Abstract
Aim
The aim was to find an optimal setup image matching position and minimal setup margins to maximally spare the organs at risk in breast radiotherapy.
Background
Radiotherapy of breast cancer is a routine task but has many challenges. We investigated residual position errors in whole breast radiotherapy when orthogonal setup images were matched to different bony landmarks.
Materials and methods
A total of 1111 orthogonal setup image pairs and tangential field images were analyzed retrospectively for 50 consecutive patients. Residual errors in the treatment field images were determined by matching the orthogonal setup images to the vertebrae, sternum, ribs and their compromises. The most important region was the chest wall as it is crucial for the dose delivered to the heart and the ipsilateral lung. Inter-observer variation in online image matching was investigated.
Results
The best general image matching position was the compromise of the vertebrae, ribs and sternum, while the worst position was the vertebrae alone (p ≤ 0.03). The setup margins required for the chest wall varied from 4.3 mm to 5.5 mm in the lung direction while in the superior–inferior (SI) direction the margins varied from 5.1 mm to 7.6 mm. The inter-observer variation increased the minimal margins by approximately 1 mm. The margin of the lymph node areas should be at least 4.8 mm.
Conclusions
Setup margins can be reduced by proper selection of a matching position for the orthogonal setup images. To retain the minimal margins sufficient, systematic error of the chest wall should not exceed 4 mm in the tangential field image.
Keywords: Radiotherapy, Breast cancer, Setup errors, Image guidance, Setup margins, Free breathing
1. Background
Radiotherapy (RT) of the breast is a challenging task. The shape of the breast may vary both intra- and inter-fractionally. Moreover, respiratory breathing cycle causes uncertainties in the treatment localization. The breast may move up to 1 cm1 with respiration while the average motion has been found to vary from 2 to 4 mm, similar to that of the chest wall.2 Recently, breathing control techniques such as gating3 or voluntary deep inspiration breath hold (vDIBH)4 have been introduced. Unfortunately, these techniques are resource-intensive and cannot be applied for non-cooperative patients or patients with reduced breath-holding capability. While the target shape may best be evaluated with 3D techniques, such as cone beam computed tomography (CBCT),5 the frequency of 3D acquisitions varies considerably between the centers and routine treatment setup is usually based on 2D images. Moreover, there is no clear consensus on the benefits of the CBCT for standard breast cancer patients.6 Therefore, investigation of target localization with 2D position verification still remains highly relevant.
The existing 2D image guided radiotherapy (IGRT) protocols vary considerably between centers. Some clinics use merely orthogonal setup images or tangential images from treatment beam directions while others use both of these.7 The breast itself is not visible in the orthogonal setup images and choice of the representative anatomic landmarks for image alignment is not a straightforward task because the correlation of the landmarks with the breast is not obvious. On the other hand, the breast is visible in the tangential images but these are susceptible to respiratory motion. Moreover, it is impossible to decide appropriate couch corrections in anterior–posterior and lateral directions based merely on the tangential images. Therefore, acquisition of orthogonal images or patient re-simulation is needed, when the setup errors exceed the tolerances in the tangential Images.8
The guidelines of the matching position vary for the orthogonal images. Some centers use the sternum and the ribs9 while others include also the vertebrae6 or use the vertebrae alone. To the best of our knowledge, residual position errors in the tangential images have not previously been evaluated and compared for different matching positions of the orthogonal setup images.
2. Aim
In this study, we investigated residual position errors in the tangential treatment field images when the orthogonal setup images were aligned in different ways. These alignments were based on relevant bony landmarks, such as the vertebrae, the sternum, the ribs and their combinations. The aim was to find the best landmarks with the smallest position errors and thus minimal setup margins to maximally spare the organs at risk. The magnitude of margins is most pronounced with modern intensity modulated techniques providing highly conformal dose distributions.10 We evaluated inter-observer variation in the image matching advised to the optimal matching position by determining residual errors in the online IGRT performed by 25 experienced radiation therapists. Moreover, we determined residual errors of the landmarks relevant for the lymph node areas after the online match.
