Abstract
INTRODUCTION
An infiltration of urological organs is found in 5–10% of patients with colorectal carcinoma. Total pelvic exenteration is the standard procedure for locally advanced rectal cancer. In selected patients with rectal cancer involving the prostate or seminal vesicles, the bladder can be preserved and en bloc radical prostatectomy with abdominoperineal rectal resection can be performed. We report two patients who treated with this combined approach.
PRESENTATION OF CASE
Two patients with symptoms of rectal bleeding and pelvic pain were investigated. Colonoscopy demonstrated a tumor in the lower rectum. Biopsies revealed adenocarcinoma. Both pelvic MRI and endorectal ultrasound showed tumors that invaded the prostate and the seminal vesicles directly but without invasion of the bladder. After neoadjuvant chemoradiation, combined radical prostatectomy and abdominoperineal amputation was performed. None has developed local recurrence, but one of them was operated on for a single lung metastasis. After a follow-up of 28 and 20 months, respectively, the patients are alive without evidence of local recurrence or distant disease.
DISCUSSION
This procedure obviates the need for urinary diversion without compromising the local tumor control. Intraoperative and postoperative diagnostic difficulties, and clinical aspects in relation to postoperative anastomotic leak and survival of patients are discussed.
CONCLUSION
En bloc radical prostatectomy and proctosigmoidectomy is feasible in selected patients with rectal cancer and invasion limited to the prostate or seminal vesicles because it provides good local tumor control and significantly improves the patient's quality of life in comparison to total pelvic exenteration.
Keywords: Rectal cancer, Locally advanced rectal cancer, Radical prostatectomy, Abdominoperineal resection
1. Introduction
The incidence of colorectal carcinoma is very high in the Western world where it is the second commonest cause of cancer death and fourth commonest cause of death from cancer worldwide.1 During surgery for colorectal carcinoma, an infiltration of adjacent urological organs is found in 5–10% of all cases and this rate may rise to 50% when considering patients with locally advanced tumors (T4) at presentation.2 Total pelvic exenteration and its modifications are surgical options for the treatment of locally advanced rectal cancer.3 Total pelvic exenteration may involve en bloc removal of the rectum, bladder, prostate or ureters since it is essential to create clear margins if the procedure is to be curative. As a result, patients often require double stomas and compromises quality of life severely, despite achieving acceptable locoregional control.
A combined radical prostatectomy and proctosigmoidectomy as an alternative to total pelvic exenteration for patients with rectal carcinoma with isolated extension to the prostate or seminal vesicles has been recommended, because it fulfils the oncological surgical requirements and carries out a significant improvement in the patient’s quality of life in comparison to total pelvic exenteration.4 Owing to the very scarce published literature we present two case reports of patients treated with combined radical prostatectomy and abdominoperineal excision of the rectum with reconstruction of the urinary tract by urethrovesical anastomosis.
2. Presentation of case
2.1. Patient A
A 61-year-old male with no past medical history presented with rectal bleeding and perineal discomfort that had initiated nine months before and was associated with asthenia and weight loss in the last 3 months. A large lesion in the lower third of the rectum was palpable on rectal examination, close to the dentate line. Colonoscopy showed a 7-cm tumor on the right lateral rectal wall, distant 2 cm from the anal verge. Biopsies revealed adenocarcinoma. Abdominal CT scan demonstrated a circumferential thickening of the low rectum. Pelvic MRI and endorectal ultrasound revealed a rectal tumor infiltrating the perirectal fat and with invasion of the prostate and the right seminal vesicle but without bladder involvement (Fig. 1). After the diagnosis, the patient started with neoadjuvant radiochemotherapy. Eight weeks after the end of neoadjuvant therapy, a surgical treatment was performed. Surgery consisted in a combined abdominoperineal resection and radical prostatectomy with urethrovesical anastomosis for en bloc removal of locally invasive carcinoma of the rectum. Also, a colostomy was created. Pathologic examination revealed a poorly differentiated adenocarcinoma of the rectum invading the prostatic parenchyma (Fig. 2). Lymph nodes were negative for cancer. The tumor was included into stage II (ypT4b N0 M0). A pelvic abscess was detected in the postoperative period, but a cystography did not show any extravasation of contrast from the urethrovesical anastomosis. The abscess completely resolved with antibiotherapy and prolonged vesical catheterization. After discharge, the patient received outpatient chemotherapy. At 18 months after surgery, a chest CT scan revealed a left upper lobe solitary pulmonary nodule, and a fine-needle aspiration biopsy showed its metastatic nature. Subsequently, the patient underwent pulmonary segmentectomy. A histopathological examination confirmed the diagnosis of pulmonary metastasis from rectal cancer. Once again, the patient received outpatient chemotherapy. At present, after 28 months of rectal surgery and after 11 months of surgery for lung metastasis, the patient is alive without evidence of local recurrence or distant disease.
