Abstract
This article addresses the emergence of echinocandin resistance among Candida species, mechanisms of resistance, factors that promote resistance and confounding issues surrounding standard susceptibility testing. Fungal infections remain a significant cause of global morbidity and mortality, especially among patients with underlying immunosupression. Antifungal therapy is a critical component of patient management for acute and chronic diseases. Yet, therapeutic choices are limited due to only a few drug classes available to treat systemic disease. Moreover, the problem is exacerbated by the emergence of antifungal resistance, which has resulted in difficult to manage multidrug resistant strains. Echinocandin drugs are now the preferred choice to treat a range of candidiasis. These drugs target and inhibit the fungal-specific enzyme glucan synthase, which is responsible for the biosynthesis of a key cell wall polymer. Therapeutic failures involving acquisition of resistance among susceptible organisms like Candida albicans is largely a rare event. However, in recent years, there is an alarming trend of increased resistance among strains of Candida glabrata, which in many cases are also resistant to azole drugs. Echinocandin resistance is always acquired during therapy and the mechanism of resistance is well established to involve amino acid changes in “hot-spot regions of the Fks subunits carrying the catalytic portion of glucan synthase. These changes significantly decrease the sensitivity of the enzyme to drug resulting in higher MIC values. A range of drug responses, from complete to partial refractory response, is observed depending on the nature of the amino acid substitution, and clinical responses are recapitulated in pharmacodynamic models of infection. The cellular processes promoting the formation of resistant Fks strains involve complex stress response pathways, which yield a variety of adaptive compensatory genetic responses. Stress-adapted cells become drug tolerant and can form stable drug resistant FKS mutations with continued drug exposure. A major concern for resistance detection is that classical broth microdilution techniques show significant variability among clinical microbiology laboratories for certain echinocandin drugs and Candida species. The consequence is that susceptible strains are misclassified according to established clinical breakpoints, and this has led to confusion in the field. Clinical factors that appear to promote echinocandin resistance include the expanding use of antifungal agents for empiric therapy and prophylaxis. Furthermore, host reservoirs such as biofilms in the gastrointestinal tract or intra-abdominal infections can seed development of resistant organisms during therapy. A fundamental understanding of the primary molecular resistance mechanism, along with cellular and clinical factors that promote resistance emergence, is critical to develop better diagnostic tools and therapeutic strategies to overcome and prevent echinocandin resistance.
1. Introduction
Fungal infections are increasingly recognized as a major global health problem. There are more than 300 million people afflicted by a serious fungal infection resulting in nearly 1.4 million deaths annually (www.gaffi.org) [1]. Fungal diseases cause life-threatening illnesses such as meningitis and pneumonias, chronic asthma, other respiratory distress syndromes, and recurrent diseases like oral and vaginal thrush. Serious fungal infections are a consequence of underlying health problems such as asthma, AIDS, cancer, organ transplantation and corticosteroid therapies with a majority of fungal deaths due to Cryptococcus, Candida and Aspergillus species [1]. The management of fungal diseases requires antifungal therapy. Yet, treatment options are limited, as the most prominent antifungal drugs target either the plasma membrane, nucleic acid biosynthesis or cell wall, and they comprise only a few chemical classes represented by polyenes, azoles, flucytosine, and echinocandins [2]. Azoles drugs, which include fluconazole, itraconazole, voriconazole, posaconazole and isavuconazole inhibit the biosynthesis of the plasma membrane sterol ergosterol. The pore-forming polyene drug amphotericin B binds to ergosterol in the plasma membrane. Flucytosine (5-fluorocytosine) broadly inhibits pyrimidine metabolism and DNA synthesis, while the echinocandins drugs caspofungin, anidulafungin, and micafungin inhibit glucan synthase and are the first cell wall active agents. Echinocandins are recommended as first-line therapy for non-neutropenic patients with Candida albicans, Candida glabrata and suspected severe invasive candidiasis [3]. Recent CDC surveillance indicates that >60% of candidemia patients now receive an echinocandin [4]. It is the expanding application of echinocandins worldwide and emerging resistance among certain Candida species, which will be discussed in this review.
2. Echinocandin class drugs
Echinocandin drugs are lipopeptides that inhibit glucan synthase, which is responsible for the biosynthesis of β-1,3-D-glucan, a major structural component of fungal cell walls [5]. The U.S. Food and Drug Administration approved them for the treatment of esophageal and invasive candidiasis, including candidemia, empirical therapy in febrile neutropenic patients and prophylaxis in patients undergoing hematopoietic stem cell transplantation (HSCT) [6, 7]. The first in-class drug, caspofungin, was also approved for salvage therapy for patients with invasive aspergillosis [8]. Maintenance of the fungal cell wall is essential for cell survival and echinocandin drugs often show in vitro fungicidal activity against susceptible Candida spp. [9, 10]. Echinocandins are fungistatic against molds where they can lyse the apical tips of expanding hyphae, alter morphology and modify cell wall composition and organization [11, 12]. However, they are largely inactive against invasive Zygomycetes, Cryptococcus spp., or Fusarium spp. The echinocandin drugs have a distinct mechanism of action, which enable them to be highly effective against yeasts with reduced susceptibility to azoles, such as C. glabrata and C. krusei [13, 14] [15], as well as some Candida biofilms [16–19]. The echinocandins have an excellent therapeutic index with a low potential for renal or hepatic toxicity or serious drug-drug interactions [20, 21]. All echinocandins have low oral bioavailability, and distribute well into tissues, but poorly into the CNS and eye. The echinocandin target, β-1,3-D-glucan synthase, is a fungal-specific multi-subunit enzyme complex comprised of Rho, a GTP-binding protein, which helps regulate the overall activity of glucan synthase [22] and a catalytic subunit Fks encoded by three related genes, FKS1, FKS2, and FKS3. The FKS1 gene is essential in C. albicans [23, 24] and other Candida spp., while in C. glabrata, FKS1 and FKS2 are functionally redundant [25]. The FKS3 gene is expressed at a very low level relative to the other genes [26].
3. Epidemiology of Echinocandin Resistance
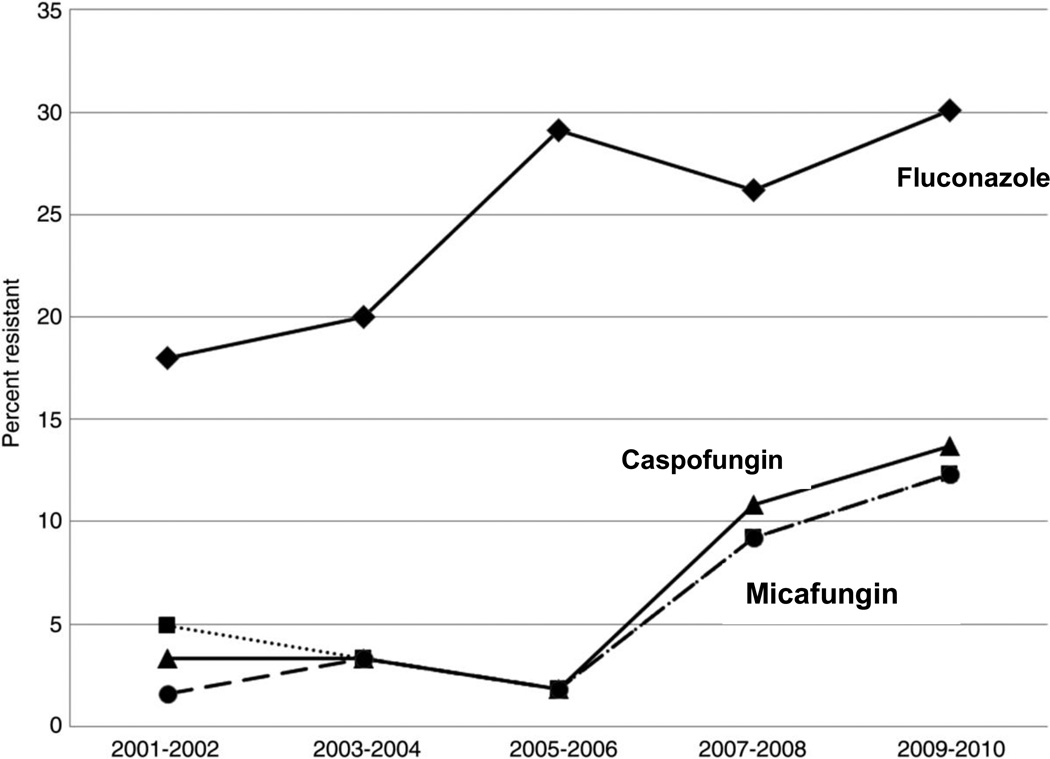
Most major Candida species are highly susceptible to echinocandin drugs [27, 28]. The notable exceptions are C. parapsilosis complex (Candida parapsilosis sensu stricto, C. orthopsilosis, and C. metapsilosis) and C. guilliermondii, which display higher echinocandin antifungal MIC values relative to other highly susceptible Candida species [29–31] [32–34] and is reflected in higher breakpoints [35]. Intrinsic reduced susceptibility has an unclear clinical significance as patients are often successfully treated with echinocandin drugs [36–38] [39], although clinical efficacy may vary with patient population [40–42]. Since first reported in 2005, susceptible Candida spp. isolates resistant to echinocandin drugs are increasingly encountered [43, 44, 26, 45–51] [52, 53] [54], although the frequency remains relatively low (<2–3%) with C. albicans and most other Candida spp. [55–57] [58] [58]. The notable exception is C. glabrata, where resistance is growing more rapidly [59, 60]. In many healthcare centers, the growing use of echinocandins and azoles for prophylaxis has resulted in an epidemiologic shift with C. glabrata represented as the most dominant fungal bloodstream pathogen [61] [30]. Echinocandin resistance may occur after prolonged therapy [52] or it may be rapid, even shortly after initiation of therapy [62] [53]. Recently, the SENTRY Antimicrobial Surveillance Program from 2006–2010 reported echinocandin resistance of 8.0–9.3% among 1669 blood stream isolates (BSI) of C. glabrata [63]. Furthermore, in a ten year study involving 293 unique episodes of C. glabrata BSI, echinocandin resistance of C. glabrata rose from 2–3% during 2001–2006 to >13% in the years 2009–2010 [59]. Disturbingly, this rise in echinocandin resistance among C. glabrata paralleled a rise in azole resistance resulting in multidrug resistant strains (Fig 1). The generally excellent wild-type susceptibility of C. glabrata to the echinocandin drugs, even among azole resistant strains, has driven the widespread use of echinocandins for treatment of infections due to C. glabrata. Yet, at the same time, it has generated selection pressure for multidrug resistant organisms [59]. The underlying genetic basis for rapid emergence of resistance in C. glabrata is largely unknown, but it may stem from its haploid state and/or from its inherent genetic plasticity. In molds, echinocandin resistance has also been described in rare circumstances for A. fumigatus [64] and more readily for A. lentulus [65].
