Abstract
The aim of the present study was to determine a good discriminatory cutoff for long working hours as a surrogate of chronic overload at work, which is associated with the approval of workers’ compensation claims for work-related cerebro-cardiovascular disease (WR-CVD) in Korea. We evaluated weekly working hours for four weeks prior to the onset of disease for all manufacturing industry claimants (N=319) of WR-CVD in 2010. The discrimination of long working hours in predicting approval of worker’s compensation pertaining to WR-CVD was compared across cases. The cutoff was calculated with sensitivity, specificity, and the area under the curve with 95% CI using the receiver operating curve (ROC) method. The cutoff point was thus calculated to be 60.75 h (AUC=0.89, 95% CI [0.84–0.93]), showing a sensitivity value of 65% and specificity of 94%. This is the first study to report that long working hours could be a predictor with good discrimination and high specificity of approval of WR-CVD cases. In Korea, long working hours and widespread chronic overload at work are recognized as a social problem. Our study results suggest an appropriate cutoff for working hours as an indicator of chronic overload for the purpose of approving claims of WR-CVD. Furthermore, these results could contribute to improving the consistency of evaluation.
Keywords: Workers’ compensation, Working hours, Cerebrovascular disease, Cardiovascular disease, ROC curve, Karoshi
Introduction
Workers’ compensation claims for work-related cerebro-cardiovascular disease (WR-CVD) are very costly compared to other claims in South Korea. WR-CVD claims represented 4.07% (284 cases) of all claims (5,986 cases) and 43.33% (354 cases) of total fatal claims in 20101). Thus, the proportion of indemnity costs for WR-CVD was 6.5% although the number of cases comprised only 2.5% of the total2). The indemnity cost for WR-CVD and the estimated direct medical and socioeconomic costs were $13 billion and $45 billion US dollars in 2005, respectively3).
WR-CVD and its diagnostic criteria were added by presidential decree to the Industrial Accident Compensation Insurance (IACI) system in 1978 initially, with more details amended in 2008. The diagnostic criteria for WR-CVD are as follows: 1) a sudden change in work environment within 24 h prior to the onset of WR-CVD; 2) a rapid increase in workload within 7 days prior to the onset of WR-CVD; and 3) chronic overload resulting from changes in responsibilities, the work environment, or in the amount, duration, and intensity of work for three months prior to the onset of WR-CVD. However, the number of approved claims of WR-CVD has decreased since 2005, as the application of the diagnostic criteria is not specified, especially for the final criterion of “chronic overload.” As a result, these criteria are applied differently depending on the panel gathered to judge and evaluate each claim; many have remarked on discrepancies observed among the final approval decisions. Furthermore, all claimants received their decision of approval through one of the six regional offices of the Work-related Disease Adjudication Committee (WDAC). The WDAC oversees occupational medicine, clinical medicine, and legal claims. Both the attendance and approval of a majority of the members are required for approval decisions for work-related claims. In the absence of practical guidelines, the final determining decision on workers’ compensation claims is vulnerable to the subjective perceptions of each WDAC member. Some dissenting opinions have pointed out the lack of consistent work-related patterns of chronic overload between approved and disapproved cases in the WDAC’s deliberations on WR-CVD cases.
The diagnostic criteria, including chronic overload, were adopted from a medical viewpoint holding that an excessive workload can cause vascularlesions and outcomes such as hypertension with chronic fatigue. However, “chronic overload” is difficult to quantify and evaluate. Chronic overload at work can be complicated by several factors such as long working hours, incidents at work, and mental stress. Among these, “long working hours” is useful in that it provides an objective measurement to support approval of WR-CVD claims; it is also a simple and easily understood indicator.
