Short abstract
This review discusses the specific uses and potential advantages of forceps over other modes of delivery. To enable women to make an informed choice about mode of delivery, obstetricians need to be adequately trained and supervised in the use of forceps
Global increases in rates of caesarean section show no sign of abating. The US National Center for Health Statistics reported that deliveries by caesarean section in 2001 had increased to almost a quarter, the highest level since 1989.w1 A similar rate was observed in England, Wales, and Northern Ireland in 2000.1 The greatest increases and variation between institutions are seen among first time mothers with a singleton pregnancy at term and women who have had a previous caesarean section. The American College of Obstetrics and Gynecology has recommended training in instrumental delivery to control and reduce the rates of caesarean section.w2
In the United States the rates of forceps delivery have decreased despite an increase in operative deliveries.w3-w6 In the United Kingdom, the rates of instrumental vaginal delivery range between 10% and 15%1 w7; these have remained fairly constant, although there has been a change in preference of instrument. In the 1980s most instrumental vaginal deliveries were by forceps, but by 2000 this had decreased to under a half. Much of the decline has been attributed to an increasing preference for vacuum extraction or for caesarean section when complex vaginal delivery is anticipated.2,3 w8 Lively discussion in both the medical and the lay press has centred on morbidity associated with operative deliveries, the importance of maternal choice, and best clinical practice.4 w9 w10 Most women still aim for spontaneous vaginal delivery. If complications do arise during labour it should be possible to offer women suitable alternatives and not solely caesarean section. Here we review the role of forceps delivery in modern obstetric practice.
Sources and selection criteria
We searched PubMed and the Cochrane Library database using as free text words, and in combination with morbidity and outcome, forceps delivery, vacuum extraction, caesarean section, instrumental delivery, and operative delivery. Reference lists were manually searched and reviewed. Guidelines, protocols, and review articles addressing instrumental delivery were searched through the websites of the American College of Obstetrics and Gynecology and the Royal Colleges of Obstetrics and Gynaecology. We critically reviewed articles focusing on morbidity and mortality issues relating to operative delivery.
Summary points
Most women aim for spontaneous vaginal delivery
When complications arise in the second stage of labour there is a choice between instrumental vaginal delivery and caesarean section
Obstetricians are increasingly choosing caesarean section when complications arise in the second stage of labour
Injury to the pelvic floor and trauma to the baby are more common after forceps delivery, but major maternal haemorrhage and separation from the baby are more common after caesarean section
Women are more likely to achieve a spontaneous vaginal delivery in a subsequent pregnancy after forceps delivery than after caesarean section
Forceps and indications for use
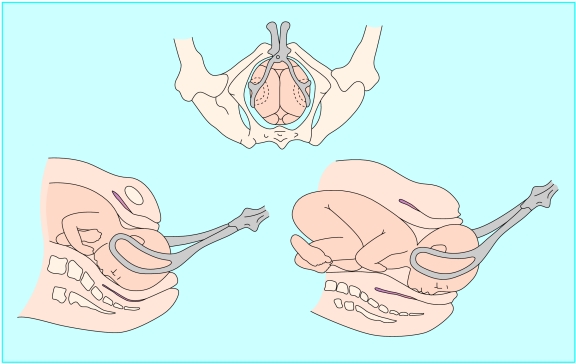
More than 700 types of obstetric forceps have been described.w11 Each of the three main types (outlet, midcavity, or rotational forceps) is appropriate to specific situations and requires differing levels of expertise (box). Typically, forceps are used when a singleton fetus in the cephalic position fails to progress or when delivery needs to be expedited in the second stage of labour because of fetal distress (fig 1). In these instances there may be a real choice between forceps and alternative methods of delivery—namely, caesarean section and vacuum extraction.
Fig 1.
