Abstract
Agranulocytosis is defined as an absolute neutrophil count less than 100/mm3 in association with infectious disease. The risk of agranulocytosis is 0.38% of all clozapine treated cases and there is a relatively lesser incidence in Indian population. The risk of clozapine-induced agranulocytosis and neutropenia is highest in the first 6 months and higher in the initial 18 months after the onset of treatment. There have been very few reports of neutropenia and agranulocytosis after this period. There have so far been no reports of late onset clozapine induced agranulocytosis has been reported from India. A case of late onset clozapine induced agranulocytosis with possible mechanism of the same is reported.
Keywords: Agranulocytosis, clozapine, granulocyte-colony stimulating factor, neutropenia, schizophrenia
INTRODUCTION
Clozapine has emerged as the gold standard for the treatment of treatment refractory schizophrenia. The most serious clozapine induced adverse effect is agranulocytosis. Agranulocytosis is defined as an absolute neutrophil count (ANC) less than 100/mm3 in association with infectious disease.[1]
The risk of agranulocytosis is 0.38% of all clozapine treated cases and there is a relatively lesser incidence in Indian population.[1,2] The risk of clozapine-induced agranulocytosis and neutropenia is highest in the first 6 months and higher in the initial 18 months after the onset of treatment.[1] There have been very few reports of neutropenia and agranulocytosis after this period. The reports of clozapine induced agranulocytosis in co-morbid multiple sclerosis and delayed onset neutropenia[3] and 2 reports of early treatment phase clozapine induced agranulocytosis have been reported from India,[3] so far no reports of late onset clozapine induced agranulocytosis has been reported from India.
CASE REPORT
A 44-year-old female patient with a diagnosis of paranoid schizophrenia, on clozapine treatment and regular follow-up presented in psychiatry outpatient department with fever, rigor, swelling of the right hand and sore throat. She has a 22 year history of fear suspicion and hearing voices with history of treatment with typical and atypical antipsychotics and poor treatment response. She was started on clozapine around 5 years back and subsequently given risperidone and trihexyphenidyl. At the time of presentation, she was on 150 mg of clozapine, 6 mg of risperidone and 4 mg of trihexyphenidyl. A total count done 1 week back showed 6,700/mm3 with 70% neutrophils, 26% lymphocytes and 4% eosinophils. She was on examination, conscious, oriented, febrile, had a pulse rate of 96/min, her blood pressure was 110/60 mm of Hg, diffuse swelling of right upper limb, her systemic examination was normal and had on mental status examination persecutory delusions and third person auditory hallucinations. She was admitted under the department of internal medicine and worked up.
On admission, her hemoglobin level was 8.1 g/dl, total count was 700, her differential count was N4P95E1, packed cell volume (PCV) was 25.3%, erythrocyte sedimentation rate - 140 mm/1st h, platelet count was 6.8 lakhs/dl, random blood sugar was 100 mg/dl, urea - 14 mg/dl, creatinine - 1.1 mg/dl, total bilirubin - 0.8 mg/dl, serum glutamic oxaloacetic transaminase - 103 IU/L, serum glutamic-pyruvic transaminase - 102 IU/L, serum alkaline phosphatase (SAP) - 125IU/L, total protein - 8 g/dl, A:G ratio was 1:2, human immunodeficiency virus and hepatitis B surface antigens were negative, chest X-ray was normal, electrocardiogram was normal, computed tomography head was normal, ultrasonography abdomen was normal, but Doppler of right upper limb showed dilatation of cephalic vein (4.2 mm) with echogenic content and thrombus extending up to axillary vein with non-compressibility and no internal flow. Her peripheral smear showed leucopenia with agranulocytosis and thrombocytosis. Her ANC was less than 100. She was diagnosed as having - drug induced agranulocytosis and deep vein thrombosis of right upper limb.
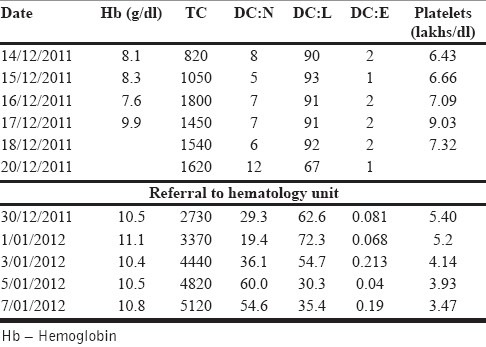
She was started on antibiotics (cefoperazone + sulbactum), warfarin, analgesics, proton pump inhibitors, supportive measures, barrier nursing and was given granulocyte-colony stimulating factor 300 μg for 7 days. The bone marrow examination and biopsy carried out post-treatment showed lymphocytosis with 6% blasts. She however was at request referred to a specialized hematology unit and was treated there with antibiotics (amoxicillin + clavulanic acid) warfarin, analgesics, proton pump inhibitors, supportive measures and barrier nursing. The sequential counts are summarized in Table 1.
