Abstract
A significant body of research among female sex workers (FSWs) has focused on individual-level HIV risk factors. Comparatively little is known about their non-commercial, steady partners who may heavily influence their behavior and HIV risk. This cross-sectional study of 214 FSWs who use drugs and their male steady partners aged ≥18 in two Mexico-U.S. border cities utilized a path-analytic model for dyadic data based upon the Actor-Partner Interdependence Model to examine relationships between sexual relationship power, intimate partner violence (IPV), depression symptoms, and unprotected sex. FSWs’ relationship power, IPV perpetration and victimization were significantly associated with unprotected sex within the relationship. Male partners’ depression symptoms were significantly associated with unprotected sex within the relationship. Future HIV prevention interventions for FSWs and their male partners should address issues of sexual relationship power, IPV, and mental health both individually and in the context of their relationship.
Keywords: female sex workers, couples, drug use, intimate partner violence, dyadic data analysis, HIV risk, Mexico
INTRODUCTION
Tijuana and Ciudad Juarez, Mexico are two Mexico-U.S. border cities situated along key drug trafficking routes (1). Sex work is legal within specified city zones in Tijuana and Ciudad Juarez (2). Although Mexico has a low prevalence of HIV overall, HIV prevalence among female sex workers (FSWs) in Tijuana and Ciudad Juarez is significantly higher than the general population and has been increasing over the past decade (3-5). For example, the estimated HIV prevalence among FSWs in Tijuana is around 6%, and 14% among FSWs who inject drugs (4, 6); whereas, the national HIV prevalence in Mexico is around 0.3% (3).
Patterson et al. (7) tested a brief HIV/STI risk reduction intervention for FSWs (Mujer Segura or ‘Healthy Woman’) in Mexico which resulted in significant decreases in unprotected sex with male clients, but did not decrease FSWs’ unprotected sex with non-commercial, steady partners (8). Among FSWs who reported consistent condom use with clients, STI incidence at follow-up was 20 per 100 person/years, whereas STI prevalence among clients was less than 5% (9, 10). FSWs’ lack of condom use with their non-commercial steady partners and the continued high STI incidence among FSWs suggested STI infection from steady partners (8, 9). As a result, we designed this couples-based study to examine both FSWs’ and their non-commercial steady partners’ influence on each other’s HIV sex risk behavior.
While most previous research has focused on individual-level risk factors among FSWs who use drugs, comparatively little is known about their non-commercial steady partners, who may heavily influence their behavior and level of risk. To our knowledge, this is one of the first studies among FSWs who use drugs and their non-commercial steady partners to apply dyadic data analysis to examine how each person in the couple may affect his or her partner’s HIV sex risk. Information from this study may identify dimensions of individual and partner-based risk that are amenable to change in future interventions.
Theoretical Framework
The theoretical framework for this study is based upon the Theory of Gender and Power (11, 12), and the Syndemic Model of Substance Abuse, Intimate Partner Violence (IPV), HIV infection, and Mental Health among Hispanics (13, 14). The Theory of Gender and Power, applied to the context of HIV risk, posits that gender-based power inequities in society and in heterosexual relationships (including IPV) can reduce women’s control over their use of condoms, thus increasing their risk for HIV. Gonzalez-Guarda et al.’s Syndemic Model (13), based upon Substance Abuse, Violence, and AIDS (SAVA) Syndemic theory (15, 16), conceptualizes substance abuse, IPV, mental health (e.g., depression), and HIV infection as interwoven conditions with common social, cultural, and environmental roots that contribute to disproportionate disease burden among Hispanics and other vulnerable groups.
Intimate Partner Violence, Relationship Power, and HIV Sex Risk
IPV is defined as the occurrence of psychological, physical, or sexual victimization in the context of an intimate dating or married relationship (17). The association between IPV and HIV risk among heterosexual women has been documented in different international settings (18, 19) and age groups (20). The relationship between forms of abuse such as history of childhood abuse, IPV, and client-perpetrated violence and HIV infection among FSWs is well documented (21-25), but few studies focused on IPV specifically. However, previous research with FSWs in Mexico has shown IPV to be associated with history of abuse as a child, having a spouse or steady partner who is having sex with another partner (e.g., partner concurrency), and having less sexual relationship power (26). IPV among general population samples of Mexican women has been shown to be associated with women’s depression, history of child abuse, working outside of the home, and male partners’ unemployment and high frequency of alcohol use (27, 28). Other studies in Mexico, however, have found women’s employment and ability to decide whether to work reduced the risk of IPV (29, 30). Thus, additional research is still needed examining the context and social implications of IPV in Mexico.
Although the causal links between IPV and HIV sex risk have not been established, women’s relationship power may play an important role. For example, gender-based power imbalances may constrain women’s ability to negotiate condom use. Some define relationship power in terms of economic status (e.g. higher education, higher paying job) (31), whereas others define it as having control and dominating decisions in sexual relationships (32). Since the proposed study focuses on HIV sex risk behaviors, we utilized the Pulerwitz et al. (32) definition of relationship power. Empirically-tested studies designed to address IPV and relationship power among FSWs who use drugs are lacking. Results from this study will provide important information addressing this research gap. A better understanding of the role of gendered-power relationships among Mexican FSWs who use drugs and their partners will help to inform future HIV prevention interventions with this population.
Psychological Distress and HIV Risk
The prevalence of psychological distress among FSWs is well documented internationally (33-38). In 1998, Farley et al. (39) suggested that psychological distress among sex workers should be treated as a health crisis just as important as the HIV epidemic. Recently, Surrat et al. (36) found that serious mental illness mediated the relation between trauma and unprotected sex among FSWs in Miami, and Lau et al. (35) found that psychological problems were significantly associated with inconsistent condom use among FSWs in Hong Kong. Despite these studies, there is little research examining depression specifically, and its relation to HIV risk. “Psychological distress,” “serious mental illness,” and “psychological problems” are general terms usually comprised of any combination of anxiety, depression, and posttraumatic stress disorder symptoms making comparisons of mental health status across FSW studies difficult. This study examined depression symptoms specifically given the consistently high rates of depression symptoms documented among FSW populations (33, 35, 37, 40, 41).
