Abstract
We report the case of a 33-year-old man who presented several times to healthcare professionals over a 6-week period with a painful swollen right knee. He had a history of chronic osteomyelitis of the left femur and had recently stopped taking suppressive antibiotics. A joint aspirate did not demonstrate any organisms. On subsequent review by the orthopaedic team MRI was performed which revealed an isolated area of osteomyelitis and an abscess in his right patella. He underwent arthrotomy, debridement and irrigation of the joint alongside antibiotic treatment. We highlight this case, as isolated osteomyelitis of the patella is a rare condition, especially in adults. In addition, the presenting features of osteomyelitis of the patella are varied and joint fluid aspirates often do not reveal an organism. This case therefore aims to raise an awareness of this condition and thereby ensure a high index of suspicion when symptoms or signs are present and inform clinicians of the investigative steps in order to avoid a delay in diagnosis as seen in this case.
Background
Osteomyelitis is a condition in which an infecting microorganism causes an inflammatory process accompanied by progressive destruction and necrosis of bone and surrounding tissues. Although uncommon, it can cause significant morbidity, pose substantial challenges in management and can progress to chronic and persistent infection.1
Osteomyelitis can be classified according to the aetiology, pathogenesis as well as the age and immune status of the patient.2 It can result from direct inoculation, for example, following trauma, secondary infection from a contiguous focus in the surrounding bone or soft tissues, seeding from a distant focus through haematogeneous spread and vascular insufficiency.3 4
Isolated osteomyelitis of the patella is rare. It is more commonly seen in children between the ages of 5 and 15 years than in adults. In the paediatric population it is often secondary to seeding from a haematogenous infection as the patella ossifies. The majority, of the albeit limited number of cases in adults reported in the literature, have an associated history of trauma, systemic infections including tuberculosis, behaviours risking systemic infection such as intravenous drug use or immunocompromised states such as HIV infection.5–7
Diagnosis is often delayed due to the rarity and lack of familiarity with the condition and variability of presentation. Joint aspiration is also often negative.
Clinicians should therefore consider osteomyelitis as a potential diagnosis in patients presenting with an acutely inflamed, painful, swollen knee after septic arthritis has been excluded. A particularly high index of suspicion should be raised if associated factors as previously outlined are present.
Both septic arthritis and osteomyelitis require intravenous antibiotic therapy as part of treatment. However, osteomyelitis, in particular with abscess formation requires more invasive surgical intervention and prolonged antibiotic treatment targeted towards the isolated pathogen.
We report the case of a 33-year-old man with isolated osteomyelitis of the patella after treatment for chronic osteomyelitis of the contralateral femur for several years.
Case presentation
The patient initially presented to the accident and emergency department with a 5-day history of a painful swollen right knee.
The patient had a history of chronic osteomyelitis of the contralateral femur initially diagnosed 14 years previously (figure 1). This had been treated with several episodes of surgical debridement and multiple courses of antibiotics including ciprofloxacin and flucloxacillin. He had previously been referred to a specialist centre for definitive surgery but was not considered to be a suitable candidate. Recently, long-term suppressive flucloxacillin had provided good symptomatic control.
Figure 1.

Anteroposterior and lateral view of the left femur demonstrating changes associated with previous osteomyelitis.
His medical history also included intravenous drug use, although the patient denied injecting in the preceding months and a previous left calf deep vein thrombosis. The patient was on a methadone programme.
On examination, the patient was unable to weight bear but could actively flex the knee to 90°. He was non-feverish and no discrepancy in calf or thigh measurements was noted.
Crucially the patient reported that he had stopped taking his suppressive antibiotics 3 weeks prior to presentation.
Blood tests were attempted but no samples could be obtained due to poor peripheral venous access. Plain radiograph of the right knee did not reveal any abnormality (figure 2) and a Doppler ultrasound examination of the lower limb vessels did not demonstrate a deep vein thrombosis. The patient was diagnosed with a meniscal injury and discharged.
