Abstract
Objective
Patient-centredness has become an important aspect of health service delivery; however, there are a limited number of studies that focus on this concept in the domain of hearing healthcare. The objective of this study was to examine and compare audiologists’ preferences for patient-centredness in Portugal, India and Iran.
Design
The study used a cross-sectional survey design with audiologists recruited from three different countries.
Participants
A total of 191 fully-completed responses were included in the analysis (55 from Portugal, 78 from India and 58 from Iran).
Main outcome measure
The Patient–Practitioner Orientation Scale (PPOS).
Results
PPOS mean scores suggest that audiologists have a preference for patient-centredness (ie, mean of 3.6 in a 5-point scale). However, marked differences were observed between specific PPOS items suggesting these preferences vary across clinical situations. A significant level of difference (p<0.001) was found between audiologists’ preferences for patient-centredness in three countries. Audiologists in Portugal had a greater preference for patient-centredness when compared to audiologists in India and Iran, although no significant differences were found in terms of age and duration of experience among these sample populations.
Conclusions
There are differences and similarities in audiologists’ preferences for patient-centredness among countries. These findings may have implications for the training of professionals and also for clinical practice in terms of optimising hearing healthcare across countries.
Keywords: International health services < HEALTH SERVICES ADMINISTRATION & MANAGEMENT, MEDICAL EDUCATION & TRAINING
Strengths and limitations of this study.
A response rate of 76% was obtained for this questionnaire-based study and there was diversity in the data from audiologists distributed across three countries.
Some variables such as differing healthcare delivery models and educational systems were not controlled for, and may have contributed to the differences and similarities noticed in audiologists preferences.
A sampling bias may have been present, since audiologists with particular preferences may have been more inclined to respond to the questionnaire.
The fact that identifiable information may have been present in the emailed responses had the potential to influence/discourage an individual's response.
Introduction
There has been an increase in advocacy towards patients’ involvement in their health and care delivery, hence the concept ‘patient-centredness’ has received much attention over the past few decades.1 Patient-centeredness involves aspects such as increased importance placed on patient participation, self-determination of patients in their healthcare (ie, the rights and abilities of patients to make their own choices and decisions about the medical care they receive) and the creation of a power-balanced therapeutic relationship between patients and professionals.2 Although there has been little consensus over the meaning of this concept universally, patient-centredness has been described in the field of general practice with five main dimensions: (1) biopsychosocial perspective; (2) patient as a person; (3) shared knowledge and power; (4) therapeutic alliance; and (5) clinician as a person.1 Patient-centeredness has been suggested to be a fundamental part of the successful management of chronic health conditions.3
Studies from a variety of areas of healthcare (including oncology, skin disorders, amyotrophic lateral sclerosis) have suggested that the health professional's preferences towards patient-centeredness is important in determining outcomes, including patient satisfaction.4–7 A shortfall in patient-centredness has also been linked to malpractice claims,8 and in general a measured preference for patient-centeredness correlates well with clinical practices such as open communication and a positive rapport between patient and clinician.9
The profession of Audiology is particularly interesting in this context since, traditionally, there has been a focus on the technological aspects of hearing healthcare.10 Some researchers believe that the past two decades has seen a paradigm shift, moving from a focus on the technological aspects of hearing healthcare to a more person-centred approach to rehabilitation.10 11 The empirical evidence for this shift is limited, with only a small number of published studies on patient-centredness specific to audiology: Grenness et al12 studied the views of older adults who own hearing aids in order to further define patient-centred care in the context of audiological rehabilitation. Interviews were conducted with 10 older adults with hearing aids, exploring their views and the data were analysed using qualitative content analysis. The results suggested three dimensions: (1) the therapeutic relationship; (2) the players—patient and audiologist; and (3) the clinical process, and an overarching theme of individualised care specific to audiological rehabilitation.
A recent study focusing specifically on audiologists in Australia found that they report a high preference for patient-centredness.13 Moreover, demographic factors such as age, duration of work experience and employment type (ie, public/private) acted as influencing factors towards explaining patient-centredness. For example, older audiologists and those who had practiced longer had a significantly greater preference for patient-centredness when compared to younger and less-experienced audiologists. This is the only published study that has explicitly explored audiologists’ preferences towards patient-centredness.
Two further studies have been conducted in the field of Audiology, which, while not explicitly focusing on patient centredness as a distinct entity, are highly relevant: Laplante-Lévesque et al14 conducted a qualitative study exploring shared decision-making in adults with acquired hearing impairment, which suggested that patients wanted rehabilitative audiologists to hear their experiences and preferences and to tailor their interventions accordingly. Poost-Foroosh et al15 studied the factors in the interaction between audiologists and clients in the decision to purchase a hearing aid. The study asked 12 clients with acquired hearing loss and 10 audiologists, from University as well as private practices, to supply statements regarding which clinician–patient factors they felt influenced the decision to purchase a hearing aid. Client-centred interaction was identified as one of two major themes in the responses provided (client-empowerment was the other).
