Abstract
The ECG is a test that is used frequently in the acute setting. It has a significant impact on decisions regarding patient discharge and further investigations. On a single day in the ambulatory emergency care setting two patients presented with chest pain. The ECG findings were abnormal, but also out of context with the clinical findings. On close inspection of the ECG machine it was identified that although all leads attached to the patient were in the correct position, the two cables connecting the leads to the machine had been reversed. Had the error not been discovered promptly there was the potential that further, more harmful investigations would have been performed. These cases highlight that although the ECG is a simple and non-invasive investigation it should be an adjunct to clinical working diagnosis.
Background
The ECG is a test that is used frequently in the acute setting. It has a significant impact on decisions regarding patient discharge and further investigations. Common mistakes discussed in the literature include lead placement. Below we discuss repeated unexpected ECG findings on a single day in the ambulatory emergency care setting, which was caused by incorrect assembly of the machine. Had the error not been discovered promptly more harmful investigations would have been organised, such as a CT pulmonary angiogram or coronary angiogram. Although these machines are not disassembled and reassembled regularly it is concerning that the error was not noticed prior to the machine being used on patients. The patients were both reviewed on the same morning in an ambulatory emergency care unit and were discharged on the same day, however, had the error not been found they may have required inpatient stays and unnecessary investigations.
Case presentation
Case 1
A 77-year-old man was referred by his general practitioner (GP) with a 1-week history of sharp retrosternal chest pain with some exertional breathlessness. He had a history of moderate aortic stenosis, hypertension, chronic obstructive pulmonary disease, polymyalgia rheumatic, transitional cell carcinoma of the bladder and prostate carcinoma. His regular medication included prednisolone 10 mg daily, amlodipine 5 mg daily, ramipril 5 mg daily, lansoprazole 30 mg daily, aspirin 75 mg daily, alendronic acid 70 mg weekly and goserelin injections every 3 months. On examination, blood pressure was 121/29 mm Hg, pulse 94 bpm and regular, and saturations 99% on room air. He had an ejection systolic murmur, tenderness in the epigastric region and palpation of the right-sided subscapular region replicated his pain. The remainder of the examination was normal. The clinical impression was musculoskeletal chest pain.
Investigations
The GP had commented on an ECG with left bundle branch block, however, our initial ECG (figure 1) demonstrated a right bundle branch block; this raised concerns of massive pulmonary embolus. This was out of keeping with the clinical findings and the ECG in the GP surgery. The older ECG's used for comparison demonstrated a left bundle branch block. The ECG was repeated and the positions of all leads were checked, but the ECGs consistently demonstrated a right bundle branch block. As this contradicted the clinical findings the ECG machine was exchanged for an alternative one. The repeat ECG showed a left bundle branch block, which was unchanged from previous tracings. (figure 2)
Figure 1.
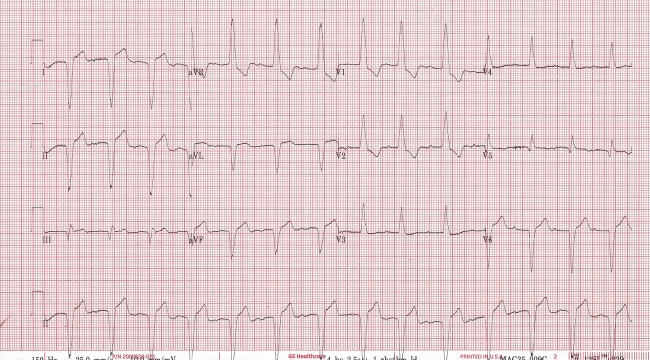
Case 1 ECG tracing from an incorrectly assembled machine.
Figure 2.