Figure 2.

Initial anteroposterior and lateral view of the right knee revealing no abnormality.
The patient continued to have pain and swelling of his right knee, but despite several interim visits, only reported this again to his general practitioner (GP) 4 weeks later. The patient's GP noted that the knee was swollen and tender but he had a good range of motion; he was referred for a further radiograph of the right knee (figure 3). The radiograph was performed the following day but the report was not reviewed for a further 11 days. This stated that there was no bony abnormality, destruction or periosteal reaction seen but there was a supra-patellar joint effusion and soft tissue thickening. It was recommended by the reporting radiologist that septic arthritis be excluded and advised an urgent ultrasound scan of the knee and blood tests. A routine orthopaedic referral was sent.
Figure 3.

Subsequent anteroposterior and lateral view of the right knee showing a supra-patella effusion and soft tissue thickening.
Forty-eight hours later, the patient presented for blood tests. His pain had significantly worsened and he was unable to move the knee. An urgent referral was therefore made to the on-call orthopaedic team who made arrangements to review the patient the same day.
Orthopaedic review found the patient to have a swollen right knee with a large effusion (figure 4) and an active range of motion of 30–60°. He was unable to weight bear due to pain. Blood samples were obtained using ultrasound guidance and revealed a white cell count (WCC) of 8.1×109/L and a C reactive protein (CRP) of 74 mg/L. Blood cultures were negative. Aspiration of fluid from the right knee was performed; the results are shown in table 1.
Figure 4.
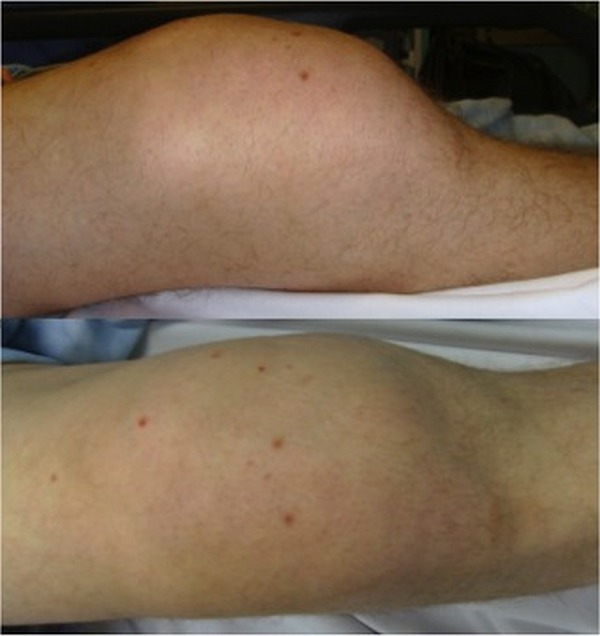
Anteroposterior and lateral view of the right knee demonstrating the gross swelling.
Table 1.
Joint fluid aspirate results
| Parameter | Value |
|---|---|
| White cell count | 6300 µ/L |
| Red blood cell count | 495 µ/L |
| Polymorphs | 95% |
| Lymphocytes | 5% |
| Microscopy | No organism seen |
The patient was advised that he should be admitted but declined. He was reviewed in clinic the following day and the suspicion of osteomyelitis around the right knee was raised.
An urgent MRI was arranged; this revealed isolated changes within the right patella measuring 14×13×15 mm, which had destroyed the cortex with partial destruction of the cartilage (figures 5–7). The changes were consistent with osteomyelitis and an abscess formation. There were no changes in the adjacent femur or tibia which would suggest contiguous spread.
Figure 5.