3. Materials and methods
3.1. Patient group and the IGRT protocol
A total of 50 consecutive left-sided breast cancer patients receiving adjuvant radiotherapy after breast conserving surgery were included in this study. The mean patient age was 63 years. The patients were immobilized with Candor's ConBine fixation device (Candor, Gislev, Denmark) with both arms elevated above the head. The device has adjustable arm supports and head cushion. The palm of contralateral hand was attached to the wrist of the ipsilateral hand. CT imaging for treatment planning was done with free breathing at 120 kVp with either Philips Brilliance Big Bore (Philips Medical Systems, Eindhoven, The Netherlands) or Toshiba Aquilion LB (Toshiba Medical System, Tokyo, Japan) scanners using a slice thickness of 3 mm. In our setup protocol, skin tattoo marks for laser setup were placed on the patients’ sternum and below the breast. Patients were treated to 50 Gy at 25 fractions with the two tangential field technique (n = 25) or four-field technique for lymph node irradiation (axillary and supraclavicular areas, n = 25) using 6 MV photon beams of Clinac 2300 iX accelerator (Varian Medical Systems, Palo Alto, CA).
The orthogonal kV-images were acquired daily with an onboard imaging system (OBI) at 75 kV/200 mA/25 ms for anterior images and at 95 kV/200 mA/200 ms for lateral images. The orthogonal kV images were used for couch translational corrections. The daily image guidance (IGRT) protocol included also a tangential MV field image acquired after the couch corrections for final verification of treatment localization. The dose related to the MV imaging (2 monitor units per image) was taken into account in the treatment planning. The acquired onboard images were analyzed retrospectively offline. All together, 1111 orthogonal X-ray image pairs and tangential field images were analyzed. 139 image sessions were not imaged for unknown reasons.
3.2. Estimation of the best bony landmarks for 2D image guidance
Region of the breast and lymph nodes was divided into relevant landmarks or subregions. These were the upper, middle and lower parts of the vertebrae (UP_V, MID_V, LOW_V), lower and middle parts of the ribs (LOW_R, MID_R), the middle part of the sternum (MID_ST) and the shoulder joint presented in Fig. 1. Residual position errors in the tangential field images were retrospectively determined for different matching locations of the orthogonal setup images. The setup images were aligned according to the vertebrae, the sternum and the ribs, and the compromise of these structures. All of these matching locations were in the middle of the breast in the superior–inferior direction (see Fig. 1). In alignments where several landmarks were used, average position of the given landmarks was used to determine the position correction. The retrospective match was done by the same observer (ML) for all 50 patients.
Fig. 1.
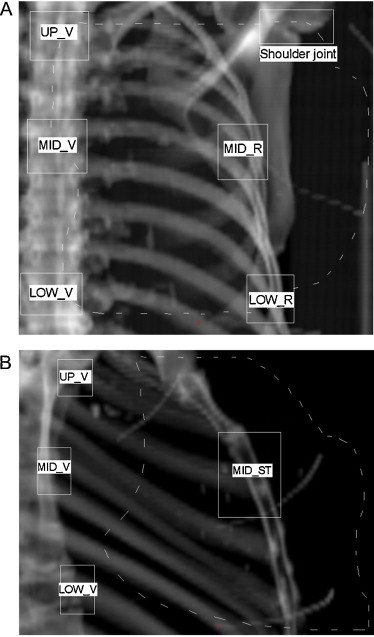
Selection of bony landmarks for alignment of orthogonal setup images and for determination of residual errors after the alignment. Residual errors are caused by flexible patient anatomy and rotation. The matching positions (open white boxes) are shown in (a) anterior reference image and (b) lateral reference image. The distances between the subregions were within ±2 cm for all patients. The projection of the target breast tissue is illustrated with a dashed line.