In all cases, the research discussed above consistently demonstrates the significant value that patients place in their relationship with the clinician. Across the studies it can be seen that different clinician-specific factors were found to influence the degree of patient-centredness. As of yet there is little strong evidence for improved rehabilitation outcomes, although hearing aid purchase was observed to be positively influenced by more client-centred practice. The reader is referred to a recent literature review by Grenness et al2 for further details on patient-centred care in relation to rehabilitative audiology.
Given the clinician-specific differences observed in the studies discussed above, and the fact that audiology practices vary considerably across countries,16 it would be useful to examine audiologists’ preferences for patient-centredness across different countries, which vary in terms of culture and healthcare systems. Moreover, it has been highlighted in general that there are few cross-cultural studies in the area of hearing healthcare, highlighting the need for such studies.17
Cultural competence is a key aspect that is known to influence healthcare quality.17 18 We hypothesise that the present culture to which an individual is exposed, as well as their cultural background, can influence patients’ as well as providers’ preferences in healthcare and towards patient-centredness. We were particularly interested in understanding and comparing the preferences for patient-centredness among audiologists in European and Asian countries. Asian countries, compared to European countries, are considered to be more collectivist societies, with a greater emphasis placed on the role of the individual as part of a local group and/or community with less of a tendency to focus on ‘looking after oneself’.19 Further to this, it has been posited that Asian countries have a tendency towards a high ‘power distance’ within levels of organisations—this reflects how willing the less powerful members of an organisation or group are to accept an unequal distribution of power.19 In the context of patient-centredness, such cultural effects might result in different opinions towards a hierarchical ‘paternalistic’ approach to audiological management (where the clinician may display an attitude of superiority over the patient), versus a patient centred-approach.
The aim of the current study was to examine and compare audiologists’ preferences for patient-centredness in Portugal, India and Iran. These countries vary in terms of healthcare system, culture and socioeconomic status. However, they were chosen as they all have a minimum educational level requirement of a Bachelor's degree education for audiologists, and also due to convenience in data collection.
Method
Ethical considerations
Ethical approval was obtained from the School of Allied Health Sciences, Polytechnic Institute of Porto at Porto and All India Institute of Speech and Hearing at Mysore for data collection in Portugal and India, respectively. This type of study did not require ethical approval under the Department of Audiology, University of Social Welfare and Rehabilitation Sciences at Tehran for data collection in Iran.
Study design and participants
The current study used a cross-sectional survey design and purposive sampling to recruit participants. The email mailing list was obtained from university and professional associations and consisted of audiologists distributed throughout each of the three countries. The Patient–Practitioner Orientation Scale (PPOS) questionnaires, with some additional demographics questions (ie, age, gender, number of years of experience, work set-up, country of origin and country in which currently practicing), were sent to 260 audiologists (80 in Portugal, 110 in India and 70 in Iran) via email, with a request for them to complete and return the questionnaires to the researcher by email. Two email reminders were sent for non-respondents after 2 and 4 weeks, respectively. As the email ID might have contained some information that may have helped identify the individual, the survey was not fully anonymous. In the interest of keeping the survey short, only limited demographic information was requested and the choice was made to consider the most important aspects based on the findings of the previous studies,12–14 as discussed in the introduction.
Questionnaire
The PPOS was developed by Krupat et al20 to study physician preferences towards patient-centredness. However, a modified version of the PPOS that has previously been used to study audiologists’ preferences towards patient-centredness was used in the current study.13 This modified version of the PPOS was found to have acceptable internal consistency (α=0.78). This scale has 18 questions which are scored on a 6-point Likert scale (1=strongly agree; 6=strongly disagree). The total score ranges from 18 (most audiologist-centred) to 108 (most patient-centred), and there are two subscales: The first nine-item subscale, sharing, reflects the extent to which the respondent believes that patients desire information and should be part of the decision-making process (eg, patients should be treated as if they were partners with the audiologists, equal in power and status). The other nine-item subscale, caring, reflects the extent to which the respondent sees the patient's expectations, feelings, and life circumstances as critical elements in the treatment process (eg, a treatment plan cannot succeed if it is in conflict with a patient's lifestyle or values).
An English version of the questionnaire was administered in India. Portuguese and Farsi translated versions were used in Portugal and Iran, respectively. The questionnaire translation process was aimed at achieving different language versions of the English instrument that are conceptually equivalent in each of the target countries/cultures. That is, the focus was on cross-cultural and conceptual, rather than on linguistic/literal equivalence. We followed the well accepted forward-translations and back-translations method.21 This process involved four main stages: forward translation; expert back translation; review and resolution of any discrepancies; and pretesting with five participants each, in Portugal as well as in Iran.