Fig. 1.
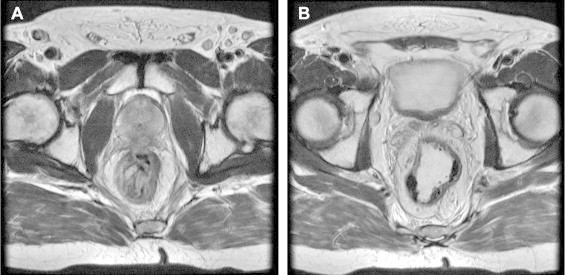
Axial T2 pelvic MRI demonstrates (A) infiltration of the prostate and (B) right seminal vesicle invasion (patient A).
Fig. 2.
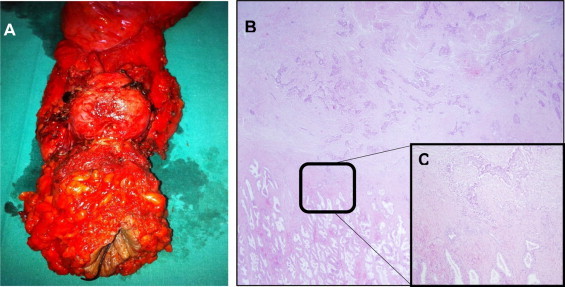
(A) Surgical specimen showing en bloc resection of the prostate and the rectum. (B) Histopathology confirmed a rectal adenocarcinoma infiltrating the prostate (H&E stain, 20×). (C) Cancer cells invading the prostate (H&E stain, 100×) (patient A).
2.2. Patient B
A 51-year-old male with a past medical history of hypertension was admitted to the hospital with rectal bleeding, pelvic pain and constipation alternating with diarrhea lasting for two months. The rectal examination revealed an ulcerated mass just above the dentate line. Colonoscopy showed a vegetant and ulcerated mass circumferentially involving the rectum, distant 3–4 cm from the anal verge, and 5-cm long. Microscopic examination revealed adenocarcinoma. An irregular and concentric thickening in lower third of the rectum was seen in abdominal CT scan. Endorectal ultrasound identified a circumferential rectal malignant lesion starting at level of the prostate and extending beyond the seminal vesicles. Pelvic RMI showed a 5-cm rectal mass located to 3.5 cm from de anal verge, with a significant mucinous component and involvement of mesorectal fascia and the posterior aspect of the prostate (Fig. 3). The case was discussed by the multidisciplinary oncological team who decided that chemoradiation followed by surgical excision should be performed. Seven weeks after completion of neoadjuvant therapy the patient was operated on. Surgery consisted of simultaneous abdominoperineal amputation and radical prostatectomy with urethrovesical anastomosis for locally advanced rectal cancer. A colostomy was constructed to complete the procedure. The postoperative histopathological findings were in accordance with the diagnosis of well-differentiated mucinous adenocarcinoma with evident perirectal fat infiltration and presence of tumor cells in periprostatic adipose tissue (Fig. 4). Lymph nodes examined were free of cancer. The tumor was classified as ypT4b N0 M0 and was included into stage II. After surgery, the patient had a pelvic fluid collection which was treated with antibiotics until complete resolution and prolonged vesical catheterization. A postoperative cystography demonstrated no extravasation of contrast from the urethrovesical anastomosis. After hospitalization, the patient received in the hospital outpatient setting. At present, after 20 months of surgery, the patient remains tumor-free and without evidence of local recurrence.