Sleep deficiency related to long working hours exacerbates mental and physical fatigue. Further, long working hours limits individual leisure and relaxation time. In addition, longer working hours means that workers are more likely to be exposed to chemical and physical health risks at work. Consequently, long working hours have been suggested as an independent risk factor for WR-CVD4, 5). Through a literature review and based on knowledge, we identified a few variations of the cutoff of long working hours related to WR-CVD claims. In addition, the relationship between long working hours and CVD in Korea is distinctly different from that in many Western countries. Baseline working hours in Korea were somewhat higher than in other countries among members of Organisation for Economic Co-operation and Development (OECD), with an average of 2,193 working hours per year. In contrast, the average for OECD countries is 1,749 hs per year6). This suggests that the diagnostic criteria should be defined based on valid evidence of the association between long working hours and WR-CVD, especially in working conditions associated with chronic overload such as those in Korea.
The purpose of this study was to assess the casedatabase and suggest an appropriate cutoff for long working hours to support the fair evaluation of WR-CVD claims. Among the risk factors for chronic overload, a measurement of working hours can be used as an objective, quantifiable indicator in the approval criteria for WR-CVD claims. The findings as evaluated here can lead to litigation to obtain scientific evidence to contribute to the consistency and fairness of the administration of benefits related to WR-CVD.
Subjects and Methods
Subjects
All data from WDAC claims filed nationwide by employees in the manufacturing industry diagnosed with CVD in 2010 were reevaluated by an occupational physician; the utilized data were established as the inclusion criteria. There were 629 claims from the manufacturing industry from the data of CVD cases on WDAC in 2010. The operational definition of “working hours” as a variable to differentiate long working hours as a factor of chronic overload was set as the average working hours for four weeks prior to the onset of CVD. The operational definition of “approval” and “disapproval” was the final decision whether the cause of the disease was work-related (and therefore eligible to receive benefits) or not according to a majority of the WDAC members. The exclusion criteria were claims filed by shift workers with a fixed-type shift without an extended working schedule, an unknown cause of death, part-time workers (less than 30 h per week), and those entries with incomplete information pertaining to our operational definition of working hours. A final total of 319 claims were selected for analysis according to our inclusion and exclusion criteria. The information was blinded using codes without private identifiers for confidentiality. All participants had signed informed consent forms regarding the sharing of data prior to submitting their claims.
Methods
Information recorded in each claim includes age, sex, type of CVD, survival, any predisposing chronic disease such as hypertension, diabetes, or dyslipidemia, and whether the claim is related to an accident that occurred on duty. This information was classified into the following three groups: no disease, disease without medical care, and predisposed to disease with medical care. Occupations were classified as blue collar, white collar, and other, which included transportation and maintenance workers in the manufacturing industry. Factory size was classified as follows: fewer than 10, 10–49, 50–300, and over 300 full-time equivalent employees.
Statistical analysis
Descriptive analyses of socioeconomic characteristics and working conditions are presented in a Table 1 according to approval status. The χ2 method was used to test differences in the claims by the specified subjects for Approval and Disapproval, and the receiver operating curve (ROC) method was used to calculate and compare the discrimination in cases of long working hours predicting approval of WR-CVD. The gold standard for ROC was set as “Approval” with a test variable of “Working Hours” according to our operational definitions. The cutoff for the best discrimination was set to the analysis by the area under the curve (AUC) with 95% confidential intervals (CI). To examine the sensitivity and specificity of the cutoff, the true positive was set as the gold standard used in the ROC curve; the test positive was set as the point at which the AUC was highest on the ROC curve. The sensitivity, specificity, and AUC values with the 95% CI for the cutoff value were calculated.
Table 1. The general characteristics of subjects and comparison according to approval for the claim to the workers’ compensation about cerebro-cardiovascular disease (CVD).