Data analysis
In the first instance, descriptive statistics (ie, mean, SD), a test of normality and a test of homogeneity of variance were performed. Mean total PPOS scores for audiologists from three countries were compared using an independent one-way analysis of variance (ANOVA). An α level of 0.01 was used to determine significance. Bonferroni post hoc analysis was performed to further examine the relationship between groups. Further, a one-way analysis of covariance (ANCOVA) was performed with age and duration of work experience as covariates in order to exclude the influence of these variables on the observed differences between the group means.
Results
A total of 198 responses (response rate of 76%) were received. This included: 55 responses from Portugal (response rate of 69%); 82 responses from India (response rate of 75%); and 61 responses from Iran (response rate of 87%). However, three responses from Iran (incomplete data) and four responses from India (audiologists currently practicing in a different country) were excluded. A total of 191 responses (ie, 73%) were included in the analysis (55 from Portugal, 78 from India and 58 from Iran). Table 1 presents the demographic information and table 2 presents PPOS scores. ANOVA showed no difference between groups in terms of age (F (2, 188)=2.13, p=0.121) or in terms of duration of work experience (F (2, 188)=1.16, p=0.313).
Table 1.
Demographic information
| All participants (n=191) | Portugal (n=55) | India (n=78) | Iran (n=58) | |
|---|---|---|---|---|
| Age in years (mean±SD) | 30.9±8.4 | 31.0±8.4 | 29.6±8.6 | 32.5±8.0 |
| Gender (%) | ||||
| Male | 37 | 20 | 55 | 30 |
| Female | 63 | 80 | 45 | 70 |
| Work set-up (%) | ||||
| Clinic public | 35 | 23 | 39 | 41 |
| Clinic private | 50 | 51 | 61 | 33 |
| Clinic both | 12 | 15 | 0 | 26 |
| Education | 1 | 2 | 0 | 0 |
| Not known | 2 | 9 | 0 | 0 |
| Education (%) | ||||
| Bachelors | 47 | 72 | 18 | 60 |
| Masters | 48 | 22 | 74 | 40 |
| Doctorate | 5 | 6 | 8 | 0 |
| Work experience in years (mean±SD) | 7.2±8.1 | 7.8±8.2 | 6.1±8.8 | 8.1±6.5 |
Table 2.
Modified Patient–Practitioner orientation scale (PPOS): Mean scores and SD
| All participants (n=191) | Portugal (n=55) | India (n=78) | Iran (n=58) | |
|---|---|---|---|---|
| PPOS Items (Mean±SD) | ||||
| 1. The audiologist is the one who should decide what gets discussed during an appointment | 2.4±1.1 | 2.4±1.2 | 2.3±1.2 | 2.5±1.2 |
| 2. Although healthcare is less personal these days, this is a small price to pay for audiological advances | 3.0±1.4 | 4.3±1.2 | 2.7±1.2 | 2.1±1.0 |
| 3. The most important part of the standard audiological appointment is the hearing test | 2.7±1.4 | 3.4±1.2 | 2.5±1.5 | 2.3±1.1 |
| 4. It is often best for clients if they do not have the full explanation of their audiological condition | 4.6±1.3 | 5.0±1.0 | 4.5±1.5 | 4.2±1.3 |
| 5. Clients should rely on their audiologist’s knowledge and not try to find out about their conditions on their own | 3.2±1.7 | 4.2±1.4 | 3.4±1.6 | 2.0±1.3 |
| 6. When audiologists ask a lot of questions about a client's background, they are prying too much into personal matters | 4.4±1.3 | 5.0±1.0 | 4.0±1.3 | 4.2±1.4 |
| 7. If audiologists are truly good at diagnosis and treatment, the way they relate to clients is not that important | 4.8±1.2 | 5.5±0.7 | 4.4±1.3 | 4.6±1.2 |
| 8. Many clients continue asking questions even though they are not learning anything new | 3.2±1.2 | 3.4±1.2 | 3.2±1.2 | 3.0±1.2 |
| 9. Clients should be treated as if they were partners with the audiologist, equal in power and status* | 4.1±1.6 | 4.7±1.6 | 3.7±1.5 | 4.0±1.5 |
| 10. Clients generally want reassurance rather than information about their audiological condition | 2.8±1.1 | 3.3±1.0 | 2.7±1.1 | 2.5±1.1 |
| 11. If an audiologist's primary tools are being open and warm, the audiologist will not have a lot of success | 4.3±1.4 | 4.6±1.1 | 3.8±1.4 | 4.6±1.3 |
| 12. When clients disagree with their audiologist, this is a sign that the audiologist does not have the client's respect and trust | 3.8±1.2 | 4.6±1.0 | 3.7±1.1 | 3.1±1.2 |
| 13. A management plan cannot succeed if it is in conflict with a client's lifestyle or values* | 4.7±1.1 | 4.7±1.1 | 4.6±1.0 | 4.7±1.2 |
