Abstract
INTRODUCTION
Inflammatory fibroid polyps (IFPs) are rare and small benign lesions throughout the digestive tract. The most common location is gastric antrum, but rarely at the upper part. Clinical manifestations of IFPs usually include intestinal obstruction, intussusception, abdominal pain, nausea and vomiting, but rare massive digestive tract hemorrhage.
PRESENTATION OF CASE
We describe a rare case presenting with massive gastrointestinal bleeding due to a huge gastric fundus IFP (11 cm). Finally, the patient was treated successfully by the laparoscopic assisted partial gastrectomy (LAPG) and recovered uneventfully. To our knowledge, this is the first reported case presenting with massive alimentary tract hemorrhage due to giant gastric fundus IFP.
DISCUSSION
Giant IFP rarely originates in the gastric fundus, but occasionally results in serious consequence, such as massive gastrointestinal bleeding. It is important to recognize IFP because it responds favorably to operation with no relapse or metastasis.
CONCLUSION
In the differential diagnosis of alimentary hemorrhage of uncertain etiology, gastric IFP should be considered. For huge gastric IFP, laparoscopic therapy is an apt choice.
Keywords: Inflammatory fibroid polyp, Stomach, Laparoscopy, Alimentary hemorrhage
1. Introduction
IFPs are unusual benign lesions originating from submucosa of the gastrointestinal tract. The most prominent features of IFPs are semi-pedunculated protrusions covered by normal mucosa.1 The most common site of IFP is the gastric antrum, followed by the small bowel, but very rare in the gastric fundus. Clinical manifestations of IFPs usually include intestinal obstruction, intussusception, abdominal pain, nausea and vomiting, but rare massive digestive tract hemorrhage. The treatment of IFP depends on its size, location and biological property. We herein report a very rare case with huge gastric IFP, at the posterior wall of the gastric fundus, presenting with serious hematemesis and hematochezia.
2. Case presentation
A 78-year-old female patient with massive hematemesis and hematochezia for two days, without abdominal pain or abdominal distension, was admitted to Peking University Cancer Hospital, Beijing, China. The physical examination revealed the body temperature was 36.4 °C, blood pressure was 95/75 mmHg, resting heart rate was 100 beats/min, respiratory rate was 20 breaths/min and abdomen was flat, no palpable mass. Routine hematological examination showed hemoglobin and hematocrit were 85.0 g/dL (reference range 110–150 g/L) and 33.7% (reference range 37.0–49.0), respectively. A gastroscopy revealed a huge semi-pedunculated polyp (11 cm) with smooth surface, which originated at the posterior wall of the gastric fundus. The histology of specimens obtained with biopsy forceps showed inflammatory exudate, granulation tissue with necrosis and focal atypical hyperplasia. Abdominal computed tomography (CT) demonstrated a low-density mass, with slight peripheral enhancement (Fig. 1, arrow). A colonoscopy revealed no obvious lesions, so the gastric polyp was suspected to be the cause of bleeding. Because of the giant dimension and the possibility of other malignant lesions, so we carried out LAPG and identified a depressed ulcer lesion at the base of the tumor (Fig. 2, arrow). Postoperative histopathologic evaluation revealed proliferation of a large number of spindle cells and infiltration of many lymphocytes, mainly including plasma cells and eosinophils, as well as extensive thick-walled capillary vessels, compatible with an inflammatory fibroid polyp (Fig. 3). Immunohistochemistry showed that SMA, CD34, Desmin and Calponin were positive, but CD117, CD21, CD35 and S-100 were negative. With the treatment of LAPG, the above clinical symptoms disappeared. The patient was discharged after operation one week without any complication.
Fig. 1.
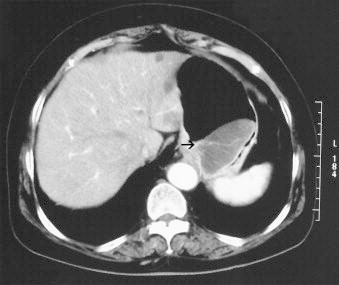
Tumor appearance of abdominal computed tomography. An oval and sharply circumscribed low-density mass, with slight peripheral enhancement and a blood vessel through the mass (arrow).
Fig. 2.
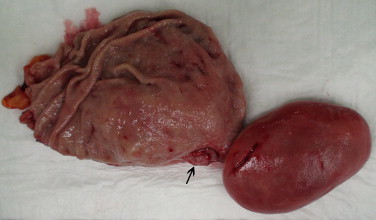
Postoperative specimen. The tumor was completely resected without any complications. The 11 × 6.5 cm sized polyp with a depressed ulcer at the base of the tumor (arrow).
Fig. 3.