Fig 1.
Temporal trends in antifungal resistance of Candida glabrata isolates to fluconazole, anidulafungin, caspofungin, and micafungin. Adapted from Alexander et al. [59]
4. Mechanism of Acquired Resistance
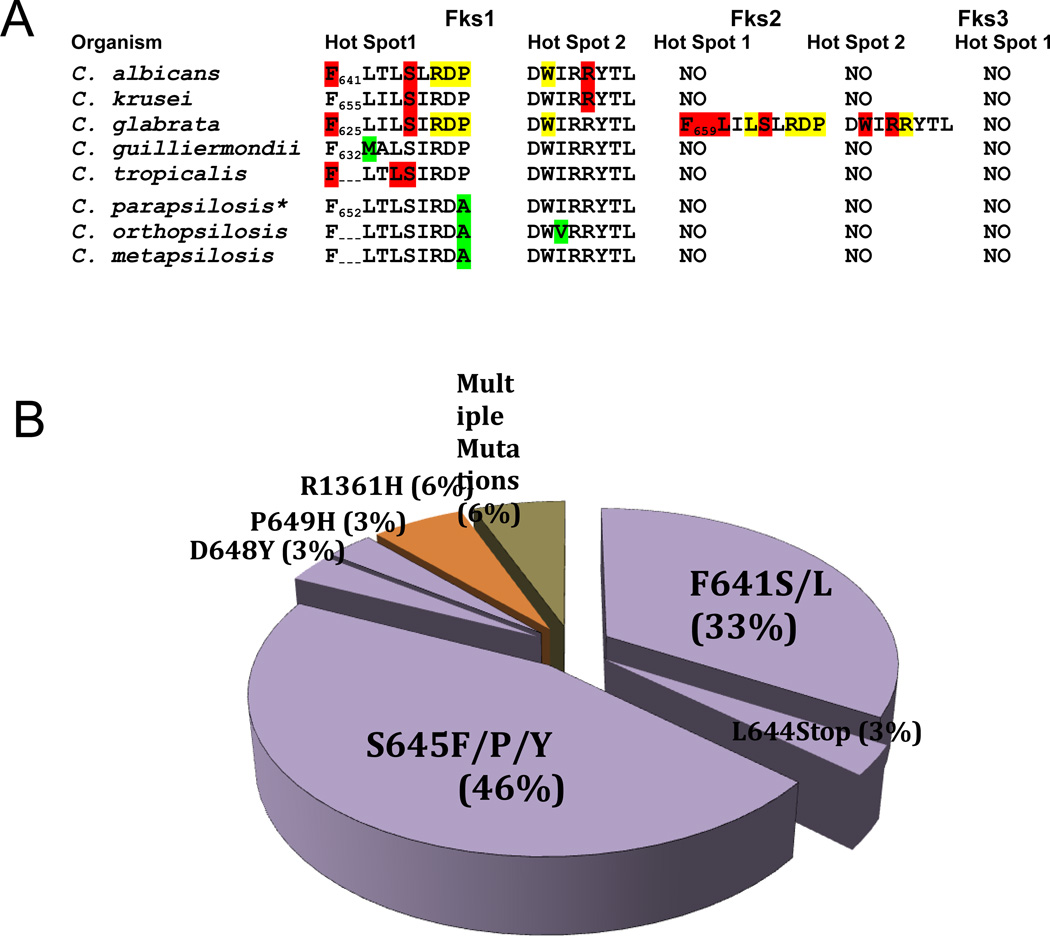
Clinical resistance resulting in therapeutic breakthrough infections involves modification of the catalytic Fsk subunit (Fks1 and Fks2) of glucan synthase. Unlike azole antifungal agents, echinocandins are not substrates for multidrug transporters [16, 15]. Echinocandin resistance is conferred by characteristic amino acid substitutions in Fks subunits [7], which induce elevated MIC values (10–100 fold) and reduce the sensitivity of glucan synthase (IC50) to drug by 50- to 3000-fold [26, 45, 66]. Characteristic mutations in FKS genes are prominently associated with reduced clinical response [67, 68]. In a recent study of patients with invasive candidiasis, the presence of an FKS mutation was the only independent risk factor associated with echinocandin failure and among C. glabrata isolates, and the presence of an FKS mutation was superior to MIC in predicting echinocandin therapeutic responses among patients [68]. In C. albicans and most other Candida spp., mutations occur in two highly conserved “hot-spot” regions of FKS1 [45, 69, 70] encompassing residues Phe641-Pro649 and Arg1361 (Fig 2). Amino acid substitutions at Ser645 and Phe641 are the most abundant, nearly 80% in C. albicans (Fig 2), and cause the most pronounced resistance phenotypes [26, 45, 7, 71]. These fks mutants are effectively insensitive to drug and fail to respond in pharmacodynamic studies of murine models of infection [72–75]. In C. glabrata, resistance-associated mutations occur in homologous regions of FKS1 and FKS2 [26, 66], although amino acid substitutions in Fks2 occur in clinical isolates at twice the frequency of Fks1 [26, 7, 71]. Alterations at Fks1 positions S629 and S663 and Fks2 position F659S confer the highest MIC values. Nonsense mutations in either FKS1 or FKS2 are also observed in C. glabrata [26, 66] [76]. The echinocandin resistance level conferred by hot spot mutations in FKS1 or FKS2 can also depend on the relative expression of their genes, which can vary more than 20-fold [26, 25]. FKS2 expression is calcineurin dependent and down regulated by FK506 [77], and resistance conferred by FKS2 can be reversed with FK506 [25]. Finally, mutations in FKS1 for Candida species such as C. tropicalis, C. krusei and C. kefyr have been linked with increases in echinocandin MIC and clinical failures [78, 79, 62].
Fig 2.
A. Amino acid sequences of Fks “hot-spot” sequences for major Candida species and positions associated with prominent resistance (red), weaker resistance (yellow) and naturally-occurring polymorphisms that cause reduced susceptibility (green). B. Relative frequency of Fks amino acid substitutions in C. albicans causing echinocandin resistance from Perlin Lab echinocandin reference center.
4. 1 FKS3, Virulence and Biofilms
A third highly conserved hot-spot region defined by W695 of S. cerevisiae Fks1 was recently identified [80], but it is not associated with clinical failures. Amino acid substitutions in Fks1 of C. albicans confer reduced fitness [26, 25] [81], since they can decrease the catalytic reaction rate maximum for glucan biosynthesis [26, 45] and alter cell wall morphology [81]. Echinocandin resistant strains compete poorly with their wild-type counterpart [81], which may explain why resistance is associated with acquired de novo resistance and horizontal transmission is not a factor.
Biofilms are an important complex communal structure of fungi contributing to antifungal drug resistance [82]. For echinocandin drugs, the extracellular matrix of the biofilm comprised mainly of β-glucan sequesters the drugs by decreasing their effective concentration at the surface of the fungal cell membrane [83]. The application of genetic or chemical means to decrease glucan production renders the biofilms more susceptible to antifungal agents [84]. Transcription factor Rlm, Smi1 and glucan synthase Fks1 are important factors that regulate glucan formation yielding drug-sequestering biofilms [84].
4.2 Serum, cellular stress and resistance emergence
The development of characteristic FKS mutations is an end stage event in the resistance process and there are a number of factors that condition cells and influence mutant selection. Firstly, the echinocandin drugs are highly serum protein bound, which reduces their relative efficacy and shifts MICs upward [85–87]. The nature of the shift depends on interactions with specific drugs; anidulafungin and micafungin show a larger relative shift than caspofungin. A consequence of this shift in efficacy is that serum alters the relative fungicidal properties of the drugs, often resulting in fungistatic behavior against certain Candida species [88, 89]. This drug shift permits cellular responses, which promote survival. In particular, fungi possess a range of adaptive response mechanisms that help protect cells against environmental stresses [90, 91]. Secondly, yeast acutely sense cell wall stress. Inhibition of glucan biosynthesis by the echinocandins induces a variety of stress tolerance pathways including cell wall integrity, PKC, Ca2+/calcineurin/Crz1, and HOG [92, 93]. Hsp90 induces tolerance to echinocandin drugs through its principal client protein calcineurin and the downstream effector crz1 [94, 95]. Finally, echinocandin action results in compensatory increases in chitin synthesis, which serves to maintain the structural integrity of the cell wall, as chitin replaces β-1,3 glucan [92], and cell wall mutants with enhanced chitin contents are less susceptible to echinocandins both in vitro [96, 92, 97, 93] and in vivo [98]. Elevated chitin and adaptive responses have been linked to paradoxical growth whereby susceptible cells show growth at very high levels of drug [99] [100] [101]. It has been proposed that sphingolipids can interact with echinocandins near their target and differentially decrease sensitivity to caspofungin while increasing sensitivity to micafungin [102, 103]. The collective adaptive cellular responses help stabilize cells in the presence of drug. Ultimately, they likely predispose cells and promote selection for FKS mediated resistance, even though by themselves they are insufficient to induce therapeutic failure.
5. Susceptibility Testing and Its Foibles
The goal of susceptibility testing is to establish an in vitro marker to characterize infecting strains as either “susceptible” to a drug and likely to respond to therapy or “resistant” with a heightened probability to fail therapy. This probability is best described as the “90-60 rule” in which infections due to susceptible isolates respond to therapy approximately 90% of the time, whereas infections due to resistant isolates respond 60% of the time [104]. To address this need, the antifungal susceptibility testing subcommittees (AFST) of the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) established independent, yet closely related standards for broth microdilution (BMD) antifungal susceptibility testing of echinocandins against Candida species, which generally yield comparable MIC results [105, 34, 106]. In 2007, the CLSI used clinical and microbiological data to establish a preliminary clinical breakpoint (CBP) for echinocandins against Candida spp. (Pfaller et al., 2008b) with an MIC ≤ 2 µg/ml considered susceptible for all three echinocandins and all species of Candida. However, it soon became apparent that resistant strains with acquired FKS mutations were often misclassified by this CBP [107, 45]. To address this issue, CLSI revised the CBP based on pharmacokinetic, microbiological and enzyme kinetic data, along with the clinical experience. New species and drug-specific breakpoints were established for CLSI BMD testing that accounted for strains containing FKS mutations (Pfaller et. 2011) (Table 1).
Table 1.