The position resulting in the smallest residual errors in the tangential treatment field image was considered optimal. The residual errors were determined for the chest wall (denoted usually as central lung distance (CLD)8) and for the breast surface (denoted usually as central flash distance (CFD) and inferior central margin (ICM)8). For the sternum and ribs, only the superior–inferior direction was investigated, because it was impossible to determine either lateral or anterior–posterior direction reliably. Because of the daily imaging, the effect of respiratory motion is well averaged in the data acquired during the treatment course.
3.3. Setup accuracy in the online match
Based on our preliminary data, the best matching position for the orthogonal images was the compromise of the vertebrae, the sternum and the ribs. Errors related to this image alignment in practice were investigated. This was done by determining residual errors of the above mentioned subregions, the clavicula and the shoulder joint after the online image match performed by 25 experienced radiation therapists in actual treatment situation. The errors were determined by the same observer (ML) for all 50 patients. The errors obtained include inter-observer variation in the interpretation of the optimal image matching position. The action level of zero (0 mm) was applied for couch corrections in each direction. The tangential field image was acquired after the couch corrections. Adequate setup margins relevant for the whole breast RT were calculated using the van Herk's formula , where Σ is systematic error and σ is random error. All directions are given as superior–inferior (SI), anterior–posterior (AP) and lateral (LAT). The AP and LAT directions are combined in the tangential images and this direction is denoted as AP/LAT direction.
3.4. Statistical analysis
The two-tailed F-test was chosen to evaluate the differences in systematic errors (test for equality of variances). This was considered relevant because the distributions of systematic errors are very close to Gaussian. The Wilcoxon signed rank test was used for paired testing of the systematic errors. The Wilcoxon rank sum test was used for the random errors (test for equality of means). For the last two, the most common non-parametric tests were chosen to avoid assumptions on error distributions. A p-value ≤0.05 was considered statistically significant.
4. Results
There were no significant differences (p > 0.5) between the breast-only group and the group treated for breast and lymph node regions. Therefore, the results of these groups were analyzed together.
4.1. Estimation of best bony landmarks for alignment of orthogonal setup images
Residual errors in the tangential field images and adequate setup margins are presented in Table 1 for different alignments of the orthogonal setup images. The means of signed residual errors were within 1 mm for all alignments. The matching position had only a small impact in the AP and LAT directions, while greater effect can be seen in the SI direction. The best general matching position was the compromise of the vertebrae, the sternum and the ribs (MID_V + MID_ST + MID_R) to minimize the position errors in the tangential images. This alignment had the smallest errors in the most important AP and LAT directions (regarding the sparing of the heart and lung). Moreover, the systematic error was only slightly larger in the SI direction than the smallest error obtained for the MID_R + MID_ST. In this alignment, position correction was based on the average position of these three landmarks. It can be seen from Table 1 that many alignments have only small differences in the SI direction.
Table 1.
The residual errors (mm) of the central lung distance and the breast surface (in parenthesis) with different combinations of matching positions for the orthogonal kV setup images.
| Landmark/combination of landmarks | Systematic error Σ (1 SD) |
Random error σ (1 SD) |
||
|---|---|---|---|---|
| AP/LAT direction | SI direction | AP/LAT direction | SI direction | |
| Laser setup | 2.9 (3.7) | 3.1 (2.5) | 2.7 (2.7) | 2.9 (2.5) |
| MID_V | 1.6 (2.7) | 2.3 (3.4) | 2.1 (2.2) | 2.7 (2.9) |
| MID_R + MID_ST | 1.6 (2.5) | 1.4 (2.8) | 1.9 (2.0) | 2.3 (2.4) |
| MID_V + MID_ST | 1.4 (2.4) | 1.7 (2.9) | 1.9 (2.0) | 2.3 (2.4) |
| MID_V + MID_R | 1.5 (2.6) | 2.0 (3.2) | 1.9 (2.1) | 2.4 (2.8) |
| MID_V + MID_ST + MID_R | 1.2 (2.3) | 1.6 (2.8) | 1.8 (1.9) | 2.3 (2.4) |
| MID_ST | – | 1.7 (2.9) | – | 2.4 (2.4) |
| MID_R | – | 2.0 (3.3) | – | 2.6 (2.4) |
| Online match to optimal positiona | 1.5 (2.6) | 1.8 (3.0) | 1.9 (2.0) | 2.6 (2.8) |
| Margins for the online match | 5.1 (7.9) | 6.3 (9.5) | – | – |
The results include inter-observer variation in image matching.