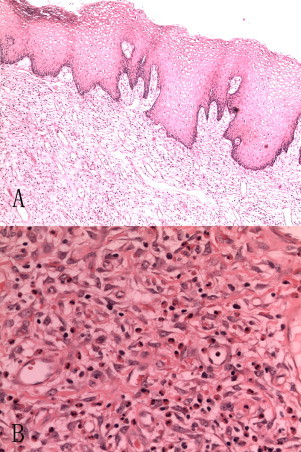
Microscopic features. (A) Surface coating of keratinized squamous epithelium, a large number of thin-walled capillary vessels and loose fibrous connective tissue (H&E, original magnification ×40). (B) Infiltration of lymphocytes in the stroma, mainly including plasma cells and eosinophils (H&E, original magnification ×200).
3. Discussion
IFPs are rare mucosal or submucosal lesions of the digestive tract that follow a benign course. They were first described as “gastric submucosal granuloma with eosinophilic infiltration” by Vanek in 1949.2 The term of “IFP” was finally made by Helwig and Ranier in 1953.3
Clinical manifestations depend on the tumor location and the size, usually including intestinal obstruction, intussusception,4 abdominal pain, nausea and vomiting and constipation, iron deficiency anemia and hyperpyrexia,5 but rare massive digestive tract hemorrhage.6 Coincidentally, the present rare huge gastric IFP brought out massive gastrointestinal bleeding. So, in the differential diagnosis of alimentary hemorrhage of uncertain etiology, gastric IFP should be considered.
The typical endoscopic features of IFPs are smooth sessile or pedunculated polyps with exudates and white spots. It is difficult to give a definite diagnosis before operation because of their volatile position and variable clinical appearances. The final diagnosis relies on the pathological findings; however, the histological findings of the biopsy specimen are usually hard to diagnose.7–9 Besides, differentiation is very difficult, especially between IFPs and gastrointestinal stromal tumors (GISTs).10 Interestingly, our case was suspected to be GIST before surgery, but the immunohistochemical result revealed spindle cells expressing CD34, smooth muscle actin(SMA), Desmin and Calponin, but not CD 117. Some scholars have confirmed that the proliferating stromal cells in IFPs were diffusely positive for CD34, SMA and Calponin. They also concluded that IFPs were unrelated to GISTs.11
Most IFPs are smaller than 5 cm,12,13 but the size of present gastric IFP is up to 11 cm. The most common site is gastric antrum, followed by the small bowel, other locations such as rectum,14 colon,15 esophagus and duodenum12 in the previous literature, but very rare at the upper part of the stomach.
Although the pathogenesis of IFPs largely remain not to be elucidated, there are many causes supposed to be associated with IFPs. First, the IFP could be a result of extreme reaction of the body to trauma or a localized variant of eosinophilic gastroenteritis. Moreover, inflammatory stimuli such as bacterial, chemical, metabolic or traumatic factors are also related with IFPs.3 Pantanowitz et al. deemed that the proliferating stromal cells were of dendritic cell origin with possible myofibroblastic differentiation.11
Exploratory laparotomy is frequently recommended as a treatment for IFPs.16 Some authors considered submucosal dissection as useful for treatment of small submucosal tumor, usually by endoscopy.14,17–19 However, if the tumor is large or malignant lesion can’t be excluded, laparoscopic assisted or conventional open surgery should be considered. After complete resection, inflammatory fibroid polyps usually do not recur and metastasize, making any other adjunct therapies unnecessary.
4. Conclusion
We report a rare case with massive digestive tract hemorrhage caused by the huge IFP at the gastric fundus, which was successfully treated by LAPG. Based on the results in the present case and reviewed literatures, uncommon massive gastrointestinal bleeding may be caused by digestive tract IPFs. Besides, laparoscopic surgery is appropriate and useful treatment for patients with giant gastric IPFs.
Conflict of interest statement
None.
Funding
This study was supported by the grants from the National Natural Science Foundation of China (No. 81272766).
Ethical approval
Not applicable.
Author contributions
Chenhai Zhang wrote the manuscript. Chenhai Zhang, Ming Cui, Jiadi Xing and Xiangqian Su participated in the diagnosis and treatment of present case. Yunfei Shi carried out pathological analysis. All authors approved the final manuscript.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Key learning points
IFPs rarely originate in the gastric fundus, but occasionally result in serious consequence, such as massive gastrointestinal bleeding. So, in the differential diagnosis of alimentary hemorrhage of uncertain etiology, gastric IFP should be considered. For huge gastric IFP, laparoscopic therapy is an apt choice.
Contributor Information
Chenghai Zhang, Email: chenghai.zlyy@gmail.com.
Ming Cui, Email: doctor_cui2008@sina.com.
Jiadi Xing, Email: Jiadixing@hotmail.com.
Yunfei Shi, Email: shiyunfei@126.com.
Xiangqian Su, Email: suxiangqian@bjmu.edu.cn, suxiangqian@gmail.com.