Purpose
The purpose of this study was to examine both individual and partner-level correlates of HIV risk among FSWs who use drugs and their main sexual partners in Tijuana and Ciudad Juarez, Mexico. We applied dyadic modeling techniques based upon the Actor-Partner Interdependence Model (APIM)(42) to assess multiple risk factors for unprotected sex at both the individual and couple level. Based upon previous research with Latina samples (18, 26, 43), we hypothesized that for FSWs who use drugs lower relationship power, higher prevalence of IPV, and more depression symptoms would be associated with increased unprotected sex with their male, non-commercial steady partners. We hypothesized for male partners, higher relationship power, higher prevalence of IPV, and more depression symptoms would be associated with higher rates of unprotected sex with their FSW partners.
METHODS
Participants
This study utilized data obtained from baseline interviews of 428 participants (214 couples) enrolled in a prospective epidemiological study (Proyecto Parejas) of HIV, STIs, and associated risk behaviors among FSWs who use drugs and their non-commercial male partners in Tijuana (n = 212) and Ciudad Juarez (n = 216), Mexico (44). Eligibility criteria for the women were: being at least 18 years old; report having exchanged sex for money, drugs, shelter, or goods in the past 30 days; report ever using heroin, cocaine, crack, or methamphetamine; report having a non-commercial male sexual partner for at least 6 months; report having sex with that partner in the past 30 days, and agree to receive antibiotic treatment for STIs if they tested positive (to allow for the differentiation of incident from prevalent cases at follow-up in the Proyecto Parejas study). Women were excluded if they planned to break up with their non-commercial partner, move in the next 24 months (participants were to be followed up every six months for twenty-four months), or if they reported extreme IPV in their current relationship or fear of IPV as a result of their participation in the study. Eligibility criteria for the male partners were: age 18 years or older; report being in a sexual relationship with the eligible FSW partner for at least 6 months; and report having had sex with this partner within the past 30 days.
Procedures
Participants were recruited through the female partner first using targeted sampling by pairs of male and female outreach workers in areas where sex workers and drug users are known to frequent (bars, motels, streets, alleys). Snowball sampling also occurred in which enrolled FSWs who use drugs could refer other FSWs who they knew to the study. All couples enrolled in the study underwent a two-step screening process (44). First, the female partner completed a 10-minute, interviewer-administered primary screening questionnaire to assess her eligibility. Women received $5 for their time regardless if they qualified for the study. Next, FSWs who met the eligibility criteria brought their primary male partner to the study offices for further screening. The second step was a couple verification screening process to assess their knowledge of each other and determine whether the couple might be falsifying their couple-status to enroll in the study and receive compensation. The couples underwent verification screening separately. The primary and couple verification screening questionnaires were programmed with Questionnaire Development System (QDS) software (45) to automatically exclude potential participants who did not meet the eligibility criteria or pass the couple verification process. Potential participants were not informed why they were ineligible for the study to protect the safety of the female partner in cases of extreme IPV and to prevent potential participants from informing other potential participants about the enrollment criteria.
A total of 335 women were screened; 245 (73.1%) were eligible. The top two reasons for not being eligible were: no lifetime use of cocaine, methamphetamine, or heroin (10.4%); and no sex work in the last month (6.9%). Fourteen (4.2%) FSWs were excluded at the primary screener phase because of risk for severe IPV. These women were referred to IPV services in the community. A total of 239 couples underwent the couple verification screening process: 230 (96.2%) passed and were eligible to enroll in the study. Of the nine couples who did not pass the couple verification screening process, two couples were excluded because of the male partner’s concerns about IPV, and seven were determined not to be real couples. Complete details on the development and methods of the screening and couple verification process, our IPV safety protocol, number of potential participants screened, and reasons for not being eligible are published elsewhere (44).
Couples who passed the screening process provided written informed consent, and underwent one-hour baseline interviews both together and separately by gender-matched interviewers. Individual interviews were confidential: no information from the individual interviews was shared with the other partner. Couples received $20 USD for the joint interview and an additional $20 USD for each individual interview. Institutional review boards at the University of California, San Diego, the Hospital General and El Colegio de la Frontera Norte in Tijuana, and the Universidad Autónoma de Ciudad Juárez approved all study protocols.
Measures
Demographics
A series of questions about demographic characteristics included age, education, marital status, whether or not they have children, and income.
Relationship power
Relationship power within the FSW’s and her steady male partner’s relationship was assessed using 12-items modified from the Relationship Control subscale of the Sexual Relationship Power Scale (32). Three condom-related items out of the 15 original Relationship Control subscale items were not included as recommended by Pulerwitz et al. (32) to reduce bias when conducting condom use research. Examples of the items used in this study include: “[Name of Partner] has more of a say than I do about important decisions that affect us;” and “[Name of Partner] always wants to know where I am.” Response choices were: “strongly disagree,” “disagree,” “agree,” and “disagree.” The SRPS was developed for use in HIV/STI research with a community health clinic sample of mostly (89%) Latina women and is available in both English and Spanish. Higher scores indicate greater relationship power. Cronbach’s alpha for the 12-item modified Relationship Control subscale in this study was 0.89 for women and 0.71 for men.
Intimate partner violence
Past year prevalence of IPV behaviors within the FSW’s and partner’s relationship was measured using 8 modified items from the Revised Conflict Tactics Scales Short Form (CTS2 ‘short form’) (46). For each item, participants were asked whether or not (yes or no) they perpetrated that behavior against their partner in the past year (e.g., “I punched or kicked or beat up my partner one or more times in the past year.”). They were also asked whether their partner had perpetrated that behavior against them in the past year (i.e., victimization). We computed separate IPV perpetration and victimization total scores by summing the number of “yes” responses to the IPV perpetration and victimization items. Cronbach’s alpha for the eight IPV perpetration items was 0.84 for FSWs and 0.75 for male partners. Cronbach’s alpha for the eight IPV victimization items was 0.84 and 0.76 for FSWs and male partners, respectively.
