Abstract
Objectives Ageing of the population brings the possibility of increased burdens for acute hospital services because of the marked increase in many common diseases with age. We aimed to examine the relation between age and use of acute services in hospitals in the period before death in a national sample of deaths in hospital.
Design Retrospective cohort analysis of English hospital episode statistics database.
Setting All NHS hospitals in England.
Data set All post-neonatal deaths occurring in English NHS hospitals during financial year 1999-2000, with episodes of care in the previous three years determined through matching on sex, date of birth, and postcode.
Main outcome measures Total bed days, mean and median length of stay.
Results 253 799 in-hospital deaths were identified, representing about 45% of all deaths occurring in 1999-2000. Patients who died in hospital spent a median of 23 days in hospital in the three years before death; the median rose with age up to 45 years, but was fairly stable for ages 45 and above. The number of admissions to NHS hospitals in the three years before death averaged 3.6; this peaked at 10.4 in patients aged 5-9 years and decreased with age to 2.2 in those aged 85 and over.
Conclusions The average number of bed days spent in hospital in the period before death does not increase with increasing age.
Introduction
With life expectancy continually increasing in most countries, population ageing has become an important issue worldwide. This has led to concerns about the impact this will have on healthcare systems, given the almost exponential relation between age and many diseases. Public debate over the perceived overuse of healthcare services by older people has included discussions of equity, the “fair innings” argument, and age based rationing of health care.
One view is that the increasing number of older people will inevitably result in a greater burden of chronic and degenerative diseases, such as cardiovascular diseases, osteoarthritis, cancers, diabetes, cataract and macular degeneration, and dementia syndromes, which will result in an increased demand for health care and hence soaring costs.1,2 An alternative suggestion is that the increase in total life expectancy has been accompanied by an increase in healthy life expectancy, due to a compression of morbidity into a shorter period, effectively postponing the onset of chronic diseases and associated disabilities.1,3,4 This second scenario would result in a lower burden on healthcare resources than the first.5
A key concern in this debate has been the utilisation and cost of acute care. In his interim report on estimating the resources required to run the English health service in 2020, Wanless stated: “Age and people's proximity to death are the the most significant determinants of health status and health needs, but the impact of ageing on future expenditure is likely to be relatively small when compared to other cost drivers.”6 In the acute setting, to what extent does age, rather than proximity to death, lead to higher costs? This paper examines that question by considering the acute phase of care provided by the public sector. We asked: does the total time spent in hospital or the number of spells in hospital, or both, in the three years before death vary with age?
Methods
We analysed hospital episode statistics for England. The database (held by the Department of Health, http://www.dh.gov.uk/PublicationsAndStatistics/Statistics/HospitalEpisodeStatistics/fs/en) holds information on patients who are admitted, either as a day case or as an ordinary admission, to NHS hospitals in England. Each record in the database relates to one finished consultant episode, the period an individual spends under the care of one NHS consultant. Private hospital procedures are excluded from the database as there is no requirement for such hospitals to provide routine data.
The information held in the hospital episode statistics database includes the age and sex of the patient, area of usual residence, reason for admission to hospital (diagnosis), and procedure performed. Information is now available for financial years April 1989 to March 2003. Data for this analysis were derived from the database extract held at the University of Bristol, which currently contains data for financial years from 1 April 1991 to 31 March 2001. In this extract the patient's postcode and date of birth are stored in an encrypted format to allow record linkage while preserving confidentiality.
We identified all episodes (excluding births) for financial year 1999 (1 April 1999 to 31 March 2000) which resulted in the patient's death. Records in which the sex, postcode, or date of birth of the patient were missing were excluded (1485 episodes, 0.6%). Long term cases comprised 1153 patients (0.4%) whose stay in hospital consisted of a single episode exceeding three years at time of death; these were excluded from the analysis (median length of stay 5.3 years, 95th centile 11.5 years, maximum 69 years), as were 287 patients (0.1%) who had had more than one episode but had been in continuous hospital care for more than three years at time of death. The most common diagnoses among these people were mental and behavioural disorders (dementia; mental retardation; schizophrenia) and diseases of the nervous system (Alzheimer's disease; multiple sclerosis). We also excluded a further 10 patients whose admission dates could not be determined and 20 whose dates of death were unclear.
