Abstract
A 53-year-old male patient presented with low back pain radiating to both lower limbs for 2 years and urinary incontinence for 2 months. He had swelled over his lower back since birth. The neurological examination revealed a decreased perianal sensation. Local examination of the lumbar swelling showed a brilliantly transilluminant, cystic midline swelling in the lumbar area with underlying spina bifida. Magnetic resonance imaging revealed a low-lying conus at L3 level associated with spina bifida at L5 and a meningocoele sac. The patient underwent excision of the meningocoele and detethering of cord by extirpation of hypertrophied filum terminale. The patient had an immediate relief of his symptoms. At 3 month follow-up the lumbar wound had healed well, and there was a significant improvement in the perianal hypoesthesia. The adult presentation of a congenital meningocoele and spinal dysraphism is rare, especially in the fifth decade. The possible causes of this delayed presentation are analyzed, and the relevant literature on the subject is presented.
Keywords: Adult meningocoele, spinal dysraphism, tethered cord
INTRODUCTION
Spinal dysraphism manifests as an incomplete fusion of the neural arch, varying from the occult to more severe open neural tube defects (NTD). Meningocele is the simplest form of open NTD characterized by cystic dilatation of meninges containing cerebrospinal fluid without any neural tissue. The natural course of meningocele has been rarely discussed.[1] The majority of meningocoeles are identified and treated perinatally. We describe the delayed presentation of a meningocoele in adulthood with relevant review of the literature.
CASE REPORT
A 53-year-old male had presented with complaints of low backache for 2 years radiating to both lower limbs and difficulty in walking. The patient had urinary incontinence for 2 months. He had a cystic swelling in the lower back since birth. The swelling was asymptomatic and hence he had not sought any medical advice for the same. On neurological examination, the patient had decreased perianal sensation with normal anal reflex. Local examination revealed a 10 cm × 8 cm × 5 cm cystic midline swelling in the lumbosacral region. The skin over the swelling was thickened, but normal [Figure 1]. The swelling was brilliantly transilluminant. The magnetic resonance images showed a low lying conus, spina bifida defect at L5 level and protrusion of the meningocoele sac [Figures 2 and 3]. The urodynamic studies indicated internal sphincter abnormalities with normal detrusor muscle patterns. The somato-sensory evoked potential (SSEP), electromyographic and nerve conduction studies of lower limbs was normal. Due to the progressive nature of the symptoms, the patient was offered surgery. The patient underwent excision of the meningocoele sac and detethering of cord by extirpation of hypertrophied filum terminale. The patient had an immediate relief of lower limb pain postoperatively. At 3 months follow-up the lumbar wound had healed well, and there was a significant improvement in the perianal hypoesthesia and urinary incontinence.
Figure 1.

Clinical photograph of the patient showing a midline lumbosacral swelling with normal skin covering it
Figure 2.

T1-weighted saggital magnetic resonance image shows a low lying conus associated with lumbar meningocoele
Figure 3.
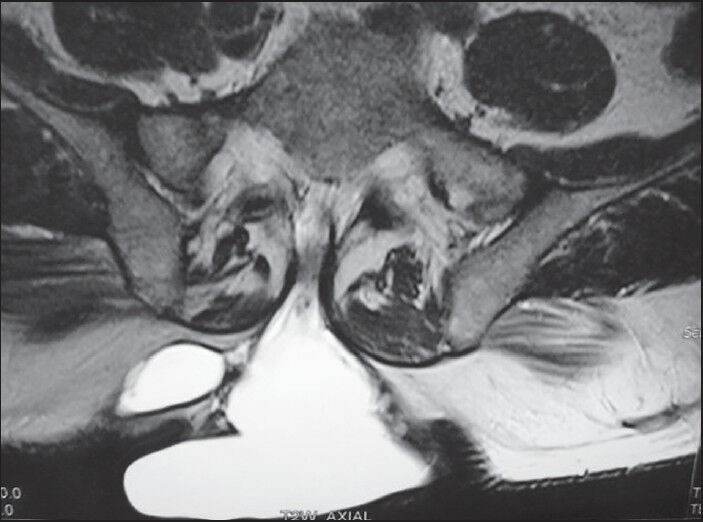
T2-weighted axial magnetic resonance image demonstrates spina bifida defect and a large meningocoele sac
DISCUSSION
Spinal dysraphism represents a spectrum of congenital anomalies that cause rostrocaudal traction on the spinal cord. The resulting constellation of symptoms includes varying combinations of pain, neurological deficits and bowel and bladder dysfunction. This syndrome is referred as tethered cord syndrome.[2] Adult meningocoele is very rare cause of tethered cord syndrome.