Depression symptoms
Depression symptoms (past week) were assessed using the 10-item, short form of the Center for Epidemiologic Studies – Depression Scale (47). The CES-D is reliable for use with Latino populations (48) and is available in Spanish. Response choices ranged from 0 = “rarely or none of the time (<1 day)” to 3 = “most or all of the time (5-7 days)”. We computed a depression symptoms total score by summing the responses of all ten CES-D items. Cronbach’s alpha for the CES-D in this study was 0.83 and 0.76 for FSWs and male partners, respectively.
Unprotected sex
Participants were asked to report the number of times they engaged in vaginal sex with their steady partner in the past month. They were then asked to report the number of acts that were unprotected. An unprotected sex ratio was calculated by dividing the total number of unprotected sex acts by the total number of sex acts in the past month.
Data Analyses
First, we examined descriptive statistics such as frequencies, means, and standard deviations for the demographic, relationship power, IPV, depression symptoms, and unprotected sex variables. Differences between FSWs and male partners were examined using paired t-tests or McNemar’s tests. IPV perpetration, victimization, and unprotected sex had non-normal distributions, therefore the more conservative Wilcoxon paired signed-rank test was used to examine gender differences for those variables. Pearson product-moment correlation coefficients were used to determine correlations among the variables of interest.
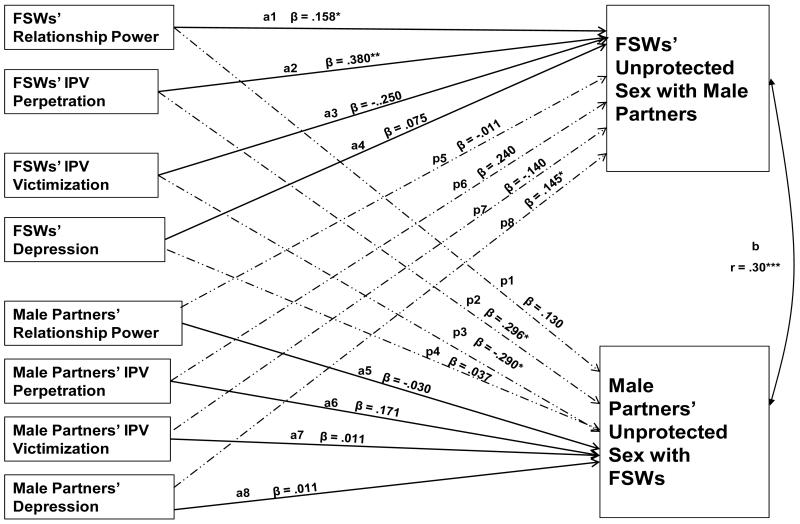
A path-analytic model for dyadic data based upon the Actor-Partner Interdependence Model (APIM) with distinguishable dyads(42) was tested to determine how unprotected sex is influenced by both members of the couple (Figure 1). The APIM model simultaneously estimates what are referred to as actor and partner effects on an outcome variable. For this study, the actor effects were the impact of a person’s relationship power, IPV perpetration and victimization, and depression symptoms on his or her own self-reported unprotected sex with their partner. The partner effects were the impact of each person’s relationship power, IPV perpetration and victimization, and depression symptoms on his or her partner’s unprotected sex. Paths labeled a1-a8 are the proposed actor effects; paths labeled p1-p8 are the proposed partner effects. The curved, double-headed arrow on the right (labeled b) represents the correlation between the two error terms as is required in dyadic data analysis. All predictor variables were allowed to correlate in the model, but are not depicted in the figure. The path analyses to assess the proposed model were conducted in Mplus 6.0 (49). Model fit was assessed using the χ2 statistic.
Figure 1.
Path-analytic model for dyadic data based upon the Actor-Partner Interdependence Model (APIM) examining the relations between relationship power, IPV, depression symptoms, and unprotected sex.
Note: Covariances between FSW and male partner error terms are estimated but not shown.
* Significant at p < .05
** Significant at p < .01
*** Significant at p < .001
RESULTS
Characteristics of FSW-intimate partner dyads
A total of 214 dyads participated in this study. The average length of relationship was 4.2 years (SD = 4.5), the majority of them were currently living together (99%), and 98% reported being married or in a common law relationship with each other. The majority of participants identified as heterosexual (97%). The mean age of participants was 35.3 years (SD = 9.4); the mean number of years of education was 7.3 years (SD = 2.6). The mean number of children participants had was 2.9 (SD = 1.7), and the mean number of financial dependents was 1.7 (SD = 1.5). In regards to income, more men than women (55% versus 40%, respectively) earned less than $2500 pesos a month (≤ US$200/month). By design the study targeted FSWs with a lifetime history of drug use (91% reported drug use in the past 6 months), but drug use in the past 6 months was also high for their partners (86%).
Means and standard deviations for the study variables by gender appear in Table 1. In regards to relationship power, FSWs had significantly higher mean total scores on the Relationship Control Subscale of the Sexual Relationship Power Scale than male partners: M = 33.7 (SD = 6.2) and M = 27.2 (SD = 4.8), respectively; t (211) = 10.78, p < .001. Among FSWs and their male partners, 47% of FSWs and 51% of male partners reported that they had perpetrated IPV in the past year. The mean number of IPV perpetration items engaged in by FSWs was M = 1.3 (SD = 1.9) and for male partners was M = 1.1 (SD = 1.5). This was not significantly different by gender: Z = −.775, p = .23. The mean number of IPV victimization items endorsed were M = 1.1 (SD = 1.8) and M = 1.2 (SD = 1.6) for FSWs and male partners, respectively (Z = −2.014, p < .05). In regards to depression symptoms, FSWs’ had significantly higher mean total scores on the CES-D compared to male partners: M = 11.8 (SD = 6.4), and M = 8.4 (SD = 5.2); t (213) = −6.37, p <.001. Lastly, FSWs differed significantly from male partners in regards to self-reported unprotected vaginal or anal sex acts with their study partner (past month). The mean percent of unprotected sex reported by FSWs was 87%, whereas male partners reported 81%: Z = −2.44, p < .01. Correlations of the study variables appear in Table 2. The only variable significantly correlated with either of the outcome variables was male partners’ depression symptoms: male partners’ depression symptoms was significantly correlated with FSWs’ unprotected sex (r = .14, p < .05). FSWs’ and male partners’ reports of unprotected sex with each other were significantly correlated (r = .33, p < .001).
