Abstract
Background
Persistent disparities in access and quality of mental health care for Latinos indicate a need for evidence-based, culturally adapted and outside-the-clinic-walls treatments.
Objective
Evaluate treatment effectiveness of telephone (ECLA –T) or face-to-face (ECLA-F) delivery of a 6–8 session cognitive behavioral therapy and care-management intervention for low-income Latinos, as compared to usual care for depression.
Design
Multi-site randomized controlled trial.
Setting
Eight community health clinics in Boston, Massachusetts and San Juan, Puerto Rico.
Participants
257 Latino patients recruited from primary care between May 2011 and September 2012.
Main Outcome Measures
The primary outcome was severity of depression, assessed with the Patient Health Questionnaire-9 (PHQ-9) and the Hopkins Symptom Checklist-20 (HSCL-20). The secondary outcome was functioning over the previous 30 days, measured using the World Health Organization Disability Assessment Schedule (WHO-DAS 2.0).
Results
Both telephone and face-to-face versions of the ECLA were more effective than usual care. The effect sizes of both intervention conditions on PHQ-9 were moderate when combined data from both sites are analyzed (.56 and .64 for face-to-face and telephone, respectively). Similarly, effect sizes of ECLA-F and ECLA-T on the HSCL were quite large in the Boston site (.64 and .73. respectively) but not in Puerto Rico (.10 and .03).
Conclusions and Relevance
The intervention appears to help Latino patients reduce depressive symptoms and improve functioning. Of particular importance is the higher treatment initiation for the telephone vs. face-to-face intervention (89.7% vs. 78.8%), which suggests that telephone-based care may improve access and quality of care.
Introduction
Although evidence-based depression treatments have shown benefits to ethnic and racial minorities, (1) there are enduring disparities in depression treatment for Latinos, (2–4) as evidenced by problems in access to care, (5, 6) early dropout, and high rates of missed follow-up appointments. (7–10) Additional barriers include: lack of ethnic/racial and language matching between patient and provider, (11) cultural mistrust of the health care system, (12) and service inadequacies (e.g. long treatments, insufficient tailoring for low literacy). (5, 13) Demand for mental health services for Latinos has already outgrown available supply, (11) and the Latino population’s projected growth of 30% by 2050(14) indicates that treatment needs vastly exceed current availability. Alternative ways of delivering evidence-based and culturally adapted care that accommodate Latinos’ life circumstances are sorely needed.
One strategy for improving clinical outcomes has been the use of telephone-based psychotherapeutic interventions. (15–17) Studies have demonstrated (16–19) that telephone-based psychotherapy can lower depression scores at follow-up and improve self-reported mood, reducing barriers to care among low-income minority patients. A pilot study for Latinos in rural Washington state (20) found that participants appreciated the convenience and privacy of telephone-based therapy and were more likely to complete all 6 treatment sessions (44%)(20) compared to a similar in-person treatment (36%). (21) Recent studies have been conducted for perinatal depression among Latinas (22) and for depression among HIV+ minority patients. (23) However, these typically do not compare telephone versus face-to-face, nor include more than one site. Given the heterogeneity of the Latino population, and geographical variations in access and quality, there is a critical need for more research on telephone psychotherapy to identify groups that will benefit from its implementation.
We conduct the “Comparando Estrategias para Reducir el Estres y la Depresion” (CERED) study to contribute to the comparative effectiveness field, while supporting improvement efforts in depression care for Latinos. The study compares the outcomes of an evidence-based cognitive behavioral therapy (CBT) and care management intervention - delivered by telephone or face-to-face - to usual care, for Latino primary care patients. CBT plus care management was chosen because manualized CBT with proven effectiveness ensures that participants receive quality, evidence-based treatment while care management provides a resource to address system-level barriers like work schedule conflict, insurance difficulties or health system problems. A two-site design (Boston and San Juan) may increase generalizability of findings to Latino sub-ethnic groups (i.e., Puerto Ricans, South Americans) and at more than one geographical location. (24, 25)
Methods
Setting and Study Sample