| 14. Most clients want to get in and out of the audiologist's office as quickly as possible | 3.5±1.4 | 4.4±1.2 | 3.3±1.2 | 2.9±1.3 |
| 15. The client must always be aware that the audiologist is in charge | 2.6±1.3 | 2.7±1.2 | 2.4±1.1 | 2.9±1.5 |
| 16. It is not that important to know a client's culture and background in order to treat the client's audiological condition | 4.6±1.3 | 5.3±0.9 | 4.3±1.4 | 4.6±1.2 |
| 17. Humour is a major ingredient in the audiologist's management of the client* | 4.1±1.3 | 4.8±1.0 | 3.8±1.3 | 3.8±1.4 |
| 18. When clients look up audiological information on their own, this usually confuses more than it helps | 2.9±1.3 | 2.6±1.0 | 2.8±1.4 | 3.4±1.3 |
| PPOS scales (mean±SD) | ||||
| Full scale | 3.6±0.6 | 4.2±0.5 | 3.5±0.6 | 3.4±0.4 |
| Sharing subscale | 3.6±0.7 | 4.2±0.6 | 3.4±0.7 | 3.2±0.5 |
| Caring subscale | 3.7±0.6 | 4.1±0.5 | 3.5±0.5 | 3.6±0.5 |
Score of 1 (strongly agree), most clinician-centred; Score of 6 (strongly disagree), most patient-centred. Items 9, 13 and 17 (*) are reversely worded items which were reverse scored.
PPOS,
Data for full-scale as well as subscales were found to be normally distributed (based on Kolmogorov-Smirnov test and visual examination of histograms). Homogeneity of variances (based on Levene's test) was found for caring and total mean (p=0.625 and 0.129, respectively) and not for sharing (p=0.020). Since our data were found to be normally distributed, we elected to use ANOVA for our analysis, despite the fact that homogeneity of variances could not be assumed for the sharing subscale. A robust procedures (Welch and Brown-Forsythe) test was performed to check ANOVA findings, which indicated the same significant differences between group means (p<0.001 in all cases).
The PPOS mean scores from each population were analysed using a one way between-subjects ANOVA (see table 3). A significant result was found for sharing subscale (F (2, 188)=39.76), caring subscale (F (2, 188)=24.61) and the full scale (F (2, 188)=42.49). Further, post hoc tests with Bonferroni correction showed that the difference between Portugal and India and also Portugal and Iran were significant for sharing subscale, caring subscale and full scale (p=0.001, 0.001 and 0.001, respectively). However, the difference between India and Iran was not statistically significant for the sharing subscale, caring subscale and full scale (p=0.171, p=0.841 and p=1, respectively).
Table 3.
Differences in audiologists’ preferences for patient-centredness between countries
| Degree of freedom | F-test | p Value | |
|---|---|---|---|
| Sharing | 2 | 39.76 | <0.001 |
| Caring | 2 | 24.61 | <0.001 |
| Full scale | 2 | 42.49 | <0.001 |
These results show some differences and some similarities in audiologists’ preferences towards patient-centredness from different countries (see figure 1). Audiologists in Portugal had significantly greater preference for patient-centredness when compared to audiologists in India and Iran whose preferences did not differ much.
Figure 1.
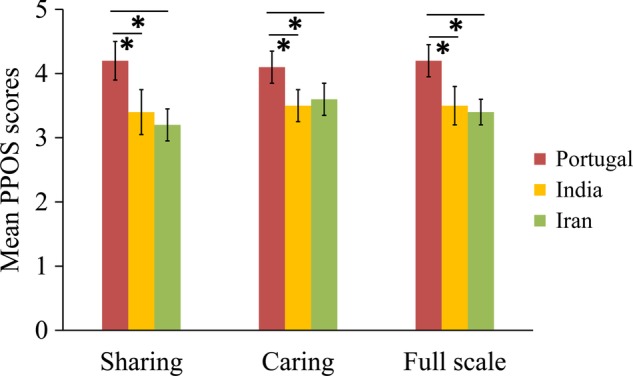
Bar Graphs showing the mean total PPOS Score (‘Full Scale’), and the mean PPOS Score for the ‘Sharing’ and ‘Caring’ Subscales for audiologists from Portugal, India and Iran. (*) indicates a significant difference (p<0.01).
While our sample populations were well matched, with no significant differences with respect to age and experience, this does not exclude some possible influence of these variables on the data. Therefore, we elected to include these variables as covariates, and assess if this had an influence on the main effect observed: The data met the necessary assumptions (ie, linearity, homoscedasticity and homogeneity of regression slopes), and the ANCOVA results with age and duration of work experience as covariates and PPOS scores as dependent variable gave results consistent with the ANOVA, with a significant main effect for the full scale and subscales only, and no significant interaction was observed. Thus we conclude that differences exist between the responses from audiologists from these countries in preference for patient-centredness, even after accounting for age and duration of work experience.