The worst image matching position was the vertebrae alone for all of the investigated patients. If the alignment is based purely on the vertebrae, the error of the chest wall exceeding 4 mm occurs in 14% and 30% of the cases in AP/LAT and SI directions, respectively. If the alignment is the best compromise of the vertebrae, sternum and ribs, the corresponding values were reduced to 6% and 15%, respectively. For the breast surface, the error of 7 mm in the SI direction is exceeded with the vertebrae alignment in 15% of the cases and with the best compromise match in 10% of the images.
For the best and worst orthogonal image alignments, the difference in the posterior breast setup margins differed 1.2 mm in the AP/LAT direction and 2.5 mm in the SI direction. Margins for the breast surface varied from 8.7 to 10.5 mm in the SI direction. The systematic errors were significantly different for these positions in the SI direction (p = 0.02) as were the random errors (p = 0.003). The systematic and random errors were not significantly different in the AP/LAT direction for other matching positions, but the systematic errors were significantly different in the paired comparison of the best and worst alignments (p = 0.03). In the SI direction, the random error in the best alignment was significantly better than the MID_R match (p = 0.02) and the online match (p = 0.02). Notice that the laser setup was not included in the p-comparisons.
4.2. Analysis of the online match
The online match results in Table 1 demonstrate that systematic errors in treatment localization can be reduced by introducing the guidelines for the optimal match position, but there is noticeable contribution from inter-observer variation. We observed that the orthogonal images tended to overestimate the correction for the breast surface in SI direction.
Residual errors of the subregions after the optimal online match are listed in Table 2. For the chest wall, the error of 4 mm is exceeded for 8% of the cases in the AP/LAT direction and for 28% in the SI direction. For the breast surface, the error of 7 mm was exceeded in 12% of the cases in the SI direction but not in the AP/LAT direction. The most unstable landmark was the shoulder joint.
Table 2.
Residual errors (mm) of different landmarks after the optimal online match with the daily IGRT protocol.
| Landmark | Systematic error Σ (1 SD) |
Random error σ (1 SD) |
||||
|---|---|---|---|---|---|---|
| AP | SI | LAT | AP | SI | LAT | |
| MID_V | 0.9 | 1.0 | 0.9 | 1.7 | 1.9 | 1.5 |
| MID_ST | 1.6 | 2.2 | – | 2.0 | 2.1 | – |
| UP_V | 1.4 | 1.3 | 1.0 | 1.8 | 2.1 | 1.7 |
| LOW_V | 1.2 | 1.1 | 1.4 | 1.7 | 2.2 | 1.9 |
| MID_R | – | 1.6 | 0.9 | – | 2.4 | 1.3 |
| LOW_R | – | 1.6 | 1.2 | – | 2.7 | 1.5 |
| Clavicula | – | 2.4 | 2.2 | – | 2.7 | 2.3 |
| Shoulder joint | – | 3.4 | 2.7 | – | 3.6 | 3.1 |
| Setup corrections | 2.0 | 2.9 | 2.0 | 2.0 | 3.1 | 2.6 |
5. Discussion
In this study, we investigated the position errors in RT of left-sided breast cancer accomplished in free tidal breathing. Due to patient rotation, breast shape changes and respiratory motion, we found it relevant to investigate optimal matching position for orthogonal 2D setup images. We also estimated how much the accuracy of the treatment field localization was reduced in daily treatment situation due to inter-observer variation in image matching. Furthermore, we estimated sufficient setup margins for the optimal matching position. The image matching was based on the bony landmarks related to the whole breast and lymph node areas. The results presented in Table 2 can be used in the evaluation of the consistency of our results against different immobilization systems and practices.