Fig. 3.
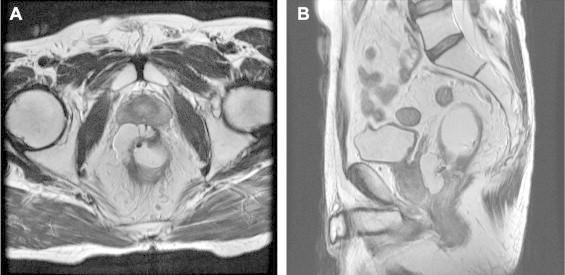
Axial (A) and sagittal (B) T2 pelvic MRI revealing prostatic involvement by cancer of the rectum (Patient B).
Fig. 4.
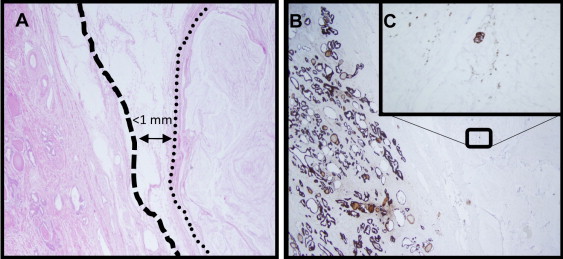
(A) Mucin pools are observed (area bounded by a dotted line) less than 1 mm from the prostatic capsule (dashed line) (H&E stain, 50×). (B) Immunostaining was positive for CK AE1/AE3 demonstrating the presence of the tumor cells within collections of mucin (20× magnification). (C) Positive staining for CK 20 confirmed that the tumor cells belong to a rectal adenocarcinoma (400× magnification) (Patient B).
3. Discussion
En bloc excision of locally invasive rectal cancer in the absence of extrapelvic metastases can be curative, and total pelvic exenteration is the standard procedure performed for patients with this type of rectal cancer, to achieve negative surgical margins and to avoid intra-abdominal dissemination. This major procedure carries a high morbidity and mortality, with a substantial negative impact on long-term quality of life.5,6 In locally advanced rectal cancer, reported rates of 5-year overall survival after exenterative surgery are between 43% and 54%.3 In the 1960s, the possibility to perform a prostatectomy, and at the same time a rectal abdominoperineal amputation was suggested.7 This procedure remained without precise indication until 1993, when Campbell et al.4 reported the radical prostatectomy in conjunction with low anterior resection for two patients with rectal cancer invading into the prostate. Since then, few references about this combined approach have been reported in the literature. Thus, until 2010 only 18 patients had been described with the use of combined radical prostatectomy and proctosigmoidectomy for en bloc removal of locally invasive cancer of the rectum.8
Currently, although preoperative imaging for staging of rectal cancer provide a high diagnostic accuracy,9 to determine if limited en bloc resection of invasive rectal cancer is feasible may be a problem, since discrimination between cancerous involvement and inflammatory adhesions is very difficult intraoperatively. In this regard, some authors have postulated careful intraoperative examination using frozen sections to evaluate the extent of pelvic invasion.10 However, intraoperative decisions based on frozen sections may carry some risk, since tumor exposure can occur and convert a potentially curative resection into a non-curative resection. In general, most authors recommend en bloc radical prostatectomy if involvement of the prostate for rectal cancer is suspected, since the dissection between the rectum and prostate clearly diminishes the survival.2,11 The diagnostic difficulty cannot be only preoperative, but may also be evident during pathological examination, as occurred in our second patient (case B), in which was even necessary to use immunohistochemistry to demonstrate the presence of cancer cells in the periprostatic adipose tissue.