EUCAST and CLSI antifungal breakpoint comparison for major Candida species1
| Antifungal agent |
MIC breakpoint (mg/L) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Candida albicans |
Candida glabrata |
Candida krusei |
Candida parapsilosis |
Candida tropicalis | ||||||
| S≤ | R> | S≤ | R> | S≤ | R> | S≤ | R> | S≤ | R> | |
| Anidulafungin | ||||||||||
| EUCAST | 0.03 | 0.03 | 0.06 | 0.06 | 0.06 | 0.06 | 0.002 | 4 | 0.06 | 0.06 |
| CLSI | 0.25 | 0.5 | 0.12 | 0.25 | 0.25 | 0.5 | 2 | 4 | 0.25 | 0.5 |
| Caspofungin | ||||||||||
| EUCAST | ND2 | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| CLSI | 0.25 | 0.5 | 0.12 | 0.25 | 0.25 | 0.5 | 2 | 4 | 0.25 | 0.5 |
| Micafungin | ||||||||||
| EUCAST | 0.016 | 0.016 | 0.03 | 0.03 | IE3 | IE | 0.002 | 2 | IE | IE |
| CLSI | 0.25 | 0.5 | 0.06 | 0.125 | 0.25 | 0.5 | 2 | 4 | 0.25 | 0.5 |
Adapted from Arendrup et al. [114]
ND- Not determined due to significant inter-laboratory variation in MIC ranges
IE- Insufficient evidence (IE) due to small number of cases
Yet the new lower CBPs posed a testing challenge, as BMD testing was not sufficiently robust to enable consistent interlaboratory testing without major errors encountered between groups [108–110]. Wide modal ranges were especially present with C. glabrata and caspofungin where numerous groups were unable to provide consistent testing with either CLSI or EUCAST methods [108–110] [111]. The underlying factor(s) contributing to this variability has not been ascertained. Since the use of a CLSI species-specific caspofungin CBP can lead to reporting an excessive number of wild-type isolates as either non-WT or resistant isolates [109], it has been recommended that micafungin or anidulafungin be used as a surrogate class marker, since either drug behaves more predictably [110]. The problem with this approach is that many physicians who depend on caspofungin for therapy are uncomfortable with a drug surrogate, even among the same drug class. Epidemiological cutoff values (ECVs) have been established to define the upper limit of the “wild type” MIC distribution for each species with no acquired resistance mechanisms [112]. Species-specific ECVs aid in detecting non-WT isolates with reduced susceptibility to anidulafungin and micafungin due to fks mutations, and have been shown to classify 92.2% and 100% of the fks mutant strains, respectively [27] (Table 2). EUCAST has established breakpoints for anidulafungin (Table 1) and recommends anidulafungin MIC testing as a marker for the echinocandin class of drugs [113] [114]. However, due to the irregularities observed with testing between laboratories, EUCAST has not set caspofungin breakpoints and does not currently recommend caspofungin MIC testing for clinical decision-making involving echinocandin drugs [114].
TABLE 2.
Anidulafungin and micafungin ECVs for eight species of Candida1
| Antifungal agent |
Species | No. of isolates |
MIC (µg/ml) | ECV (µg/ml)2 | |||
|---|---|---|---|---|---|---|---|
| Range | Mode | ≥95% | ≥97.5% | ≥99% | |||
| Anidulafungin | C. albicans | 8,210 | 0.008–2 | 0.03 | 0.06 | 0.12 | 0.12 |
| C. glabrata | 2,680 | 0.008–4 | 0.06 | 0.12 | 0.12 | 0.25 | |
| C. parapsilosis | 3,976 | 0.008–8 | 2 | 4 | 8 | 8 | |
| C. tropicalis | 2,042 | 0.008–2 | 0.03 | 0.12 | 0.12 | 0.12 | |
| C. krusei | 322 | 0.008–2 | 0.06 | 0.12 | 0.25 | 0.25 | |
| C. lusitaniae | 234 | 0.008–1 | 0.25 | 1 | 1 | 1 | |
| C. guilliermondii | 222 | 0.03–4 | 1 | 4 | 8 | 8 | |
| C. dubliniensis | 131 | 0.015–4 | 0.03 | 0.12 | 0.12 | 0.12 | |
| Micafungin | C. albicans | 7,874 | 0.008–4 | 0.015 | 0.03 | 0.03 | 0.03 |
| C. glabrata | 3,102 | 0.008–4 | 0.015 | 0.03 | 0.03 | 0.03 | |
| C. parapsilosis | 3,484 | 0.015–4 | 1 | 2 | 4 | 4 | |
| C. tropicalis | 1,605 | 0.008–8 | 0.015 | 0.06 | 0.06 | 0.12 | |
| C. krusei | 617 | 0.015–1 | 0.06 | 0.25 | 0.25 | 0.25 | |
| C. lusitaniae | 258 | 0.008–≥16 | 0.25 | 0.5 | 0.5 | 1 | |
| C. guilliermondii | 234 | 0.015–8 | 0.5 | 2 | 2 | 4 | |
| C. dubliniensis | 117 | 0.008–8 | 0.06 | 0.12 | 0.12 | 0.12 | |
Adapted from Pfaller et al. 2014 [27]
Calculated ECVs comprising ≥95%, ≥97.5%, or ≥99% of the statistically modeled MIC population.
5.1 Is it time for molecular testing?
The problem of conventional susceptibility testing to distinguish wild type susceptible isolates from echinocandin resistant isolates bearing FKS mutations raises the notion that molecular testing may be long overdue for this field. There is overwhelming data linking the presence of specific hot-spot mutations in FKS genes to reduced clinical efficacy, which is supported by extensive studies of pharmacodynamics, inhibition of glucan synthase, and MIC [35]. Several clinical studies have shown that the presence of an FKS mutation is the most important independent risk factor in predicting echinocandin therapeutic responses among patients with IC [68] [76, 67]. The downside of molecular testing is that not all FKS mutations harbor the same potential for high-level resistance [67] [7], which would require stratification of mutations. Nevertheless, only a few mutations account for the vast majority of therapeutic failures (Fig. 2), which would support a role for molecular testing [115]. Molecular testing requires knowledge of known resistance mechanisms, and any unknown mechanism would not be detected. Yet, this probability is sufficiently remote given the current body of data. Thus, it may be time to implement molecular testing to directly identify mutant strains containing fks mutations and end the susceptibility testing controversies, which prevent timely and proper assessment of resistance.
6. Prophylaxis: Benefits with a potential resistance cost
Antifungal prophylaxis is now a standard prevention in many settings involving patients at high risk for development of invasive fungal infections, especially patients undergoing transplantation or other conditions resulting in severe immune deficiency. For many years, fluconazole was the antifungal drug of choice for primary prophylaxis in HSCT recipients [116, 117]. However, fluconazole has a limited spectrum, even among prominent Candida spp., some of which are inherently less sensitive to azoles (e.g. C. glabrata and C. krusei). Furthermore, it is inactive against Aspergillus species and other molds, which led to a call for more potent antifungal drugs in prophylactic regimens [118].
Echinocandin drugs are an attractive alternative for prophylaxis since they display favorable pharmacokinetics, have an excellent safety profile and are active against azole resistant yeasts and molds. This is particularly true for micafungin, which minimizes the potential for drug interactions since it does not interact with compounds whose metabolism is mediated via cytochrome P450 [119]. In an early prospective trial of micafungin and fluconazole involving 899 patients, micafungin was shown to have a higher overall treatment success rate demonstrating its effectiveness as a prophylactic agent [120]. Similarly, caspofungin was evaluated as primary prophylaxis against invasive fungal infections in 123 stem cell transplant recipients who were poor candidates for triazole or polyene prophylaxis, and it was deemed an effective and well-tolerated option for primary antifungal prophylaxis for the highly immunosuppressed stem cell transplant patient population [121]. Caspofungin was equally effective as itraconazole in preventing invasive fungal infections in patients with hematologic malignancies and it was effective in both adult [122] and pediatric populations [123]. Micafungin was somewhat more effective than fluconazole for the prevention of all mold infections and invasive aspergillosis and reducing the need for empiric antifungal treatment [124]. In large meta analyses involving 17 studies covering 5122 patients [125] and 20 studies covering 4823 patients [124], respectively, echinocandin prophylaxis reduced the incidence of invasive fungal infections greater than fluconazole or itraconazole. Micafungin is now approved by the FDA for prophylaxis of Candida infections in patients undergoing hematopoietic SCT or expected to be neutropenic for at least 10 days [126]. The latest European Society of Clinical Microbiology and Infectious Diseases guidelines also recommend micafungin for prophylaxis against Candida infections in allogeneic HSCT adult and pediatric patients, as well as in pediatric patients with acute myeloid and recurrent leukemia. There is a recommendation for caspofungin prophylaxis to prevent invasive candidiasis/candidemia, as well as intra-abdominal Candida infection [127]. There is a marginal recommendation for prophylaxis of adult HSCT patients with caspofungin and no recommendation for the use of anidulafungin [128].
6.1 Prophylaxis as a resistance driver
The expanding use of echinocandins for prophylaxis and therapy, while beneficial in reducing the overall incidence of invasive disease in high-risk settings, raises a critical question about its role in inducing significantly higher rates of echinocandin drug resistance, especially among C. glabrata. In a recent report, involving a 25-year-old patient receiving micafungin prophylaxis, five C. glabrata isolates were obtained from blood cultures and were classified as multidrug-resistant isolates, since all exhibited high MICs for echinocandin and azole drugs [129]. The co-evolution of azole and echinocandin multidrug resistance among C. glabrata is an alarming trend [59]. Similarly, breakthrough infections involving C. albicans are also being reported in patients with graft-versus-host disease following a stem cell transplant who received micafungin prophylaxis [130]. Most recently, a disturbing report from a retrospective observational study involving echinocandin-based anti-Aspergillus prophylaxis for 152 patients with acute myeloid leukemia during remission-induction chemotherapy showed a higher risk of breakthrough IFI [131]. It is not surprising that broadening patient exposure to echinocandin drugs would promote development of resistance. Beyond anecdotal reports, there is firm data emerging that the FKS resistance mechanism is an important risk factor for therapeutic failure [68] and resistance emergence is directly linked to prior exposure [132]. There is a danger that broadening echinocandin prophylaxis may continue to fuel an increase in the frequency of isolates that are resistant to multiple classes of antifungal drugs, which may reflect genomic plasticity among otherwise clonal organisms [133]. The trend toward echinocandin prophylaxis should be coupled with a renewed evaluation of drug dosing to ensure suitably high levels of drug are achieved. It may be time to reassess dosing strategy in the context of prophylactic regimens.