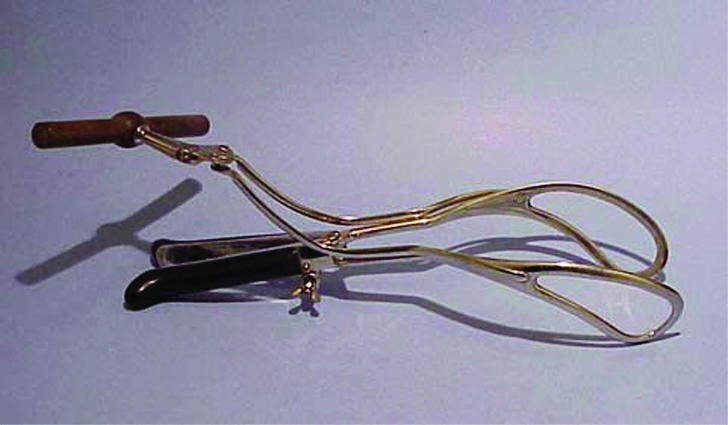
Forceps with traction handle
In some situations forceps may be the safest option for delivery—for example, with an undiagnosed breech presentation at full cervical dilation or for delivery of the second twin. In these cases forceps enable the controlled delivery of the fetus's head (fig 2). Assisted vaginal delivery of a fetus with a face presentation can only be achieved by forceps; vacuum extraction is contraindicated. Forceps is the only option for delivery of premature fetuses because of the risk of cephalohaematoma and intracranial haemorrhage with vacuum extraction.5 Additionally there are medical conditions (cardiac, respiratory, and neurological) that preclude maternal effort, required for successful vacuum extraction, in the second stage of labour. Forceps may also be chosen when maternal effort is minimal secondary to epidural analgesia. Outlet forceps can be useful at caesarean section for controlled delivery of the fetus's head.
Fig 2.
Application of forceps to fetus's head in occipito-anterior position followed by controlled traction and assisted delivery of head
Indications for forceps delivery
Relative indications (vacuum extraction or caesarean section may be an alternative option)
Delay or maternal exhaustion in the second stage of labour
Dense epidural block with diminished urge to push
Rotational instrumental delivery for malpositioned fetus
Suspected fetal distress
Specific indications (forceps delivery is usually superior to vacuum extraction or caesarean section in these circumstances)
Delivery of the head at assisted breech delivery (singleton or twin)
Assisted delivery of preterm infant (< 34 weeks' gestation)
Controlled delivery of head at caesarean section
Assisted delivery with a face presentation
Assisted delivery with suspected coagulopathy or thrombocytopenia in fetus
Instrumental delivery for maternal medical conditions that preclude pushing
Instrumental delivery under general anaesthesia
Cord prolapse in the second stage of labour
Reasons for decline in use of forceps
The decline in the use of obstetric forceps is multifactorial although many of the factors are inter-related. Litigation has grown over recent years in all areas, but it is often related to care on the labour ward and departures from practice guidelines.w12 w13 North American guidelines for instrumental delivery emphasise that “extreme care in patient selection and strict adherence to guidelines is necessary in order to prevent morbidity and mortality.”6 In the United Kingdom the Royal College of Obstetrics and Gynaecology has produced clinical guidelines in recognition of the wide variation in forceps rates between hospitals and a desire to reduce morbidity through training.7 The authors recommend the vacuum extractor as the instrument of choice. The decline in forceps has been further reinforced by opinion leaders suggesting that rotational deliveries of more than 45 degrees are likely to be abandoned.w14 A subsequent survey showed that most obstetricians in North America have abandoned rotational instrumental delivery in favour of caesarean section.3 In Australia, obstetricians preferred using a vacuum extractor for rotational instrumental delivery.w15
Issues of litigation and practice guidelines relate to widespread concerns over the training of obstetricians. Obstetric forceps are potentially dangerous in the hands of untrained or inexperienced obstetricians. Most residency training programmes in North America no longer expect proficiency in mid-cavity forceps delivery, and in one residency programme 14% of the institutions surveyed were no longer performing such deliveries.8 w16 Training in the use of forceps has been further reduced with awareness that the sequential use of instruments (failed vacuum extraction followed by forceps) is inappropriate and associated with increased morbidity.2 w17
Advantages of forceps delivery
Evidence suggests that forceps are associated with less failure than vacuum extraction (table).7,9,10 Delivery by forceps is also quicker than by vacuum extraction, which may be of critical importance with fetal distress.11 Women who have instrumental vaginal deliveries typically have a shorter hospital stay and fewer readmissions than women who have caesarean sections.9 w18 Worldwide this has cost implications to healthcare providers and social benefits to women.
Table 1.