Discussion
This study examined and compared audiologists’ preferences for patient-centredness in Portugal, India and Iran. The PPOS scores indicate the self-reported preference for patient-centredness. An overall mean score per item of greater than three for all three countries included suggests that there is a tendency for audiologists to favour patient-centredness, rather than a clinician-centred approach. This is true for caring as well as sharing subscales. These values can be compared to those observed across other medical specialities.5 For example, general practitioners and oncology physicians had higher PPOS mean scores (ie, 4.3 and 5.0, respectively) when compared with physicians with a surgical background (ie, 2.9). Thus, in general, it appears that patient-centred practices vary depending on the specific duties of the professional. We hypothesise that this could be linked to differences in training routes for medical subspecialties, in combination with the expectation of the role fulfilled by the clinician within their specialty. This is of relevance to audiology, since training routes vary between countries, with education provision that may follow either a medical, scientific, technician, paramedical model or a combination thereof.22
From examination of the responses to each item it can be seen that audiologists’ preferences for patient-centredness vary depending on the situation described (see table 2). For example, item 1 (ie, the audiologist is the one who should decide what gets discussed during an appointment), item 2 (ie, the most important part of the standard audiological appointment is the hearing test), item 10 (ie, clients generally want reassurance rather than information about their audiological condition) and item 15 (ie, the client must always be aware that the audiologist is in charge) show markedly lower mean scores (2.4–2.8) than the mean PPOS scores (4.6–4.8) in item 4 (ie, it is often best for clients if they do not have the full explanation of their audiological condition), item 7 (ie, if audiologists are truly good at diagnosis and treatment, the way they relate to clients is not that important) and item 13 (ie, a management plan cannot succeed if it is in conflict with a client's lifestyle or values). The content of the items showing a lower mean score are consistent with traditional audiological practices focusing on application of diagnostic testing, diagnosis and treatment, whereas the other items with higher mean scores are more explicit on their focus towards rehabilitation (using terms such as ‘management plans’ and words such as ‘relate’). Similar patterns of PPOS results have been reported in a recent Australian study.13 Thus it appears that an audiologist's views towards patient-centredness vary depending on whether they are considering their diagnostic or rehabilitative roles, and this is shared across countries. Some researchers suggest that there is a growing trend towards a greater role of client-centred rehabilitation by audiologists.10 11 Therefore, it may be useful to monitor audiologists’ preferences for patient-centredness over time.
The study results suggest some country-specific differences and some similarities in the overall preference for patient-centredness among audiologists from Portugal (M=4.2; SD=0.5), India (M=3.5; SD=0.6) and Iran (M=3.4; SD=0.4). Generally, audiologists in Portugal had a high preference for patient-centredness, when compared to audiologists in India and Iran. Moreover, a recent study found that Australian audiologists14 have high preference for patient-centredness (M=4.46; SD=0.52), which is similar to Portugal audiologists’ preferences reported in the current study. As discussed later, there are a number of possible factors that may affect audiologists’ preferences for patient-centredness, and it is likely that a number of these factors are more similar between Portugal and Australia than Portugal and India, or Portugal and Iran.
When comparing scores across countries, the trend for higher PPOS scores provided by audiologists from Portugal compared to their peers from India and Iran was true for almost all questionnaire items when analysed individually. However, some variations exist. For example, scores for item 1 (ie, the audiologist is the one who should decide what gets discussed during an appointment), was similar among audiologists in all three countries. This might reflect a similarity in service delivery that places restricted time allowances on the clinical session, which would encourage the audiologist to keep the conversation ‘on task’. Scores for item 18 (ie, when clients look up audiological information on their own, this usually confuses more than it helps) followed the reverse trend with audiologists in India and Iran scoring higher than audiologists in Portugal, albeit by relatively small differences in score. In this case, the ability of the patient population to find relevant information may be related to local factors such as internet access and language-specific information resources. Item 2 had the largest difference in score between Portugal and the other two countries (ie, although healthcare is less personal these days, this is a small price to pay for audiological advances). The responses could have been influenced by how the respondent views recent audiological advances. Improvements in technology have occurred at different times in different countries; it may be that audiologist's responses are reflecting their opinion on which technological advancements they feel have helped clients, as much as reflecting their opinion on the changing personal aspect of healthcare. An example would be if the move from analogue to digital technology was more recent for India and Iran; this may be valued more highly against a loss of personal involvement in healthcare than in Portugal, if this development had occurred further in the past. Studies from other disciplines have shown that the PPOS scores indicating preference for patient-centredness can vary among professionals in different countries. For example, medical practitioners’ mean PPOS scores of 4.8 in the USA,4 compared to 3.3 in Greece.23
The key influencing factors for the differences observed are the local healthcare system, national culture, organisational-related factors (see Grenness et al2), ethnicity24 and cross-cultural aspects,19 as indicated in studies from other areas. We hypothesise that one of the main contributing factors could be the ‘culture’. Geert Hofstede defines culture as “the collective programming of the mind distinguishing the members of one group or category of people from another”.25 Figure 2 represents Hofstede's dimensions of national culture in Portugal, India and Iran, which include: power distance; individualism; masculinity; uncertainty avoidance; pragmatism; and indulgence.25 A greater number of similarities are noticed between India and Iran when compared to Portugal (eg, individualism, masculinity and uncertainty avoidance). These observations are consistent with a contribution of culture to differences and similarities in preferences for patient-centredness noticed among different countries in this study. It would also be consistent with the previously reported findings of medical practitioners from the USA, a country with a very high score of Individualism, compared to Greece, considered to be a collectivist culture. Given this finding, we argue that there is a need for increased focus on cultural competency for professionals in order to deliver patient-centred care.26
Figure 2.