References
- 1.Matsushita M., Uchida K., Nishio A. Endoscopic and EUS features of gastric inflammatory fibroid polyps. Gastrointest Endosc. 2009;69:188. doi: 10.1016/j.gie.2008.04.048. (author reply 188–9) [DOI] [PubMed] [Google Scholar]
- 2.Vanek J. Gastric submucosal granuloma with eosinophilic infiltration. Am J Pathol. 1949;25:397–411. [PMC free article] [PubMed] [Google Scholar]
- 3.Helwig E.B., Ranier A. Inflammatory fibroid polyps of the stomach. Surg Gynecol Obstet. 1953;96:335–367. [PubMed] [Google Scholar]
- 4.Akbulut S. Intussusception due to inflammatory fibroid polyp: a case report and comprehensive literature review. World J Gastroenterol. 2012;18:5745–5752. doi: 10.3748/wjg.v18.i40.5745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.He H.Y., Shen Z.B., Fang Y. Bleeding and hyperpyrexia in an adult with gastric inflammatory fibroid polyp. Chin Med J (Engl) 2013;126:2594. [PubMed] [Google Scholar]
- 6.Gutu E., Ghidirim G., Misin I. Bleeding gastric inflammatory fibroid polyp (Vanek's tumor) Chirurgia (Bucur) 2010;105:137–140. [PubMed] [Google Scholar]
- 7.Hirasaki S., Endo H., Nishina T. Gastric cancer concomitant with inflammatory fibroid polyp treated with endoscopic mucosal resection using an insulation-tip diathermic knife. Intern Med. 2003;42:259–262. doi: 10.2169/internalmedicine.42.259. [DOI] [PubMed] [Google Scholar]
- 8.Hirasaki S., Tanimizu M., Tsubouchi E. Gastritis cystica polyposa concomitant with gastric inflammatory fibroid polyp occurring in an unoperated stomach. Intern Med. 2005;44:46–49. doi: 10.2169/internalmedicine.44.46. [DOI] [PubMed] [Google Scholar]
- 9.Chongsrisawat V., Yimyeam P., Wisedopas N. Unusual manifestations of gastric inflammatory fibroid polyp in a child. World J Gastroenterol. 2004;10:460–462. doi: 10.3748/wjg.v10.i3.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Calabuig-Farinas S., Lopez-Guerrero J.A., Ribera M.J. Inflammatory fibroid polyp of the small bowel with a mutation in exon 12 of PDGFR alpha. Virchows Arch. 2009;454:327–331. doi: 10.1007/s00428-008-0715-5. [DOI] [PubMed] [Google Scholar]
- 11.Pantanowitz L., Antonioli D.A., Pinkus G.S. Inflammatory fibroid polyps of the gastrointestinal tract: evidence for a dendritic cell origin. Am J Surg Pathol. 2004;28:107–114. doi: 10.1097/00000478-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Wysocki A.P., Taylor G., Windsor J.A. Inflammatory fibroid polyps of the duodenum: a review of the literature. Dig Surg. 2007;24:162–168. doi: 10.1159/000102099. [DOI] [PubMed] [Google Scholar]
- 13.Liu T.C., Lin M.T., Montgomery E.A. Inflammatory fibroid polyps of the gastrointestinal tract: spectrum of clinical, morphologic, and immunohistochemistry features. Am J Surg Pathol. 2013;37:586–592. doi: 10.1097/PAS.0b013e31827ae11e. [DOI] [PubMed] [Google Scholar]
- 14.Shimura T., Kataoka H., Sasaki M. Rectal inflammatory fibroid polyp resected with endoscopic submucosal dissection. Intern Med. 2008;47:2029–2031. doi: 10.2169/internalmedicine.47.1357. [DOI] [PubMed] [Google Scholar]
- 15.Hirasaki S., Matsubara M., Ikeda F. Inflammatory fibroid polyp occurring in the transverse colon diagnosed by endoscopic biopsy. World J Gastroenterol. 2007;13:3765–3766. doi: 10.3748/wjg.v13.i27.3765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akbulut S., Sevinc M.M., Cakabay B. Giant inflammatory fibroid polyp of ileum causing intussusception: a case report. Cases J. 2009;2:8616. doi: 10.4076/1757-1626-2-8616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odashima M., Otaka M., Nanjo H. Hamartomatous inverted polyp successfully treated by endoscopic submucosal dissection. Intern Med. 2008;47:259–262. doi: 10.2169/internalmedicine.47.0360. [DOI] [PubMed] [Google Scholar]
- 18.Yoon D.W., Lee B.J., Lee J.H. A case of giant inflammatory ileal polyp removed by double-balloon enteroscopy. Clin Endosc. 2012;45:198–201. doi: 10.5946/ce.2012.45.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ergun M., Zengin N., Kayacetin E. Loop observe and snare technique for endoscopic resection of a gastric inflammatory fibroid polyp. Endoscopy. 2012;44(Suppl 2 UCTN):E86–E87. doi: 10.1055/s-0031-1291640. [DOI] [PubMed] [Google Scholar]