Advantages and disadvantages of forceps delivery compared with vacuum extraction and emergency caesarean section
|
Forceps delivery
|
||
|---|---|---|
| Comparator | Advantages | Disadvantages |
| Vacuum extraction | More expedient delivery of fetus in distress; lower failure rate; reduced need for sequential use of instruments; fewer cases of cephalohaematoma and retinal haemorrhage | Stronger maternal analgesia needed; greater maternal perineal trauma; facial bruising and facial nerve palsy more common |
| Emergency caesarean section | Major obstetric haemorrhage and admission to neonatal intensive care less common; shorter hospital stay; fewer readmissions; subsequent spontaneous vaginal delivery more likely | Trauma to baby more likely; perineal trauma, dyspareunia, and urinary incontinence more common |
Use of forceps requires greater clinical skill than use of vacuum extractor, which can be advantageous or disadvantageous.
A Cochrane meta-analysis found that women who experienced vaginal delivery were less anxious about their babies and more satisfied with the birth than women who had a caesarean section.12 Women who had a vaginal delivery were also more likely to breast feed, have more positive reactions to their infants immediately after birth, and interact with them more at home. These outcomes concern all types of vaginal deliveries compared with caesarean sections.
The implication for future mode of delivery is one of the central issues regarding chosen mode of delivery. Repeat caesarean section is one of the principal factors implicated in increasing rates of caesarean section.1 w1 By minimising primary caesarean sections this should have a noticeable effect on the overall caesarean section rate. Furthermore, the risk of intrapartum complications in subsequent pregnancies is reduced if a woman has not had a previous caesarean section.13
Morbidity after forceps delivery
Maternal morbidity
In the immediate post partum period forceps have been associated with increased perineal and vaginal trauma and a greater requirement for analgesia compared with vacuum extractors.14 These findings were confirmed by another study, which also found that cervical laceration, post partum infection and other complications, and prolonged hospital stay were more common in women who had forceps delivery compared with those who had vacuum assisted delivery.15 A higher rate of third degree tears has been reported with forceps than with vacuum extractors, although one study found the contrary.16 w19 w20 Johanson and coworkers found no significant differences between forceps delivery and vacuum extraction in the rates of urinary and bowel dysfunction after five years.w21 Yet other studies have reported greater symptoms of altered faecal continence associated with forceps delivery.17 w22
One study found that major haemorrhage and prolonged hospital stay were more likely in women who had caesarean section in the second stage of labour compared with instrumental delivery.9 This may be offset by subsequent pelvic floor morbidity, although evidence is inconsistent.18 w23 Data addressing reproductive morbidity after instrumental vaginal delivery or caesarean section are scarce. A recent study found a delay in subsequent conception among women who had caesarean section compared with women who delivered vaginally.19 A small increase in both voluntary and involuntary infertility has been reported after caesarean section.w24
Fetal and neonatal morbidity
If the fetus's head needs to be rotated, there is now a tendency to use manual rotation, rotation with a vacuum extractor, or caesarean section in preference to Kielland's rotational forceps. This change in practice arose in the 1980s after high rates of neonatal morbidity and mortality were associated with Kielland's forceps.w25 A subsequent Australian study reported good neonatal outcomes, no perinatal deaths, and only minor cases of trauma with Keilland's forceps.20 Nonetheless, Kielland's forceps are only used for select cases and by experienced obstetricians.
Evidence evaluating neonatal morbidity after instrumental vaginal delivery is inconsistent. A systematic review of 10 trials comparing vacuum extraction with forceps delivery found no significant differences in Apgar scores at one and five minutes and few serious injuries in neonates, although the vacuum extractor was associated with an increase in cephalohaematoma and retinal haemorrhage.14 Evidence addressing long term outcomes is lacking, with one study reporting no significant differences in development at 5 years of age between children born by forceps and those born by vacuum extraction.w21 A prospective cohort study comparing instrumental vaginal deliveries with caesarean sections at full dilation found an increase in admissions to the neonatal intensive care unit after caesarean section.9
Sequelae in neonates is an important consideration if instrumental vaginal delivery is unsuccessful.7 One study retrospectively comparing outcomes after caesarean section in the second stage of labour either immediately or after failed instrumental delivery found no difference in neonatal or maternal morbidity.21 A more recent prospective study found that neonatal trauma and fetal acidosis were more common after failed instrumental vaginal delivery than after immediate caesarean section.9 Increased rates of neonatal encephalopathy, associated with cerebral palsy and neonatal death, have been reported after emergency caesarean section and instrumental vaginal delivery.22 It remains difficult to establish whether complications in labour result in operative delivery or whether the mode of delivery itself contributes to adverse outcomes.
