nicolini G, Angeloni S, et al. Incidence and natural history of small esophageal varices in cirrhotic patients. J Hepatol 2003;38:266-72. [DOI] [PubMed] [Google Scholar]
- 3.D’Amico G, Pagliaro L, Bosch J.Pharmacological treatment of portal hypertension: an evidence-based approach. Semin Liver Dis 1999;19:475-505. [DOI] [PubMed] [Google Scholar]
- 4.North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices . Prediction of the first variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter study. N Engl J Med 1988;319:983-9. [DOI] [PubMed] [Google Scholar]
- 5.Bosch J, Garcia-Pagan JC. Prevention of variceal rebleeding. Lancet 2003;361:952-4. [DOI] [PubMed] [Google Scholar]
- 6.Villanueva C, Piqueras M, Aracil C, et al. A randomized controlled trial comparing ligation and sclerotherapy as emergency endoscopic treatment added to somatostatin in acute variceal bleeding. J Hepatol 2006;45:560-7. [DOI] [PubMed] [Google Scholar]
- 7.Idezuki Y.General rules for recording endoscopic findings of esophagogastric varices (1991). Japanese Society for Portal Hypertension. World J Surg 1995;19:420-2; discussion 423. [DOI] [PubMed] [Google Scholar]
- 8.The Japan Society for Portal Hypertension. eds. The general rules for Study of Portal Hypertension, 2nd end. Tokyo: Kanehara Co., 2004:37-50. [Google Scholar]
- 9.Irisawa A, Saito A, Obara K, et al. Endoscopic recurrence of esophageal varices is associated with the specific EUS abnormalities: severe periesophageal collateral veins and large perforating veins. Gastrointest Endosc 2001;53:77-84. [DOI] [PubMed] [Google Scholar]
- 10.Miller L, Banson FL, Bazir K, et al. Risk of esophageal variceal bleeding based on endoscopic ultrasound evaluation of the sum of esophageal variceal cross-sectional surface area. Am J Gastroenterol 2003;98:454-9. [DOI] [PubMed] [Google Scholar]
- 11.Schiano TD, Adrain AL, Vega KJ, et al. High-resolution endoluminal sonography assessment of the hematocystic spots of esophageal varices. Gastrointest Endosc 1999;49:424-7. [DOI] [PubMed] [Google Scholar]
- 12.Hino S, Kakutani H, Ikeda K, et al. Hemodynamic assessment of the left gastric vein in patients with esophageal varices with color Doppler EUS: factors affecting development of esophageal varices. Gastrointest Endosc 2002;55:512-7. [DOI] [PubMed] [Google Scholar]
- 13.Iwase H, Suga S, Morise K, et al. Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc 1995;41:150-4. [DOI] [PubMed] [Google Scholar]
- 14.Lee YT, Chan FK, Ng EK, et al. EUS-guided injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc 2000;52:168-74. [DOI] [PubMed] [Google Scholar]
- 15.Park WG, Yeh RW, Triadafilopoulos G. Injection therapies for variceal bleeding disorders of the GI tract. Gastrointest Endosc 2008;67:313-23. [DOI] [PubMed] [Google Scholar]
- 16.Villanueva C, Colomo A, Aracil C, et al. Current endoscopic therapy of variceal bleeding. Best Pract Res Clin Gastroenterol 2008;22:261-78. [DOI] [PubMed] [Google Scholar]
- 17.Helmy A, Hayes PC. Review article: current endoscopic therapeutic options in the management of variceal bleeding. Aliment Pharmacol Ther 2001;15:575-94. [DOI] [PubMed] [Google Scholar]
- 18.Hashizume M, Kitano S, Yamaga H, et al. Haptoglobin to protect against renal damage from ethanolamine oleate sclerosant. Lancet 1988;2:340-1. [DOI] [PubMed] [Google Scholar]
- 19.de Franchis R, Primignani M.Endoscopic treatments for portal hypertension. Semin Liver Dis 1999;19:439-55. [DOI] [PubMed] [Google Scholar]
- 20.Schuman BM, Beckman JW, Tedesco FJ, et al. Complications of endoscopic injection sclerotherapy: a review. Am J Gastroenterol 1987;82:823-30. [PubMed] [Google Scholar]
- 21.Soehendra N, Binmoeller KF. Is sclerotherapy out? Endoscopy 1997;29:283-4. [DOI] [PubMed] [Google Scholar]
- 22.Hall RJ, Lilly JR, Stiegmann GV. Endoscopic esophageal varix ligation: technique and preliminary results in children. J Pediatr Surg 1988;23:1222-3. [DOI] [PubMed] [Google Scholar]
- 23.Stiegmann GV, Goff JS, Sun JH, et al. Technique and early clinical results of endoscopic variceal ligation (EVL). Surg Endosc 1989;3:73-8. [DOI] [PubMed] [Google Scholar]
- 24.Takase Y, Ozaki A, Orii K, et al. Injection sclerotherapy of esophageal varices for patients undergoing emergency and elective surgery. Surgery 1982;92:474-9. [PubMed] [Google Scholar]
- 25.Yoshida H, Mamada Y, Taniai N, et al. A randomized control trial of bi-monthly versus bi-weekly endoscopic variceal ligation of esophageal varices. Am J Gastroenterol 2005;100:2005-9. [DOI] [PubMed] [Google Scholar]