The remaining deaths were matched on date of birth, postcode, and sex to the records of all general episodes (not including deliveries, births, or formal detentions of psychiatric patients) to identify all episodes of acute care provided in the three financial years before death (1996-7 to 1998-9) to patients who died in hospital in the financial year 1999-2000. In 144 cases (0.06%) the date of birth, postcode, and sex combination could be matched to two or more concurrent hospital episodes, one or both of which ended in death. These cases were excluded as they could not be uniquely identified by the matching process.
For each patient we calculated the total number of days spent in hospital and the number of separate admissions in the year, two years, and three years before death. For this purpose a day in hospital was defined as an overnight stay; episodes which started and ended on the same day therefore had a length of stay of zero days.
Results
sex Record matching identified 253 779 deaths in NHS hospitals between 1 April 1999 and 31 March 2000. Of these, 216 341 (85.3%) were in patients aged 65 years or over and 72 579 (28.6%) in patients aged 85 years or over (table 1). Nearly two thirds (64.5%) of those aged 85 or over were female. The average age at death was 74.2 years for males and 78.0 years for females. The most common primary diagnoses recorded overall were diseases of the circulatory system (30.1%), neoplasms (20.1%), and diseases of the respiratory system (19.0%); however, diagnoses varied by age (table 2).
Table 1.
Deaths in hospital, 1 April 1999 to 31 March 2000, England
|
Males
|
Females
|
|||
|---|---|---|---|---|
| Age group | No (%) | Cumulative %* | No (%) | Cumulative %* |
| 0-4† | 771 (0.63) | 100 | 636 (0.48) | 100 |
| 5-9 | 82 (0.07) | 99.38 | 75 (0.06) | 99.51 |
| 10-14 | 112 (0.09) | 99.31 | 106 (0.08) | 99.45 |
| 15-19 | 263 (0.21) | 99.22 | 148 (0.11) | 99.37 |
| 20-24 | 301 (0.25) | 99.01 | 198 (0.15) | 99.26 |
| 25-29 | 349 (0.29) | 98.76 | 301 (0.23) | 99.11 |
| 30-34 | 548 (0.45) | 98.47 | 421 (0.32) | 98.88 |
| 35-39 | 753 (0.62) | 98.02 | 670 (0.51) | 98.56 |
| 40-44 | 1096 (0.90) | 97.40 | 998 (0.76) | 98.05 |
| 45-49 | 1827 (1.49) | 96.50 | 1579 (1.20) | 97.29 |
| 50-54 | 3212 (2.62) | 95.01 | 2556 (1.95) | 96.09 |
| 55-59 | 4505 (3.68) | 92.39 | 3382 (2.57) | 94.14 |
| 60-64 | 7311 (5.97) | 88.71 | 5238 (3.99) | 91.57 |
| 65-69 | 11780 (9.62) | 82.74 | 8288 (6.31) | 87.58 |
| 70-74 | 18007 (14.71) | 73.12 | 13844 (10.54) | 81.27 |
| 75-79 | 25191 (20.58) | 58.41 | 22723 (17.30) | 70.73 |
| 80-84 | 20568 (16.80) | 37.83 | 23361 (17.78) | 53.43 |
| 85-89 | 17276 (14.11) | 21.03 | 26190 (19.94) | 35.65 |
| 90-94 | 7043 (5.75) | 6.92 | 15779 (12.01) | 15.71 |
| 95 and over | 1427 (1.17) | 1.17 | 4864 (3.70) | 3.70 |
| Total | 122422(100) | 131357(100) | ||
Source: Hospital episode statistics, Department of Health.
Cumulative percentage is presented so that the percentage of hospital deaths arising at increasing age thresholds is readily apparent. For example, in men 58.41% of all in-hospital deaths occur in those aged 75 and over.
Excludes newborns.
Table 2.