| Characteristics | Total (N=319) | Disapproval (N=257) | Approval (N=62) | p-value2 | |
|---|---|---|---|---|---|
| Age | 0.165 | ||||
| –29 | 4 (1.3) 1 | 2 (0.8) | 2 (3.2) | ||
| 30–39 | 57 (17.9) | 47 (18.3) | 10 (16.1) | ||
| 40–49 | 128 (40.1) | 99 (38.5) | 29 (46.8) | ||
| 50–59 | 100 (31.3) | 81 (31.5) | 19 (30.6) | ||
| 60– | 30 (9.4) | 28 (10.9) | 2 (3.2) | ||
| Gender | 0.178 | ||||
| Male | 270 (84.6) | 214 (83.3) | 56 (90.3) | ||
| Female | 49 (15.4) | 43 (16.7) | 6 (9.7) | ||
| Disease entity | 0.094 | ||||
| ICH | 106 (33.2) | 87 (33.9) | 19 (30.6) | ||
| SAH | 71 (22.3) | 52 (20.2) | 19 (30.6) | ||
| Cerebral infarction | 60 (18.8) | 54 (21.0) | 6 (9.7) | ||
| AMI | 51 (16.0) | 42 (16.3) | 9 (14.5) | ||
| Others | 31 (9.7) | 22 (8.6) | 9 (14.5) | ||
| Survival | 0.094 | ||||
| Survival | 221 (69.3) | 189 (71.6) | 37 (59.7) | ||
| Death | 98 (30.7) | 73 (28.4) | 25 (40.3) | ||
| Predisposing disease | 0.503 | ||||
| Negative | 160 (50.2) | 126 (49.0) | 34 (54.8) | ||
| Positive,without medical care | 79 (24.8) | 63 (24.5) | 16 (25.8) | ||
| Positive, with medical care | 80 (25.1) | 68 (26.5) | 12 (19.4) | ||
| Accident at duty | 0.887 | ||||
| On duty | 193 (60.5) | 155 (60.3) | 38 (61.3) | ||
| Off duty | 126 (39.5) | 102 (39.7) | 24 (38.7) | ||
| Type of occupation | 0.957 | ||||
| Blue-collars | 202 (63.3) | 162 (63.0) | 40 (64.5) | ||
| White-collars | 83 (26.0) | 67 (26.1) | 16 (25.8) | ||
| Others | 34 (10.7) | 28 (10.9) | 6 (9.7) | ||
| Factory size (workers) | 0.002 | ||||
| 1–9 | 98 (30.7) | 90 (35.0) | 8 (12.9) | ||
| 10–49 | 130 (40.8) | 97 (37.7) | 33 (53.2) | ||
| 50–299 | 55 (17.2) | 39 (15.2) | 16 (25.8) | ||
| 300– | 36 (11.3) | 31 (12.1) | 5 (8.1) | ||
1 N (%), 2 χ2 test (p<0.05).
Results
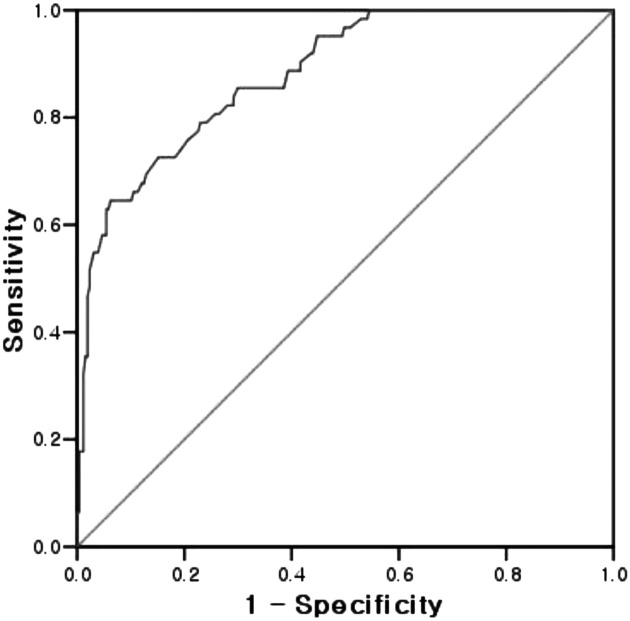
Of all CVD claims judged in 2010, 62 (19.4%) were approved and 257 were denied (Table 1). The 62 approved claimants were more likely to work in a factory with 10–49 FTEW (full-time equivalent workers; 53.2%) as compared to workers in a factory under 50 FTEW with Disapproval (37.7%). This trend showed a statistically significant difference (p<0.002). The most common characteristics among the approved claimants were the following: over age 40 (46.8%); male (90.3%); intracerebral hemorrhage (30.6%); survival case (59.7%); negative for a predisposing disease (54.8%); accident on duty (61.3%); and blue collar (64.5%); however, these were not significant. The ROC for “Working Hours” predicting approval of WR-CVD was calculated (Fig. 1). The cutoff point was 60.75 h (AUC=0.89, 95% CI [0.84–0.93]), which had a sensitivity rate of 65% and specificity of 94% (Table 2).