Table 1.
Characteristics by FSWs vs. Male Partners (N = 428)
| FSWs (n = 214) |
Male Partners (n = 214) |
Test statistic (t, Z, or X2) |
|||
|---|---|---|---|---|---|
|
| |||||
| n (%) | Mean (SD) | n (%) | Mean (SD) | P value | |
| Age | 33.4 (9.0) | 37.3 (9.5) | .00*** | ||
| Years of school completed | 6.7 (2.9) | 7.4 (2.9) | .01** | ||
| Income (≤ $2500 pesos/month) |
85 (40%) | 118 (55%) | .00*** | ||
| Used drugs in last 6 months | 194 (91%) | 183 (86%) | .05* | ||
| Relationship Power | 33.7 (6.2) | 27.2 (4.8) | .00*** | ||
| IPV perpetration behaviors | 1.3 (1.9) | 1.1 (1.5) | .22 | ||
| IPV victimization behaviors | 1.1 (1.8) | 1.2 (1.6) | .02* | ||
| Depression symptoms | 11.8 (6.4) | 8.4 (5.2) | .00*** | ||
| % Unprotected Sex with study partner |
87.1 (30.5) | 80.6 (35.7) | .01** | ||
Significant at p < .05
Significant at p < .01
Significant at p < .001
Table 2.
Pearson Correlations for Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. FS Ws’ Relationship Power | --- | |||||||||
| 2. Male Partners’ Relationship Power |
−.29*** | --- | ||||||||
| 3. FS Ws’ IPV Perpetration | −.33*** | .18** | --- | |||||||
| 4. Male Partners’ IPV Perpetration | −.22*** | .28*** | .22*** | --- | ||||||
| 5. FS Ws’ IPV Victimization | −.33*** | .19** | .87*** | .28*** | --- | |||||
| 6. Male Partners’ IPV Victimization | −.17** | .21** | .27*** | .88*** | .26*** | --- | ||||
| 7. FS Ws’ Depression Symptoms | −.19** | .02 | .14* | .11 | .17** | .13 | --- | |||
| 8. Male Partners’ Depression Symptoms |
−.06 | .04 | −.02 | .11 | .04 | .10 | .14* | --- | ||
| 9. FS Ws’ Unprotected Sex with Male Partners |
.07 | .00 | .13 | .12 | .07 | .10 | .09 | .14* | --- | |
| 10. Male Partners’ Unprotected Sex with FSWs |
.10 | −.03 | .03 | .09 | −.04 | .09 | .02 | .00 | .33*** | --- |
Correlation is significant at the p < .05 level.
Correlation is significant at the p < .01 level.
Correlation is significant at the p < .001 level.
Dyadic Analyses
The resulting model fit the data well; χ2 = .05 for FSWs’ unprotected sex and χ2 = .08 for partners’ unprotected sex. Of the hypothesized paths specified within the model, two actor effects were statistically significant (see Figure 1): FSWs’ relationship power (path a1) and IPV perpetration (path a2) were positively associated with FSWs’ reports of unprotected sex with their partners (β = .158, p < .05; and β = .380, p < .01, respectively). There were three significant partner effects (see Figure 1): FSWs’ IPV perpetration (path p2) was positively associated with their partners’ reports of unprotected sex (β = .296, p < .05); FSWs’ IPV victimization (path p3) was negatively associated with their partners’ reports of unprotected sex (β = −.290, p < .05); and male partners’ depression symptoms (path p8) were positively associated with FSWs’ reports of unprotected sex (β = .145, p < .05).
DISCUSSION
This study was important in that to our knowledge, it is the first to simultaneously examine effects of sexual relationship power, IPV perpetration and victimization, and depression symptoms from both FSWs who use drugs and their non-commercial steady partners on unprotected sex within the relationship. Male partners’ depression symptoms were significantly associated with unprotected sex within the relationship, whereas, FSWs’ relationship power, IPV perpetration and victimization were significantly associated with unprotected sex within the relationship. Hypothesized paths between male partners’ sexual relationship power and IPV perpetration and victimization to unprotected sex in the relationship were non-significant. The results suggests that issues of relationship control and IPV may be more salient factors in relation to unprotected sex for FSWs compared to their male partners.
We hypothesized that FSWs’ with less relationship power and higher rates of IPV victimization would have a higher proportion of unprotected sex with their partners. Instead, FSWs’ greater sexual relationship power and higher IPV perpetration were associated with an increased proportion of unprotected sex with their male partners. This is consistent with findings from a study of women in substance abuse treatment where an increase in relationship control (measured by the SRPS) was significantly associated with increased unprotected sex for women with more severe substance use (≥ 13 days of drug use in past month) (50). In addition, Campbell and colleagues (51) found that women who did not intend to use condoms with their primary male partner had more unprotected sex as their relationship control increased. These findings underscore the importance of addressing desire to use condoms with steady partners. We assumed that FSWs’ greater sexual relationship power would translate to FSWs’ choosing to use condoms more often with their steady partners. However, greater relationship power may simply suggest that FSWs have a greater role in making decisions in their relationship. It does not necessarily mean that they will choose to use condoms or that they will have the presence of mind (i.e., not be under the influence of drugs which may impair their judgment) to be able to make safer sex decisions. In addition, FSWs may perceive condom use with their steady partners as a barrier to intimacy in the relationship, or as an implication of mistrust (52). They may also see condom use as a way of distinguishing work-related sexual relationships from personal sexual relationships (53).Therefore, sexual relationship power may not be sufficient in increasing drug-using FSWs’ condom use with their steady partners. Future HIV prevention research and interventions for FSWs who use drugs and their steady partners should address sexual relationship power and IPV in addition to attitudes about condoms, desire to use condoms within the relationship, trust, perceived HIV/STI risk from steady partners, and having sex under the influence of drugs (50).