Table 1.
Improvement of blood picture
Patient in the meantime had an exacerbation of psychotic symptoms and was given risperidone, chlorpromazine and trihexiphenidyl. The patient on improvement of blood picture was discharged on oral antibiotics, warfarin, mupirocin ointment, glycerine mag sulfate thrombocytophobe dressing, risperidone 3 mg, chlorpromazine 150 mg and trihexyphenidyl 2 mg. The patient had an asymptomatic course and was reviewed by both medicine and psychiatry. At 6 months post event follow-up, she has a total count of 7,800 with differentials of P72L26E2. She is currently on 8 mg of risperidone, 50 mg of chlorpromazine and 4 mg of trihexiphenidyl and is in partial symptom remission and not on any other medication.
DISCUSSION
The mechanism of clozapine-induced of agranulocytosis is unclear especially as neither clozapine nor its major stable metabolites, N-desmethylclozapine at therapeutic drug concentrations (1-3 μM), have been found to be directly cytotoxic to neutrophils or interfere with the turnover of bone marrow precursor cells.[4,5] A strong possibility is for an immune-mediated mechanism or at least an immunological background for clozapine-induced agranulocytosis, as on re-exposure to the drug, the course is more severe and the time interval to recurrence of toxicity is shorter.[6] Of the known risk factors of agranulocytosis such as female sex and increased age or age less than 21 of which this case had one risk factor. There is also an association between eosinophilia and neutropenia, which was not seen in this case.[1] The report of delayed onset agranulocytosis is very rare and this is the first reported from India on a patient without co-morbidity. The mechanism of delayed onset agranulocytosis is unclear. Treatment with clozapine generally lasts months or even years. It is hypothesized modest growth-inhibiting effects of clozapine on bone marrow may be amplified in patients undergoing long-term therapy with clozapine. Dose and serum levels of clozapine may not be directly associated with clozapine-induced agranulocytosis, although some reports suggest a dose-related aspect of this phenomenon.[7,8] The phenomenon of late onset agranulocytosis should therefore be considered with care and all clinicians should insist to regular guideline based monitoring of white cell count, even in patients who have been on clozapine for years.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Alvir JM, Lieberman JA, Safferman AZ, Schwimmer JL, Schaaf JA. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med. 1993;329:162–7. doi: 10.1056/NEJM199307153290303. [DOI] [PubMed] [Google Scholar]
- 2.Srinivasan TN, Thomas K. Clozapine-induced agranulocytosis and use of G-CSF. Indian J Psychiatry. 1998;40:70–2. [PMC free article] [PubMed] [Google Scholar]
- 3.Raveendranathan D, Sharma E, Venkatasubramanian G, Rao MG, Varambally S, Gangadhar BN. Late-onset clozapine-induced agranulocytosis in a patient with comorbid multiple sclerosis. Gen Hosp Psychiatry. 2012;35:574. doi: 10.1016/j.genhosppsych.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 4.Pirmohamed M, Park K. Mechanism of clozapine-induced agranulocytosis: Current status of research and implications for drug development. CNS Drugs. 1997;7:139–58. doi: 10.2165/00023210-199707020-00005. [DOI] [PubMed] [Google Scholar]
- 5.Williams DP, Pirmohamed M, Naisbitt DJ, Uetrecht JP, Park BK. Induction of metabolism-dependent and-independent neutrophil apoptosis by clozapine. Mol Pharmacol. 2000;58:207–16. doi: 10.1124/mol.58.1.207. [DOI] [PubMed] [Google Scholar]
- 6.Dunk LR, Annan LJ, Andrews CD. Rechallenge with clozapine following leucopenia or neutropenia during previous therapy. Br J Psychiatry. 2006;188:255–63. doi: 10.1192/bjp.188.3.255. [DOI] [PubMed] [Google Scholar]
- 7.Flanagan RJ, Dunk L. Haematological toxicity of drugs used in psychiatry. Hum Psychopharmacol. 2008;23(Suppl 1):27–41. doi: 10.1002/hup.917. [DOI] [PubMed] [Google Scholar]
- 8.Pessina A, Turlizzi E, Bonomi A, Guizzardi F, Cavicchini L, Croera C, et al. In vitro toxicity of clozapine, olanzapine, and quetiapine on granulocyte-macrophage progenitors (GM-CFU) Pharmacopsychiatry. 2006;39:20–2. doi: 10.1055/s-2006-931475. [DOI] [PubMed] [Google Scholar]