Maternal perspective
Most women aim for spontaneous vaginal delivery, although a growing minority request elective caesarean section in the absence of an obstetric indication. Elective caesarean section has received undue attention, and this has detracted attention from women who would prefer vaginal delivery but are traumatised by their experience of delivery. One study found that a greater proportion of women who had experienced instrumental delivery or caesarean section remained frightened about future childbirth compared with women who had a normal delivery.w24 Similar high rates of psychological morbidity seem to apply to women who undergo instrumental delivery in theatre and women who experience caesarean section in the second stage of labour.13 In some cases this is sufficient to deter them from further pregnancies. A qualitative study reported that women seem unprepared for operative delivery in these circumstances, have a poor understanding of the indication for such delivery, and would welcome a detailed review at some time after the delivery.23 Debriefing and stress minimising strategies have been largely ineffective to date, and further work is required to understand how maternal satisfaction with the birth experience can be enhanced in the context of obstetric complications.w26-w28
Additional educational resources
National Collaborating Centre for Women's and Children's Health (www.rcog.org.uk/resources/pdf/cs_section_full.pdf)—clinical guidelines on caesarean section commissioned by the National Institute for Clinical excellence
Johanson R, Cox C, Grady K, Howell C, ed. Managing obstetric emergencies and trauma. The MOET course manual. London: RCOG Press; 2003.
Information for patients
NHS Helpline 0800 22 44 88
National Childbirth Trust 0870 444 8707 (www.nct-online.org)
Association for Improvements in the Maternity Services 0131 229 6259 (www.aims.org.uk)
Royal College of Midwives 0131 225 1633 (www.rcm.org.uk)
Midwives Information and Resource Service 0117 925 1791 (www.midirs.org)
Health Education Board for Scotland 0131 536 5500 (www.hebs.scot.nhs.uk)
Scottish Programme for Clinical Effectiveness in Reproductive Health Expert Advisory Group on Caesarean Section 01224 554476 (www.show.scot.nhs.uk/spcerh)
UK Online—Having a Baby (www.ukonline.gov.uk)
Personal perspective
As a first time mother, I was looking forward to the delivery of my daughter. After a prolonged labour of 16 hours, plans were made for an emergency caesarean section. I was prepared for theatre and given a spinal anaesthetic in addition to my epidural. I agreed to forceps after a further failed attempt to deliver my daughter naturally. I assisted by pushing down when requested and, to my amazement, Kaylyn was born after only three pushes. I experienced no pain or adverse reactions after delivery and admit that it was a very positive experience for both me and my husband. I believe that had it not been a forceps delivery it would have proceeded to a caesarean section, which I am sure would have had many negative aspects. (Fiona Scott)
Interestingly, a prospective cohort study found that women were more likely to prefer a future vaginal delivery after a successful forceps delivery than after a caesarean section.24 These women were more likely to achieve a vaginal delivery in subsequent pregnancies (over three quarters of women after instrumental delivery compared with almost a third after caesarean section).13
The future
Practice guidelines and protocols may help to ensure safe and consistent obstetric practice. Forceps delivery may offer advantages over caesarean section, but only if short and long term health benefits can be shown, including the potential for future uncomplicated spontaneous vaginal deliveries. Further research is required to evaluate women's overall reproductive outcome and satisfaction with the birth experience. The challenge for obstetricians is to make sure that options for safe delivery are not limited for women who experience complications in labour.
Supplementary Material
 References w1 to w28 and a patient's perspective on caesarean section are on bmj.com
References w1 to w28 and a patient's perspective on caesarean section are on bmj.com
Contributors: RRP and DJM coresearched and cowrote the review. DJM will act as guarantor for the review.
Competing interests: DJM has experienced a rotational forceps delivery and subsequently two spontaneous vaginal deliveries.
References
- 1.Thomas J, Paranjothy S. National sentinel caesarean section audit report. London: Royal College of Obstetricians and Gynaecologists Clinical Effectiveness Support Unit, 2001.
- 2.Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med 1999;341: 1709-14. [DOI] [PubMed] [Google Scholar]
- 3.Bofill JA, Rust OA, Perry KG, Roberts WE, Martin RW, Morrison JC. Operative vaginal delivery: a survey of fellows of ACOG. Obstetrics Gynecology 1996;88: 1007-10. [DOI] [PubMed] [Google Scholar]
- 4.Bewley S, Cockburn J. The unethics of `request' caesarean section. Br J Obstetr Gynaecol 2002;109: 593-6. [DOI] [PubMed] [Google Scholar]
- 5.Vacca A. The trouble with vacuum extraction. Curr Obstetr Gynaecol 1999;9: 41-5. [Google Scholar]
- 6.College of Physicians and Surgeons of Manitoba. Guidelines and statements. Assisted vaginal delivery: the use of forceps or vacuum extractor. www.umanitoba.ca/colleges/cps/Guidelines_and_Statements/638.html (accessed 18 Jun 2003).