FSWs’ relatively high rates of sexual relationship power compared to their male partners in this study and its association with unprotected sex may also be a result of non-adherence to traditional gender roles such as machismo (a traditional gender role orientation that accepts male dominance as a proper form of male conduct) and marianismo (a traditional female role orientation that accepts motherly nurturance and the demure and pure identity of a virgin as a proper form of female conduct)(54) by both the women and the men in this study. This is consistent with a previous qualitative study of FSWs and male partners in the Dominican Republic that found traditional Latino gender role conceptualizations were overly simplistic and did not capture the nuances of these unique relationships (55). It is possible that because of their status as sex workers and drug users, FSWs in our study violate traditional Mexican gender role norms for women, and therefore do not conform to more traditional Mexican gender roles in their personal relationships as well. It is also possible that the male partners’ lower income levels led to a more equal division of power in the relationship or higher levels of sexual relationship power for the FSWs. More research needs to be done in order to explain these findings in the social context of Mexico.
FSWs’ rates of IPV victimization in this study (42%) were higher than other studies of FSWs in Mexico (35%) (26), and Latina immigrants in San Diego County (16%) (56), but lower than other studies of FSWs in South Africa (63%) (25) and women who use drugs in the U.S. (68%) (57). Male partners’ rates of IPV perpetration (51%) in this study were higher than other studies of injection drug-using men (40%) (58) and Latino immigrant men in San Diego County (32%) (56). Reports of IPV victimization among male partners of FSWs are difficult to find, but IPV victimization rates in our study (51%) were higher than other studies reporting IPV victimization among drug-using males (25%) (59), and a community sample of homosexual, bisexual, and heterosexual Latino men in the U.S. (20%) (60). The high rates of IPV perpetration and victimization reported by both the male partners and the FSWs in the current study may be indicative of high conflict relationships in which it is difficult to negotiate relationship issues, including condom use. Unfortunately, this study did not ask who initiated the IPV; therefore it is unknown which member of the couple was engaging in IPV out of self-defense or in response to their partners’ acts of IPV.
In our study, FSWs’ higher sexual relationship power was significantly correlated with decreased IPV perpetration and victimization among both partners. In contrast, male partners’ increased sexual relationship power was significantly correlated with increased IPV perpetration and victimization among both partners. Therefore, when women in this study had greater sexual relationship power there was less conflict in the relationship, whereas when the male partners in this study had greater sexual relationship power, there was more conflict in the relationship. This is consistent with a study of women in Mexico which found that dimensions of women’s empowerment such as women’s ability to decide whether to work, when to have sexual relations, and the extent of their partners’ participation in household chores reduced the risk of IPV(29). It is possible that FSWs were dissatisfied with their partner’s higher level of sexual relationship power resulting in IPV, or it is also possible that men with more relationship power were also more combative. Future research may benefit from more in-depth mixed methods approaches that examine the context in which IPV occurs, who initiates IPV behaviors, what themes or areas of conflict result in IPV, and how this effects safer sex negotiation and practices within the relationship.
The significant association between male partners’ depression symptoms and FSWs’ unprotected sex may be indicative of male partners’ overall disadvantage and dependence on their FSW partners. Significantly more male partners earned less than $2500 pesos/month than FSWs in this study. This may be a result of the partners being more reliant on the FSWs and their income to support them and their drug habits. Male partners increased depression symptoms and lower earnings may reflect a dimension of personal capital. Having greater personal capital is consistent with the Theory of Gender and Power’s assertion that increased financial capital increases sexual relationship power. However, current measures of relationship power are lacking items assessing resource control and economic dependence. In post-hoc analyses, we re-ran our model with income as a covariate, but it did not change the significance level of any of the predictor variables on the outcomes. Future research should examine how male partners’ economic dependence on their FSWs partners and their compromised mental health may be capturing a part of relationship power dynamics not previously considered.
Limitations
There are a few limitations that should be recognized. First, this study was cross-sectional and did not examine changes in relationship status or power dynamics over time through repeated measures. A further limitation of cross-sectional data is that they do not support causal inferences. Future studies could benefit from the longitudinal exploration of relationship dynamics and HIV risk among high risk couples. Second, the results of this study may not be generalizable to other ethnic groups of couples, other FSWs and their partners, or other couples who do not use drugs. The sample in this study was a convenience sample from Tijuana and Ciudad Juarez, and may not be representative of couples in other Mexican cities or FSWs and their partners in Tijuana and Ciudad Juarez as a whole. Couples in this study were relatively stable in the length of time they were together and how long they had lived in Tijuana and Ciudad Juarez, so they may not be representative of less stable or more mobile couples. Third, the recruitment of male partners through the FSWs may have introduced self-selection bias. FSWs who were concerned about IPV or negative reactions from their male partners may have opted out of the study, and couples reporting extreme levels of IPV during the screening process were not eligible for this study, thus biasing the sample in favor of relationships that were less prone to violence or conflict. However, we decided it was more important to maintain the safety of the participants, and place the decision on whether to recruit male partners under the women’s control. Nonetheless, this possible bias should be taken into account when interpreting the results. Fourth, it is possible that men were less likely to report IPV perpetration because of social desirability. However, there was not a significant statistical difference between FSWs and their male partners in regards to self -reported IPV perpetration. FSWs did report significantly more IPV behaviors than partners, albeit a small difference: 1.3 vs. 1.1, respectively. Lastly, FSWs’ and male partners’ responses to the IPV questions were higher correlated compared to their reports of unprotected sex. However, FSWs’ and male partners’ reports of condom use with each other were still significantly correlated at a moderate level (.33). This was likely due to the different ways in which IPV and unprotected sex were measured. Each member of the couple was asked whether or not a specific IPV event happened in the past year, with the response choices being either “yes” or “no.” Whereas, condom use was assessed by first asking each member of the couple (separately) how often they had vaginal and anal sex in the past month, and then how many of these times they used condoms. This more open-ended question could produce a wider range of possible answered compared to “yes” or “no” responses. We do not think this changes the validity or conclusions of study, but it is something to note. Accurate reporting of condom use is an issue in condom use research in general, with researchers having to rely solely on self-report.
