Abstract
The purpose of this study was to examine the effects of two 15-min naps on nurses who work at night in a three-shift system. Of the 15 nurses who were included as study subjects on a night shift, eight took two short naps (the Nap condition), and seven worked without taking a nap (the No-nap condition) during the night shift. We measured sublingual temperature and the bispectral index (BIS), obtained heart rate and heart rate variability measures from an electrocardiogram (ECG), and evaluated sleepiness and fatigue levels every hour using the Visual Analog Scale (VAS). Both subjective sleepiness and fatigue increased between 4:00 and 5:00, with no significant differences observed between the two groups. However, the low- to high-frequency ratio (LF/HF) in the Nap condition group was found to be significantly lower than in the No-nap condition group. Furthermore, a sudden, brief increase in HF values was observed in the No-nap condition group in the morning. The results of this study suggest that taking two short naps may effectively reduce tension and prevent a brief increase in HF values by suppressing sympathetic nervous activity in the morning.
Keywords: Two 15-min naps, Nurse, Sleepiness, Fatigue, Night shift work, Heart rate variability
Introduction
In Japan today, a variety of businesses, including medical care organizations, manufacturers, and service industries, provide 24-h services; our modern society would not function without night work. However, night or shift work disrupts regular life rhythms, posing a wide range of safety and health risks, such as increased fatigue and lack of rest1,2,3). In this context, it is essential to develop and implement measures to enhance the safety of night shift workers.
In particular, nurses work shifts because they are required to provide patients with around-the-clock health care services. In Japan, nurses work on a two- or three-shift system. According to the results of previous studies, nurses working a night shift often feel sleepy, fatigued and weighed down in the morning4, 5), which increases the risk of accidents, burnout, and turnover6). It has also been pointed out that car accident rates are high among night shift nurses on their way home7).
Humans have biological clocks that follow a circadian rhythm of approximately 24 h. The circadian rhythm may be seen in patterns of sleeping and waking8), secretion of hormones such as melatonin9, 10) and in body temperature8). Normally, patterns of sleeping and waking are synchronized with internal rhythms such as body temperature. People sleep during periods of low body temperature10) and are aroused and active during periods of high body temperature.
However, shift workers are forced to work with their patterns of sleeping and waking out of balance with their body temperature and hormonal rhythms, which poses a high risk to their health11). In addition to increased early morning sleepiness, fatigue, and decreased performance, the risk of cancer, high blood pressure, heart disease, and gastrointestinal disease can also increase as shift work continues12).
In recent years, napping has received attention as a method of reducing the bodily fatigue of night shift nurses and alleviating their sleepiness13, 14). A 15-min nap in the daytime is believed to effectively maintain arousal levels15, 16). Napping during a night shift is regarded as a feasible measure to reduce the burden on night shift nurses because it helps reduce the disruption of the regular sleep-wake rhythms of those who work in the daytime and sleep at night14, 17). Napping is also expected to reduce fatigue and sleepiness, and improve how the time during off-duty hours is spent. Previous studies have shown that napping for 60–120 min during the night shift is effective for reducing fatigue and sleepiness and maintaining performance4, 18). Japanese law stipulates that nurses working for more than 8 h must take at least a 60-min break, and most hospital nurses working on a three-shift system take a 60- to 75-min rest at night19). However, it is difficult for nurses to spend the entire break napping since the break must also include time for eating and providing care to patients. As a substitute for 60 min of napping, 40-min napping has been shown to improve performance20), and 30-min napping frequently resulted in improved awakening and alertness21, 22). Similarly, 20-min napping prevented sleepiness. Therefore, even napping ≤60 min may be considered effective for awakening, alertness, and sleepiness.
However, 40-min napping resulted in a feeling of sleepiness after awaking due to sleep inertia23). Hayashi et al.18) reported that a short daytime nap of <20 min is effective as a countermeasure against the post lunch dip. Moreover, napping for 15 min or more during the daytime results in the appearance of slow-wave sleep24), which causes sleep inertia and negatively impacts nighttime sleep. According to other studies, 30-min napping prevented sleepiness for 2 to 3 h21, 22). Similarly, 20-min napping to prevent sleepiness continued for only 1 to 2 h25, 26). It is considered difficult to prevent drowsiness and the sense of fatigue until 9:00, which is the usual end of a night shift. When taking a 15-min nap at 3:00, sleepiness increased 3 h after the nap27).