6.2 Reservoirs for resistance emergence?
The gastrointestinal (GI) tract is a normal commensal site for Candida species with the burden often exceeding 107 cfu/g of feces [134–141] and molecular genotyping has demonstrated that colonizing isolates often are the infecting strain for most patients with invasive candidiasis [142]. Candida colonization of the GI tract is often in the form of a mixed microbial biofilm [143]. A consequence of the biofilm microbial community is that there is varying levels of drug exposure to different parts of the biofilm, since there are induced mechanisms against azole drugs [144] and drug penetration into the glucan matrix is irregular [83]. Thus, there is a potential to select for resistant variants, which can desorb from the biofilm and cause systemic infections. The biofilm is difficult to eradicate and it can act as a reservoir that seeds resistant infections. Intra-abdominal candidiasis, including peritonitis and intra-abdominal abscesses, may occur in >40% of patients following repeat gastrointestinal surgery, GI perforation or necrotizing pancreatitis [145]. The high burden of Candida coupled with poor drug penetration into the biofilm creates a strong environment for selection of resistant variants.
7. New Therapy Trends: Large-daily infrequent doses
The echinocandins exhibit concentration-dependent effects on Candida species. Preclinical studies and pharmacokinetic and pharmacodynamic studies support the administration of large, infrequent doses and better outcomes were observed with higher maximum concentrations of drug in serum and large, infrequent doses [146]. Once-weekly micafungin therapy is as efficacious as daily therapy in a murine model of disseminated candidiasis [147]. This emerging therapeutic strategy may be appealing for certain forms of Candidiasis. Resistance emergence may be a concern as drug levels diminish. However, the development of resistance may actually be less likely to occur as the larger doses may place the drug exposure level within the mutant prevention concentration window that precludes development of single step resistance [148, 149].
8. CONCLUSIONS AND PERSPECTIVE
Echinocandin resistance is on the rise, especially among clinical isolates of Candida glabrata. This resistance trend is particularly alarming since such strains may also carry azole resistance leading to multidrug resistant strains resulting in difficult to manage infections. The Fks mechanism of resistance involving modification of the target enzyme glucan synthase is well established. But there is now emerging evidence that cellular stress pathways play a critical role in establishing drug adaptive states, which facilitate development of stable resistance with FKS genotypes. A current challenge and concern for clinical laboratories is the recent refinement of breakpoints by the CLSI to distinguish resistant strains containing FKS mutations from wild type susceptible strains using broth microdilution methodology. This has led to inter-laboratory variability resulting in the misclassification of susceptible isolates as resistant. It has been suggested that either micafungin or anidulafungin, which show greater in vitro sensitivity under conventional MIC testing can serve as a surrogate for the class. However, as the objective of such testing is to identify strains with fks genotypes, it may be time for the field to move to direct sequence-based detection, as is done routinely for bacteria and viruses. Finally, the expanding use of echinocandin prophylaxis increases drug exposure in the host leading to resistance, as reservoirs of colonization and/or infections may have less than adequate drug exposure. It may be time to reassess prophylactic dosing regimens in patients at high risk for invasive fungal disease.
Key Points.
Echinocandin drugs are important first line therapy for Candida species infections but drug resistance, especially among C. glabrata, is an emerging problem that impacts clinical outcome
Mutations in FKS genes resulting in amino acid substitutions in the drug target glucan synthase confer higher MIC values, reduced enzyme sensitivity to drug, and diminished pharmacodynamics response.
The emergence of FKS-mediated resistance requires drug adaptation involving a wide range of cellular responses to cell wall stress.
Problems with susceptibility testing may necessitate the development of alternative methodologies, such as molecular profiling of FKS genes.
Echinocandin prophylaxis is effective but may help fuel an increase in the frequency of isolates that are resistant to multiple classes of antifungal drugs
ACKNOWLEDGMENTS
D.S.P. was partially supported by NIH grant AI069397 and Pfizer, and is an inventor in a pending U.S. patent application entitled “Assays for Resistance to Echinocandin-Class Drugs.”
REFERENCES
- 1.Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4(165):165rv13. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- 2.Odds FC, Brown AJ, Gow NA. Antifungal agents: mechanisms of action. Trends Microbiol. 2003;11(6):272–279. doi: 10.1016/s0966-842x(03)00117-3. [DOI] [PubMed] [Google Scholar]
- 3.Pappas PG, Kauffman CA, Andes D, Benjamin DK, Jr, Calandra TF, Edwards JE, Jr, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(5):503–535. doi: 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cleveland AA, Farley MM, Harrison LH, Stein B, Hollick R, Lockhart SR, et al. Changes in incidence and antifungal drug resistance in candidemia: results from population-based laboratory surveillance in Atlanta and Baltimore, 2008–2011. Clin Infect Dis. 2012;55(10):1352–1361. doi: 10.1093/cid/cis697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Onishi J, Meinz M, Thompson J, Curotto J, Dreikorn S, Rosenbach M, et al. Discovery of novel antifungal (1,3)-beta-D-glucan synthase inhibitors. Antimicrob Agents Chemother. 2000;44(2):368–377. doi: 10.1128/aac.44.2.368-377.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turner MS, Drew RH, Perfect JR. Emerging echinocandins for treatment of invasive fungal infections. Expert Opin Emerg Drugs. 2006;11(2):231–250. doi: 10.1517/14728214.11.2.231. [DOI] [PubMed] [Google Scholar]
- 7.Perlin DS. Current perspectives on echinocandin class drugs. Future Microbiol. 2011;6(4):441–457. doi: 10.2217/fmb.11.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh TJ, Anaissie EJ, Denning DW, Herbrecht R, Kontoyiannis DP, Marr KA, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46(3):327–360. doi: 10.1086/525258. [DOI] [PubMed] [Google Scholar]
- 9.Barchiesi F, Spreghini E, Tomassetti S, Arzeni D, Giannini D, Scalise G. Comparison of the fungicidal activities of caspofungin and amphotericin B against Candida glabrata. Antimicrobial agents and chemotherapy. 2005;49(12):4989–4992. doi: 10.1128/AAC.49.12.4989-4992.2005. doi:49/12/4989 [pii] 10.1128/AAC.49.12.4989-4992.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ernst EJ, Klepser ME, Ernst ME, Messer SA, Pfaller MA. In vitro pharmacodynamic properties of MK-0991 determined by time-kill methods. Diagn Microbiol Infect Dis. 1999;33(2):75–80. doi: 10.1016/s0732-8893(98)00130-8. doi:S0732-8893(98)00130-8 [pii]. [DOI] [PubMed] [Google Scholar]
- 11.Bowman JC, Abruzzo GK, Flattery AM, Gill CJ, Hickey EJ, Hsu MJ, et al. Efficacy of caspofungin against Aspergillus flavus, Aspergillus terreus, and Aspergillus nidulans. Antimicrobial agents and chemotherapy. 2006;50(12):4202–4205. doi: 10.1128/AAC.00485-06. doi:AAC.00485-06 [pii] 10.1128/AAC.00485-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowman JC, Hicks PS, Kurtz MB, Rosen H, Schmatz DM, Liberator PA, et al. The antifungal echinocandin caspofungin acetate kills growing cells of Aspergillus fumigatus in vitro. Antimicrobial agents and chemotherapy. 2002;46(9):3001–3012. doi: 10.1128/AAC.46.9.3001-3012.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfaller MA, Messer SA, Boyken L, Rice C, Tendolkar S, Hollis RJ, et al. Caspofungin activity against clinical isolates of fluconazole-resistant Candida. J Clin Microbiol. 2003;41(12):5729–5731. doi: 10.1128/JCM.41.12.5729-5731.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bachmann SP, Patterson TF, Lopez-Ribot JL. In vitro activity of caspofungin (MK-0991) against Candida albicans clinical isolates displaying different mechanisms of azole resistance. J Clin Microbiol. 2002;40(6):2228–2230. doi: 10.1128/JCM.40.6.2228-2230.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Niimi K, Maki K, Ikeda F, Holmes AR, Lamping E, Niimi M, et al. Overexpression of Candida albicans CDR1, CDR2, or MDR1 does not produce significant changes in echinocandin susceptibility. Antimicrob Agents Chemother. 2006;50(4):1148–1155. doi: 10.1128/AAC.50.4.1148-1155.2006. doi:50/4/1148 [pii] 10.1128/AAC.50.4.1148-1155.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bachmann SP, Ramage G, VandeWalle K, Patterson TF, Wickes BL, Lopez-Ribot JL. Antifungal combinations against Candida albicans biofilms in vitro. Antimicrobial agents and chemotherapy. 2003;47(11):3657–3659. doi: 10.1128/AAC.47.11.3657-3659.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira JA, Carr JH, Starling CE, de Resende MA, Donlan RM. Biofilm formation and effect of caspofungin on biofilm structure of Candida species bloodstream isolates. Antimicrobial agents and chemotherapy. 2009;53(10):4377–4384. doi: 10.1128/AAC.00316-09. doi:AAC.00316-09 [pii] 10.1128/AAC.00316-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuhn DM, George T, Chandra J, Mukherjee PK, Ghannoum MA. Antifungal susceptibility of Candida biofilms: unique efficacy of amphotericin B lipid formulations and echinocandins. Antimicrobial agents and chemotherapy. 2002;46(6):1773–1780. doi: 10.1128/AAC.46.6.1773-1780.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simitsopoulou M, Peshkova P, Tasina E, Katragkou A, Kyrpitzi D, Velegraki A, et al. Species-specific and drug-specific differences in susceptibility of Candida biofilms to echinocandins: characterization of less common bloodstream isolates. Antimicrobial agents and chemotherapy. 2013;57(6):2562–2570. doi: 10.1128/AAC.02541-12. doi:10.1128/AAC.02541-12 AAC.02541-12 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen SC, Slavin MA, Sorrell TC. Echinocandin antifungal drugs in fungal infections: a comparison. Drugs. 2011;71(1):11–41. doi: 10.2165/11585270-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 21.Kofla G, Ruhnke M. Pharmacology and metabolism of anidulafungin, caspofungin and micafungin in the treatment of invasive candidosis: review of the literature. Eur J Med Res. 2011;16(4):159–166. doi: 10.1186/2047-783X-16-4-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mazur P, Baginsky W. In vitro activity of 1,3-beta-D-glucan synthase requires the GTP-binding protein Rho1. J Biol Chem. 1996;271(24):14604–14609. doi: 10.1074/jbc.271.24.14604. [DOI] [PubMed] [Google Scholar]