The degree of traction of the conus is thought to determine the age of onset of symptoms in cases of marked tethering and severe stretching of the conus, neurological symptoms appear in infancy or early childhood. Minimal tethering may remain subclinical until adulthood. 29% of patients with symptomatic tethered cord, have been found to be older than 35 years The mechanism of late onset of symptoms is explained by the cumulative effect of repeated cord traction by various postures.[2] Yamada et al. stated that neurological dysfunction in patients with tethered cord correlates with mitochondrial anoxia within the conus.[3] It has been suggested that the longitudinal stress within the spinal cord may be transmitted more distally along the lateral columns as they are fixed by dentate ligaments. Direct trauma to the lumbosacral region may precipitate the symptoms causing deformation of the marginally functioning neuronal elements within the stretched cord.[1] The bending movements, lithotomy position during childbirth, movements occurring during motor accidents may precipitate symptoms.[2] The narrowing of the spinal canal by lumbar spinal stenosis and disc prolapse and resultant increased tension in a congenitally tethered spinal cord may also precipitate symptoms.[1] In the present case, the patient had additional degenerative lumbar spine disease.
Neural tube defects are the second most common type of birth defect after congenital heart defects, and myelomeningocele is the most common form of neural tube defect, accounting for greater than 90% of cases of spina bifida. A posterior meningocele, however, represents the least common form of neural tube defect. The incidence of NTD ranges from 1.0 to 10.0/1,000 live births divided into two major categories of equal frequency: Anencephaly and spina bifida. Meningocele results from a developmental failure in the caudal end of the neural tube, resulting in a sac containing cerebrospinal fluid, meninges, and overlying skin. The development of the spinal cord is normal, and there is usually no associated neurologic deficit, although there is an association with a tethered spinal cord.[4] Although anterior sacral meningocoele and dorsal cervical meningocoele are commonly reported, very few cases of adult dorsal lumbosacral meningocoele have been reported, after first description of by Chambers and Revilla in 1948.[5] Most of these cases described are in between 20 and 30 years age group except for 3 patients. These patients include the present case and those reported by Chambers and Revilla, who was 53 years old and Gok et al. who was 48 years old[1,4,5,6,7,8] [Table 1]. Out of the 8 reported patients, including the present case, seven patients were males.
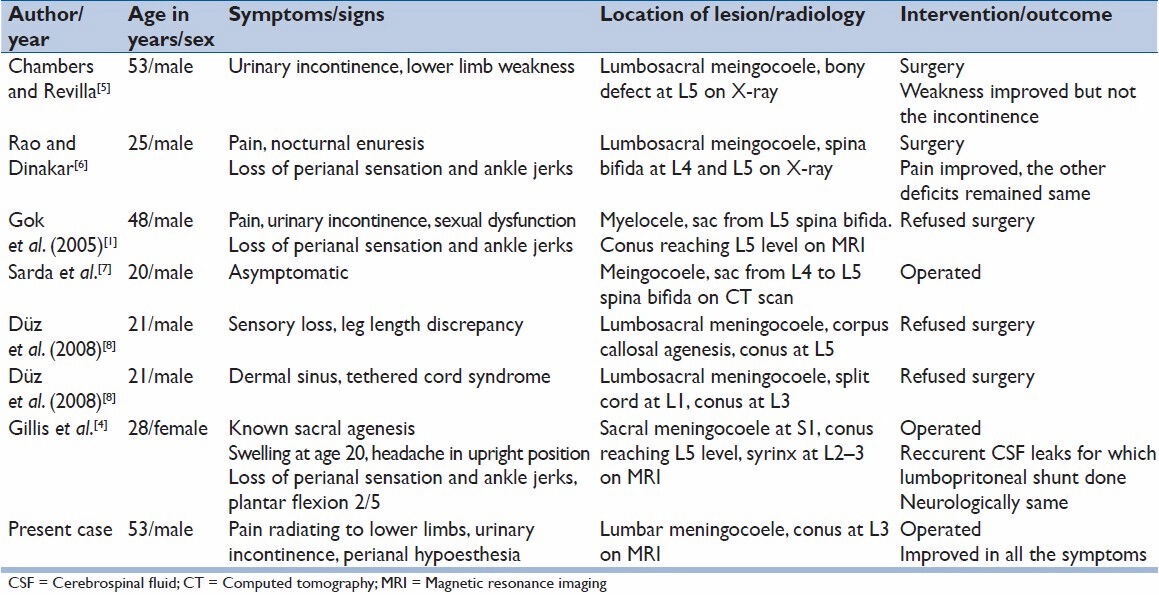
Table 1.