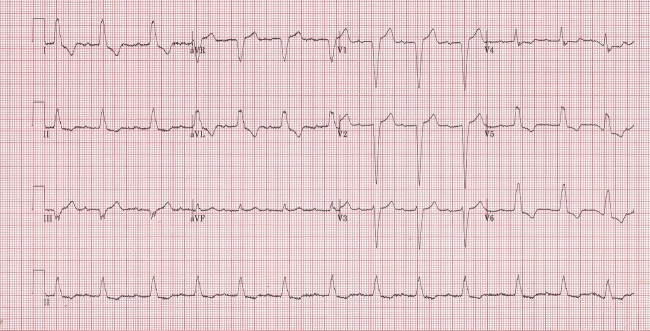
Case 1 ECG tracing from a correctly assembled machine.
Case 2
A 72-year-old man presented with exertional shortness of breath associated with central chest pain and epigastric discomfort. He had a history of type two diabetes mellitus, hypertension, hypercholesterolaemia and osteoarthritis. His medications included lisinopril 10 mg daily, simvastatin 40 mg daily, allopurinol 300 mg daily and aspirin 75 mg daily. Observations showed: blood pressure 136/71 mm Hg, pulse 74 bpm and oxygen saturation 100% on room air. Clinical examination was unremarkable and he was pain free. The clinical impression was gastritis.
Investigations
An initial ECG revealed T wave inversion in leads V2–6 (figure 3). This raised the concern of an acute coronary syndrome with the need for immediate treatment and further investigations. In view of the previous case a repeat ECG with a different machine revealed a normal tracing (figure 4).
Figure 3.
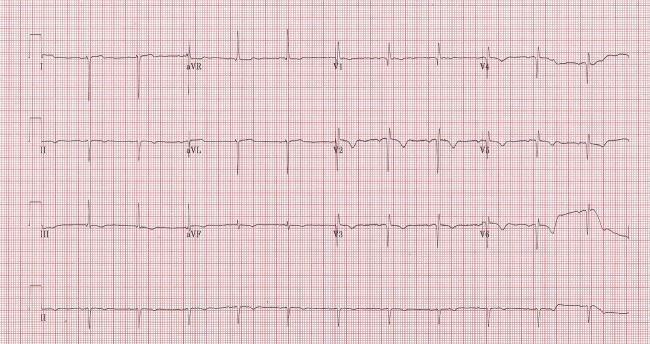
Case 2 ECG tracing from an incorrectly assembled machine.
Figure 4.
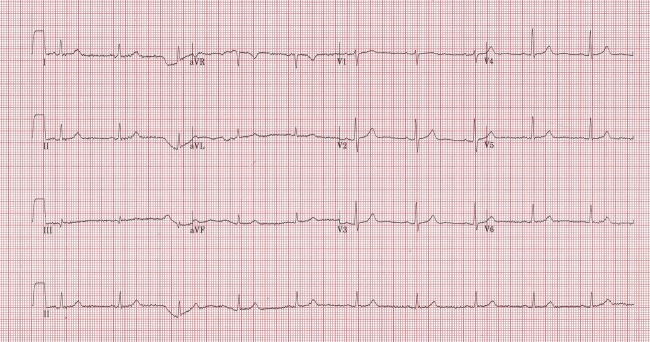
Case 2 ECG tracing from a correctly assembled machine.
Outcome and follow-up
The ECG machine was carefully reviewed, it was identified there are two cables that insert into the ECG machine from the leads attached to patients, one carries information from the right limb leads and chest leads 1–3, and the other from the left limb leads and chest leads 4–6. These cables had been reversed and were, therefore, incorrectly inserted into the machine (figure 5). After reversing the insertion of the cables (figure 6) the ECG tracings returned to normal for the patients involved. Within the acute medical unit the ECG automatic interpretation is not used, so it is not known what this would have contributed to the interpretation of these patients’ ECGs. It is not known how long the machine was incorrectly assembled or why these cables were removed, but it was presumed to be during cleaning of the machine. An incident form was completed to highlight the importance of appropriate medical equipment calibration and the effect this can have on patient care. The patients have all been made aware of the error and have come to no harm as a result of it.