Fig. 1.
The ROC curve of working hours for 4 wk prior the accident on the approval of the claims for the workers’ compensation about cerebro-cardiovascular disease.
Table 2. The indeces of validity test of working hours before accident on the approval of work-related cerebro-cardiovascular disease (WR-CVD).
| Test variables | Cutoff | AUC | 95% CI | Sensitivity | Specificity |
|---|---|---|---|---|---|
| Average working hours for 4 weeks prior the onset of diseases | 60.75 | 0.88 | 0.84–0.93 | 0.65 | 0.94 |
Discussion
Working hours showed good discrimination with high specificity (94%) in predicting approval of WR-CVD when average weekly working hours exceeded 60.75 h for four weeks prior to the onset of CVD. The results from previous studies are consistent with our findings, and suggest that working hours in excess of 60 h per week are likely to be associated with WR-CVD7). Among incoming AMI (acute myocardial infarction) patients, individuals working over 60 h a week were 2.1 times more likely to have an AMI incident compared to those who worked less than 60 h per week8). In a case-controlled study conducted in Japan, working more than 65 h per week was associated with a 14-fold increased risk of incidents of AMI9). In one Korean cross-sectional study, workers who worked more than 60 h per week on average were 33 times more likely to be approved for WR-CVD compared to those who worked 52–60 h10). Similar to the present study, an analysis of data from 203 compensated workers with WR-CVD in Japan revealed that in two-thirds of cases, working more than 60 h a week was noted as a main triggering factor related to the WR-CVD11).
The following results pertain to the mechanisms by which long working hours heighten the risk of WR-CVD. First, prolonged tension and stress arising from long working hours lead to the dysregulation of the hypothalamic-pituitary-adrenal axis and lead to a high level of sympathetic tone, which constitutes the stress response12). According to a survey of 223 white-collar workers in Japan, heart rate variability shown as sympathetic hyperactivity in workers working over 60 h per week and long commuting time showed a statistically significant positive associations respectively (F=5.7, p<0.01; F=3.6, p<0.05). Sympathetic hyperactivity is known to cause dysfunction of myocardium and cardiovascular disease; thus, commuting time and long working hours may be risk factors for cardiovascular disease13).
Working long hours also leads to a decrease in sleep duration. A survey of white-collar workers in Japan showed that the quantity of sleep was significantly associated with commuting time and the amount of overtime at work13). Sleep deficiency (below 5 h per night) or sleep disturbance was associated with the incidence of or hospital admission for CVD7, 14) and elevated blood pressure15), which is linked to strong risk factors of CVD. Poor sleep quality also showed statistically significant associations with sympathetic predominance in heart rate variability16). This can be seen in the results of recent studies7, 14) describing the adverse effect of sleep deprivation on cardiovascular disease.