- 23.Mio T, Adachi-Shimizu M, Tachibana Y, Tabuchi H, Inoue SB, Yabe T, et al. Cloning of the Candida albicans homolog of Saccharomyces cerevisiae GSC1/FKS1 and its involvement in beta-1,3-glucan synthesis. J Bacteriol. 1997;179(13):4096–4105. doi: 10.1128/jb.179.13.4096-4105.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson JR, Douglas CM, Li W, Jue CK, Pramanik B, Yuan X, et al. A glucan synthase FKS1 homolog in cryptococcus neoformans is single copy and encodes an essential function. J Bacteriol. 1999;181(2):444–453. doi: 10.1128/jb.181.2.444-453.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Katiyar SK, Alastruey-Izquierdo A, Healey KR, Johnson ME, Perlin DS, Edlind TD. Fks1 and Fks2 are functionally redundant but differentially regulated in Candida glabrata: implications for echinocandin resistance. Antimicrob Agents Chemother. 2012;56(12):6304–6309. doi: 10.1128/AAC.00813-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Garcia-Effron G, Lee S, Park S, Cleary JD, Perlin DS. Effect of Candida glabrata FKS1 and FKS2 mutations on echinocandin sensitivity and kinetics of 1,3-beta-D-glucan synthase: implication for the existing susceptibility breakpoint. Antimicrob Agents Chemother. 2009;53(9):3690–3699. doi: 10.1128/AAC.00443-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pfaller MA, Espinel-Ingroff A, Bustamante B, Canton E, Diekema DJ, Fothergill A, et al. Multicenter study of anidulafungin and micafungin MIC distributions and epidemiological cutoff values for eight Candida species and the CLSI M27-A3 broth microdilution method. Antimicrob Agents Chemother. 2014;58(2):916–922. doi: 10.1128/AAC.02020-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pfaller MA, Messer SA, Woosley LN, Jones RN, Castanheira M. Echinocandin and triazole antifungal susceptibility profiles for clinical opportunistic yeast and mold isolates collected from 2010 to 2011: application of new CLSI clinical breakpoints and epidemiological cutoff values for characterization of geographic and temporal trends of antifungal resistance. J Clin Microbiol. 2013;51(8):2571–2581. doi: 10.1128/JCM.00308-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pfaller MA, Boyken L, Hollis RJ, Kroeger J, Messer SA, Tendolkar S, et al. Wild-type MIC distributions and epidemiological cutoff values for the echinocandins and Candida spp. J Clin Microbiol. 2010;48(1):52–56. doi: 10.1128/JCM.01590-09. doi:JCM.01590-09 [pii] 10.1128/JCM.01590-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tortorano AM, Prigitano A, Lazzarini C, Passera M, Deiana ML, Cavinato S, et al. A 1-year prospective survey of candidemia in Italy and changing epidemiology over one decade. Infection. 2013;41(3):655–662. doi: 10.1007/s15010-013-0455-6. [DOI] [PubMed] [Google Scholar]
- 31.Pfaller MA, Boyken L, Hollis RJ, Kroeger J, Messer SA, Tendolkar S, et al. In vitro susceptibility of invasive isolates of Candida spp. to anidulafungin, caspofungin, and micafungin: six years of global surveillance. J Clin Microbiol. 2008;46(1):150–156. doi: 10.1128/JCM.01901-07. doi:JCM.01901-07 [pii] 10.1128/JCM.01901-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garcia-Effron G, Canton E, Peman J, Dilger A, Roma E, Perlin DS. Epidemiology and echinocandin susceptibility of Candida parapsilosis sensu lato species isolated from bloodstream infections at a Spanish university hospital. J Antimicrob Chemother. 2012;67(11):2739–2748. doi: 10.1093/jac/dks271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spreghini E, Orlando F, Tavanti A, Senesi S, Giannini D, Manso E, et al. In vitro and in vivo effects of echinocandins against Candida parapsilosis sensu stricto, Candida orthopsilosis and Candida metapsilosis. J Antimicrob Chemother. 2012;67(9):2195–2202. doi: 10.1093/jac/dks180. [DOI] [PubMed] [Google Scholar]
- 34.Pfaller MA, Castanheira M, Diekema DJ, Messer SA, Moet GJ, Jones RN. Comparison of European Committee on Antimicrobial Susceptibility Testing (EUCAST) and Etest methods with the CLSI broth microdilution method for echinocandin susceptibility testing of Candida species. J Clin Microbiol. 2010;48(5):1592–1599. doi: 10.1128/JCM.02445-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfaller MA, Diekema DJ, Andes D, Arendrup MC, Brown SD, Lockhart SR, et al. Clinical breakpoints for the echinocandins and Candida revisited: integration of molecular, clinical, and microbiological data to arrive at species-specific interpretive criteria. Drug Resist Updat. 2011;14(3):164–176. doi: 10.1016/j.drup.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Mora-Duarte J, Betts R, Rotstein C, Colombo AL, Thompson-Moya L, Smietana J, et al. Comparison of caspofungin and amphotericin B for invasive candidiasis. N Engl J Med. 2002;347(25):2020–2029. doi: 10.1056/NEJMoa021585. doi:10.1056/NEJMoa021585 347/25/2020 [pii]. [DOI] [PubMed] [Google Scholar]
- 37.Kale-Pradhan PB, Morgan G, Wilhelm SM, Johnson LB. Comparative efficacy of echinocandins and nonechinocandins for the treatment of Candida parapsilosis Infections: a meta-analysis. Pharmacotherapy. 2010;30(12):1207–1213. doi: 10.1592/phco.30.12.1207. doi:10.1592/phco.30.12.1207 10.1592/phco.30.12.1207 [pii]. [DOI] [PubMed] [Google Scholar]
- 38.Colombo AL, Perfect J, DiNubile M, Bartizal K, Motyl M, Hicks P, et al. Global distribution and outcomes for Candida species causing invasive candidiasis: results from an international randomized double-blind study of caspofungin versus amphotericin B for the treatment of invasive candidiasis. Eur J Clin Microbiol Infect Dis. 2003;22(8):470–474. doi: 10.1007/s10096-003-0973-8. [DOI] [PubMed] [Google Scholar]
- 39.Fernandez-Ruiz M, Aguado JM, Almirante B, Lora-Pablos D, Padilla B, Puig-Asensio M, et al. Initial Use of Echinocandins Does Not Negatively Influence Outcome in Candida parapsilosis Bloodstream Infection: A Propensity Score Analysis. Clin Infect Dis. 2014;58(10):1413–1421. doi: 10.1093/cid/ciu158. [DOI] [PubMed] [Google Scholar]
- 40.Ghannoum MA, Chen A, Buhari M, Chandra J, Mukherjee PK, Baxa D, et al. Differential in vitro activity of anidulafungin, caspofungin and micafungin against Candida parapsilosis isolates recovered from a burn unit. Clin Microbiol Infect. 2009;15(3):274–279. doi: 10.1111/j.1469-0691.2008.02660.x. doi:10.1111/j.1469-0691.2008.02660.x CLM2660 [pii]. [DOI] [PubMed] [Google Scholar]
- 41.Kabbara N, Lacroix C, Peffault de Latour R, Socie G, Ghannoum M, Ribaud P. Breakthrough C. parapsilosis and C. guilliermondii blood stream infections in allogeneic hematopoietic stem cell transplant recipients receiving long-term caspofungin therapy. Haematologica. 2008;93(4):639–640. doi: 10.3324/haematol.11149. doi:10.3324/haematol.11149 93/4/639 [pii]. [DOI] [PubMed] [Google Scholar]
- 42.Forrest GN, Weekes E, Johnson JK. Increasing incidence of Candida parapsilosis candidemia with caspofungin usage. J Infect. 2008;56(2):126–129. doi: 10.1016/j.jinf.2007.10.014. doi:S0163-4453(07)00813-4 [pii] 10.1016/j.jinf.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 43.Cleary JD, Garcia-Effron G, Chapman SW, Perlin DS. Reduced Candida glabrata susceptibility secondary to an FKS1 mutation developed during candidemia treatment. Antimicrobial agents and chemotherapy. 2008;52(6):2263–2265. doi: 10.1128/AAC.01568-07. doi:AAC.01568-07 [pii] 10.1128/AAC.01568-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garcia-Effron G, Chua DJ, Tomada JR, DiPersio J, Perlin DS, Ghannoum M, et al. Novel FKS mutations associated with echinocandin resistance in Candida species. Antimicrobial agents and chemotherapy. 2010;54(5):2225–2227. doi: 10.1128/AAC.00998-09. doi:AAC.00998-09 [pii] 10.1128/AAC.00998-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Garcia-Effron G, Park S, Perlin DS. Correlating echinocandin MIC and kinetic inhibition of fks1 mutant glucan synthases for Candida albicans: implications for interpretive breakpoints. Antimicrob Agents Chemother. 2009;53(1):112–122. doi: 10.1128/AAC.01162-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kahn JN, Garcia-Effron G, Hsu MJ, Park S, Marr KA, Perlin DS. Acquired echinocandin resistance in a Candida krusei isolate due to modification of glucan synthase. Antimicrobial agents and chemotherapy. 2007;51(5):1876–1878. doi: 10.1128/AAC.00067-07. doi:AAC.00067-07 [pii] 10.1128/AAC.00067-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Laverdiere M, Lalonde RG, Baril JG, Sheppard DC, Park S, Perlin DS. Progressive loss of echinocandin activity following prolonged use for treatment of Candida albicans oesophagitis. J Antimicrob Chemother. 2006;57(4):705–708. doi: 10.1093/jac/dkl022. doi:dkl022 [pii] 10.1093/jac/dkl022. [DOI] [PubMed] [Google Scholar]
- 48.Miller CD, Lomaestro BW, Park S, Perlin DS. Progressive esophagitis caused by Candida albicans with reduced susceptibility to caspofungin. Pharmacotherapy. 2006;26(6):877–880. doi: 10.1592/phco.26.6.877. [DOI] [PubMed] [Google Scholar]