Participants were recruited through direct contact in clinic waiting rooms or by positive screens for depression in primary care from multiple clinics in Greater Boston, Massachusetts and San Juan, Puerto Rico. Recruitment began in May 2011 and final interviews were conducted in September 2012. Boston participants were recruited from five community-based clinics serving a diverse population including many Latinos from Central America (67.5%), South America (11.9%), and Puerto Rico (11.1%). San Juan participants were mostly Puerto Ricans (85.0%) and Dominicans (15.0%) recruited from three large community health clinics for the low-income population. Clinics were chosen because they serve large numbers of Latinos, have history of research collaboration, and regularly screen using the Patient Health Questionnaire 9 item depression scale (PHQ-9). (26)
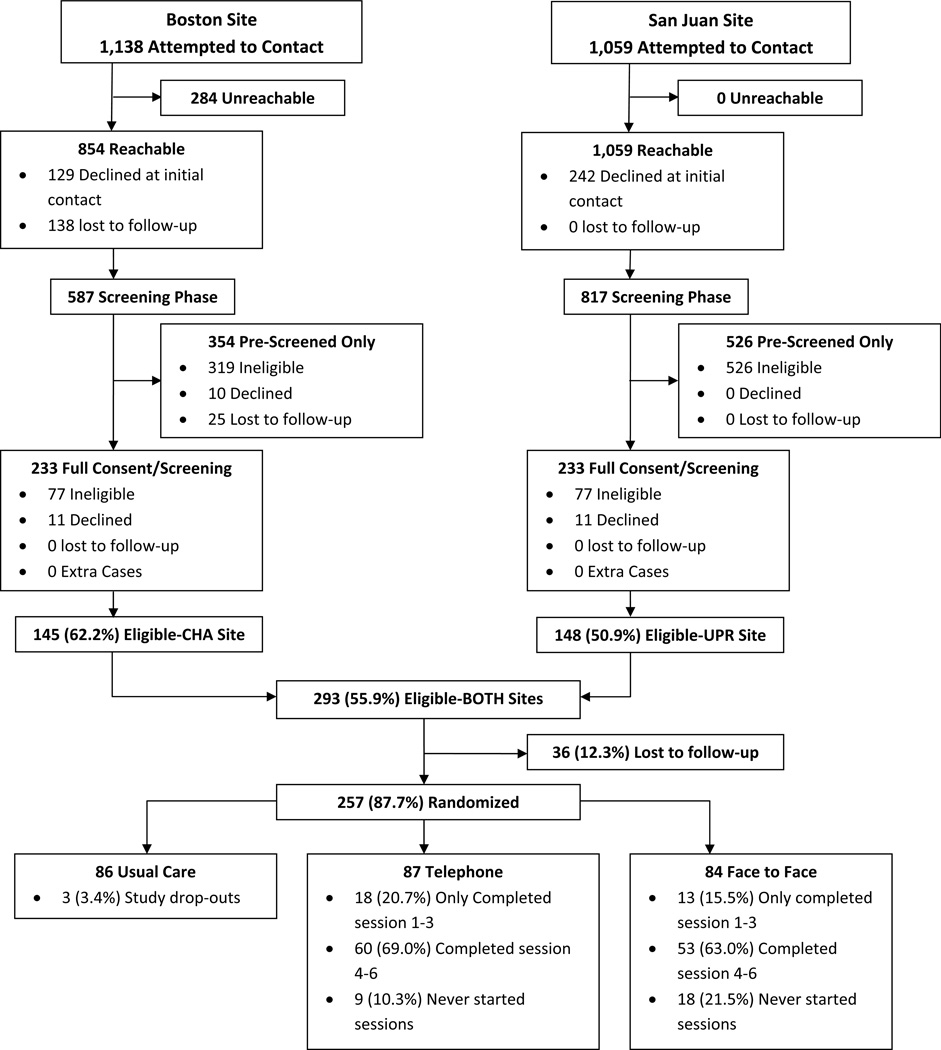
Nevertheless, there were site differences in care. In Puerto Rico, although clinics were supposed to screen for depression, this was not done, meaning all study patients were screened and recruited at the waiting areas by research staff. Those that met screening criteria were administered the baseline interview at the clinic. In Boston, where the PHQ-9 was given regularly, some patients were initially recruited through prior PHQ-9s, and some (N=284) could not be reached (see Figure 1). Baseline interviews were not all done in the clinics and thus 138 patients were lost to follow up after phone screening in Boston. Other site differences in usual care were related to the availability of psychotropic medication. Although primary care physicians can prescribe psychotropic medication, public insurance in Puerto Rico does not cover the payment unless prescribed by a psychiatrist. This restriction is not in place for the comparison patients in the Boston area.
Figure 1.
CERED ECLA CONSORT Diagram
CERED Intervention
CERED is an acronym for the Spanish phrase, “Comparando Estrategias para Reducir el Estres y la Depresion” which translates to “Comparing Strategies to Reduce Stress and Depression.” The CERED Engagement and Counseling for Latinos (ECLA) intervention has two formats: the ECLA-T (telephone) and ECLA-F (face to face). ECLA-T is based on a pilot study of a CBT telephone-plus care management intervention of 6–8 sessions provided to mainly Mexican patients at a rural family clinic (see Dwight Johnson et al.,) that has been shown to be effective in decreasing depressive symptoms, increasing client satisfaction, and improving self-perceived functioning (20). In this pilot study, CBT patients were more likely to have reduced PHQ-9 scores at the 6-month follow-up than controls, with an effect size of .53. ECLA was further adapted for the present study using interviews with the target population to condense and modify materials; add visual aids, culturally relevant metaphors, values, and proverbs; and lower health literacy requirements; with pilot testing and refining before the trial (see Ramos and Alegria, 2014) (27). ECLA-F involves the same adapted CBT intervention but delivered face-to-face. ECLA was also shorter than previous interventions (6 to 8 vs. 12 to 18 sessions). The intervention consisted of six modules focused on identifying and correcting negative cognitions, promoting behavioral activation, motivational interviewing to remain in care, and developing supportive relationships (see Appendix A, Supplemental Digital Content 1, http://links.lww.com/MLR/A816). All sessions were collaborative and tailored to patient needs in a structured format. Intervention patients were provided with a workbook and CBT exercises. The first four sessions were conducted weekly; the 5th and 6th were biweekly unless more immediate care was needed. Sessions were continued up to a total of 8. Cases that showed no improvement or deterioration were closely monitored in weekly supervision and patients in all groups were regularly assessed with the PHQ-9 and the Paykel suicide questionnaire. (28) Care Managers provided referral to social services, helped with scheduling, and connected clients with primary care providers if required (i.e. re-evaluation of medication side effects).
Study Design
Eligible patients were randomized after baseline to one of three conditions: 1) ECLA-T intervention, 2) ECLA-F intervention, and 3) usual care (see Figure 1). Participants randomized into usual care received the typical standard of care in that clinic, determined by the provider the participant was already seeing. It could include watchful waiting, prescription of antidepressants/anxiolytics (such as escitalopram, lorazepam, fluoxetine, paroxetine, and quetiapine, as shown in Table 2), or referral to a mental health clinician for psychotherapy or medication management, depending on severity and clinical opinion. All participants were called on a weekly basis to monitor depression.
Table 2.