- 7.Johanson RB. Instrumental vaginal delivery. London: Royal College of Obstetricians and Gynaecologists, 2000.
- 8.Hankins GD, Uckan E, Rowe TF, Collier S. Forceps and vacuum delivery: expectations of residency and fellowship training program directors. Am J Perinatol 1999;16: 23-8. [DOI] [PubMed] [Google Scholar]
- 9.Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R. Cohort study of the early maternal and neonatal morbidity associated with operative delivery in the second stage of labour. Lancet 2001;358: 1203-7. [DOI] [PubMed] [Google Scholar]
- 10.Mesleh RA, Al-Sawadi HM, Kurdi AM. Comparison of maternal and infant outcomes between vacuum extraction and forceps deliveries. Saudi Med J 2002;23: 811-3. [PubMed] [Google Scholar]
- 11.Okunwobi-Smith Y, Cooke I, MacKenzie IZ. Decision to delivery intervals for assisted vaginal vertex delivery. Br J Obstetr Gynaecol 2000;107: 467-71. [DOI] [PubMed] [Google Scholar]
- 12.DiMatteo MR, Morton SC, Lepper HS, Damush TM, Carney MF, Pearson M, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychology. NHS Centre for Reviews and Dissemination 1996;15: 303-14. [DOI] [PubMed] [Google Scholar]
- 13.Bahl R, Strachan B, Murphy DJ. Outcome of subsequent pregnancy three years after previous operative delivery in the second stage of labour: cohort study. BMJ 2004;328: 311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johanson RB, Menon V. Vacuum extraction versus forceps for assisted vaginal delivery. Cochrane Database Syst Rev 2000;(2): CD000224. [DOI] [PubMed]
- 15.Kabiru WN, Jamieson D, Graves W, Lindsay M. Trends in operative vaginal delivery rates and associated maternal complication rates in an innercity hospital. Am J Obstetr Gynecol 2001;184: 1112-4. [DOI] [PubMed] [Google Scholar]
- 16.Handa VL, Danielsen BH, Gilbert WM. Obstetric anal sphincter lacerations. Obstetr Gynecol 2001;98: 225-30. [DOI] [PubMed] [Google Scholar]
- 17.Fitzpatrick M, Behan M, O'Connell PR, O'Herlihy C. Randomised clinical trial to assess anal sphincter function following forceps or vacuum assisted vaginal delivery. Br J Obstetr Gynaecol 2003;110: 424-9. [PubMed] [Google Scholar]
- 18.Liebling RE, Swingler R, Patel RR, Verity L, Soothill PW, Murphy DJ. Pelvic floor morbidity up to one year following difficult instrumental delivery and caesarean section in the second stage of labour: a cohort study. Am J Obstetr Gynecol 2004. (in press). [DOI] [PubMed]
- 19.Murphy DJ, Stirrat GM, Heron J, ALSPAC Study Team. The relationship between caesarean section and subfertility in a population-based sample of 14,541 pregnancies. Hum Reprod 2002:17: 1914-7. [DOI] [PubMed] [Google Scholar]
- 20.Chow SL, Johnson CM, Anderson TD, Hughes JH. Rotational delivery with Kielland's forceps. Med J Aust 1987;146: 616-9. [DOI] [PubMed] [Google Scholar]
- 21.Revah A, Ezra Y, Farine D, Ritchie K. Failed trial of vacuum or forceps—maternal and fetal outcome. Am J Obstetr Gynecol 1997;176: 200-4. [DOI] [PubMed] [Google Scholar]
- 22.Badawi N, Kurinczuk JJ, Keogh JM, Alessandri LM, O'Sullivan F, Burton PR, et al. Intrapartum risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ 1998;317: 1554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy DJ, Pope C, Frost J, Liebling RE. Women's views on the impact of operative delivery in the second stage of labour—qualitative study. BMJ 2003;327: 1132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy DJ, Liebling RE. Cohort study of maternal views on future mode of delivery following operative delivery in the second stage of labor. Am J Obstetr Gynecol 2003;188: 542-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.