5.1. Estimation of the best bony landmarks for alignment of orthogonal setup images
The optimal image matching position for the orthogonal setup images was the compromise of the vertebrae, the sternum and the ribs (MID_V + MID_ST + MID_R). By using this position, the combined effect of both even and uneven respiratory motion and changes in patient posture and shape can be minimized for the tangential fields. With this alignment, the posterior breast setup margin in the AP/LAT direction was 4.3 mm. This is not much greater than the magnitude of a normal respiratory motion (typically within 1 mm but can be as large as 4 mm according to our clinical findings, and from 2 to 4 mm reported by Bedi et al.2). Therefore, this margin may be close to smallest possible margin of the posterior part of the breast achievable without breathing control techniques. In practice, however, the margin is rounded to 5 mm. To retain this margin sufficient, maximal acceptable systematic error should not exceed 4 mm (calculated as 2.5Σ by using the van Herk's formula and experimentally determined σ for the online match, as suggested by Kapanen et al.11). The difference in margins (1.2 mm) between the best and worst image alignments is over half of the planning organ at risk (PRV) margin of approximately 2 mm obtained for the heart12 or to the average maximal movement of the heart during treatment.1 This distance is clinically important as it corresponds to dose delivery of several grays to the heart13 and the ipsilateral lung.
The effect of image matching position was most pronounced in the SI direction. The lowest margin for that direction was 5.1 mm for the posterior part of the breast achievable by using the compromise of the ribs and the sternum (MID_R + MID_ST). The compromise of the MID_V + MID_ST + MID_R increased the margin only by 0.5 mm.
For the patients with the largest rotations and most flexible anatomy (n = 12), the inclusion of the vertebra reduced the optimality of the match. For such patients, the compromise of the MID_R and MID_ST was the most optimal choice, but we recommend that optimal image matching should be individually evaluated by comparing the orthogonal and tangential images (offline and/or online). Optimal setup of such challenging patients is under further investigation in our clinic.
Because dose to the most radiation sensitive organs, such as the heart and the ipsilateral lung, is determined by the margin in the AP/LAT direction, we consider that the MID_V + MID_ST + MID_R alignment is the best general choice for majority of patients. In practice, the margin is rounded to 6 mm in the SI direction. This is sufficient when systematic errors exceeding 4 mm are corrected (calculated as above). Correspondingly, systematic errors exceeding 7 mm should be corrected for the breast surface to retain the minimal margin of 9 mm sufficient (rounded from 8.7 mm). In our practice, however, we always confirm that the whole breast is inside the treatment field.
Our minimal margins are consistent with the values of 3.8 mm (AP/LAT direction) and 4.7 mm (SI direction) obtained with CBCT offline corrections by aligning the images to the sternum and the ribs.9 With online corrections, however, small margins of approximately 0.2 mm have been reported for the CBCT in both directions, while with the portal images a margin of 2.2 mm has been considered sufficient for the AP/LAT direction and 5.7 mm for the SI direction.9 The greater margins in our study can be explained by a more stringent formula used in the margin calculation and contribution of inter-fractional variation in patient posture. By using the same formula , our minimal margins would be only 3.1 (AP/LAT) and 4.1 mm (SI). Moreover, respiratory motion is averaged in the small CBCT margins.
By accounting for the inter-observer variation in image matching, approximately 1 mm should be added to the lowest margins obtained. The margin for the breast surface is not critical in the AP/LAT direction, because the tangential field size can be expanded freely in that direction to account for setup errors. Breast shape changes have negligible dosimetric effect on the tangential moderately intensity-modulated fields.14
The presented margins are valid for whole breast irradiations performed in free breathing. For partial breast irradiations,15 larger margins up to 1 cm16 and the use of implanted markers are recommended.16,17 Average marker movements of 4 mm have typically been observed.17 Optimal image alignment and required margins should be estimated separately for breast treatments in deep inspiration breath hold. This topic is under investigation in our clinic.