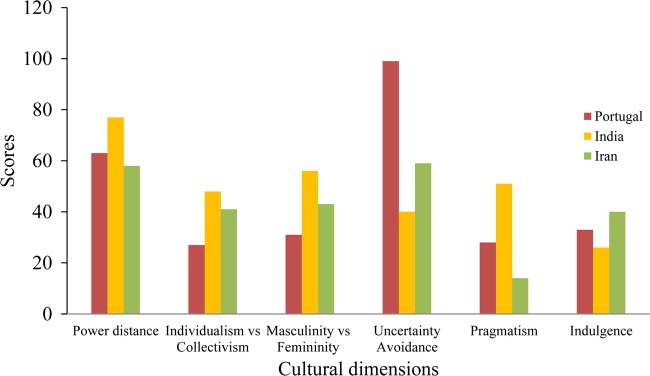
Bar graph showing Hofstede’s cultural dimension values for Portugal, India and Iran. A high score power distance expresses that the less powerful members of a society accept and expect that power is distributed unequally. A high score on Individualism versus Collectivism can be defined as a preference for a loosely-knit social framework in which individuals are expected to take care of only themselves and their immediate families. A high score on ‘Masculinity versus Femininity’ suggests a preference in society for achievement, heroism, assertiveness and material rewards for success as opposed to cooperation, modesty, caring for the weak and quality of life. A high score on ‘Uncertainty Avoidance’ suggests members of a society feel uncomfortable with uncertainty and ambiguity. A high score on ‘Pragmatism’ suggests the society encourages thrift and efforts in modern education as a way to prepare for the future, as opposed to relying on time-honoured traditions. A high score on ‘Indulgence’ suggests the society follows gratification of basic and natural human drives related to enjoying life and having fun, as opposed to restraint in such activities based on social norms.
It is important to note that the current study focused on self-reported preferences for patient-centredness and not the actual clinical behaviour. Previous studies have suggested that the preferences for patient-centredness measured using PPOS correlate well with the actual clinical behaviour of professionals as measured by verbal exchange between patients and professionals.9 However, not much is known about patients’ preferences for hearing healthcare services and more importantly for ‘patient-centred healthcare’ within these countries. Further studies with a qualitative design may help explore these aspects. A further consideration is to what extent the clinician population will reflect the general ‘culture’ that is assigned to a nation. It is likely that this demographic would vary from the general population as regards educational level in addition to other socioeconomic factors, and the degree of difference is likely to be specific to the particular profession, and also country, being considered.
Other potential influences on audiologists’ preferences for patient centredness are age, duration of work experience and employment type.13 In the current study no significant differences existed between groups in terms of age and duration of work experience. The distribution of audiologists among different areas of employment was broadly similar between countries. However, differences were noted in terms of participants’ gender between countries. The estimates of male/female ratio practicing in audiology in these countries, as indicated by the professional bodies, are 1:4, 1:2 and 1:2 in Portugal, India and Iran, respectively. The current study sample had a similar gender pattern of audiologists even though not exactly matching these ratios. Gender has been found to influence the practitioners’ preference for patient-centredness with women displaying a greater preference for patient-centredness than their male counterparts,27 28 although this was not found to be a significant factor for audiologists’ preferences for patient-centredness in a large scale Australian study.13 Hence, further exploration of a gender effect in preference for patient-centredness is necessary in future studies.
Study implications and future directions
Patient-centredness is important in healthcare as it is linked to patient-outcomes such as increased satisfaction, adherence and health outcomes29 30 and also to perceived quality of service delivery.17 Considering that there is evidence that rehabilitative audiology patients also prefer patient-centred care,13 this concept has direct clinical implications in hearing healthcare.