Most common primary diagnoses of in-hospital deaths, England, 1999-2000. Values are percentages of deaths in age group
| Diagnosis | 0-4 years | 5-15 years | 16-24 years | 25-44 years | 45-64 years | 65-84 years | 85 and over |
|---|---|---|---|---|---|---|---|
| Perinatal conditions | 32.8 | ||||||
| Congenital disorders | 19.1 | ||||||
| Signs and symptoms not else classified | 9.6 | ||||||
| Injury and poisoning | 24.3 | 26.8 | |||||
| Neoplasms | 17.3 | 16.5 | 26.7 | 35.9 | 22.0 | 9.9 | |
| Diseases of respiratory system | 13.8 | 13.0 | 19.1 | 22.4 | |||
| Diseases of circulatory system | 12.5 | 16.1 | 23.0 | 31.8 | 31.4 | ||
| Diseases of digestive system | 13.7 |
Source: Hospital episode statistics, Department of Health.
Time spent in hospital
Patients who died in hospital in 1999 spent a mean of 38.5 days and a median of 23 days in hospital in the three years before death (table 3). Much of this time was accumulated during the year immediately before death (mean 29.9 days (median 18 days) in hospital). Time spent in hospital ranged from the day of death only to the entire three year period; however, 60% of all patients who died in hospital spent less than one month in hospital over the three years before death, and only 5% spent more than four months of their final three years in hospital. (This does not include time spent in a hospice, nursing home, or residential care.) The mean number of days spent in hospital was lower for those aged 45 and over than for all other age groups, apart from the youngest age group (0-4). The median number of days spent in hospital rose with age up to 45 years, but was fairly stable for ages 45 and above. The patterns for the amount spent in hospital in the one, two, and three years before death were broadly similar.
Table 3.
Number of days spent in hospital in the year, two years (cumulative), and three years (cumulative) before death, England, 1999-2000
|
One year before death
|
Two years before death
|
Three years before death
|
||||
|---|---|---|---|---|---|---|
| Age group | Mean (SD) | Median (interquartile range) | Mean (SD) | Median (interquartile range) | Mean (SD) | Median (interquartile range) |
| 0-4 | 28.4 (49.0) | 7 (1-32) | 31.1 (54.3) | 8 (1-34) | 32.2 (56.9) | 8 (1-35) |
| 5-15 | 32.6 (54.8) | 8 (1-39) | 42.5 (82.0) | 9 (2-54) | 50.5 (102.0) | 10 (2-61.5) |
| 16-24 | 31.2 (52.1) | 8 (2-37) | 38.9 (69.1) | 9 (2-46) | 43.4 (79.9) | 10 (2-50) |
| 25-44 | 32.3 (47.8) | 16 (4-40) | 39.3 (65.2) | 18 (5-48) | 43.2 (77.4) | 20 (5-51) |
| 45-64 | 29.4 (38.4) | 18 (6-38) | 34.8 (50.7) | 21 (7-44) | 37.9 (58.1) | 22 (8-47) |
| 65-84 | 29.9 (39.1) | 18 (6-39) | 35.3 (51.5) | 21 (7-45) | 38.6 (58.3) | 23 (8-49) |
| ≥85 | 30.0 (38.4) | 18 (6-40) | 34.9 (50.4) | 21 (7-46) | 38.2 (57.6) | 23 (8-49) |
| Total | 29.9 (39.2) | 18 (6-39) | 35.2 (51.6) | 21 (7-45) | 38.5 (58.7) | 23 (8-49) |
Source: Hospital episode statistics, Department of Health.
The groups of diagnoses at death associated with the most hospital days over three years were mental and behavioural disorders (median 59 days); use of other health services (for example, cancer treatment, palliative or respite care, or rehabilitation after a stroke (median 54 days); and diseases of the nervous system (median 33 days).