Patient Demographics and Mental Health Scores by Site
| Boston | PR | ||||
|---|---|---|---|---|---|
| n=127 | % | n=130 | % | p-value | |
| Sex | |||||
| 1.male | 23 | 1 8% | 24 | 18% | 0.942 |
| 2.female | 104 | 82% | 106 | 82% | |
| Age | |||||
| 1.18–34yr | 36 | 28% | 28 | 22% | 0.022 |
| 2.35–49yr | 54 | 43% | 40 | 31% | |
| 3.50–64yr | 34 | 27% | 55 | 42% | |
| 4.>=65yr | 3 | 2% | 7 | 5% | |
| Race (Note: all are Latino) | |||||
| White | 30 | 24% | 43 | 33% | <0.001 |
| Black/Dark skinned | 25 | 20% | 61 | 47% | |
| Unreported (Latino) | 63 | 50% | 19 | 15% | |
| Mixed Race /Indian | 9 | 7% | 7 | 5% | |
| Education | |||||
| 1.6th grade or less | 45 | 35% | 13 | 10% | <0.001 |
| 2.7−11th grade | 36 | 28% | 38 | 29% | |
| 3.HS diploma, GED, voc. school or more | 46 | 36% | 79 | 61% | |
| Employment status | |||||
| 1.full-time | 31 | 24% | 11 | 8% | <0.001 |
| 2.part-time | 32 | 25% | 28 | 22% | |
| 3.unemployed | 27 | 21% | 18 | 14% | |
| 4.out of labor force | 25 | 20% | 60 | 46% | |
| 5.illness/disabled | 12 | 9% | 12 | 9% | |
| Personal Income | |||||
| 1.<15k | 76 | 60% | 120 | 92% | <0.001 |
| 2.15k−35k | 35 | 28% | 1 | 1% | |
| 3.35−75k | 10 | 8% | 0 | 0% | |
| Unreported | 6 | 5% | 9 | 7% | |
| US born | 19 | 15% | 99 | 76% | <0.001 |
| Medication use (baseline)* | 46 | 36% | 20 | 15% | <0.001 |
| Antidepressant use only(baseline) | 34 | 27% | 10 | 8% | 0.000 |
| Exposure to any trauma (baseline) | 105 | 83% | 112 | 86% | 0.442 |
| Baseline Mental Health scores | Mean | SD | Mean | SD | P-value |
| PHQ-9 | 16.20 | 3.87 | 17.22 | 4.57 | 0.057 |
| HCSL | 1.49 | 0.78 | 2.25 | 0.86 | <0.001 |
| WHO-DAS | 25.08 | 10.32 | 30.54 | 11.67 | <0.001 |
| PSWQ | 61.07 | 10.87 | 62.61 | 10.60 | 0.252 |
| SF12-physical | 38.64 | 10.03 | 34.69 | 10.28 | 0.002 |
| SF12-mental | 30.62 | 9.37 | 28.01 | 10.62 | 0.038 |
| RA3 Mental Health scores | |||||
| PHQ-9 | 8.15 | 6.19 | 11.93 | 6.88 | <0.001 |
| HCSL | 1.02 | 0.77 | 1.62 | 1.03 | <0.001 |
| WHO-DAS | 22.48 | 10.36 | 27.64 | 12.08 | 0.001 |
| PSWQ | 54.62 | 11.78 | 56.41 | 11.90 | 0.248 |
| SF12-physical | 41.86 | 9.21 | 35.04 | 10.79 | <0.001 |
| SF12-mental | 36.11 | 10.90 | 35.40 | 12.36 | 0.643 |
any medication due to problems with emotions, drug and alcohol use, nerves, energy level, concentration, sleep or ability to cope with stress
All participants were Latino primary care patients with moderate or severe depressive symptoms at baseline, assessed by a PHQ-9 score of 10 or greater, (26) and without receipt of specialty mental health care in the past 3 months or appointments in the next 2 months. The study was approved by the institutional review boards of the University of Puerto Rico and the Cambridge Health Alliance.
Research Procedures
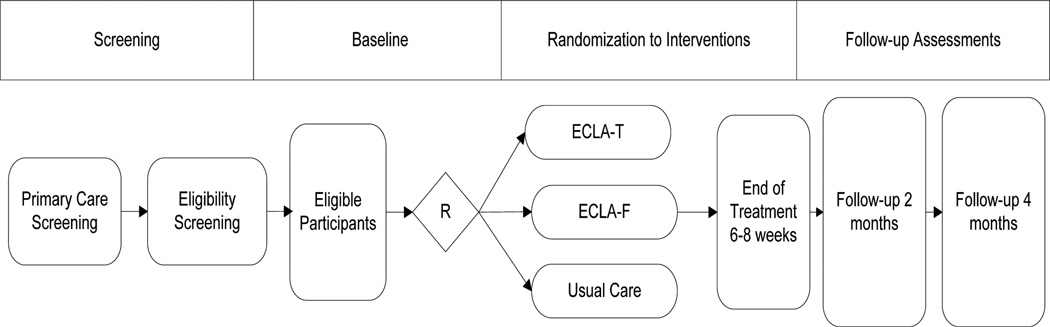
Bilingual research assistants recruited patients, obtained informed consent, and conducted follow-up assessments blind to treatment condition. Figure 2 depicts the process. (29) After screening and consent, 257 eligible Latino patients were randomized to ECLA-T (n=87), ECLA-F (n=84), or usual care (n=86). After randomization, some patients in all arms missed all research assessments. Consequently, the sample for the primary outcome completer analyses consisted of 233 individuals, whose observations were used to impute missing values and create a dataset with 257 observations. Two months after baseline, patients completed a follow-up assessment. Baseline measurements were repeated and working alliance, communication, and treatment effectiveness were assessed. At four months from baseline, we replicated the two-month assessment and included additional questions on satisfaction and treatment experience. We also contacted usual care participants weekly to administer the PHQ-9, Paykel Suicide Scale and monitor safety.
Figure 2.