5.2. The online match
Localization errors caused by inter-observer variation in the selection of optimal matching position are rarely determined in the literature. In our study, these errors were included in the online match results. According to initial results of our ongoing study, the extracted contribution of inter-observer variation in the orthogonal image matching is 1.2 and 1.5 mm in AP/LAT and SI directions, respectively. The smallest residual errors for the vertebrae suggest that the match was done slightly more toward the vertebrae than to the pure compromise of the landmarks. This may be solved by improving the matching guidelines. Because the error in the online match was most pronounced in the SI direction, it might be useful to utilize the tangential images for the final verification of the SI direction. Our results suggest that the setup margins for the breast surface should still be close to 1 cm, which is conventionally recommended in literature.8 For patients treated with free breathing, it would be interesting to investigate potential benefits of breathing training18 when breathing pattern is clearly uneven.
In the online match, the margin required for the upper part of the vertebrae was up to 4.8 mm and up to 7.8 mm for the clavicula. These margins should be applied for planning of the lymph node volumes but the relation between the planned volume and these landmarks should be confirmed (e.g. by using CBCT). The average movement of the lymph node volume with respiratory motion is less than 2 mm.1 The best image matching position (the compromise of the MID_V + MID_ST + MID_R) is feasible also for the breast treatments including the lymph node areas because the vertebrae are included. The relation of the shoulder joint to the lymph node volume has not been investigated.
6. Conclusions
In conclusion, the best matching position for the orthogonal setup images is the compromise of the vertebrae, the sternum and the ribs to minimize residual position errors in the tangential treatment field images and to minimize the setup margins required to maximally spare the organs at risk (OAR). In that alignment, position corrections in the AP, LAT and SI directions are based on the average position of these landmarks. The effect of image matching position was most pronounced in the SI direction, while it was smaller in the AP and LAT directions. Application of minimal margins to maximally spare the OARs is possible if systematic errors in central lung distance are not allowed to exceed 4 mm in any direction. If this limit is exceeded (systematically in 3–4 successive fractions), we propose corrective actions. In the SI direction, at least 8.7 mm margin is required for the breast surface. After the couch corrections, we suggest re-acquisition of the tangential field image for the final confirmation of the setup of breast surface, especially in the SI direction. Margins ranging from 4.8 mm to 7.8 mm should be used for the lymph node areas depending on the relevant bony landmarks for the planned area.
Conflict of interest
None declared.
Financial disclosure
This study was supported by the Pirkanmaa Hospital District, Finland, Elna Kaarina Savolainen fund (Grant No. R12536).
Acknowledgements
Radiation therapist students Helmi Luukkanen and Risto Manninen are greatly acknowledged for participating in the analysis of inter-observer variation.
Contributor Information
Marko Laaksomaa, Email: marko.laaksomaa@pshp.fi.
Mika Kapanen, Email: mika.kapanen@pshp.fi.
Tanja Skyttä, Email: tanja.skytta@pshp.fi.
Simo Hyödynmaa, Email: simo.hyodynmaa@pshp.fi.
Pirkko-Liisa Kellokumpu-Lehtinen, Email: pirkko-liisa.kellokumpu-lehtinen@pshp.fi.