Number of admissions
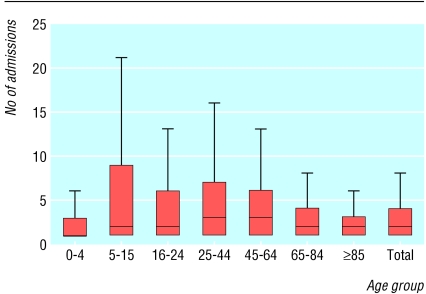
Patients who died in hospital had on average 3.6 admissions to NHS hospitals in the three years before death. The average number of admissions peaked at 10.4 in the 5-9 years age group and then decreased with age to 2.2 in patients aged 85 and over (figure). The maximum number of admissions was 441. Of patients who died in hospital, 78% had four or fewer admissions, and only 5% had more than 10 admissions over the three years. A very small proportion of patients (0.03%; 78 patients) were admitted to hospital more than 100 times in the three years before their death; 37 (47%) of these were receiving cancer treatment, 21 (27%) were having dialysis, and 13 (17%) had diseases requiring regular blood transfusions. As most admissions for these people were day admissions, their total lengths of stay do not generally reflect these high numbers of admissions.
Figure 1.
Number of admissions to hospitals in the three years before death, England, 1999-2000. Lines represent medians, boxes represent interquartile ranges, whiskers represent 1.5 times the interquartile range
Diagnoses at death associated with higher numbers of admissions over the previous three years were blood and immune system disorders (mean 6.3 admissions) and neoplasms (mean 5.5 admissions). Treatment for these types of conditions is often periodic and thus results in a series of short, generally day case, admissions.
Discussion
Deaths below the age of 65 and above the age of 85 years accounted for about 15% and 29% respectively of the nearly 254 000 in-hospital deaths occurring in 1999-2000. Neither total hospital days nor the number of admissions in the three years before death showed the expected positive relation to age at death. Although the median number of days in hospital in the three years before death increased up to age 45, it remained fairly stable after this age. Mean hospital days also stabilised from 65 years of age, having peaked in the 5-15 years age group. The number of admissions in the three years before death decreased after age 25-44.
An earlier report that used Oxford record linkage data for 1985 to examine prior hospital admissions of patients who died in or out of hospital showed that the mean (and median) number of days spent in hospital before death by patients admitted at least once was markedly higher in people over 85 years than in the 65-74 age group, but our more recent data showed no such increase. The Oxford study also examined the use of hospital beds by patients who died outside hospital and showed that excessively long stays among elderly people were uncommon.7 A more extensive examination of a wider age range and time before death using the same record linkage system of 18 524 deaths found a similar pattern of increasing bed days with increasing age, but also showed that irrespective of age, patients tended to use most of their lifetime bed days in the year immediately before death.8 The investigators interpreted this finding as indicating that older people, far from “using up” their entitlement to hospital care, had deferred drawing on their “account” until their final years of life.
Such results provide further counterpoint to the “pervasive image” described by Cohen of “an extremely elderly and terminally ill patient consuming large amounts of resources shortly before he or she dies” through the use of expensive technology and treatments, multiple admissions, and long lengths of stay.9 Our sample of patients who died in hospital showed no increase in median total bed days or number of admissions after the age of 45 years, and in fact the group most likely to have had multiple admissions was children. While as a whole the older age groups account for a larger total number of admissions and bed days in the three years before death, this is due to the fact that as age increases, a higher proportion of people are in the final stages of their lives.
Limitations
Our study has several limitations. Firstly, it included only people who died in hospital. At all ages, 50-55% of deaths each year occur in NHS hospitals.10 This analysis has captured 85% of the number of deaths recorded as occurring in NHS hospitals in 1999, and therefore accounts for around 45% of all deaths in that year. (Long stay patients, newborns, and people who died before being formally admitted to hospital probably make up a large proportion of the remaining 15% of hospital deaths.)