Description of Research Design
Measures
Primary outcomes for effectiveness were scores on the Patient Health Questionnaire (PHQ-9) (26) and the Hopkins Symptom Checklist (HSCL-20). (30) The PHQ-9 is a nine-item depression scale used in screening for probable depression and monitoring treatment progress. (31, 32) The HSCL-20 is a widely used (33–36) measure of depression and distress that tracks clinical symptom change. Both have excellent reliability and validity in Latino samples. (37, 38) The secondary outcome was the World Health Organization Disability Assessment Schedule (WHO-DAS 2), of past 30 day functioning. Previous versions of the WHO-DAS have (39) showed good to excellent internal consistency (α = .72 to .97). (40)
Screening and Assessments
Patients from participating clinics were contacted by a research assistant to participate in a full assessment, including informed consent, PHQ-9, and eligibility questions. Eligible patients were Latinos, at least 18 years of age, who scored 10 or more on the PHQ-9 and met at least one essential criteria for Major Depressive Disorder (MDD): at least two weeks of depressed mood or loss of interest in the last year. (41) Exclusion criteria included psychosis history, use of specialty care within the 3 months prior to baseline or a mental health appointment within the next two months, inability to demonstrate capacity to consent (assessed with a screener), or evidence of suicidal thoughts or ideation as measured by an affirmative response to questions 4 or 5 on the Paykel Suicide Questionnaire. (42)
The baseline interview, administered prior to randomization, assessed depressive symptoms, (26) anxiety symptoms (Penn State Worry Questionnaire), (43, 44) trauma history (PTSD-PC), (45) medication use, alcohol and illicit drug use, (46) functional impairment, (39) and physical comorbidities. (47) Sociodemographic and clinical information (age, gender, education, insurance, marital history, immigration history, health literacy, previous clinical history, etc.) were also collected.
Clinician Training
All training procedures and supervision were carried out in the same way across sites. Six clinicians participated in the Boston area, including one post-doctoral level psychologist, two master’s level psychologists, two licensed social workers, and one counselor. All were female and Latino and four had prior CBT experience. In San Juan, all clinicians were licensed PhDs in psychology because social workers and other providers are not commonly reimbursed for providing psychotherapy in Puerto Rico. There were six female and one male therapist in Puerto Rico, and all were Latino.
Clinicians participated in HIPAA and CBT training consisting of at least 12 hours of didactic instruction and role play and recorded observations of at least 6 sessions with two cases. Weekly supervision calls, led by two psychiatrists at each site, addressed new cases, cases with difficult follow up, and medication concerns.
Fidelity Checks
Several procedures were implemented to ensure treatment fidelity, standardize delivery, and minimize differences by clinician. Clinicians were required to fill out checklists of all intervention components (e.g., psycho-education, homework review) and procedural tasks (e.g., depressive symptoms, scheduling) and to document session duration to monitor exposure. A random 20% sample of recordings and treatment fidelity checklists were evaluated by the supervisory clinicians.
Coverage was evaluated using three numerical ratings; full coverage=2, partial coverage= 1, and no coverage = 0. Full coverage included fully discussing a component or completing a task, partial coverage was not fully discussing or completing the component/task, and 0 was if a component/task was completely missed. Ratings were summed to yield a clinician session score. Fidelity scores were calculated by dividing the clinician session score by the total possible rating. Two independent evaluators (Ph.D. and M.D.) listened to audio recordings from a randomly selected subsample of 32 patient cases in Boston and 30 in Puerto Rico to review fidelity (average of 22 per clinician). To calibrate, the two independent evaluators completed and discussed ratings on 14 cases, with substantial inter-rater reliability (81.88%). Clinicians exhibited substantial fidelity to the intervention and covered on average 84.55% of the required tasks in Boston and 80.23% in San Juan.
Analyses
First, we compared distributions of baseline characteristics between the ECLA-T and F interventions and the usual care groups to assess the balance of the observed covariates among the three randomized groups. Covariates included generational status, nativity, language proficiency, insurance, migration status, and physical comorbidities as measured by the Short Form Health Survey (SF-12). (47)
All analyses used intention-to-treat principles. Of 257 patients who completed the baseline assessment (RA1), 56 did not complete the first follow-up (RA2), and 24 did not complete the 2nd follow-up interview (RA3). To address missing data, we used multiple imputation methods in STATA (48) (version 12) statistical analysis software (STATA command “mi estimate”). This technique creates ten complete datasets, imputing missing values using a chained equations approach that incorporates demographic characteristics and outcome scores using standard rules. (49, 50, 51)
Effectiveness of the two interventions was compared to usual care by estimating a multiple linear regression model using the baseline score as a covariate. Primary outcomes (PHQ-9 and HSCL-20) and secondary outcome (WHO-DAS) measured at the last follow-up were regressed on the baseline score as well as other covariates representing treatment group membership and site (Boston vs. San Juan). Treatment effects were defined as differences in the primary outcome at the second follow-up for individuals having a similar score at baseline. The effect sizes for each outcome measure were computed using the estimated coefficients in these multiple linear regression models. Specifically, the effect sizes were computed by dividing the estimated coefficient on treatment group (i.e. the treatment effect) by the standard deviation of baseline score. To evaluate whether treatment effectiveness was different in Boston versus San Juan (exploratory aim), we estimated multiple regression models with site by study group interaction terms.
We also performed a sensitivity analysis to see whether differences between study groups can be explained in part by different medication use patterns. We included an additional control variable (medication use at baseline) to all regression models, but adjusting for medication use did not substantially change the magnitude or significance of coefficients in Table 3. We present these results with the actual data since the estimated coefficients and significance levels are almost identical when the actual data are used as compared to the imputed data in Table 3. (Results with imputed data are available from the authors).
Table 3.