References
- 1.Qi S., White J., Rabinovitch R. Respiratory organ motion and dosimetric impact on breast and nodal irradiation. Int J Radiat Oncol Biol Phys. 2010;78:609–617. doi: 10.1016/j.ijrobp.2009.11.053. [DOI] [PubMed] [Google Scholar]
- 2.Bedi C., Kron T., Willis D., Hubbard P., Milner A., Chua C. Comparison of radiotherapy treatment plans for left sided breast cancer patients based on three- and four-dimensional computed tomography imaging. Clin Oncol. 2011;23:601–607. doi: 10.1016/j.clon.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Korreman S.S., Pedersen A.N., Nøttrup T.J., Specht L., Nyström H. Breathing adapted radiotherapy for breast cancer: comparison of free breathing gating with the breath-hold technique. Radiother Oncol. 2005;76:311–318. doi: 10.1016/j.radonc.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Borst G.R., Sonke J.J., den Hollander S. Clinical results of image-guided deep inspiration breath hold breast irradiation. Int J Radiat Oncol Biol Phys. 2010;78:1345–1351. doi: 10.1016/j.ijrobp.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Hasan Y., Kim L., Wloch J. Comparison of planned versus actual dose delivered for external beam accelerated partial breast irradiation using cone-beam CT and deformable registration. Int J Radiat Oncol Biol Phys. 2011;80:1473–1476. doi: 10.1016/j.ijrobp.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Fatunase T., Wang Z., Yoo S. Assessment of the residual error in soft tissue setup in patients undergoing partial breast irradiation: results of a prospective study using cone-beam computed tomography. Int J Radiat Oncol Biol Phys. 2008;70:1025–1034. doi: 10.1016/j.ijrobp.2007.07.2344. [DOI] [PubMed] [Google Scholar]
- 7.National Cancer Action Team (NCAT) NCAT; London: 2012. National radiotherapy implementation group report – image guided radiotherapy: guidance for implementation and use. [Google Scholar]
- 8.Royal College of Radiologists (RCR) Royal College of Radiologists; London: 2008. On target: ensuring geometric accuracy in radiotherapy (BFCO (08)5) [Google Scholar]
- 9.Topolnjak R., Sonke J.J., Nijkamp J. Breast patient setup error assessment: comparison of electronic portal image devices and cone-beam computed tomography matching results. Int J Radiat Oncol Biol Phys. 2010;78:1235–1243. doi: 10.1016/j.ijrobp.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Poortmans P., Marsiglia H., De las Heras M., Algara M. Clinical and technological transition in breast cancer. Rep Pract Oncol Radiother. 2013;18:345–352. doi: 10.1016/j.rpor.2013.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kapanen M., Laaksomaa M., Tulijoki T. Estimation of adequate setup margins and threshold for position errors requiring immediate attention in head and neck cancer radiotherapy based on 2D image guidance. Radiat Oncol. 2013;8:212. doi: 10.1186/1748-717X-8-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Topolnjak R., Borst G.R., Nijkamp J., Sonke J.J. Image-guided radiotherapy for left-sided breast cancer patients: geometrical uncertainty of the heart. Int J Radiat Oncol Biol Phys. 2012;82:e647–e655. doi: 10.1016/j.ijrobp.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 13.Mavroidis P., Axelsson S., Hyödynmaa S. Effects of positioning uncertainty and breathing on dose delivery and radiation pneumonitis prediction in breast cancer. Acta Oncol. 2002;41:471–485. doi: 10.1080/028418602320405078. [DOI] [PubMed] [Google Scholar]
- 14.van Mourik A., van Kranen S, den Hollander S. Effects of setup errors and shape changes on breast radiotherapy. Int J Radiat Oncol Biol Phys. 2011;79:1557–1564. doi: 10.1016/j.ijrobp.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 15.Anbumani S., Palled S.R., Prabhakar G.S., Nambiraj N.A., Pichandi A. Accelerated partial breast irradiation using external beam radiotherapy – a feasibility study based on dosimetric analysis. Rep Pract Oncol Radiother. 2012;17:200–206. doi: 10.1016/j.rpor.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Coles C.E., Harris E.J., Donovan E.M. Evaluation of implanted gold seeds for breast radiotherapy planning and on treatment verification: a feasibility study on behalf of the IMPORT trialists. Radiother Oncol. 2011;100:276–281. doi: 10.1016/j.radonc.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Leonard C.E., Tallhamer M., Johnson T. Clinical experience with image-guided radiotherapy in an accelerated partial breast intensity-modulated radiotherapy protocol. Int J Radiat Oncol Biol Phys. 2010;76:528–534. doi: 10.1016/j.ijrobp.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Chopra S., Dinshaw K.A., Kamble R., Sarin R. Breast movement during normal and deep breathing, respiratory training and set up errors: implications for external beam partial breast irradiation. Br J Radiol. 2006;79:766–773. doi: 10.1259/bjr/98024704. [DOI] [PubMed] [Google Scholar]