Secondly, the use of hospital bed days as a proxy for use of hospital costs assumes that patients of all ages and diagnoses consume the same amount of resources per bed day. This is obviously not the case: while fixed costs such as food, maintenance, and nursing salaries should be standard, different treatments and regimens of care will have different costs. The data held in the Bristol hospital episodes system extract do not allow us to consider costs directly, but the care of older people is unlikely to be more expensive: despite their greater likelihood of comorbidity and the need for a longer recuperation period (reflected in bed days), they are much less likely to receive intensive care or undergo surgery or complex interventions. Few of the patients in this sample underwent complex operations in the three years before their death, and about 40% had had no procedures at all (in NHS hospitals) during this time. A German study similarly reported that the oldest patients received less costly treatment than younger patients for the same illness and that older patients generally had illnesses that required less expenditure than younger patients.11
Conclusions
The average number of bed days spent in hospital in the period before death shows no discernable increase with increasing age. These findings concur with previous studies that have shown that the highest proportion of costs for acute care are incurred in the final years of life, no matter at what age this happens to be, and that total costs of acute care are greater in elderly people simply because this age group makes up a larger proportion of dying people.12-14 Such findings have important implications for understanding the use of acute hospital resources and for distinguishing the costs of dying from the costs of ageing.
What is already known on this topic
Population ageing brings with it the possibility of increased burden on acute hospital services because of the increase in many common diseases with age
Although average costs for acute care increase with age, these costs are related to life remaining rather than life lived
What this paper adds
Among patients who died in NHS hospitals, use of acute services did not increase with age in the three years before death
The number of admissions over this period decreased with age, and average length of stay was stable above age 45 years
The older sector of the population accounts for a high proportion of acute healthcare resources because they are nearing the end of their lives, not because care is individually more expensive
The hospital episodes statistics (HES) data were made available by the Department of Health.
Contributors: TD analysed the data. All authors contributed to writing and revising the text. SE is guarantor.
Funding: Medical Research Council (UK). MS is funded by the South West Public Health Observatory. HES analyses conducted within the Department of Social Medicine are supported by the South West Public Health Observatory.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Brameld KJ, Holman CDJ, Bass AJ, Codde JP, Rouse IL. Hospitalisation of the elderly during the last year of life: an application of record linkage in Western Australia 1985-1994. J Epidemiol Community Health 1998;52: 740-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guralnik JM, Land KC, Blazer D, Fillenbaum GG, Branch LG. Educational status and active life expectancy among older blacks and whites. N Engl J Med 1993;329: 110-6. [DOI] [PubMed] [Google Scholar]
- 3.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med 1980;303: 130-5. [DOI] [PubMed] [Google Scholar]
- 4.Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982-1994. Proc Natl Acad Sci USA 1997;94: 2593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maynard A, Sheldon T, Loudon I, Webster C, Rao JN, Frankel S, et al. Limits to demand for health care. BMJ 2001;322: 734. [Google Scholar]
- 6.Wanless D. Securing our future health: taking a long-term view. Interim report. London: HM Treasury, 2001.
- 7.Henderson J, Goldacre MJ, Griffith M. Hospital care for the elderly in the final year of life: a population based study. BMJ 1990;301: 17-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Himsworth RL, Goldacre MJ. Does time spent in hospital in the final 15 years of life increase with age at death? A population based study. BMJ 1999;319: 1338-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen GD. Health care at an advanced age. Myths and misconceptions. Ann Intern Med 1994;121: 146-7. [DOI] [PubMed] [Google Scholar]
- 10.Office for National Statistics. Mortality statistics: general. London: ONS, 2000. (Series DH1 No 33.)
- 11.Brockman H. Why is less money spent on health care for the elderly than for the rest of the population? Health care rationing in German hospitals. Soc Sci Med 2002;55: 593-608. [DOI] [PubMed] [Google Scholar]
- 12.McGrail K, Green B, Barer ML, Evans RG, Hertzman C, Normand C. Age, costs of acute and long-term care and proximity to death: evidence for 1987-88 and 1994-95 in British Columbia. Age Ageing 2000;29: 249-53. [DOI] [PubMed] [Google Scholar]
- 13.Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ 1999;8: 485-96. [DOI] [PubMed] [Google Scholar]
- 14.Busse R, Krauth C, Schwartz FW. Use of acute hospital beds does not increase as the population ages: results from a seven year cohort study in Germany. J Epidemiol Community Health 2002;56: 289-93. [DOI] [PMC free article] [PubMed] [Google Scholar]