- 49.Garcia-Effron G, Kontoyiannis DP, Lewis RE, Perlin DS. Caspofungin-resistant Candida tropicalis strains causing breakthrough fungemia in patients at high risk for hematologic malignancies. Antimicrobial agents and chemotherapy. 2008;52(11):4181–4183. doi: 10.1128/AAC.00802-08. doi:AAC.00802-08 [pii] 10.1128/AAC.00802-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wiederhold NP, Grabinski JL, Garcia-Effron G, Perlin DS, Lee SA. Pyrosequencing to detect mutations in FKS1 that confer reduced echinocandin susceptibility in Candida albicans. Antimicrobial agents and chemotherapy. 2008;52(11):4145–4148. doi: 10.1128/AAC.00959-08. doi:AAC.00959-08 [pii] 10.1128/AAC.00959-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pfeiffer CD, Garcia-Effron G, Zaas AK, Perfect JR, Perlin DS, Alexander BD. Breakthrough invasive candidiasis in patients on micafungin. J Clin Microbiol. 2010;48(7):2373–2380. doi: 10.1128/JCM.02390-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thompson GR, 3rd, Wiederhold NP, Vallor AC, Villareal NC, Lewis JS, 2nd, Patterson TF. Development of caspofungin resistance following prolonged therapy for invasive candidiasis secondary to Candida glabrata infection. Antimicrobial agents and chemotherapy. 2008;52(10):3783–3785. doi: 10.1128/AAC.00473-08. doi:10.1128/AAC.00473-08 AAC.00473-08 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lewis JS, 2nd, Wiederhold NP, Wickes BL, Patterson TF, Jorgensen JH. Rapid Emergence of Echinocandin Resistance in Candida glabrata Resulting in Clinical and Microbiologic Failure. Antimicrobial agents and chemotherapy. 2013 doi: 10.1128/AAC.01144-13. doi:AAC.01144-13 [pii] 10.1128/AAC.01144-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dannaoui E, Desnos-Ollivier M, Garcia-Hermoso D, Grenouillet F, Cassaing S, Baixench MT, et al. Candida spp. with Acquired Echinocandin Resistance, France, 2004–2010(1) Emerg Infect Dis. 2012;18(1):86–90. doi: 10.3201/eid1801.110556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pfaller MA, Castanheira M, Messer SA, Moet GJ, Jones RN. Echinocandin and triazole antifungal susceptibility profiles for Candida spp., Cryptococcus neoformans, and Aspergillus fumigatus: application of new CLSI clinical breakpoints and epidemiologic cutoff values to characterize resistance in the SENTRY Antimicrobial Surveillance Program (2009) Diagn Microbiol Infect Dis. 2011;69(1):45–50. doi: 10.1016/j.diagmicrobio.2010.08.013. doi:S0732-8893(10)00342-1 [pii] 10.1016/j.diagmicrobio.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 56.Pfaller MA, Messer SA, Moet GJ, Jones RN, Castanheira M. Candida bloodstream infections: comparison of species distribution and resistance to echinocandin and azole antifungal agents in Intensive Care Unit (ICU) and non-ICU settings in the SENTRY Antimicrobial Surveillance Program (2008–2009) Int J Antimicrob Agents. 2011;38(1):65–69. doi: 10.1016/j.ijantimicag.2011.02.016. doi:S0924-8579(11)00132-4 [pii] 10.1016/j.ijantimicag.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 57.Pfaller MA, Moet GJ, Messer SA, Jones RN, Castanheira M. Geographic variations in species distribution and echinocandin and azole antifungal resistance rates among Candida bloodstream infection isolates: report from the SENTRY Antimicrobial Surveillance Program (2008 to 2009) J Clin Microbiol. 2011;49(1):396–399. doi: 10.1128/JCM.01398-10. doi:JCM.01398-10 [pii] 10.1128/JCM.01398-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Castanheira M, Woosley LN, Diekema DJ, Messer SA, Jones RN, Pfaller MA. Low prevalence of fks1 hot spot 1 mutations in a worldwide collection of Candida strains. Antimicrobial agents and chemotherapy. 2010;54(6):2655–2659. doi: 10.1128/AAC.01711-09. doi:AAC.01711-09 [pii] 10.1128/AAC.01711-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alexander BD, Johnson MD, Pfeiffer CD, Jimenez-Ortigosa C, Catania J, Booker R, et al. Increasing echinocandin resistance in Candida glabrata: clinical failure correlates with presence of FKS mutations and elevated minimum inhibitory concentrations. Clin Infect Dis. 2013;56(12):1724–1732. doi: 10.1093/cid/cit136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pfaller MA, Castanheira M, Lockhart SR, Ahlquist AM, Messer SA, Jones RN. Frequency of decreased susceptibility and resistance to echinocandins among fluconazole-resistant bloodstream isolates of Candida glabrata. J Clin Microbiol. 2012;50(4):1199–1203. doi: 10.1128/JCM.06112-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lortholary O, Desnos-Ollivier M, Sitbon K, Fontanet A, Bretagne S, Dromer F. Recent exposure to caspofungin or fluconazole influences the epidemiology of candidemia: a prospective multicenter study involving 2,441 patients. Antimicrobial agents and chemotherapy. 2011;55(2):532–538. doi: 10.1128/AAC.01128-10. doi:AAC.01128-10 [pii] 10.1128/AAC.01128-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fekkar A, Meyer I, Brossas JY, Dannaoui E, Palous M, Uzunov M, et al. Rapid emergence of echinocandin resistance during Candida kefyr fungemia treatment with caspofungin. Antimicrob Agents Chemother. 2013;57(5):2380–2382. doi: 10.1128/AAC.02037-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pfaller MA, Castanheira M, Lockhart SR, Ahlquist AM, Messer SA, Jones RN. Frequency of Decreased Susceptibility and Resistance to Echinocandins Among Fluconazole-Resistant Bloodstream Isolates of Candida glabrata: Results from the SENTRY Antimicrobial Surveillance Program (2006–2010) and the Centers for Disease Control and Prevention Population-Based Surveillance (2008–2010) J Clin Microbiol. 2012 doi: 10.1128/JCM.06112-11. doi:JCM.06112-11 [pii] 10.1128/JCM.06112-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Arendrup MC, Perkhofer S, Howard SJ, Garcia-Effron G, Vishukumar A, Perlin D, et al. Establishing in vitro-in vivo correlations for Aspergillus fumigatus: the challenge of azoles versus echinocandins. Antimicrob Agents Chemother. 2008;52(10):3504–3511. doi: 10.1128/AAC.00190-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Balajee SA, Gribskov JL, Hanley E, Nickle D, Marr KA. Aspergillus lentulus sp, nov., a new sibling species of A. fumigatus. Eukaryot Cell. 2005;4(3):625–632. doi: 10.1128/EC.4.3.625-632.2005. doi:4/3/625 [pii] 10.1128/EC.4.3.625-632.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Katiyar S, Pfaller M, Edlind T. Candida albicans and Candida glabrata clinical isolates exhibiting reduced echinocandin susceptibility. Antimicrobial agents and chemotherapy. 2006;50(8):2892–2894. doi: 10.1128/AAC.00349-06. doi:50/8/2892 [pii] 10.1128/AAC.00349-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lackner M, Tscherner M, Schaller M, Kuchler K, Mair C, Sartori B, et al. Position and numbers of FKS mutations in C. albicans selectively influence in vitro and in vivo susceptibility to echinocandin treatment. Antimicrob Agents Chemother. 2014 doi: 10.1128/AAC.00123-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shields RK, Nguyen MH, Press EG, Kwa AL, Cheng S, Du C, et al. The presence of an FKS mutation rather than MIC is an independent risk factor for failure of echinocandin therapy among patients with invasive candidiasis due to Candida glabrata. Antimicrob Agents Chemother. 2012;56(9):4862–4869. doi: 10.1128/AAC.00027-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Johnson ME, Katiyar SK, Edlind TD. A new Fks hotspot for acquired echinocandin resistance in yeast, and its contribution to intrinsic resistance of Scedosporium species. Antimicrobial agents and chemotherapy. 2011 doi: 10.1128/AAC.01811-10. doi:AAC.01811-10 [pii] 10.1128/AAC.01811-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Katiyar SK, Edlind TD. Role for Fks1 in the intrinsic echinocandin resistance of Fusarium solani as evidenced by hybrid expression in Saccharomyces cerevisiae. Antimicrobial agents and chemotherapy. 2009;53(5):1772–1778. doi: 10.1128/AAC.00020-09. doi:AAC.00020-09 [pii] 10.1128/AAC.00020-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Perlin DS. Echinocandin-resistant Candida: molecular methods and phenotypes. Curr Fungal Infect Rep. 2011;5:113–119. [Google Scholar]
- 72.Arendrup MC, Perlin DS, Jensen RH, Howard SJ, Goodwin J, Hope W. Differential In vivo activity of Anidulafungin, Caspofungin and Micafungin against C. glabrata with and without FKS resistance mutations. Antimicrobial agents and chemotherapy. 2012 doi: 10.1128/AAC.06369-11. doi:AAC.06369-11 [pii] 10.1128/AAC.06369-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Howard SJ, Lestner JM, Sharp A, Gregson L, Goodwin J, Slater J, et al. Pharmacokinetics and pharmacodynamics of posaconazole for invasive pulmonary aspergillosis: clinical implications for antifungal therapy. J Infect Dis. 2011;203(9):1324–1332. doi: 10.1093/infdis/jir023. doi:jir023 [pii] 10.1093/infdis/jir023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Slater JL, Howard SJ, Sharp A, Goodwin J, Gregson LM, Alastruey-Izquierdo A, et al. Disseminated Candidiasis Caused by Candida albicans with Amino Acid Substitutions in Fks1 at Position Ser645 Cannot Be Successfully Treated with Micafungin. Antimicrob Agents Chemother. 2011;55(7):3075–3083. doi: 10.1128/AAC.01686-10. doi:AAC.01686-10 [pii] 10.1128/AAC.01686-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wiederhold NP, Najvar LK, Bocanegra RA, Kirkpatrick WR, Patterson TF. Caspofungin dose escalation for invasive candidiasis due to resistant Candida albicans. Antimicrobial agents and chemotherapy. 2011;55(7):3254–3260. doi: 10.1128/AAC.01750-10. doi:10.1128/AAC.01750-10 AAC.01750-10 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Castanheira M, Woosley LN, Messer SA, Diekema DJ, Jones RN, Pfaller MA. Frequency of fks mutations among Candida glabrata isolates from a 10-year global collection of bloodstream infection isolates. Antimicrob Agents Chemother. 2014;58(1):577–580. doi: 10.1128/AAC.01674-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Eng WK, Faucette L, McLaughlin MM, Cafferkey R, Koltin Y, Morris RA, et al. The yeast FKS1 gene encodes a novel membrane protein, mutations in which confer FK506 and cyclosporin A hypersensitivity and calcineurin-dependent growth. Gene. 1994;151(1–2):61–71. doi: 10.1016/0378-1119(94)90633-5. [DOI] [PubMed] [Google Scholar]
- 78.Jensen RH, Johansen HK, Arendrup MC. Stepwise development of a homozygous S80P substitution in Fks1p, conferring echinocandin resistance in Candida tropicalis. Antimicrob Agents Chemother. 2013;57(1):614–617. doi: 10.1128/AAC.01193-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pasquale T, Tomada JR, Ghannoun M, Dipersio J, Bonilla H. Emergence of Candida tropicalis resistant to caspofungin. J Antimicrob Chemother. 2008;61(1):219. doi: 10.1093/jac/dkm453. [DOI] [PubMed] [Google Scholar]