CONCLUSIONS
The results suggest that increasing relationship power among FSWs who use drugs alone is not likely to result in increased condom use with their non-commercial steady partners. Future intervention research should examine whether couples’ attitudes about condom use change over time while addressing both sexual relationship power and IPV. Additional research is needed regarding issues of trust, intimacy, having sex while under the influence of drugs, and motivations to use condoms among couples. It is also important for future HIV prevention research with couples to address mental health issues such as depression symptoms and economic stability.
ACKNOWLEDGMENTS
The authors respectfully acknowledge the participation of all the men and women in this study who shared their stories with us. Without them this work would not be possible. We also thank the U.S.-Mexico bi-national investigators and staff. Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under awards number K01 DA026307, and R01 DA027772.
REFERENCES
- 1.Beittel JS. Mexico’s Drug Trafficking Organizations: Source and Scope of the Rising Violence. In: Service CR, editor. Diane Publishing Co.; Darby, PA: 2011. [Google Scholar]
- 2.Bucardo J, Semple SJ, Fraga-Vallejo M, Davila W, Patterson TL. A qualitative exploration of female sex work in Tijuana, Mexico. Arch Sex Behav. 2004;33(4):343–51. doi: 10.1023/B:ASEB.0000028887.96873.f3. 2004/08// [DOI] [PubMed] [Google Scholar]
- 3.CENSIDA Casos de SIDA en Mexico [AIDS cases in Mexico] 2009 http://www.censida.salud.gob.mx/interior/cifras.html [cited 2009 October 30]; Available from:
- 4.Strathdee SA, Philbin MM, Semple SJ, Pu M, Orozovich P, Martinez G, et al. Correlates of injection drug use among female sex workers in two Mexico-U.S. border cities. Drug And Alcohol Dependence. 2008;92(1-3):132–40. doi: 10.1016/j.drugalcdep.2007.07.001. 2008/01/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ulibarri MD, Strathdee SA, Patterson TL. Sexual and drug use behaviors associated with HIV and other sexually transmitted infections among female sex workers in the Mexico-US border region. Current Opinion in Psychiatry. 2010;23(3):215–20. doi: 10.1097/YCO.0b013e32833864d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iñiguez-Stevens E, Brouwer KC, Hogg RS, Patterson TL, Lozada R, Magis-Rodríguez C, et al. [Estimating the 2006 prevalence of HIV by gender and risk groups in Tijuana, Mexico] Gaceta Médica De México. 2009;145(3):189–95. [PMC free article] [PubMed] [Google Scholar]
- 7.Patterson TL, Mausbach B, Lozada R, Staines-Orozco H, Semple SJ, Fraga-Vallejo M, et al. Efficacy of a brief behavioral intervention to promote condom use among female sex workers in Tijuana and Ciudad Juarez, Mexico. American Journal Of Public Health. 2008;98(11):2051–7. doi: 10.2105/AJPH.2007.130096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ulibarri MD, Strathdee SA, Lozada R, Staines-Orozco HS, Abramovitz D, Semple S, et al. Condom use among female sex workers and their non-commercial partners: effects of a sexual risk intervention in two Mexican cities. International Journal Of STD & AIDS. 2012 Apr;23(4):229–34. doi: 10.1258/ijsa.2011.011184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strathdee SA, Lozada R, Staines-Orozco H, Abramovitz D, Semple S, Martinez G, et al. No Effect of a Sexual Risk Intervention on Condom Use with Female Sex Workers and their Regular Partners in Two Mexico-US Border Cities International Harm Reduction Association’s 20th International Conference; Bangkok, Thailand2009. April, 2009. [Google Scholar]
- 10.Patterson TL, Goldenberg S, Gallardo M, Lozada R, Semple SJ, Orozovich P, et al. Correlates of HIV, STIs and associated high risk behaviors among male clients of female sex workers in Tijuana, Mexico. AIDS. 2009;23(13):1765–71. doi: 10.1097/QAD.0b013e32832f08a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Connell RW. Gender and power: Society, the person and sexual politics. Stanford University Press; 1987. [Google Scholar]
- 12.Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior: The Official Publication Of The Society For Public Health Education. 2000;27(5):539–65. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez-Guarda RM, Florom-Smith AL, Thomas T. A syndemic model of substance abuse, intimate partner violence, HIV infection, and mental health among Hispanics. Public Health Nurs. 2011 Jul-Aug;28(4):366–78. doi: 10.1111/j.1525-1446.2010.00928.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gonzalez-Guarda RM, McCabe BE, Florom-Smith A, Cianelli R, Peragallo N. Substance abuse, violence, HIV, and depression: an underlying syndemic factor among Latinas. Nurs Res. 2011 May-Jun;60(3):182–9. doi: 10.1097/NNR.0b013e318216d5f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer M. AIDS and the health crisis of the U.S. urban poor: The perspective of critical medical anthropology. Social Science & Medicine. 1994;39(7):931–48. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- 16.Singer M. A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;24(2):99–110. [Google Scholar]
- 17.Aspy CB, Lippincott JA, Lippincott RB. Special populations in college counseling: A handbook for mental health professionals. American Counseling Association; Alexandria, VA US: 2007. When Dating Relationships Go Bad: Counseling Students Involved in Relationship Violence; pp. 117–28. [Google Scholar]