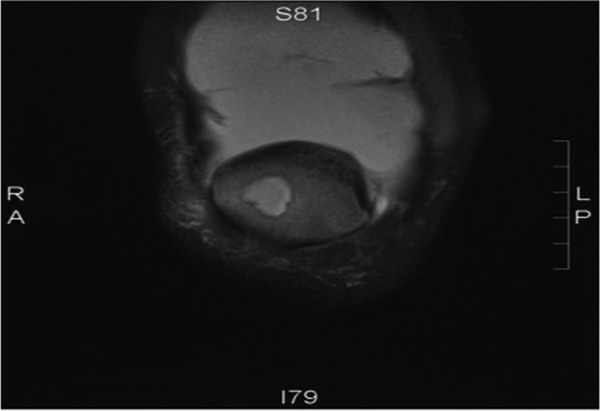
Coronal proton density fat saturated MRI showing collection in patella.
Figure 6.
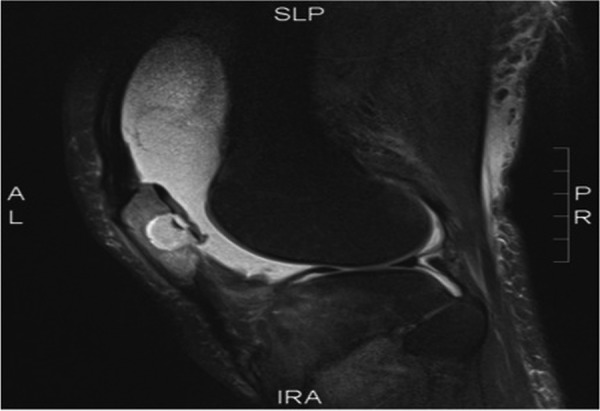
Sagittal proton density fat saturated MRI showing collection in patella.
Figure 7.
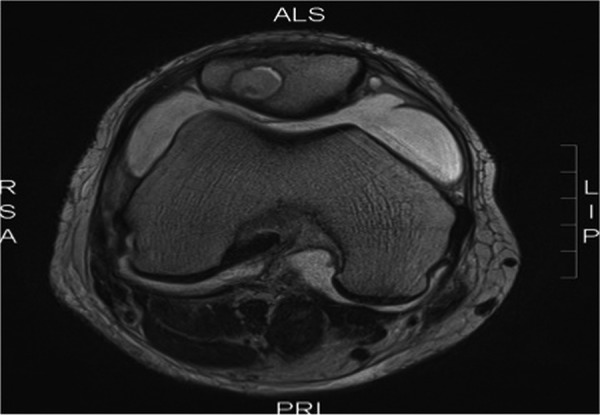
Axial T2 MRI showing proximity of collection to cartilage surface.
Treatment
The patient was admitted from clinic and underwent arthrotomy of the right knee. A large volume of serous fluid was found within the knee joint and a collection of pus was located in the supra-patellar pouch (figure 8). A cavity in the centre of the patella consistent with that seen on MRI was found to contain pus (figures 9 and 10). Microbiology and histology samples were obtained followed by thorough debridement, curettage and irrigation of the cavity and joint.
Figure 8.
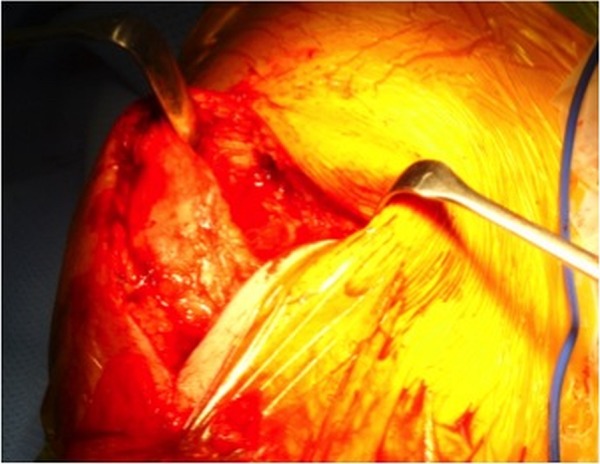
Supra-patella pouch containing a collection of pus.
Figure 9.

Pus swab in cavity in patella.
Figure 10.