In combined radical prostatectomy and rectal resection for en bloc removal of invasive rectal cancer, the bladder can be preserved avoiding the need of an urostoma and improving quality of life. Furthermore, there is lesser postoperative morbidity than after total pelvic exenteration.12,13 Urinary leakage at the urethrovesical anastomosis is one of the most important short-term complications after this simultaneous resection which can occur between 33% and 50% of cases.8,12 The anastomotic leaks are probably due to preoperative irradiation and the lack of the adjacent tissues surrounding the portion of the anastomosis when the rectum has been removed, meaning less blood flow at the anastomosis site, or both.12,14 Although postoperative presacral collections occurred in our two patients, it was not possible to demonstrate contrast extravasation during cystography in any of them.
Many reports about patients treated with en block radical prostatectomy for locally advanced rectal carcinoma describe isolated cases and only reflect short-term follow-up evaluation.11,14,15 In the studies reported by Saito et al.10 and Balbay et al.,13 which include a large number of patients and longer follow-up analysis, it is mentioned that when the rectal cancer invades just the prostate or seminal vesicles, combined radical prostatectomy and rectal resection is feasible and preferable if the tumor can be removed en bloc because it provides good local control without sacrificing survival. There was no evidence of local recurrence in none of our patients. However, one of them developed distant metastatic disease during follow-up.
4. Conclusions
En bloc radical prostatectomy and proctosigmoidectomy is a viable alternative to total pelvic exenteration in selected patients with rectal cancer and invasion limited to the prostate or seminal vesicles because fulfils the principles of surgical oncology without compromising the local tumor control and significantly improves the patient's quality of life in comparison to total pelvic exenteration.
Conflict of interest
There was no conflict of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patients for publication of these case reports and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
No identifying details are included.
Author contributions
Daniel Fernández-Martínez: design and writing the paper, Antonio Rodríguez-Infante: data collection, Elsa Castelo-Álvarez: data collection, Iván Fernández-Vega: histopathological examination, Miguel Suárez-Hevia: urologic surgeon collaborator, Nuria Truán-Alonso: data analysis and critical review of paper, Ricardo F. Baldonedo-Cernuda: data analysis and critical review of paper, José A. Álvarez-Pérez: design, writing, and final approval of paper, Herminio Sánchez-Farpón: data analysis and critical review of paper. All authors have read and approved the final manuscript.
Key learning points.
-
•
En bloc radical prostatectomy and proctosigmoidectomy is feasible in patients with locally advanced rectal cancer because it avoids performing an urostoma without compromising the local tumor control.
Contributor Information
Daniel Fernández-Martínez, Email: cibea06@hotmail.com.
Antonio Rodríguez-Infante, Email: rointonio23@hotmail.com.
Elsa Castelo-Álvarez, Email: misao_ce@hotmail.com.
Iván Fernández-Vega, Email: ivan_fernandez_vega@hotmail.com.
Miguel Suárez-Hevia, Email: hevia.urologo@gmail.com.
Nuria Truán-Alonso, Email: nuriatru@telecable.es.
Ricardo F. Baldonedo-Cernuda, Email: baldonedo@telecable.es.
José A. Álvarez-Pérez, Email: josealvar@telecable.es.
Herminio Sánchez-Farpón, Email: hfarpon@hotmail.com.