Reported cases of adult meningocoele in English literature
An SSEP examination is more sensitive than clinical testing for detection of early and subtle neurological deficits in patients with spinal cord lesion. Abnormal SSEP is a clear indication of spinal pathology. However, not all spinal pathologies are associated with abnormalities in SSEP. In the reported patient, SSEP was found to be within normal range. Preoperative urodynamic investigation is strongly recommended, even if the patient is continent. Sympathetic innervation is often impaired first in tethered cord syndrome, resulting in nonfunctioning internal urethral sphincter, which characteristically causes postvoiding dripping and stress incontinence as in our case. At latter stages, it usually causes mixed abnormalities of parasympathetic, sympathetic and somatic pathways.[1]
Although a dilemma is present about the surgical indication of asymptomatic patients, it has been recommended that the patient should be operated as soon as symptoms appear or progress because in the majority of patients stabilization of the disease is achieved by detethering of the cord.[1] The present case became symptom-free after excision of the meningocoele and detethering of the cord.
CONCLUSION
We present a rare case of delayed presentation of lumbar meningocele associated with tethered cord in an adult patient. Surgical detethering and repair of the meningocoele sac offers the best outcome to these patients even at such a late presentation in adulthood.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gok HB, Ayberk G, Tosun H, Seckin Z. Clinical course and evaluation of meningocele lesion in adulthood: A case report. Neuroanatomy. 2005;4:52–4. [Google Scholar]
- 2.Iskandar BJ, Fulmer BB, Hadley MN, Oakes WJ. Congenital tethered spinal cord syndrome in adults. J Neurosurg. 1998;88:958–61. doi: 10.3171/jns.1998.88.6.0958. [DOI] [PubMed] [Google Scholar]
- 3.Yamada S, Zinke DE, Sanders D. Pathophysiology of “tethered cord syndrome”. J Neurosurg. 1981;54:494–503. doi: 10.3171/jns.1981.54.4.0494. [DOI] [PubMed] [Google Scholar]
- 4.Gillis CC, Bader AA, Boyd M. A tail of sacral agenesis: Delayed presentation of meningocele in sacral agenesis. Eur Spine J. 2013;22(Suppl 3):S311–6. doi: 10.1007/s00586-012-2347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chambers JW, Revilla AG. Unusual case of meningocele in an adult. J Neurosurg. 1948;5:316–20. doi: 10.3171/jns.1948.5.3.0316. [DOI] [PubMed] [Google Scholar]
- 6.Rao SB, Dinakar I. Lumbosacral meningocele in an adult. A case report. J Postgrad Med. 1971;17:91–2. [PubMed] [Google Scholar]
- 7.Sarda D, Lohiya S, Jawandiya V, Gajbhiye R. Meningocoele in an adult - Case reports. Bombay Hosp J. 2006;48:505–6. [Google Scholar]
- 8.Düz B, Gocmen S, Secer HI, Basal S, Gönül E. Tethered cord syndrome in adulthood. J Spinal Cord Med. 2008;31:272–8. doi: 10.1080/10790268.2008.11760722. [DOI] [PMC free article] [PubMed] [Google Scholar]