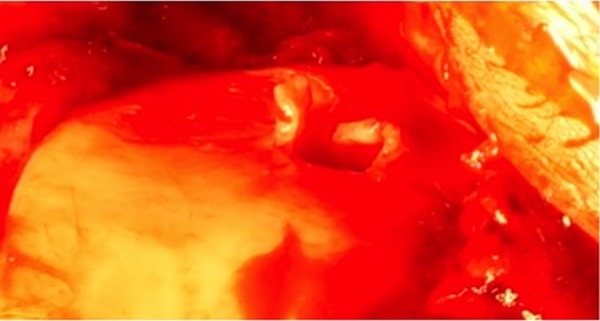
Cavity in patella.
The patient was started empirically on intravenous teicoplanin following advice from the consultant microbiologist. Three of four intraoperative cultures grew a sensitive Staphylococcus aureus in-line with previous cultures from the left femur. The patient refused central venous access and when peripheral access was lost, after 4 days, he was changed to fusidic acid and clindamycin orally.
Outcome and follow-up
The patient was reviewed 3 months postoperatively. The surgical wound had healed. He could fully extend his knee but flexion was limited to 40°. His CRP was 5 mg/L and WCC 9.1×109/L. He was continuing to take clindamycin and fusidic acid. He has failed to attend further postoperative appointments.
Discussion
Osteomyelitis of the patella is a rare condition. It has previously been described as a disease of the paediatric population, occurring most commonly in children between 5 and 15 years.8 In these cases it is predominantly related to secondary seeding of a haematogenous infection, which can be directly explained by the development of the patella and its vascular anatomy.
Prior to age 5, the patella is primarily cartilaginous, which explains the rarity of the condition in younger children.9 10 Noticeable vascularisation begins at ages 4–5, with the patella reaching its maximal blood supply by age 12. There is an anastomotic extraosseous arterial network, with contributions from the superior and inferior geniculates and the anterior tibial recurrent artery. As well as this, a well-developed intraosseous network of vessels exists.10–14
There are few reported cases of isolated osteomyelitis of the patella in adults and as a result detailed literature regarding osteomyelitis of the patella in adults is sparse. Several large series reviewing bone and joint infections failed to identify any cases.15–17
In contrast to children, proportionally few cases of isolated patella osteomyelitis in adults are related to primary haematogenous infection, as following ossification of the patella the blood supply declines. Adult cases are more often associated with risk factors such as immunocompromised states, intravenous drug use, HIV and trauma.5–7 18–20
In this case, the patient had recently stopped his long-term suppressive antibiotics so it is likely that the osteomyelitis occurred from haematogeneous spread from the contralateral femur. The culture results from the patella also grew S. aureus, similar to multiple biopsies taken during surgical debridement of the left femur on several occasions over the preceding years, supporting a diagnosis of haematogeneous spread. There were no clinical signs to raise concerns of infective endocarditis as a source of infection in this case. MRI of the knee did not show any changes in the adjacent femur or tibia that would have raised the possibility of contiguous spread.
The presentation of osteomyelitis of the patella is varied and often non-specific. Point tenderness over the patella, as well as persistent peri-patellar pain and swelling are the most consistent clinical findings and a diagnosis of osteomyelitis should be considered in these cases.21 A joint effusion may be present. As in our case, it can be sterile and is often reactionary; a negative aspirate therefore does not exclude the diagnosis.22 Involvement of the knee joint is more common in adults than children because of the presence of the thicker articular cartilage in paediatric cases.21 In contrast to septic arthritis, range of movement of the knee joint can be relatively well maintained. Systemic upset, such as fever and malaise, may or may not be present.