The current study reports some interesting findings about audiologists’ preference for patient-centredness in different countries. However, it might be more appropriate to study patient-centredness of professionals in congruence with patients.4 For example, although the mean scores in India and Iran were lower than those of Portugal, if the patients in India and Iran have similar preferences for patient-centredness as the professionals, then care delivery is likely to meet patients’ expectations. Further, it would be useful and important to understand how the concept of patient-centredness is understood and valued by professionals as well as patients in different countries. If future studies (focusing on professionals and patients as well) suggest marked differences, similar to those demonstrated here, it may be necessary to reconceptualise the principle of patient-centredness.
Given that patient-centredness has been found to be an important factor in patient satisfaction and outcomes, at least in some countries, and since it has been suggested that clinicians can learn to become patient-centred,31 it may be necessary to include such concepts in training programmes, particularly in cases where practitioners demonstrate a significantly lower preference towards patient-centredness than their patients. Moreover, future studies may also focus on understanding the differences and similarities in preferences towards patient-centredness among subcultures within the same country (eg, different ethnic groups). Such studies may further inform the arguments of researchers who have been advocating the need for cultural competence (the ability of individuals, groups and organisations to effectively interact with individuals with different cultural backgrounds) in the delivery of healthcare services.32 Moreover, this may have consequences for the increasingly international audiology workforce16 in terms of the migration of audiologists to other countries for employment and the provision of distance-learning models of audiology education. Overall, this information may highlight the need to consider patient-centredness in order to optimise hearing healthcare globally.
Strengths and limitations
A response rate of 76% was obtained for this questionnaire-based study and there was diversity in the data from audiologists distributed across three countries. Nevertheless, the study has some limitations. For example, aspects such as healthcare delivery models and educational system were not controlled for, but may have contributed to the differences and similarities noticed in audiologists’ preferences. However, there was a reasonable spread of audiologist practising in public and private audiology clinics, and audiologists in all three countries were trained to a minimum standard of a Bachelor's degree. A relatively small sample size and lack of anonymity in data collection were also limitations of the current study. We were aware that a sampling bias may have been present, since audiologists with particular preferences may have been more inclined to respond to the questionnaire. The fact that identifiable information may have been present in the emailed responses had the potential to influence/discourage an individual's response. These biases would have been present for all countries.
Conclusion
The data described here are the first in hearing healthcare to demonstrate specific differences and similarities in audiologists’ preferences for patient-centredness across three countries. We observed that the two countries with the most similar cultural profile had the most similar preference level for patient-centred care. There are several factors that might influence preference for patient-centred care, and further investigation is required in order to determine the role of the education and healthcare system, organisational-related factors and ethnicity in contributing to the differences and similarities noticed. Clinician reported patient-centredness and the cultural aspects of the clinician and patient population are different across countries and this may have implications for the training professionals and implementation of clinical practice in terms of optimising hearing healthcare across countries.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Professors Edward Krupat and Louise Hickson for allowing us to use the modified version of the PPOS.
Footnotes
Contributors: VM contributed to most parts of the work including data collection, analysis and writing. PG contributed to data analysis, interpretation and write up. DT contributed to data collection and write up. TA and KR contributed to data collection and write up.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None.
Ethics approval: Ethical approval was obtained from the School of Allied Health Sciences, Polytechnic Institute of Porto at Porto and All India Institute of Speech and Hearing at Mysore for data collection in Portugal and India respectively. This kind of study did not require ethical approval under the Department of Audiology, University of Social Welfare and Rehabilitation Sciences at Tehran for data collection in Iran.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med 2000;51:1087–110 [DOI] [PubMed] [Google Scholar]
- 2.Grenness C, Hickson L, Laplante-Lévesque A, et al. Patient-centredness care: a review for rehabilitative audiologists. Int J Audiol 2014;53:S60–7 [DOI] [PubMed] [Google Scholar]