Our findings confirm the contribution of long working hours to WR-CVD, as previously noted, and suggest a valid, practical cutoff. To the best of our knowledge following a literature review, this is the first study to investigate the validity of working hours as a proxy for chronic overload in WR-CVD with specificity and sensitivity. This can serve as both a great advantage and a great limitation of the present study. Long working hours play an important role in the concept of chronic overload, but this is a broad concept17) that also involves lack of physical activity, physical fatigue, and psychological stress. Further, the lack of consideration of risk factors, such as individual subjects’ medical susceptibility regarding chronic overload, is another limitation of this study. Although we found that 60.75 h per week is the cutoff with the highest specificity, some WR-CVD claims with fewer working hours have been approved. Considering this, it is clearly risky to presume that long working hours can fully explain chronic overload. Despite this limitation, as mentioned above, working hours can serve as an objective measurement, and the figures allow a quick and universal understanding of the risk. Therefore, in terms of assisting the Korean administrative system in its evaluation of claims through a judging panel’s majority vote, this is a very practical study that arose out of necessity given the requirements of the field. Therefore, the above limitation exists when these results are reversely applied in the litigation process; thus, judgments should be made on a case-by-case basis in consideration of other composite factors, rather than on an across-the-board application. Furthermore, even when working hours is selected as a surrogate indicator of chronic overload, the most epidemiologically appropriate method of examining the effect of working hours on claim approval would be a longitudinal epidemiological study, such as a cohort study. On the other hand, considering the ethical aspects of cardiovascular disease, it may be more appropriate the case-control study design to compare hours worked between studies using a group of control patients. A validity test such as ours cannot reveal epidemiological causal relationships such as temporal relationships or biological plausibility. Furthermore, individuals who work long hours rarely have the opportunity to visit healthcare centers because of their work schedule; as a result, their medical records may not accurately reflect their health status. Therefore, the present study carried out a retrospective analysis of peer-reviewed data for workers’ compensation insurance to avoid concerns about possible bias in hospital records. Moreover, this study is advantageous in that our analysis revealed validity scores considered as credible indicators regarding a cutoff of working hours in approving workers’ compensation claims. To maintain the advantage provided by this study, some disadvantages and prerequisites should be considered. First, the validity analysis and cutoff in this study held the true positive, which determines the accuracy of the analysis, and the gold standard as the standard for approval of workers’ compensation claims. Therefore, these results represent an analysis of appropriate indicators for the approval of workers’ compensation; it is inadvisable to extend this interpretation to risk factors or cutoffs for the occurrence or worsening of WR-CVD. For example, several factors could confound the sensitivity and specificity values in this analysis. A predisposing disease related to CVD could limit the approval of WR-CVD, thus increasing the risk of a false positive and lowering specificity. Even considering such limitations and prerequisites, the specificity suggested by these results was quite high. Because increasing specificity resulted in a much greater increased predictive value than sensitivity, high specificity was recommended as a confirmative test18). The decision to approve WR-CVD benefits incurs tremendous socioeconomic costs, including the indemnity cost of workers’ compensation. Thus, the specificity and positive predictive value of the predictor of these costs must be high, as shown in this study. Moreover, the importance of a gold standard in a validity study was noted19). The gold standard chosen here is the appropriate external true finding of WR-CVD; the decision of the WDAC would be the actual final decision and the countable value for WR-CVD. In addition, several factors could confound the sensitivity and specificity values. When disease prevalence is extremely low or severity is mild, the specificity value would increase20). However, in this study, the approval rate as a surrogate of the prevalence of WR-CVD was 19.4%, and death of the claimants occurred 30% of the time. This indicates that disease prevalence as analyzed here is not a situation of rare prevalence or mild severity of disease. Therefore, the specificity noted here is valid and not associated with a subject confounder.
Regardless of this study’s methodological strengths, there are still limitations associated with the subjects. In our study, all of the subjects were manual laborers. This differs greatly from those in previous similar studies of WR-CVD, as manual laborers are more likely to be exposed to physicochemical hazards related to CVD and strenuous activities known to be risk factors of CVD. This factor may be a confounder affecting the findings related to long working hours and CVD. However, claimants working in the manufacturing industry (22.6%) were the most common claimants in South Korea in 2010, and are thus representative of national data. Moreover, working hours in the manufacturing industry are strictly recorded and thus reliable for analysis. We used strict exclusion criteria with part-time workers who worked less than 30 h per week. The possible risks of part-time workers are reported to be elevated CVD risk21) and the bias known as the “healthy worker effect.” However, shift workers with a fixed shift were excluded. Shift work is reported as a risk factor for sleep deprivation through its hazardous effect on biorhythms22), but shift workers cannot unscheduled work extended hours due to the strict rotation of their shifts. The approval of WR-CVD was not associated with shift work23). Thus, the nature of our inclusion and exclusion criteria improved the internal consistency of our study.