Figure 5.

Picture of an incorrectly assembled machine.
Figure 6.
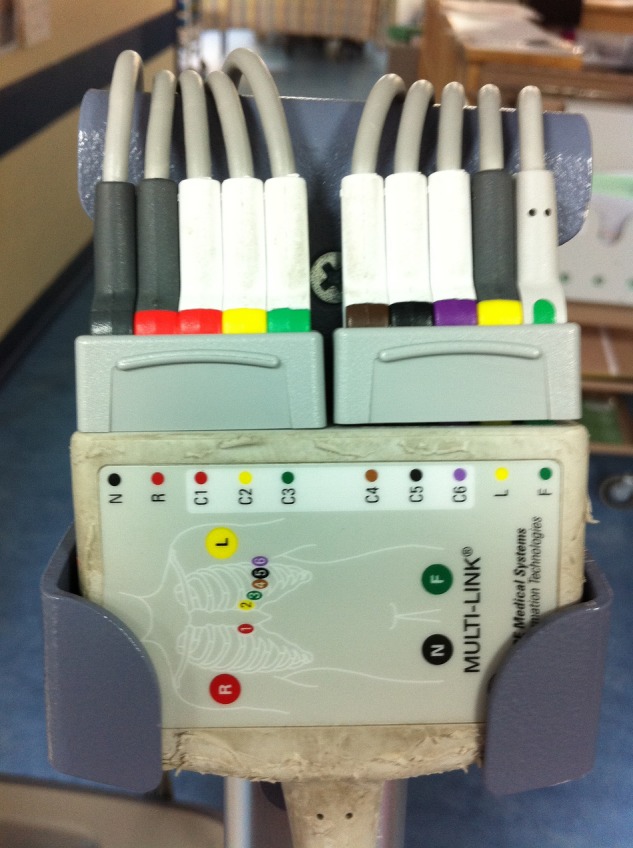
Picture of a correctly assembled machine.
Discussion
During a review of the literature there were examples of ECG tracings resulting in further investigation due to electrode misplacement1–3 but no evidence of cases where the cables carrying this information were incorrectly inserted into the machine. The ECG deflexions are dependent on the conduction of electrical impulses through heart tissue. If leads or cables, as described above, are reversed the appearance of the electrical conduction through the heart will change. This can lead to a wider differential diagnosis and unnecessary investigations for patients.
Patient's perspective.
Both patients were anxious as a result of multiple ECG's. They were both relieved when the error was identified. They were both keen for their experiences to be shared.
Learning points.
The ECG is a simple non-invasive test that should be an adjunct to clinical working diagnosis.
It is possible to assemble the ECG incorrectly and proceed to obtaining ECG tracings of patients.
In abnormal ECG tracings out of keeping with clinical context, check the machine carefully.
Individuals using the ECG machine should have formal training, which includes the potential errors in cable connection.
Training should cover the recognition of artefacts that arise due to technical issues.
Footnotes
Contributors: HJE wrote and edited the case report. HA-K was responsible for the initial management of the patients. NR was the consultant responsible for the patients’ care and edited and amended the drafts. All authors have reviewed the manuscript and agreed with the final draft.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rudiger A, Hellermann JP, Mukherjee R, et al. Electrocardiographic artifacts due to electrode misplacement and their frequency in different clinical settings. Am J Emerg Med 2007;25:174–8 [DOI] [PubMed] [Google Scholar]
- 2.Harrigan RA, Chan TC, Brady WJ. Electrocardiographic electrode misplacement, misconnection and artefact. J Emerg Med 2012;43:1038–44 [DOI] [PubMed] [Google Scholar]
- 3.García-Niebla J, García PL. An unusual case of electrode misplacement: left arm and V2 electrode reversal. J Electrocardiol 2008;41:380–1 [DOI] [PubMed] [Google Scholar]