- 18.Gonzalez-Guarda RM, Peragallo N, Urrutia MT, Vasquez EP, Mitrani VB. HIV risks, substance abuse, and intimate partner violence among Hispanic women and their intimate partners. The Journal Of The Association Of Nurses In AIDS Care: JANAC. 2008;19(4):252–66. doi: 10.1016/j.jana.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Silverman JG, Decker MR, Saggurti N, Balaiah D, Raj A. Intimate partner violence and HIV infection among married Indian women. JAMA: The Journal Of The American Medical Association. 2008;300(6):703–10. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- 20.Sormanti M, Shibusawa T. Intimate partner violence among midlife and older women: a descriptive analysis of women seeking medical services. Health Soc Work. 2008;33(1):33–41. doi: 10.1093/hsw/33.1.33. 2008/02// [DOI] [PubMed] [Google Scholar]
- 21.El-Bassel N, Witte SS, Wada T, Gilbert L, Wallace J. Correlates of partner violence among female street-based sex workers: Substance abuse, history of childhood abuse, and HIV risks. AIDS Patient Care and STDs. 2001;15(1):41–51. doi: 10.1089/108729101460092. 2001/01// [DOI] [PubMed] [Google Scholar]
- 22.Sanders T. Female street workers, sexual violence, and protection strategies. Journal of Sexual Aggression. 2001;7(1):5–18. 2001/// [Google Scholar]
- 23.Shannon K, Kerr T, Bright V, Gibson K, Tyndall MW. Drug sharing with clients as a risk marker for increased violence and sexual and drug-related harms among survival sex workers. AIDS Care. 2008;20(2):228–34. doi: 10.1080/09540120701561270. 2008/02// [DOI] [PubMed] [Google Scholar]
- 24.Surratt HL, Inciardi JA, Kurtz SP, Kiley MC. Sex Work and Drug Use in a Subculture of Violence. Crime & Delinquency. 2004;50(1):43–59. 2004/01// [Google Scholar]
- 25.Wechsberg WM, Luseno WK, Lam WK. Violence against substance-abusing South African sex workers: Intersection with culture and HIV risk. AIDS Care. 2005;17:S55–S64. doi: 10.1080/09540120500120419. 2005/// [DOI] [PubMed] [Google Scholar]
- 26.Ulibarri MD, Strathdee SA, Lozada R, Magis-Rodriguez C, Amaro H, O’Campo P, et al. Intimate partner violence among female sex workers in two Mexico–U.S. Border cities: Partner characteristics and HIV risk behaviors as correlates of abuse. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(4):318–25. doi: 10.1037/a0017500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rey GN, García FJ, Icaza MEM-M, Sainz MT. La depresión y su relación con la violencia de pareja y el consumo de alcohol en mujeres Mexicanas. Revista Mexicana de Psicología. 2007;24(2):165–73. [Google Scholar]
- 28.Valdez-Santiago R, Híjar M, Martínez RR, Burgos LÁ, de la Luz Arenas Monreal M. Prevalence and severity of intimate partner violence in women living in eight indigenous regions of Mexico. Social Science & Medicine. 2013;82:51–7. doi: 10.1016/j.socscimed.2013.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Castro R, Casique I, Brindis CD. Empowerment and physical violence throughout women’s reproductive life in Mexico. Violence Against Women. 2008;14(6):655–77. doi: 10.1177/1077801208319102. [DOI] [PubMed] [Google Scholar]
- 30.Villarreal A. Women’s employment status, coercive control, and intimate partner violence in Mexico. Journal of Marriage and Family. 2007;69(2):418–34. [Google Scholar]
- 31.Babcock JC, Waltz J, Jacobson NS, Gottman JM. Power and violence: The relation between communication patterns, power discrepancies, and domestic violence. J Consult Clin Psychol. 1993;61(1):40–50. doi: 10.1037//0022-006x.61.1.40. [DOI] [PubMed] [Google Scholar]
- 32.Pulerwitz J, Gortmaker SL, DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42(7):637–60. 2000/04// [Google Scholar]
- 33.Chukakov B, Ilan K, Belmaker RH, Cwikel J. The motivation and mental health of sex workers. Journal Of Sex & Marital Therapy. 2002;28(4):305–16. doi: 10.1080/00926230290001439. [DOI] [PubMed] [Google Scholar]
- 34.Hong Y, Zhang C, Li X, Liu W, Zhou Y. Partner Violence and Psychosocial Distress among Female Sex Workers in China. Plos One. 2013;8(4):e62290–e. doi: 10.1371/journal.pone.0062290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lau JTF, Tsui HY, Ho SPY, Wong E, Yang X. Prevalence of psychological problems and relationships with condom use and HIV prevention behaviors among Chinese female sex workers in Hong Kong. AIDS Care. 2010;22(6):659–68. doi: 10.1080/09540120903431314. [DOI] [PubMed] [Google Scholar]
- 36.Surratt HL, Kurtz SP, Chen M, Mooss A. HIV risk among female sex workers in Miami: The impact of violent victimization and untreated mental illness. AIDS Care. 2012;24(5):553–61. doi: 10.1080/09540121.2011.630342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Witte SS, Batsukh A, Chang M. Sexual risk behaviors, alcohol abuse, and intimate partner violence among sex workers in Mongolia: Implications for HIV prevention intervention development. Journal Of Prevention & Intervention In The Community. 2010;38(2):89–103. doi: 10.1080/10852351003640625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ulibarri MD, Semple SJ, Rao S, Strathdee SA, Fraga-Vallejo MA, Bucardo J, et al. History of abuse and psychological distress symptoms among female sex workers in two Mexico-U.S. border cities. Violence Vict. 2009;24(3) doi: 10.1891/0886-6708.24.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farley M, Baral I, Kiremire M, Sezgin U. Prostitution in five countries: Violence and post-traumatic stress disorder. Feminism & Psychology. 1998;8(4):405–26. [Google Scholar]