There are other claimant attributes that can affect the approval of workers’ compensation, such as age, sex, type of disease23), survival, a predisposing disease, type of occupation, whether the worker was on duty24), and the size of the factory25). In our findings, the size of the factory was the only factor significantly associated with the approval of WR-CVD. In Korea, small manufacturing enterprises tend to require long working hours and are, in many cases, labor-intensive. According to official statistics from the Ministry of Employment and Labor, excess working hours in the manufacturing industry average 7.13 h per week, much more than the average 2.5 excess hours in the service industry5). Despite this fact, there were more enterprises with an FTEW less than 10 in the Disapproval group than in the Approval group. According to a review of data at the time of enrollment, the claimants at small enterprises did not show reliable data for working hours. Research results show that small enterprises, both in Korea and abroad, have considerable deficiencies in their recognition of and attitude toward issues of occupational safety and health. This may be associated with disapprovals through litigation at the WDAC. It is possible that research subject characteristics influenced the results. For example, in our research results, some WR-CVD cases were approved although their working hours were below the 60.75 h suggested as the cutoff in our study. Some of these cases may have been approved due to the presence of other clear WR-CVD risk factors. Further, relatively large workplaces tend to have well-constructed occupational safety and health control systems and evidentiary materials; therefore, risk factors such as acute stress or dealing with hazards at work may have been preferentially applied in the evaluation instead of long working hours. To maintain the validity of the study, we limited the subject group to be as homogenous as possible and preferentially utilized claim application data that could be objectively quantified and verified. However, the fact that we did not consider various confounding elements in the enrollment and data analysis stages could be considered another limitation of the study.
Conclusion
Despite the above limitations, the ROC analysis conducted as part of this study revealed an exact cutoff with the components of the validity study, specifically sensitivity and specificity. This is the first study with good discrimination and high specificity to provide values showing that long working hours could be a predictor of approval of WR-CVD. Furthermore, this cutoff point should be useful as evidence to support effective and consistent decisions regarding the origin (work-related or not) of the CVD.
Based on this, future research should collect sufficient data about weekly working hours prior to the onset of CVD in consideration of the work-related aspects of CVD.
References
- 1.Ministry of Employment and Labor (2010) Statics of Occupational Injuries and Diseases, 362, Ministry of Employment and Labor, Gwacheon.
- 2.Kim DS, Kang SK. (2010) Work-related cerebro-cardiovascular diseases in Korea. J Korean Med Sci 25, S105–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeong YH, Go SJ. (2004) Estimating socioeconomic costs of five major diseases. Korean J Public Finance 18, 77–104. [Google Scholar]
- 4.Virtanen M, Ferrie JE, Singh-Manoux A, Shipley MJ, Vahtera J, Marmot MG, Kivimaki M. (2010) Overtime work and incident coronary heart disease: the Whitehall II prospective cohort study. Eur Heart J 31, 1737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson C, Mhurchu CN, Scott D, Bennett D, Jamrozik K, Hankey G, Australasian Cooperative Research on Subarachnoid Hemorrhage Study Group (2003) Triggers of subarachnoid hemorrhage: role of physical exertion, smoking and alcohol in the Austrailian Cooperative Research on Subarachnoiod hemorrhage Study (ACROSS). Stroke 34, 1771–6. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Employment and Labor (2010) Average annual hours actually worked per person in employment. In: 2011 yearbook of employment and labor statistics, Ministry of employment and labor, 539, Ministry of Employment and Labor, Gwacheon.