Impact of intervention modalities on PHQ9, HSCL, and WHODAS scores
| PHQ9 at RA3 | HSCL at RA3 | WHODAS at RA3 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |||||||||||||
| Coef. | [95% CI] | Coef. | [95% CI] | Coef. | [95% CI] | Coef. | [95% CI] | Coef. | [95% CI] | Coef. | [95% CI] | |||||||
| study group (ref:usual care) | ||||||||||||||||||
| ECLA−F | −2.30* | −4.24 | −0.36 | −3.95** | −6.64 | −1.26 | −0.27* | −0.52 | −0.03 | −0.51** | −0.85 | −0.16 | −3.72* | −6.64 | −0.81 | −4.65* | −8.69 | −0.61 |
| 0.98 | 1.36 | 0.13 | 0.18 | 1.48 | 2.05 | |||||||||||||
| ECLA−T | −2.98** | −4.92 | −1.04 | −4.29** | −6.99 | −1.59 | −0.33* | −0.58 | −0.08 | −0.64*** | −0.99 | −0.29 | −2.73† | −5.72 | 0.27 | −4.48* | −8.62 | −0.35 |
| 0.99 | 1.37 | 0.13 | 0.18 | 1.52 | 2.1 | |||||||||||||
| site (PR) | 2.98*** | 1.38 | 4.57 | 0.94 | −1.78 | 3.67 | 0.14 | −0.09 | 0.37 | −0.23 | −0.59 | 0.13 | 1.38 | −1.1 | 3.86 | −0.42 | −4.56 | 3.72 |
| 0.81 | 1.38 | 0.12 | 0.18 | 1.26 | 2.1 | |||||||||||||
| study group*site | ||||||||||||||||||
| ECLA−F*PR | - | - | - | 3.38† | −0.44 | 7.19 | - | - | - | 0.47† | −0.01 | 0.96 | - | - | - | 1.88 | −3.99 | 7.75 |
| - | - | - | 1.94 | - | - | - | 0.25 | - | - | - | 2.98 | |||||||
| ECLA−T*PR | - | - | - | 2.72 | −1.14 | 6.58 | - | - | - | 0.63* | 0.14 | 1.13 | - | - | - | 3.69 | −2.3 | 9.67 |
| - | - | - | 1.96 | - | - | - | 0.25 | - | - | - | 3.03 | |||||||
| Constant | 0.28 | −3.07 | 3.63 | 1.31 | −2.21 | 4.83 | 0.38** | 0.11 | 0.64 | 0.55*** | 0.25 | 0.84 | 8.97*** | 5.37 | 12.56 | 9.84*** | 5.81 | 13.87 |
| 1.7 | 1.79 | 0.13 | 0.15 | 1.82 | 2.04 | |||||||||||||
| Observations | 231 | 231 | 233 | 233 | 195 | 195 | ||||||||||||
SE are reported below the coefficients;
p<0.001,
p<0.01,
p<0.05,
p<0.10
Notes:
All regressions control for the relevant baseline mental health score (i.e. models (1)–(2) control for baseline HSCL, models (3)– (4) control for baseline PHQ9 score, models (5)– (6) control for baseline WHODAS score)
Models (1), (3), (5) do not include interactions; models (2), (4), (6) include study group * site interactions
PR stands for Puerto Rico.
Results
Total samples of intervention and control patients in both sites were comparable across study groups on the socio-demographic characteristics of gender, age, education, employment status, nativity, and income (see Table 1). Sites differed in terms of other socio-demographic and clinical characteristics (see Table 2). San Juan participants were more likely to report being black/dark skinned, less educated, out of the labor force, and lower income. They also reported more symptoms and impairment, with significantly higher HSCL and WHO-DAS scores. Completers and drop-outs (data not shown) were not different, except that patients who dropped out were more difficult to contact at baseline. Intervention participants in ECLA-F were twice as likely to not initiate care (21.4%) as those in ECLA-T (10.3%; data not shown).
Table 1.
Patient Demographics by Study Condition (Boston and San Juan combined sample
| Usual care | Face-to-Face | Telephone | p-value | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| n=86 | % | n=84 | % | n=87 | % | n=257 | % | ||
| Sex | |||||||||
| 1.male | 15 | 17% | 19 | 23% | 13 | 15% | 0.417 | 47 | 18% |
| 2.female | 71 | 83% | 65 | 77% | 74 | 85% | 210 | 82% | |
| Age | |||||||||
| 1.18–34yr | 19 | 22% | 20 | 24% | 25 | 29% | 0.831 | 64 | 25% |
| 2.35–49yr | 32 | 37% | 30 | 36% | 32 | 37% | 94 | 37% | |
| 3.50–64yr | 30 | 35% | 32 | 38% | 27 | 31% | 89 | 35% | |
| 4.>=65yr | 5 | 6% | 2 | 2% | 3 | 3% | 10 | 4% | |
| Race (Note: all are Latino) | |||||||||
| White | 27 | 31% | 22 | 26% | 24 | 28% | 0.697 | 73 | 28% |
| Black/Dark Skinned | 29 | 34% | 27 | 32% | 30 | 34% | 86 | 33% | |
| Unreported (only indicated Latino) | 28 | 33% | 28 | 33% | 26 | 30% | 82 | 32% | |
| Mixed Race/American Indian | 2 | 2% | 7 | 8% | 7 | 8% | 16 | 6% | |
| Education | |||||||||
| 1.6th grade or less | 18 | 21% | 20 | 24% | 20 | 23% | 0.240 | 58 | 23% |
| 2.7–11th grade | 23 | 27% | 31 | 37% | 20 | 23% | 74 | 29% | |
| 3.HS diploma, GED, vocational school or more | 45 | 52% | 33 | 39% | 47 | 54% | 125 | 49% | |
| Employment status | |||||||||
| 1.full-time | 17 | 20% | 14 | 17% | 11 | 13% | 0.676 | 42 | 16% |
| 2.part-time | 19 | 22% | 21 | 25% | 20 | 23% | 60 | 23% | |
| 3.unemployed | 15 | 17% | 10 | 12% | 20 | 23% | 45 | 18% | |
| 4.out of labor force | 29 | 34% | 30 | 36% | 26 | 30% | 85 | 33% | |
| 5.illness/disabled | 6 | 7% | 9 | 11% | 9 | 10% | 24 | 9% | |
| Personal Income | |||||||||
| 1.<15k | 67 | 78% | 61 | 73% | 68 | 78% | 0.576 | 196 | 76% |
| 2.15k–35k | 12 | 14% | 13 | 15% | 11 | 13% | 36 | 14% | |
| 3.35–75k | 5 | 6% | 3 | 4% | 2 | 2% | 10 | 4% | |
| Unreported | 2 | 2% | 7 | 8% | 6 | 7% | 15 | 6% | |
| US born1 | |||||||||
| 0.immigrant | 47 | 55% | 43 | 51% | 49 | 56% | 0.791 | 139 | 54% |
| 1.US born | 39 | 45% | 41 | 49% | 38 | 44% | 118 | 46% | |
A person is considered to be “US born” if born in the United States or Puerto Rico; otherwise they are considered to be an “immigrant.”