- 80.Johnson ME, Katiyar SK, Edlind TD. New Fks hot spot for acquired echinocandin resistance in Saccharomyces cerevisiae and its contribution to intrinsic resistance of Scedosporium species. Antimicrobial agents and chemotherapy. 2011;55(8):3774–3781. doi: 10.1128/AAC.01811-10. doi:AAC.01811-10 [pii] 10.1128/AAC.01811-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ben-Ami R, Garcia-Effron G, Lewis RE, Gamarra S, Leventakos K, Perlin DS, et al. The fitness and virulence cost of fks1 mutations causing echinocandin-resistance in Candida albicans. The Journal of Infectious Diseases. 2011 doi: 10.1093/infdis/jir351. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.d'Enfert C. Biofilms and their role in the resistance of pathogenic Candida to antifungal agents. Curr Drug Targets. 2006;7(4):465–470. doi: 10.2174/138945006776359458. [DOI] [PubMed] [Google Scholar]
- 83.Mitchell KF, Taff HT, Cuevas MA, Reinicke EL, Sanchez H, Andes DR. Role of matrix beta-1,3 glucan in antifungal resistance of non-albicans Candida biofilms. Antimicrob Agents Chemother. 2013;57(4):1918–1920. doi: 10.1128/AAC.02378-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Desai JV, Bruno VM, Ganguly S, Stamper RJ, Mitchell KF, Solis N, et al. Regulatory role of glycerol in Candida albicans biofilm formation. MBio. 2013;4(2):e00637–e00612. doi: 10.1128/mBio.00637-12. doi:10.1128/mBio.00637-12 e00637-12 [pii] mBio.00637-12 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Odabasi Z, Paetznick V, Rex JH, Ostrosky-Zeichner L. Effects of serum on in vitro susceptibility testing of echinocandins. Antimicrob Agents Chemother. 2007;51(11):4214–4216. doi: 10.1128/AAC.01589-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Paderu P, Garcia-Effron G, Balashov S, Delmas G, Park S, Perlin DS. Serum differentially alters the antifungal properties of echinocandin drugs. Antimicrob Agents Chemother. 2007;51(6):2253–2256. doi: 10.1128/AAC.01536-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wiederhold NP, Najvar LK, Bocanegra R, Molina D, Olivo M, Graybill JR. In vivo efficacy of anidulafungin and caspofungin against Candida glabrata and association with in vitro potency in the presence of sera. Antimicrob Agents Chemother. 2007;51(5):1616–1620. doi: 10.1128/AAC.00105-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Foldi R, Szilagyi J, Kardos G, Berenyi R, Kovacs R, Majoros L. Effect of 50% human serum on the killing activity of micafungin against eight Candida species using time-kill methodology. Diagn Microbiol Infect Dis. 2012;73(4):338–342. doi: 10.1016/j.diagmicrobio.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 89.Kovacs R, Gesztelyi R, Berenyi R, Doman M, Kardos G, Juhasz B, et al. Killing rates exerted by caspofungin in 50 % serum and its correlation with in vivo efficacy in a neutropenic murine model against Candida krusei and Candida inconspicua. J Med Microbiol. 2014;63(Pt 2):186–194. doi: 10.1099/jmm.0.066381-0. [DOI] [PubMed] [Google Scholar]
- 90.Perlin DS. Resistance to echinocandin-class antifungal drugs. Drug Resist Updat. 2007;10(3):121–130. doi: 10.1016/j.drup.2007.04.002. doi:S1368-7646(07)00040-4 [pii] 10.1016/j.drup.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Walker LA, Gow NA, Munro CA. Fungal echinocandin resistance. Fungal Genet Biol. 2010;47(2):117–126. doi: 10.1016/j.fgb.2009.09.003. doi:S1087-1845(09)00165-0 [pii] 10.1016/j.fgb.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Munro CA, Selvaggini S, de Bruijn I, Walker L, Lenardon MD, Gerssen B, et al. The PKC, HOG and Ca2+ signalling pathways co-ordinately regulate chitin synthesis in Candida albicans. Molecular microbiology. 2007;63(5):1399–1413. doi: 10.1111/j.1365-2958.2007.05588.x. doi:MMI5588 [pii] 10.1111/j.1365-2958.2007.05588.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Walker LA, Munro CA, de Bruijn I, Lenardon MD, McKinnon A, Gow NA. Stimulation of chitin synthesis rescues Candida albicans from echinocandins. PLoS Pathog. 2008;4(4):e1000040. doi: 10.1371/journal.ppat.1000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Singh SD, Robbins N, Zaas AK, Schell WA, Perfect JR, Cowen LE. Hsp90 governs echinocandin resistance in the pathogenic yeast Candida albicans via calcineurin. PLoS Pathog. 2009;5(7):e1000532. doi: 10.1371/journal.ppat.1000532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Singh-Babak SD, Babak T, Diezmann S, Hill JA, Xie JL, Chen YL, et al. Global analysis of the evolution and mechanism of echinocandin resistance in Candida glabrata. PLoS Pathog. 2012;8(5):e1002718. doi: 10.1371/journal.ppat.1002718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gow NA, Netea MG, Munro CA, Ferwerda G, Bates S, Mora-Montes HM, et al. Immune recognition of Candida albicans beta-glucan by dectin-1. J Infect Dis. 2007;196(10):1565–1571. doi: 10.1086/523110. doi:JID38665 [pii] 10.1086/523110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Plaine A, Walker L, Da Costa G, Mora-Montes HM, McKinnon A, Gow NA, et al. Functional analysis of Candida albicans GPI-anchored proteins: roles in cell wall integrity and caspofungin sensitivity. Fungal Genet Biol. 2008;45(10):1404–1414. doi: 10.1016/j.fgb.2008.08.003. doi:S1087-1845(08)00159-X [pii] 10.1016/j.fgb.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lee KK, Maccallum DM, Jacobsen MD, Walker LA, Odds FC, Gow NA, et al. Elevated cell wall chitin in Candida albicans confers echinocandin resistance in vivo. Antimicrobial agents and chemotherapy. 2012;56(1):208–217. doi: 10.1128/AAC.00683-11. doi:AAC.00683-11 [pii] 10.1128/AAC.00683-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Stevens DA, Ichinomiya M, Koshi Y, Horiuchi H. Escape of Candida from caspofungin inhibition at concentrations above the MIC (paradoxical effect) accomplished by increased cell wall chitin; evidence for beta-1,6-glucan synthesis inhibition by caspofungin. Antimicrobial agents and chemotherapy. 2006;50(9):3160–3161. doi: 10.1128/AAC.00563-06. doi:50/9/3160 [pii] 10.1128/AAC.00563-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Clemons KV, Espiritu M, Parmar R, Stevens DA. Assessment of the paradoxical effect of caspofungin in therapy of candidiasis. Antimicrobial agents and chemotherapy. 2006;50(4):1293–1297. doi: 10.1128/AAC.50.4.1293-1297.2006. doi:50/4/1293 [pii] 10.1128/AAC.50.4.1293-1297.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Stevens DA, Espiritu M, Parmar R. Paradoxical effect of caspofungin: reduced activity against Candida albicans at high drug concentrations. Antimicrobial agents and chemotherapy. 2004;48(9):3407–3411. doi: 10.1128/AAC.48.9.3407-3411.2004. doi:10.1128/AAC.48.9.3407-3411.2004 48/9/3407 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Healey KR, Katiyar SK, Raj S, Edlind TD. CRS-MIS in Candida glabrata: sphingolipids modulate echinocandin-Fks interaction. Mol Microbiol. 2012;86(2):303–313. doi: 10.1111/j.1365-2958.2012.08194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Healey KR, Katiyar SK, Castanheira M, Pfaller MA, Edlind TD. Candida glabrata mutants demonstrating paradoxical reduced caspofungin susceptibility but increased micafungin susceptibility. Antimicrobial agents and chemotherapy. 2011;55(8):3947–3949. doi: 10.1128/AAC.00044-11. doi:10.1128/AAC.00044-11 AAC.00044-11 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rex JH, Pfaller MA. Has antifungal susceptibility testing come of age? Clin Infect Dis. 2002;35(8):982–989. doi: 10.1086/342384. [DOI] [PubMed] [Google Scholar]
- 105.Arendrup MC, Garcia-Effron G, Lass-Florl C, Lopez AG, Rodriguez-Tudela JL, Cuenca-Estrella M, et al. Echinocandin susceptibility testing of Candida species: comparison of EUCAST EDef 7.1, CLSI M27-A3, Etest, disk diffusion, and agar dilution methods with RPMI and isosensitest media. Antimicrob Agents Chemother. 2010;54(1):426–439. doi: 10.1128/AAC.01256-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Pfaller MA, Castanheira M, Messer SA, Rhomberg PR, Jones RN. Comparison of EUCAST and CLSI broth microdilution methods for the susceptibility testing of 10 Systemically active antifungal agents when tested against Candida spp. Diagn Microbiol Infect Dis. 2014;79(2):198–204. doi: 10.1016/j.diagmicrobio.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 107.Andes D, Diekema DJ, Pfaller MA, Bohrmuller J, Marchillo K, Lepak A. In vivo comparison of the pharmacodynamic targets for echinocandin drugs against Candida species. Antimicrob Agents Chemother. 2010;54(6):2497–2506. doi: 10.1128/AAC.01584-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Akache B, MacPherson S, Sylvain M-A, Turcotte B. Complex interplay among regulators of drug resistance genes in Saccharomyces cerevisiae. J Biol Chem. 2004;279(27):27855–27860. doi: 10.1074/jbc.M403487200. [DOI] [PubMed] [Google Scholar]
- 109.Eschenauer GA, Nguyen MH, Shoham S, Vazquez JA, Morris AJ, Pasculle WA, et al. Real-world experience with echinocandin MICs against Candida species in a multicenter study of hospitals that routinely perform susceptibility testing of bloodstream isolates. Antimicrob Agents Chemother. 2014;58(4):1897–1906. doi: 10.1128/AAC.02163-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Espinel-Ingroff A, Arendrup MC, Pfaller MA, Bonfietti LX, Bustamante B, Canton E, et al. Interlaboratory variability of Caspofungin MICs for Candida spp. Using CLSI and EUCAST methods: should the clinical laboratory be testing this agent? Antimicrob Agents Chemother. 2013;57(12):5836–5842. doi: 10.1128/AAC.01519-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ben-Ami R, Hilerowicz Y, Novikov A, Giladi M. The impact of new epidemiological cutoff values on Candida glabrata resistance rates and concordance between testing methods. Diagn Microbiol Infect Dis. 2014;79(2):209–213. doi: 10.1016/j.diagmicrobio.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 112.Turnidge J, Kahlmeter G, Kronvall G. Statistical characterisation of bacterial wild-type MIC value distributions and the determination of epidemiological cut-off values. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2006;12(5):418–425. doi: 10.1111/j.1469-0691.2006.01377.x. [DOI] [PubMed] [Google Scholar]