Investigation involves a combination of laboratory tests and imaging, similar to osteomyelitis in other areas. Serum inflammatory markers are often raised, but are non-specific; they are helpful in supporting the diagnosis and monitoring disease resolution. Blood cultures are positive in up to 50% of cases of acute osteomyelitis.23
S. aureus is by far the most commonly described infecting organism. However other organisms, including Streptococcus, Escherichia coli and Clostridium spp have also been reported.11 21 24
Standard radiographs are often the first-line investigation for osteomyelitis. However, the patella is a sesamoid bone with no real periosteum; therefore the pathognomonic sign of periosteal elevation is absent. Plain radiographs of the knee are therefore not particularly helpful in diagnosis of osteomyelitis of the patella.5
MRI is considered to be the mainstay of imaging and is the modality of choice for diagnosis, as it provides excellent contrast between normal and abnormal areas of bone marrow.25 26
Treatment of osteomyelitis of the patella is similar to osteomyelitis in other areas. Wherever possible a tissue diagnosis with identification of the causative organism should be sought, with antibiotic therapy targeted towards this. Parenteral antibiotics should be initiated and continued until there is a clinical improvement as well as a persistent fall in inflammatory markers. Oral antibiotics can then be started with recommended minimum treatment duration of 4–6 weeks.
Often in such cases of osteomyelitis as this, acute suppurative inflammation along with sequestra formation leads to segments of avascular bone harbouring bacteria despite intravenous antibiotic treatment. In these instances, medical treatment of osteomyelitis alone is inadequate. Surgical intervention with curettage and debridement is required to remove sequestra, lower the bacterial inoculum and reducing the occurrence of persistent infection.8
In conclusion, osteomyelitis of the patella is an exceedingly rare condition in the adult population. Diagnosis is often difficult due to variable presentation and a high index of suspicion is required for prompt identification and treatment.
Osteomyelitis should be considered as a differential diagnosis in patients with persistent peri-patellar pain and swelling. There should be a low threshold for performing MRI in such patients and subsequent tissue diagnosis. Early intervention with intravenous antibiotics and surgical debridement is paramount to reduce morbidity and to prevent disease progression and complications, in particular septic arthritis of knee.
Learning points.
The clinical presentation of patella osteomyelitis is varied and often non-specific.
A low index of suspicion for osteomyelitis of the patella should be exhibited in patients with persistent peri-patellar pain and swelling without other diagnosed cause.
Most cases have associated risk factors, in particular intravenous drug use and tuberculosis—elucidating these from a full history is therefore paramount.
A negative joint aspirate does not rule out osteomyelitis or septic arthritis.
MRI is the imaging modality of choice to assist with the diagnosis of patella osteomyelitis.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Smith IM, Austin OMB, Batchelor AG. The treatment of chronic osteomyelitis: a 10 year audit. J Plast Reconstr Aesthet Surg 2006;59:11–15 [DOI] [PubMed] [Google Scholar]
- 2.Pineda C, Vargas A, Rodriguez AV. Imaging of osteomyelitis: current concepts. Infect Dis Clin North Am 2006;20:789–825 [DOI] [PubMed] [Google Scholar]
- 3.Sia IG, Berbari EF. Infection and musculoskeletal conditions: osteomyelitis. Best Pract Res Clin Rheumatol 2006;20:1065–81 [DOI] [PubMed] [Google Scholar]