- 7.Spurgeon A, Harrington JM, Cooper CL. (1997) Health and safety problems associated with long working hours: a review of the current position. Occup Environ Med 54, 367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu Y, Tanaka H, Fukuoka Heart Study Group (2002) Overtime work, insufficient sleep, and risk of non-fatal acute myocardial infarction in Japanese men. Occup Environ Med 59, 447–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fukuoka Y, Dracup K, Froelicher ES, Ohno M, Hirayama H, Shiina H. (2005) Do Japanese workers who experience an acute myocardial infarction believe their prolonged working hours are a cause? Int J Cardiol 100, 29–35. [DOI] [PubMed] [Google Scholar]
- 10.Kim IS, Ryu SC, Kim YH, Kwon YJ. (2012) Influencing factors in approving cerebrovascular and cardiovascular disease as work-related disease of workers’ in manufacturing sectors. Korean J Occup Environ Med 24, 158–266. [Google Scholar]
- 11.Uehata T. (1991) Long working hours and occupational stress-related cardiovascular attacks among middle-aged workers in Japan. J Hum Ergol (Tokyo) 20, 147–53. [PubMed] [Google Scholar]
- 12.McDougall SJ, Widdop RE, Lawrence AJ. (2005) Central autonomic integration of psychological stressors: focus on cardiovascular modulation. Auton Neurosci 123, 1–11. [DOI] [PubMed] [Google Scholar]
- 13.Kageyama T, Nishikido N, Kobayashi T, Kurokawa Y, Kaneko T, Kabuto M. (1998) Long commuting time, extensive overtime, and sympatho dominant state assessed in terms of short-term heart rate variability among male white-collar workers in the Tokyo Megalopolis. Ind Health 36, 209–17. [DOI] [PubMed] [Google Scholar]
- 14.Virtanen M, Ferrie JE, Gimeno D, Vahtera J, Elovainio M, Singh-Manoux A, Marmot MG, Kivimaki M. (2009) Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep 32, 737–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang H, Schnall PL, Jauregui M, Su TC, Baker D. (2006) Work hours and self-reported hypertension among working people in California. Hypertension 48, 744–50. [DOI] [PubMed] [Google Scholar]
- 16.Kageyama T, Nishikido N, Kobayashi T, Kurokawa Y, Kaneko T, Kabuto M. (1998) Self-reported sleep quality, job stress, and daytime autonomic activities assessed in terms of short-term heart rate variability among male white-collar workers. Ind Health 36, 263–72. [DOI] [PubMed] [Google Scholar]
- 17.von Thiele Schwarz U, Lindfors P, Lundberg U. (2008) Health-related effects of worksite interventions involving physical exercise and reduced work hours. Scand J Work Environ Health 34, 179–88. [DOI] [PubMed] [Google Scholar]
- 18.Morrison AS. (1985) Screening in Chronic Disease. Monographs in Epidemiology and Biostatistics, volume 7,142, Oxford University Press, New York. [Google Scholar]
- 19.Gordis L. (2004) Epidemiology, 3rd Ed., 75, Elsevier Saunders, Philadelphia. [Google Scholar]
- 20.Bobo JK, Lee NC, Thames SF. (2000) Findings from 752,081 clinical breast examinations reported to a national screening program from 1995 through 1998. J Natl Cancer Inst 92, 971–6. [DOI] [PubMed] [Google Scholar]
- 21.Sokejima S, Kagamimori S. (1998) Working hours as a risk factor for acute myocardial infarction in Japan: case-control study. BMJ 317, 775–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wolk R, Gami AS, Garcia-Touchard A, Somers VK. (2005) Sleep and cardiovascular disease. Curr Probl Cardiol 30, 625–62. [DOI] [PubMed] [Google Scholar]
- 23.Ryu SC, Kim IS, Lee JH, Kwon YJ. (2011) Factors in approving cerebrovascular and cardiovascular disease as work-related disease in chronic overworked workers in Seoul. Korean J Occup Environ Med 24, 379–86. [Google Scholar]
- 24.Won JU, Ha KW, Song JS, Roh J, Kim HR, Lee DH, Lee KH. (2003) Analysis of sufficient conditions in approving cerebrovascular and cardiovascular disease as occupational disease. Korean J Occup Environ Med 15, 52–60. [Google Scholar]
- 25.Ryoo JH, Ha EH, Kim SG, Kim JY, Kim YK, Lee EC, Yi CH, Son JS. (2007) Analysis of worker’s compensation claims for the cerebrovascular and cardiovascular diseases. Korean J Occup Environ Med 19, 38–46. [Google Scholar]