- 113.Arendrup MC, Rodriguez-Tudela JL, Lass-Florl C, Cuenca-Estrella M, Donnelly JP, Hope W, et al. EUCAST technical note on anidulafungin. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2011;17(11):E18–E20. doi: 10.1111/j.1469-0691.2011.03647.x. [DOI] [PubMed] [Google Scholar]
- 114.Arendrup MC, Cuenca-Estrella M, Lass-Florl C, Hope WW. Breakpoints for antifungal agents: An update from EUCAST focussing on echinocandins against Candida spp. and triazoles against Aspergillus spp. Drug Resist Updat. 2013;16(6):81–95. doi: 10.1016/j.drup.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 115.Perlin DS. Antifungal drug resistance: do molecular methods provide a way forward? Curr Opin Infect Dis. 2009;22(6):568–573. doi: 10.1097/QCO.0b013e3283321ce5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Slavin MA, Osborne B, Adams R, Levenstein MJ, Schoch HG, Feldman AR, et al. Efficacy and safety of fluconazole prophylaxis for fungal infections after marrow transplantation--a prospective, randomized, double-blind study. J Infect Dis. 1995;171(6):1545–1552. doi: 10.1093/infdis/171.6.1545. [DOI] [PubMed] [Google Scholar]
- 117.Marr KA, Seidel K, Slavin MA, Bowden RA, Schoch HG, Flowers ME, et al. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Blood. 2000;96(6):2055–2061. [PubMed] [Google Scholar]
- 118.Marr KA. Primary antifungal prophylaxis in hematopoietic stem cell transplant recipients: clinical implications of recent studies. Curr Opin Infect Dis. 2008;21(4):409–414. doi: 10.1097/QCO.0b013e328307c7d9. [DOI] [PubMed] [Google Scholar]
- 119.de la Torre P, Reboli AC. Micafungin: an evidence-based review of its place in therapy. Core Evid. 2014;9:27–39. doi: 10.2147/CE.S36304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.van Burik JA, Ratanatharathorn V, Stepan DE, Miller CB, Lipton JH, Vesole DH, et al. Micafungin versus fluconazole for prophylaxis against invasive fungal infections during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis. 2004;39(10):1407–1416. doi: 10.1086/422312. [DOI] [PubMed] [Google Scholar]
- 121.Chou LS, Lewis RE, Ippoliti C, Champlin RE, Kontoyiannis DP. Caspofungin as primary antifungal prophylaxis in stem cell transplant recipients. Pharmacotherapy. 2007;27(12):1644–1650. doi: 10.1592/phco.27.12.1644. [DOI] [PubMed] [Google Scholar]
- 122.Mattiuzzi GN, Alvarado G, Giles FJ, Ostrosky-Zeichner L, Cortes J, O'Brien S, et al. Open-label, randomized comparison of itraconazole versus caspofungin for prophylaxis in patients with hematologic malignancies. Antimicrob Agents Chemother. 2006;50(1):143–147. doi: 10.1128/AAC.50.1.143-147.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Doring M, Hartmann U, Erbacher A, Lang P, Handgretinger R, Muller I. Caspofungin as antifungal prophylaxis in pediatric patients undergoing allogeneic hematopoietic stem cell transplantation: a retrospective analysis. BMC Infect Dis. 2012;12:151. doi: 10.1186/1471-2334-12-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ziakas PD, Kourbeti IS, Mylonakis E. Systemic antifungal prophylaxis after hematopoietic stem cell transplantation: a meta-analysis. Clin Ther. 2014;36(2):292–306. e1. doi: 10.1016/j.clinthera.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 125.Xu SX, Shen JL, Tang XF, Feng B. Newer antifungal agents for fungal infection prevention during hematopoietic cell transplantation: a meta-analysis. Transplant Proc. 2013;45(1):407–414. doi: 10.1016/j.transproceed.2012.07.149. [DOI] [PubMed] [Google Scholar]
- 126.Scott LJ. Micafungin: a review of its use in the prophylaxis and treatment of invasive Candida infections. Drugs. 2012;72(16):2141–2165. doi: 10.2165/11209970-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 127.Cornely OA, Bassetti M, Calandra T, Garbino J, Kullberg BJ, Lortholary O, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: non-neutropenic adult patients. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2012;18(Suppl 7):19–37. doi: 10.1111/1469-0691.12039. [DOI] [PubMed] [Google Scholar]
- 128.Hope WW, Castagnola E, Groll AH, Roilides E, Akova M, Arendrup MC, et al. ESCMID* guideline for the diagnosis and management of Candida diseases 2012: prevention and management of invasive infections in neonates and children caused by Candida spp. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2012;18(Suppl 7):38–52. doi: 10.1111/1469-0691.12040. [DOI] [PubMed] [Google Scholar]
- 129.Bizerra FC, Jimenez-Ortigosa C, Souza AC, Breda GL, Queiroz-Telles F, Perlin DS, et al. Breakthrough candidemia due to multidrug-resistant Candida glabrata during prophylaxis with a low dose of micafungin. Antimicrob Agents Chemother. 2014;58(4):2438–2440. doi: 10.1128/AAC.02189-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ruggero MA, Topal JE. Development of echinocandin-resistant Candida albicans candidemia following brief prophylactic exposure to micafungin therapy. Transpl Infect Dis. 2014 doi: 10.1111/tid.12230. [DOI] [PubMed] [Google Scholar]
- 131.Gomes MZ, Jiang Y, Mulanovich VE, Lewis RE, Kontoyiannis DP. Effectiveness of primary anti-Aspergillus prophylaxis during remission induction chemotherapy of acute myeloid leukemia. Antimicrob Agents Chemother. 2014;58(5):2775–2780. doi: 10.1128/AAC.01527-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Fekkar A, Dannaoui E, Meyer I, Imbert S, Brossas JY, Uzunov M, et al. Emergence of echinocandin-resistant Candida spp. in a hospital setting: a consequence of 10 years of increasing use of antifungal therapy? Eur J Clin Microbiol Infect Dis. 2014 doi: 10.1007/s10096-014-2096-9. [DOI] [PubMed] [Google Scholar]
- 133.Shin JH, Chae MJ, Song JW, Jung SI, Cho D, Kee SJ, et al. Changes in karyotype and azole susceptibility of sequential bloodstream isolates from patients with Candida glabrata candidemia. J Clin Microbiol. 2007;45(8):2385–2391. doi: 10.1128/JCM.00381-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clinical microbiology reviews. 2007;20(1):133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Koh AY, Kohler JR, Coggshall KT, Van Rooijen N, Pier GB. Mucosal damage and neutropenia are required for Candida albicans dissemination. PLoS pathogens. 2008;4(2):e35. doi: 10.1371/journal.ppat.0040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kennedy MJ, Volz PA, Edwards CA, Yancey RJ. Mechanisms of association of Candida albicans with intestinal mucosa. Journal of medical microbiology. 1987;24(4):333–341. doi: 10.1099/00222615-24-4-333. [DOI] [PubMed] [Google Scholar]
- 137.Magill SS, Swoboda SM, Johnson EA, Merz WG, Pelz RK, Lipsett PA, et al. The association between anatomic site of Candida colonization, invasive candidiasis, and mortality in critically ill surgical patients. Diagnostic microbiology and infectious disease. 2006;55(4):293–301. doi: 10.1016/j.diagmicrobio.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 138.Magill SS, Swoboda SM, Shields CE, Colantuoni EA, Fothergill AW, Merz WG, et al. The epidemiology of Candida colonization and invasive candidiasis in a surgical intensive care unit where fluconazole prophylaxis is utilized: follow-up to a randomized clinical trial. Annals of surgery. 2009;249(4):657–665. doi: 10.1097/SLA.0b013e31819ed914. [DOI] [PubMed] [Google Scholar]
- 139.Miranda LN, van der Heijden IM, Costa SF, Sousa AP, Sienra RA, Gobara S, et al. Candida colonisation as a source for candidaemia. The Journal of hospital infection. 2009;72(1):9–16. doi: 10.1016/j.jhin.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 140.Voss A, Hollis RJ, Pfaller MA, Wenzel RP, Doebbeling BN. Investigation of the sequence of colonization and candidemia in nonneutropenic patients. Journal of clinical microbiology. 1994;32(4):975–980. doi: 10.1128/jcm.32.4.975-980.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Richet HM, Andremont A, Tancrede C, Pico JL, Jarvis WR. Risk factors for candidemia in patients with acute lymphocytic leukemia. Reviews of infectious diseases. 1991;13(2):211–215. doi: 10.1093/clinids/13.2.211. [DOI] [PubMed] [Google Scholar]
- 142.Reagan DR, Pfaller MA, Hollis RJ, Wenzel RP. Characterization of the sequence of colonization and nosocomial candidemia using DNA fingerprinting and a DNA probe. Journal of clinical microbiology. 1990;28(12):2733–2738. doi: 10.1128/jcm.28.12.2733-2738.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Harriott MM, Noverr MC. Importance of Candida-bacterial polymicrobial biofilms in disease. Trends Microbiol. 2011;19(11):557–563. doi: 10.1016/j.tim.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ramage G, Mowat E, Jones B, Williams C, Lopez-Ribot J. Our current understanding of fungal biofilms. Crit Rev Microbiol. 2009;35(4):340–355. doi: 10.3109/10408410903241436. [DOI] [PubMed] [Google Scholar]
- 145.Cheng S, clancy C, Hartman D, Hao B, Nguyen M. Candida glabrata intra-abdominal candidiasis is characterized by persistence within the peritoneal cavity and abscesses. Infect Immun. 2014 May 05; doi: 10.1128/IAI.00062-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Andes DR, Reynolds DK, Van Wart SA, Lepak AJ, Kovanda LL, Bhavnani SM. Clinical pharmacodynamic index identification for micafungin in esophageal candidiasis: dosing strategy optimization. Antimicrob Agents Chemother. 2013;57(11):5714–5716. doi: 10.1128/AAC.01057-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Gumbo T, Drusano GL, Liu W, Kulawy RW, Fregeau C, Hsu V, et al. Once-weekly micafungin therapy is as effective as daily therapy for disseminated candidiasis in mice with persistent neutropenia. Antimicrob Agents Chemother. 2007;51(3):968–974. doi: 10.1128/AAC.01337-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Drlica K. The mutant selection window and antimicrobial resistance. J Antimicrob Chemother. 2003;52(1):11–17. doi: 10.1093/jac/dkg269. [DOI] [PubMed] [Google Scholar]
- 149.Drlica K, Zhao X. Mutant selection window hypothesis updated. Clin Infect Dis. 2007;44(5):681–688. doi: 10.1086/511642. [DOI] [PubMed] [Google Scholar]