Table 3 shows the linear regression model estimates for the two primary outcomes and the secondary outcome as reported in RA3: PHQ-9, HSCL-20, and WHO-DAS, respectively. The first specification for each outcome measure (columns (1), (3) and (5)) estimates the joint treatment effect across sites without a term to test for differential effectiveness of treatment in each site (Boston and San Juan). The second specification for each outcome (columns (2), (4) and (6)) includes treatment by site interactions as an exploratory analysis.
For the PHQ-9, both ECLA-F (p<0.05; Effect size (ES) =.56) and ECLA-T (p=0.01; ES=.64) were significantly better than usual care in lowering depressive symptoms (Table 3, column 1) on average across sites. Patients in Boston had significantly lower PHQ-9 scores at follow-up (p<.001) compared to Puerto Rico but there were no statistically significant interactions of treatment by site.
Similarly, the results for HSCL, the other primary outcome, showed significant intervention effects of both the ECLA-F (p<0.05; ES=.32) and ECLA-T intervention (p<0.05; ES=.34) compared to usual care (Table 3, column 3). The main effect of site was not statistically significant, but there was a significant interaction (Table 3, column 4) between ECLA-T and study site (p<0.05) that showed the telephone intervention was less effective in PR than Boston (in PR ES=.03; Boston ES=.73). The interaction for ECLA-F did not meet statistical significance (p<.09), but the pattern was similar to ECLA-T (in PR ES=.10; Boston ES=.64). This is because in San Juan the usual care group improved along with the intervention groups.
For the secondary outcome of WHO-DAS, there was a statistically significant effect of ECLA-F (p<.05, ES=.24) compared to usual care, and the effect of ECLA-T showed a similar trend that did not reach significance (p<0.07; ES=.23) in the combined sample (Table 3, column 5). There was no main effect of site and there was no evidence of differential effectiveness by site for this outcome.
To compare the impact of ECLA-T intervention directly to the impact of ECLA-F, we ran the same analysis in Table 3 after dropping the usual care participants. On all three outcomes HSCL, PHQ-9 and WHODAS there is no significant difference between the impact of the two interventions (p= 0.89, 0.69, and 0.91, respectively).
Discussion
Our findings suggest that the CERED ECLA intervention is associated with meaningful reductions in depressive symptoms and functional impairment as compared to usual primary care for depression. Even under the conditions of a multi-site design with limited exclusionary criteria and a diverse Latino patient population with low education, both intervention modalities appeared to help patients decrease depressive symptoms. Significantly more participants initiated mental health care (84.2%) when offered this intervention in primary care than is typical when primary care patients are referred to mental health care, with greater initiation (i.e. at least one visit to treatment) in the phone intervention (89.7%) than the face-to-face intervention (78.8%). This difference was even more pronounced in San Juan (69.8% in face to face vs. 88.6% by phone) than in Boston (87.8% and 90.7%, respectively). Treatment initiation and retention is generally lower for mental health patients than for those with physical illness (52) and studies of mental health referrals have found that overall missed initial appointment rates typically range from 26–50%. (53–55) Other studies show an association between Latino ethnicity, (56) as well as low socioeconomic status, (54) and lower likelihood of completing specialty care referral. The relatively high rates in both ECLA-T and ECLA-F groups suggest that care management and increased outreach to Latino patients can significantly improve treatment initiation, but that telephone-based psychotherapy may be a valuable tool for reducing barriers to care and eliminating disparities.
Our results also show that patients demonstrated significant improvements at follow-up in Boston under both treatment conditions but less so in San Juan. There are several possible explanations for the differential effects by site for HSCL. There were differences between sites regarding the delivery of care. In Puerto Rico, although clinics were supposed to regularly screen for depression using the PHQ-9, this was not done in any of the three participating clinics. Although fidelity to the treatment protocol was high in both sites, clinicians in San Juan had less quality assurance feedback than in Boston, possibly decreasing treatment effectiveness. Furthermore, research assistants in San Juan (but not Boston) reported that usual care calls served as a forum for patients to voice distress and may have functioned as a psychotherapeutic intervention more than symptom monitoring. The Boston site was also able to negotiate more flexible hours (Saturdays and evenings) for face-to-face treatment than the San Juan site (open 9AM–5PM on weekdays), which could explain lower face-to-face participation in San Juan.
There are also certain study limitations. Most importantly, not following a script when calling control patients at both sites could have led to outcome differences. There are also limitations inherent in not measuring the fidelity of the care manager intervention. More work in this area is needed to understand the added benefits care management provides for depression care, particularly in underserved communities facing multiple structural and economic barriers. It is also worth noting when comparing participant improvement across sites that the San Juan site had access to more doctoral-level clinicians than the Boston site. This would suggest that structural site differences (i.e. clinical hours) are more powerful determinants of outcome than level of professional experience and supports the use of masters-level clinicians.
Also of interest are the differences in outcomes by measure. The intervention was not effective in San Juan when evaluated with the HSCL-20. Although data suggest that both measures are moderately correlated (0.54), the HSCL-20 includes items that are not diagnostic symptoms of MDD such as “feelings of being trapped or caught,” or “worrying too much about things.” These items could be indicative of distress associated with extreme poverty and thus difficult to address with a short-term psychosocial intervention.
Overall the CERED ECLA intervention provides culturally adapted depression treatment that can be offered face-to-face or by telephone in order to eliminate barriers and address service disparities in primary care for Latino populations. As such, this could be a way for the health care system to meet needs of an increasingly diverse population covered as a result of health care reform, despite a limited workforce and budget constraints.
Supplementary Material
Contributor Information
Margarita Alegría, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th floor, Somerville, MA (02143) malegria@charesearch.org, Phone: 617-503-8448, FAX: 617-503-8447.
Evette Ludman, Group Health Research Institute, Seattle, WA
Nilay Kafali, Center for Multicultural Mental Health Research, Somerville, MA.