- 26.Lo GH, Lai KH, Chang CF, et al. Endoscopic injection sclerotherapy vs. endoscopic variceal ligation in arresting acute variceal bleeding for patients with advanced hepatocellular carcinoma. J Hepatol 1994;21:1048-52. [DOI] [PubMed] [Google Scholar]
- 27.Laine L, Cook D.Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A meta-analysis. Ann Intern Med 1995;123:280-7. [DOI] [PubMed] [Google Scholar]
- 28.Seno H, Konishi Y, Wada M, et al. Endoscopic ultrasonograph evaluation of vascular structures in the gastric cardia predicts esophageal variceal recurrence following endoscopic treatment. J Gastroenterol Hepatol 2006;21:227-31. [DOI] [PubMed] [Google Scholar]
- 29.Dhiman RK, Choudhuri G, Saraswat VA, et al. Role of paraoesophageal collaterals and perforating veins on outcome of endoscopic sclerotherapy for oesophageal varices: an endosonographic study. Gut 1996;38:759-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dhiman RK, Chawla YK. A new technique of combined endoscopic sclerotherapy and ligation for variceal bleeding. World J Gastroenterol 2003;9:1090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harras F, Sheta el S, Shehata M, et al. Endoscopic band ligation plus argon plasma coagulation versus scleroligation for eradication of esophageal varices. J Gastroenterol Hepatol 2010;25:1058-65. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez R, Zamora J, Gomez-Camarero J, et al. Meta-analysis: combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med 2008;149:109-22. [DOI] [PubMed] [Google Scholar]
- 33.Sarin SK, Sachdev G, Nanda R, et al. Endoscopic sclerotherapy in the treatment of gastric varices. Br J Surg 1988;75:747-50. [DOI] [PubMed] [Google Scholar]
- 34.Gimson AE, Westaby D, Williams R. Endoscopic sclerotherapy in the management of gastric variceal haemorrhage. J Hepatol 1991;13:274-8. [DOI] [PubMed] [Google Scholar]
- 35.Yoshida T, Hayashi N, Suzumi N, et al. Endoscopic ligation of gastric varices using a detachable snare. Endoscopy 1994;26:502-5. [DOI] [PubMed] [Google Scholar]
- 36.Cipolletta L, Bianco MA, Rotondano G, et al. Emergency endoscopic ligation of actively bleeding gastric varices with a detachable snare. Gastrointest Endosc 1998;47:400-3. [DOI] [PubMed] [Google Scholar]
- 37.Shiha G, El-Sayed SS. Gastric variceal ligation: a new technique. Gastrointest Endosc 1999;49:437-41. [DOI] [PubMed] [Google Scholar]
- 38.Tan PC, Hou MC, Lin HC, et al. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology 2006;43:690-7. [DOI] [PubMed] [Google Scholar]
- 39.Sarin SK, Jain AK, Jain M, et al. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundic varices. Am J Gastroenterol 2002;97:1010-5. [DOI] [PubMed] [Google Scholar]
- 40.Oho K, Iwao T, Sumino M, et al. Ethanolamine oleate versus butyl cyanoacrylate for bleeding gastric varices: a nonrandomized study. Endoscopy 1995;27:349-54. [DOI] [PubMed] [Google Scholar]
- 41.Ramond MJ, Valla D, Mosnier JF, et al. Successful endoscopic obturation of gastric varices with butyl cyanoacrylate. Hepatology 1989;10:488-93. [DOI] [PubMed] [Google Scholar]
- 42.Tan PC, Hou MC, Lin HC, et al. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology 2006;43:690-7. [DOI] [PubMed] [Google Scholar]
- 43.Hou MC, Lin HC, Lee HS, et al. A randomized trial of endoscopic cyanoacrylate injection for acute gastric variceal bleeding: 0.5 mL versus 1.0 mL. Gastrointest Endosc 2009;70:668-75. [DOI] [PubMed] [Google Scholar]
- 44.Lo GH, Lai KH, Cheng JS, et al. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology 2001;33:1060-4. [DOI] [PubMed] [Google Scholar]
- 45.Kumar A, Singh S, Madan K, et al. Undiluted N-butyl cyanoacrylate is safe and effective for gastric variceal bleeding. Gastrointest Endosc 2010;72:721-7. [DOI] [PubMed] [Google Scholar]
- 46.Kok K, Bond RP, Duncan IC, et al. Distal embolization and local vessel wall ulceration after gastric variceal obliteration with N-butyl-2-cyanoacrylate: a case report and review of the literature. Endoscopy 2004;36:442-6. [DOI] [PubMed] [Google Scholar]
- 47.Cheng PN, Sheu BS, Chen CY, et al. Splenic infarction after histoacryl injection for bleeding gastric varices. Gastrointest Endosc 1998;48:426-7. [DOI] [PubMed] [Google Scholar]
- 48.Roesch W, Rexroth G.Pulmonary, cerebral and coronary emboli during bucrylate injection of bleeding fundic varices. Endoscopy 1998;30:S89-90. [DOI] [PubMed] [Google Scholar]
- 49.Chang CJ, Shiau YT, Chen TL, et al. Pyogenic portal vein thrombosis as a reservoir of persistent septicemia after cyanoacrylate injection for bleeding gastric varices. Digestion 2008;78:139-43. [DOI] [PubMed] [Google Scholar]