- 4.Lew DP, Waldvogel FA. Osteomyelitis. Lancet 2004;364:369–79 [DOI] [PubMed] [Google Scholar]
- 5.Kankate RK, Selvan TP. Primary haematogenous osteomyelitis of the patella: a rare cause for anterior knee pain in an adult. Postgrad Med J 2000;76:707–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vail TP, Urbaniak JR. Hematogenous patellar osteomyelitis associated with human immunodeficiency virus. Orthop Rev 1991;20:788–90 [PubMed] [Google Scholar]
- 7.Voon V, Arshad H, Davis B. Patella distal pole avulsion secondary to osteomyelitis in a healthy adult. Ann R Coll Surg Engl 2013;95:58–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Durani Y, Attia MW. An unusual case of knee pain. Pediatr Emerg Care 2006;22:426–9 [DOI] [PubMed] [Google Scholar]
- 9.Vaninbroukx J, Martens M, Verhelst M, et al. Haematogenous osteomyelitis of the patella. Report of three cases. Acta Orthop Scand 1976;47:566–9 [DOI] [PubMed] [Google Scholar]
- 10.Shim SS, Leung G. Blood supply of the knee joint. A microangiographic study in children and adults. Clin Orthop Relat Res 1986;(208):119–25 [PubMed] [Google Scholar]
- 11.Roy DR. Osteomyelitis of the patella. Clin Orthop Relat Res 2001;(389):30–4 [DOI] [PubMed] [Google Scholar]
- 12.Angella JJ. Osteomyelitis of the patella. Am J Dis Child 1967;113:590–3 [DOI] [PubMed] [Google Scholar]
- 13.Bjorkstrom S, Goldie IF. A study of the arterial supply of the patella in the normal state, in chondromalacia patellae and in osteoarthrosis. Acta Orthop Scand 1980;51:63–70 [DOI] [PubMed] [Google Scholar]
- 14.Scapinelli R. Blood supply of the human patella. Its relation to ischaemic necrosis after fracture. J Bone Joint Surg Br 1967;49:563–70 [PubMed] [Google Scholar]
- 15.Gillespie WJ, Mayo KM. The management of acute haematogenous osteomyelitis in the antibiotic era: a study of the outcome. J Bone Joint Surg Br 1981;63-B:126–31 [DOI] [PubMed] [Google Scholar]
- 16.Jackson MA, Nelson JD. Etiology and medical management of acute suppurative bone and joint infections in pediatric patients. J Pediatr Orthop 1982;2:313–23 [PubMed] [Google Scholar]
- 17.Roberts JM, Drummond DS, Breed AL, et al. Subacute hematogenous osteomyelitis in children: a retrospective study. J Pediatr Orthop 1982;2:249–54 [DOI] [PubMed] [Google Scholar]
- 18.Altschuler ELE, Yoon RSR, Dentico RR, et al. Spontaneous patella fracture presenting as osteomyelitis in focal dermal hypoplasia. Knee 2012;19:500–3 [DOI] [PubMed] [Google Scholar]
- 19.Agrawal VK, Agrawal RG. Tuberculosis of patella in an immunocompetent patient—a case report. Indian J Tuberc 2011;58:29–31 [PubMed] [Google Scholar]
- 20.Chouhan DK, Dhillon MS, Prakash M, et al. Patellar tuberculosis presenting as an osteolytic lesion. J Postgrad Med Edu Res 2013;47:221–2 [Google Scholar]
- 21.de Gheldere A. Haematogenous osteomyelitis of the patella in a child. Acta Orthop Belg 2009;75:554–6 [PubMed] [Google Scholar]
- 22.Gil-Albarova J, Gómez-Palacio VE, Herrera A. Hematogenous osteomyelitis of the patella. J Pediatr Orthop B 2012;21:411–14 [DOI] [PubMed] [Google Scholar]
- 23.Perron AD, Brady WJ, Miller MD. Orthopedic pitfalls in the ED: osteomyelitis. Am J Emerg Med 2003;21:61–7 [DOI] [PubMed] [Google Scholar]
- 24.Sanchez MC, Sebti R, Hassoun P, et al. Osteomyelitis of the patella caused by Legionella anisa. J Clin Microbiol 2013;51:2791–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Santiago Restrepo C, Gimenez CR, McCarthy K. Imaging of osteomyelitis and musculoskeletal soft tissue infections: current concepts. Rheum Dis Clin North Am 2003;29:89–109 [DOI] [PubMed] [Google Scholar]
- 26.Krogstad P. Osteomyelitis and septic arthritis. In: Textbook of paediatric infectious diseases. Editor: Ralph D Feigin. 5th edn. Philadelphia, PA: Saunders, 2004: 713–19 [Google Scholar]