Sheri Lapatin, Center for Multicultural Mental Health Research, Somerville, MA
Doriliz Vila, Behavioral Sciences Research Institute, University of Puerto Rico Medical School, San Juan, PR
Patrick E. Shrout, Dept. of Psychology, New York University, NY
Kristen Keefe, Dept. of Psychology, Clark University, MA
Benjamin Cook, Center for Multicultural Mental Health Research, Somerville, MA
Andrea Ault, Center for Multicultural Mental Health Research, Somerville, MA
Xinliang Li, Center for Multicultural Mental Health Research, Somerville, MA
Amy Bauer, University of Washington, Seattle, WA
Claudia Epelbaum, Beth Israel Deaconess Medical Center, Boston, MA
Carmela Alcantara, Columbia University Medical Center, New York, NY
Tulia Inés Guerra Pineda, Center for Multicultural Mental Health Research, Somerville, MA
Gloria Gonzalez Tejera, Department of Psychiatry, MSC-University of Puerto Rico, San Juan
Gloria Suarez, Department of Psychiatry, MSC-University of Puerto Rico, San Juan
Karla Leon, Center for Multicultural Mental Health Research, Somerville, MA
Anna S. Lessios, Center for Multicultural Mental Health Research, Somerville, MA
Rafael R Ramirez, Behavioral Sciences Research Institute, University of Puerto Rico Medical School, San Juan, PR.
Glorisa Canino, Behavioral Sciences Research Institute, University of Puerto Rico Medical School, San Juan, PR.
References
- 1.Miranda J, Green BL, Krupnick JL, et al. One-year outcomes of a randomized clinical trial treating depression in low-income minority women. Journal of Consulting and Clinical Psychology. 2006;74:99. doi: 10.1037/0022-006X.74.1.99. [DOI] [PubMed] [Google Scholar]
- 2.McGuire T, Alegría M, Cook B, et al. Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care. Health Services Research. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miranda J, Cooper L. Disparities in Care for Depression Among Primary Care Patients. Journal of General Internal Medicine. 2004;19:120–126. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wells K, Klap R, Koike A, et al. Ethnic disparities in unmet need for alcoholism, drug abuse and mental health care. American Journal of Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- 5.Alegría M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alegría M, Takeuchi D, Canino G, et al. Considering Context, Place and Culture: the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13:208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atdjian S, Vega WA. Disparities in mental health treatment in US racial and ethnic minority groups: implications for psychiatrists. Psychiatric Services. 2005;56:1600–1602. doi: 10.1176/appi.ps.56.12.1600. [DOI] [PubMed] [Google Scholar]
- 8.Lewis-Fernandez R, Das AK, Alfonso C, et al. Depression in US Hispanics: diagnostic and management considerations in family practice. The Journal of the American Board of Family Practice. 2005;18:282–296. doi: 10.3122/jabfm.18.4.282. [DOI] [PubMed] [Google Scholar]
- 9.Olfson M, Cherry DK, Lewis-Fernández R. Racial differences in visit duration of outpatient psychiatric visits. Archives of General Psychiatry. 2009;66:214. doi: 10.1001/archgenpsychiatry.2008.523. [DOI] [PubMed] [Google Scholar]
- 10.Van Voorhees BW, Walters AE, Prochaska M, et al. Reducing Health Disparities in Depressive Disorders Outcomes between Non-Hispanic Whites and Ethnic Minorities: A Call for Pragmatic Strategies over the Life Course. Medical Care Research and Review. 2007;64:157S–194S. doi: 10.1177/1077558707305424. [DOI] [PubMed] [Google Scholar]
- 11.Cook B, McGuire T, Miranda J. Measuring Trends in Mental Health Care Disparities, 2000–2004. Psychiatric Services. 2007;58:1533–1539. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- 12.Whaley AL. Cultural mistrust: An important psychological construct for diagnosis and treatment of African Americans. Professional Psychology: Research and Practice. 2001;32:555–562. [Google Scholar]
- 13.Ward EC. Examining differential treatment effects for depression in racial and ethnic minority women: a qualitative systematic review. Journal of the National Medical Association. 2007;99:265. [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Census Bureau. Projections of the Resident Populations by Race, Hispanic Origin, and Nativity: Middle Series. 2050–2070. In: U.S. Census Bureau PD, editor. Washington, D.C.: 2000. [Google Scholar]
- 15.Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment. JAMA. 2004;292:935–942. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 16.Tutty S, Ludman EJ, Simon G. Feasibility and acceptability of a telephone psychotherapy program for depressed adults treated in primary care. General Hospital Psychiatry. 2005;27:400–410. doi: 10.1016/j.genhosppsych.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Ludman EJ, Simon GE, Tutty S, et al. A randomized trial of telephone psychotherapy and pharmacotherapy for depression: Continuation and durability of effects. Journal of Consulting and Clinical Psychology. 2007;75:257–266. doi: 10.1037/0022-006X.75.2.257. [DOI] [PubMed] [Google Scholar]
- 18.Mohr DC, Ho J, Duffecy J, et al. Effect of telephone-administered vs face-to-face cognitive behavioral therapy on adherence to therapy and depression outcomes among primary care patients: A randomized trial. JAMA. 2012;307:2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Simon G, Ludman E, Operskalski B. Randomized trial of a telephone care management program for outpatients starting antidepressant treatment. Psychiatric Services. 2006;57:1441–1445. doi: 10.1176/ps.2006.57.10.1441. [DOI] [PubMed] [Google Scholar]