- 40.Hong Y, Li X. Behavioral studies of female sex workers in China: A literature review and recommendation for future research. AIDS And Behavior. 2008;12(4):623–36. doi: 10.1007/s10461-007-9287-7. [DOI] [PubMed] [Google Scholar]
- 41.Ulibarri MD, Hiller SP, Lozada R, Rangel MG, Stockman JK, Silverman JG, et al. Prevalence and Characteristics of Abuse Experiences and Depression Symptoms among Injection Drug-Using Female Sex Workers in Mexico. Journal of Environmental and Public Health. 2013;2013:11. doi: 10.1155/2013/631479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. Guilford Press; New York, NY US: 2006. [Google Scholar]
- 43.Amaro H, Larson MJ, Zhang A, Acevedo A, Dai J, Matsumoto A. Effects of trauma intervention on HIV sexual risk behaviors among women with co-occurring disorders in substance abuse treatment. Journal of Community Psychology. 2007;35(7):895–908. [Google Scholar]
- 44.Syvertsen JL, Roberston AM, Abramovitz D, Martinez G, Patterson TL, Ulibarri MD, et al. Study protocol for the recruitment of female sex workers and their non-commercial partners into couple-based HIV research. BMC Public Health. 2012;12(1):136. doi: 10.1186/1471-2458-12-136. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Questionnaire Development System. NOVA Research Company; Bethesda, MD: 2010. [Google Scholar]
- 46.Straus MA, Douglas EM. A short form of the Revised Conflict Tactics Scales, and typologies for severity and mutuality. Violence Vict. 2004;19(5):507–20. doi: 10.1891/vivi.19.5.507.63686. 2004/10// [DOI] [PubMed] [Google Scholar]
- 47.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994 Mar-Apr;10(2):77–84. [PubMed] [Google Scholar]
- 48.Grzywacz JG, Hovey JD, Seligman LD, Arcury TA, Quandt SA. Evaluating Short-Form Versions of the CES-D for Measuring Depressive Symptoms Among Immigrants From Mexico. Hisp J Behav Sci. 2006;28(3):404–24. [PMC free article] [PubMed] [Google Scholar]
- 49.Muthén LK, Muthén BO. Mplus User’s Guide. Sixth Edition Muthén & Muthén; Los Angeles, CA: 1998-2011. [Google Scholar]
- 50.Campbell AN, Tross S, Dworkin SL, Hu MC, Manuel J, Pavlicova M, et al. Relationship power and sexual risk among women in community-based substance abuse treatment. Journal Of Urban Health: Bulletin Of The New York Academy Of Medicine. 2009 Nov;86(6):951–64. doi: 10.1007/s11524-009-9405-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Campbell AN, Tross S, Hu MC, Pavlicova M, Nunes EV. Predictors of relationship power among drug-involved women. AIDS And Behavior. 2012 Aug;16(6):1532–41. doi: 10.1007/s10461-012-0208-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Murray L, Moreno L, Rosario S, Ellen J, Sweat M, Kerrigan D. The role of relationship intimacy in consistent condom use among female sex workers and their regular paying partners in the Dominican Republic. AIDS And Behavior. 2007;11(3):463–70. doi: 10.1007/s10461-006-9184-5. [DOI] [PubMed] [Google Scholar]
- 53.Castañeda X, Ortíz V, Allen B, García C, Hernandez-Avila M. Sex masks: The double life of female commercial sex workers in Mexico City. Culture, Medicine and Psychiatry. 1996;20(2):229–47. doi: 10.1007/BF00115863. [DOI] [PubMed] [Google Scholar]
- 54.Castro FG, Hernandez NT. A cultural perspective on prevention interventions. In: Velasquez RJ, Arellano LM, McNeill BW, editors. The Handbook of Chicana/o Psychology and Mental Health. Lawrence Erlbaum Associates; Mahwah, New Jersey: 2004. pp. 371–97. [Google Scholar]
- 55.Barrington C, Fleming P, Moya M, Perez M, Donastorg Y, Broxton C, et al. Emotional men and pragmatic women?: Relationship and gender dynamics between female sex workers and their regular partners in the Dominican Republic; XVIII International AIDS Conference; Washinton, D.C.2012. July 2012. [Google Scholar]
- 56.Duke MR, Cunradi CB. Measuring intimate partner violence among male and female farmworkers in San Diego County, Ca. Cultural Diversity and Ethnic Minority Psychology. 2011;17(1):59–67. doi: 10.1037/a0021826. [DOI] [PubMed] [Google Scholar]
- 57.Kalokhe AS, Paranjape A, Bell CE, Cardenas GA, Kuper T, Metsch LR, et al. Intimate partner violence among HIV-infected crack cocaine users. AIDS Patient Care and STDs. 2012;26(4):234–40. doi: 10.1089/apc.2011.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Frye V, Latka MH, Wu Y, Valverde EE, Knowlton AR, Knight KR, et al. Intimate partner violence perpetration against main female partners among HIV-positive male injection drug users. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007;46(2):S101–s9. doi: 10.1097/QAI.0b013e31815767e6. [DOI] [PubMed] [Google Scholar]
- 59.Kramer TL, Borders TF, Tripathi S, Lynch C, Leukefeld C, Falck RS, et al. Physical victimization of rural methamphetamine and cocaine users. Violence Vict. 2012;27(1):109–24. doi: 10.1891/0886-6708.27.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gonzalez-Guarda RM, De Santis JP, Vasquez EP. Sexual orientation and demographic, cultural, and psychological factors associated with the perpetration and victimization of intimate partner violence among Hispanic men. Issues in Mental Health Nursing. 2013;34(2):103–9. doi: 10.3109/01612840.2012.728280. [DOI] [PMC free article] [PubMed] [Google Scholar]