References
- 1.Jemal A., Siegel R., Ward E., Hao Y., Xu J., Thun M.J. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–249. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Stief C.G., Jonas U., Raab R. Long-term follow-up after surgery for advanced colorectal carcinoma involving the urogenital tract. Eur Urol. 2002;41:546–550. doi: 10.1016/s0302-2838(02)00062-3. [DOI] [PubMed] [Google Scholar]
- 3.Pawlik T.M., Skibber J.M., Rodriguez-Bigas M.A. Pelvic exenteration for advanced pelvic malignancies. Ann Surg Oncol. 2006;13:612–623. doi: 10.1245/ASO.2006.03.082. [DOI] [PubMed] [Google Scholar]
- 4.Campbell S.C., Church J.M., Fazio V.W., Klein E.A., Pontes J.E. Combined radical retropubic prostatectomy and proctosigmoidectomy for en bloc removal of locally invasive carcinoma of the rectum. Surg Gynecol Obstet. 1993;176:605–608. [PubMed] [Google Scholar]
- 5.Law W.L., Chu K.W., Choi H.K. Total pelvic exenteration for locally advanced rectal cancer. J Am Coll Surg. 2000;190:78–83. doi: 10.1016/s1072-7515(99)00229-x. [DOI] [PubMed] [Google Scholar]
- 6.Palmer G., Martling A., Lagergren P., Cedermark B., Holm T. Quality of life after potentially curative treatment for locally advanced rectal cancer. Ann Surg Oncol. 2008;15:3109–3117. doi: 10.1245/s10434-008-0112-y. [DOI] [PubMed] [Google Scholar]
- 7.Holund T. Routine prostatectomy in association with amputation of the rectum. Ugeskr Laeger. 1966;128:502. [PubMed] [Google Scholar]
- 8.Castro L., Kesley R., Correa J.H., Stoduto G., Barros A., Tsunoda A. Alternative to total pelvic exenteration in locally advanced rectal cancer: en bloc radical prostatectomy. Appl Cancer Res. 2010;30:295–299. [Google Scholar]
- 9.Karantanas A.H., Yarmentis S., Papanikolaou N. Gourtsoyiannis: preoperative imaging staging of rectal cancer. Dig Dis. 2007;25:20–32. doi: 10.1159/000099167. [DOI] [PubMed] [Google Scholar]
- 10.Saito N., Suzuki T., Sugito M., Ito M., Kobayashi A., Tanaka T. Bladder-sparing extended resection of locally advanced rectal cancer involving the prostate and seminal vesicles. Surg Today. 2007;37:845–852. doi: 10.1007/s00595-007-3492-x. [DOI] [PubMed] [Google Scholar]
- 11.Herranz Amo F., Muñoz Jiménez F., Subirá Ríos D., Gómez Espí M., Calvo Manuel F.A. Preservation of the bladder in rectal cancer with prostatic invasion. Actas Urol Esp. 2004;28:447–451. doi: 10.1016/s0210-4806(04)73108-3. [DOI] [PubMed] [Google Scholar]
- 12.Wiig J.N., Waehre H., Larsen S.G., Braendengen M., Giercksky K.E. Radical prostatectomy for locally advanced primary or recurrent rectal cancer. Eur J Surg Oncol. 2003;29:455–458. doi: 10.1016/s0748-7983(03)00030-1. [DOI] [PubMed] [Google Scholar]
- 13.Balbay M.D., Slaton J.W., Trane N., Skibber J., Dinney C.P.N. Rationale for bladder-sparing in patients with locally advanced colorectal carcinoma. Cancer. 1999;86:2012–2016. doi: 10.1002/(sici)1097-0142(19991201)86:11<2212::aid-cncr6>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 14.Sugita H., Egami H., Yokoyama Y., Suyama K., Ogawa M. Combined radical retropubic prostatectomy and abdominoperineal excision of the rectum for locally invasive rectal cancer as a less invasive surgery: report of a case. Int Surg. 2007;92:249–253. [PubMed] [Google Scholar]
- 15.Fujisawa M., Ueno K., Kamidono S. Novel bladder sparing surgery for select patients with advanced rectal carcinoma. J Urol. 2002;167:643–644. doi: 10.1016/S0022-5347(01)69105-5. [DOI] [PubMed] [Google Scholar]