- 20.Dwight-Johnson M, Aisenberg E, Golinelli D, et al. A randomized pilot study of telephone-based cognitive behavioral therapy for rural Latinos. Psychiatric Services. 2011;62:936–942. doi: 10.1176/ps.62.8.pss6208_0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health services research. 2003;38:613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker-Ericzén MJ, Connelly CD, Hazen AL, et al. A collaborative care telemedicine intervention to overcome treatment barriers for Latina women with depression during the perinatal period. Families, Systems, & Health. 2012;30:224. doi: 10.1037/a0028750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Himelhoch S, Medoff D, Maxfield J, et al. Telephone Based Cognitive Behavioral Therapy Targeting Major Depression Among Urban Dwelling, Low Income People Living with HIV/AIDS: Results of a Randomized Controlled Trial. AIDS and behavior. 2013;17:2756–2764. doi: 10.1007/s10461-013-0465-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kraemer HC, Wilson GT, Fairburn CG, et al. Mediators and moderators of treatment effects in randomized clinical trials. Archives of general psychiatry. 2002;59:877. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 25.Spirito A, Abebe KZ, Iyengar S, et al. Sources of site differences in the efficacy of a multisite clinical trial: the Treatment of SSRI-Resistant Depression in Adolescents. Journal of Consulting and Clinical Psychology. 2009;77:439. doi: 10.1037/a0014834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- 27.Ramos Z, Alegría M. Cultural Adaptation and Health Literacy Refinement of a Brief Depression Intervention for Latinos in a Low-Resource Setting. 2014 doi: 10.1037/a0035021. [DOI] [PubMed] [Google Scholar]
- 28.Paykel E, Myers J, Lindenthal J, et al. Suicidal feelings in the general population: a prevalence study. The British Journal of Psychiatry. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 29.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Medicine. 2010;8:18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derogatis LR, Lipman RS, Rickels K, et al. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Modern Problems of Pharmacopsychiatry. 1974;7:79. doi: 10.1159/000395070. [DOI] [PubMed] [Google Scholar]
- 31.Association AP. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Publishing, Inc.; 2000. [Google Scholar]
- 32.Löwe B, Unützer J, Callahan CM, et al. Monitoring depression treatment outcomes with the patient health questionnaire-9. Medical care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Fraser MW, Kirby LD, Smokowski PR. Risk and resilience in childhood. NASW press; 2004. [Google Scholar]
- 34.Hedrick SC, Chaney EF, Felker B, et al. Effectiveness of collaborative care depression treatment in Veterans' Affairs primary care. Journal of General Internal Medicine. 2003;18:9–16. doi: 10.1046/j.1525-1497.2003.11109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katon W, Robinson P, Von Korff M, et al. A multifaceted intervention to improve treatment of depression in primary care. Archives of general psychiatry. 1996;53:924. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 36.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 37.Huang FY, Chung H, Kroenke K, et al. Using the Patient Health Questionnaire-9 to Measure Depression among Racially and Ethnically Diverse Primary Care Patients. Journal of General Internal Medicine. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cepeda-Benito A, Gleaves DH. Cross-ethnic equivalence of the Hopkins Symptom Checklist-21 in European American, African American, and Latino College Students. Cultural Diversity and Ethnic Minority Psychology. 2000;6:297. doi: 10.1037/1099-9809.6.3.297. [DOI] [PubMed] [Google Scholar]
- 39.Organization WH. World Health Organization Disability Assessment Schedule II (WHODAS II) Geneva: World Health Organization; 2001. [Google Scholar]
- 40.Matías-Carrelo LE, Chávez LM, Negrón G, et al. The Spanish translation and cultural adaptation of five mental health outcome measures. Culture, medicine and psychiatry. 2003;27:291–313. doi: 10.1023/a:1025399115023. [DOI] [PubMed] [Google Scholar]
- 41.Association AP, DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV. Amer Psychiatric Pub Inc; 1994. APATFo. [Google Scholar]
- 42.Paykel E, Myers J, Lindenthal J, et al. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 43.Meyer TJ, Miller ML, Metzger RL, et al. Development and validation of the Penn State worry questionnaire. Behaviour research and therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- 44.Fresco DM, Mennin DS, Heimberg RG, et al. Using the Penn State Worry Questionnaire to identify individuals with generalized anxiety disorder: A receiver operating characteristic analysis. Journal of behavior therapy and experimental psychiatry. 2003;34:283–291. doi: 10.1016/j.jbtep.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 45.Schnurr P, Vielhauer M, Weathers F, et al. The brief trauma questionnaire. White River Junction, VT: National Center for PTSD; 1999. [Google Scholar]
- 46.Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wisconsin Medical Journal. 1994;94:135–140. [PubMed] [Google Scholar]
- 47.Ware JE, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 48.StataCorp. Stata 11 Multiple-Imputation Reference Manual College Station, TX: Stata Press; 2009. [Google Scholar]
- 49.Rubin DB, Schenker N. Multiple imputation for interval estimation from simple random samples with ignorable nonresponse. Journal of the American Statistical Association. 1986;81:366–374. [Google Scholar]
- 50.Rubin DB. Multiple Imputation of Nonresponse in Surveys. New York: Wiley; 1998. [Google Scholar]
- 51.Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken. NJ: Wiley; 2002. [Google Scholar]
- 52.Cramer JA, Rosenheck R. Compliance with medication regimens for mental and physical disorders. Psychiatric Services. 1998;49:196–201. doi: 10.1176/ps.49.2.196. [DOI] [PubMed] [Google Scholar]
- 53.De Figueiredo JM, Boerstler H, Doros G. Failure of high-risk minority patients to show up for outpatient psychiatric treatment. International Journal of Mental Health. 2009 [Google Scholar]
- 54.Chen A. Noncompliance in community psychiatry: a review of clinical interventions. Psychiatric Services. 1991;42:282–287. doi: 10.1176/ps.42.3.282. [DOI] [PubMed] [Google Scholar]
- 55.Compton M, Rudisch B, Craw J, et al. Predictors of missed first appointments at community mental health centers after psychiatric hospitalization. Psychiatric Services. 2006;57:531–537. doi: 10.1176/ps.2006.57.4.531. [DOI] [PubMed] [Google Scholar]
- 56.Kruse GR, Rohland BM, Wu X. Factors associated with missed first appointments at a psychiatric clinic. Psychiatric Services. 2002;53:1173–1176. doi: 10.1176/appi.ps.53.9.1173. [DOI] [PubMed] [Google Scholar]
- 57.Nadeem E, Lange J, Edge D, et al. Does stigma keep poor young immigrant and US-born black and Latina women from seeking mental health care? Psychiatric Services. 2007;58:1547–1554. doi: 10.1176/ps.2007.58.12.1547. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.