- 3.Michie S, Miles J, Weinman J. Patient-centredness in illness: what is it and does it matter? Patient Educ Couns 2003;51:197–206 [DOI] [PubMed] [Google Scholar]
- 4.Krupat E, Rosenkranz SL, Yeager CM, et al. The practice orientations of physicians and patients: the effect of doctor-patient congruence on satisfaction. Patient Educ Couns 2000;39:49–59 [DOI] [PubMed] [Google Scholar]
- 5.Chan CMH, Azman WA. Attitudes and role orientation of doctor-patient fit and patient satisfaction in cancer care. Singapore Med J 2012;53:52–6 [PubMed] [Google Scholar]
- 6.Hogden A, Greenfeild D, Nugus P, et al. Engaging in patient decision-making in multidisciplinary care for amyotrophic lateral sclerosis: the views of health professionals. Patient Prefer Adher 2012;6:691–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Umar N, Schollgen I, Terris DD. It is not always about gains: utilities and disutilities associated with treatment features in patients with moderate-to-severe psoriasis. Patient Prefer Adher 2012;6:187–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levinson W, Roter D, Mullooly J, et al. Physician-patient communication: The relationship with malpractice claims among primary care physicians and surgeons. J Am Med Assoc 1997;277:553–9 [DOI] [PubMed] [Google Scholar]
- 9.Shaw WS, Woiszwillo MJ, Krupat E. Further validation of the Patient-Practitioner Orientation Scale (PPOS) from recorded visits for back pain. Patient Educ Couns 2012;89:288–91 [DOI] [PubMed] [Google Scholar]
- 10.Sweetow RW, Davis A, Hickson L. Paradigm shift in audiology education. Audiology Today2010:32–5
- 11.Hickson L. Defining a paradigm shift. Sem Hear 2012;33:3–8 [Google Scholar]
- 12.Grenness C, Hickson L, Laplante-Lévesque A, et al. Patient-centred audiological rehabilitation: perspectives of older adults who own hearing aids. Int J Audiol 2014;53:S68–75 [DOI] [PubMed] [Google Scholar]
- 13.Laplante-Lévesque A, Hickson L, Grenness C. An Australian survey of audiologists’ preferences for patient-centredness. Int J Audiol 2014;53:S76–82 [DOI] [PubMed] [Google Scholar]
- 14.Laplante-Lévesque A, Hickson L, Worrall L. A qualitative study of shared decision making in rehabilitative audiology. J Acad Rehabil Audiol 2011;43:27–43 [Google Scholar]
- 15.Poost-Foroosh L, Jennings MB, Shaw L, et al. Factors in client-clinician interaction that influence hearing aid adoption. Trends Amplif 2011;15:127–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goulios H, Patuzzi RB. Audiology education and practice from an international perspective. Int J Audiol 2008;47:647–64 [DOI] [PubMed] [Google Scholar]
- 17.Saha S, Beach MC, Cooper LA. Patient centredness, cultural competency and healthcare quality. J Natl Med Assoc 2008;100:1275–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao F, Manchaiah V, St. Claire L, et al. Exploring the influence of culture on hearing help-seeing and hearing aid uptake: a discussion paper. Int J Audiol. [DOI] [PubMed] [Google Scholar]
- 19.Al-Bawardy R, Blatt B, Al-Shohaib S, et al. Cross-cultural comparison of the patient-centredness of the hidden curriculum between a Saudi Arabia and 9 US medical schools. Med Educ Online 2009;14:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krupat E, Putnam SM, Yeager CM. The fit between doctors and patient: can it be measured? J Gen Intern Med 1996;11:134 [Google Scholar]
- 21.Beaton DE, Bombardier C, Guillemin F, et al. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000;25:3186–91 [DOI] [PubMed] [Google Scholar]
- 22.Goulios H, Patuzzi RB. Audiology education and practice from an international perspective. Int J of Audiol 2008;47:647–64 [DOI] [PubMed] [Google Scholar]
- 23.Tsimtsiou Z, Benos A, Garyfallos AA, et al. Predictors of physicians’ attitudes toward sharing information with patients and addressing psychosocial needs: a cross-sectional study in Greece. Health Commun 2012;27:257–63 [DOI] [PubMed] [Google Scholar]
- 24.Cooper LA, Roter D, Johnson RL, et al. Patient-centred communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003;139:907–15 [DOI] [PubMed] [Google Scholar]
- 25.Hofstede Centre. National Cultural Dimensions. http://geert-hofstede.com/dimensions.html (accessed 24 Apr 2014).
- 26.Epner DE, Baile WF. Patient-centred care: the key to cultural competence. Ann Oncol 2012;23(Suppl 3):33–42 [DOI] [PubMed] [Google Scholar]
- 27.Kaplan RM, Gandek B, Greenfield S, et al. Patient and visit characteristics related to physicians participatory style: results from medical outcome study. Med Care 1995;33:1176–83 [DOI] [PubMed] [Google Scholar]
- 28.Roter D, Hall J. Doctors talking with patients, Patients talking with doctors. Westport: Auburn House, 2006 [Google Scholar]
- 29.DiMatteo MR, Giordani PJ, Lepper HS, et al. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care 2002;40:794–811 [DOI] [PubMed] [Google Scholar]
- 30.Swenson SL, Buell S, Zettler P, et al. Patient-centered communication: do patients really prefer it? J Gen Intern Med 2004;19:1069–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lewin S, Skea ZC, Entwistle VA, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2009;1:1–60 [DOI] [PubMed] [Google Scholar]
- 32.Campinha-Bacote J. The process of cultural competence in the delivery of healthcare services: a model of care. J Transcult Nurs 2002;13:181–4 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