The present study aimed to measure any reduction in sleepiness and fatigue and any physiological changes resulting from short naps taken during night shifts, at 2:30 and 4:30, through a comparison with workers who did not take naps.
Methods
Participants and procedure
This study was conducted in three public general hospitals (300 to 800 beds, 200 to 400 nurses) in Okayama and Hiroshima Prefectures, Japan, between September and November 2009. Subjects comprised 15 female nurses working on general wards (mean age: 23.71 ± 1.88 yr). Measurements were taken hourly during the night shifts. Eight of the nurses napped (Nap condition) and seven took no nap (No-nap condition).
All subjects were single, and lived in dormitories, apartments, or with their families. Two nurses in the Nap condition group worked on the surgical ward and the other six on mixed wards. The No-nap condition group included one nurse working on the surgical ward, one on the orthopedics ward, and another five on mixed wards. The ratio of patients to nurses was 7:1 in each ward, and three to four nurses worked on each ward during night shifts.
All participants were healthy nurses who did not smoke or drink regularly or use drugs. Participants were asked directly to confirm whether or not they smoked, drank regularly, or used drugs when the study was explained to them, and the researchers confirmed that the participants did not smoke or drink or use drugs during the night shift.
All participants were given explanations concerning the details of this study, including the recording methods for subjective symptoms and physiological measures prior to the start of the study, and gave their written informed consent. This study was approved by the Ethics Board of Okayama University Graduate School of Health Sciences.
Shift schedules
Three hospitals that used a three-shift system were targeted. The shifts were categorized as follows: day (8:30–17:15 or 8:00–16:45); evening (16:00–0:45 or 16:30–1:15); night (0:00–8:45 or 0:30–9:15); and off. The day before the night shift started was counted as a day off at all hospitals. Nurses therefore worked seven to eight night shifts every month. The study was carried out on the first day of the night shift. Nurses were allowed to alternatively take a 60-min break between 1:00 and 6:00 in a resting room.
Nurses were allowed 60 min of break time, and were free to take it how they wanted, either all together or divided into shorter times. They were therefore able to take two separate naps.
Study design
The present study evaluated nurses working an 8-h night shift to examine the perceptions of sleepiness and fatigue and physiological indices by comparing two groups: one group of nurses who took two 15-min naps during the break time, and the other group consisting of nurses who did not. The nurses were randomly allocated to the two (Nap and No-nap condition) groups.
Measurements
A total of five dependent variables, which included physiological and subjective ratings, were monitored during all the night shifts.
Physiological measures
These included sublingual temperature and heart frequency (HR), heart rate variability (HRV) and body movement measures. The circadian rhythm of body temperature is one of the most common indicators of circadian rhythmicity28). Sublingual temperature was measured as an index of internal body temperature. The armpit is more readily affected by external factors such as sweat or room temperature, so body temperature measured from the armpit is more prone to error than temperature measured sublingually. Aural thermometers have low reliability, as it is not possible to confirm that the probe is pointing correctly at the tympanic membrane when the temperature is being taken25). The sublingual temperature was therefore selected as the index of body temperature. When a subject drinks either cold or warm water, the oral temperature takes approximately 20 min to return to its previous level29). Therefore, assuming that body temperature measurement takes 5 min, it was confirmed that subjects had not consumed anything for 15 min prior to the measurement. Using an oral thermometer (MC-509, Omron Inc., Kyoto, Japan), body (sublingual) temperature was measured hourly to examine changes in circadian modulation during night work. To gain insights into the effects of night shift work and the associated circadian-modulated changes on heart rate, simple measures of heart rate frequency were included for the duration of each shift. HRV measures were included so as to monitor the autonomic nervous system activity throughout each night shift30). Physical activity and posture were continuously recorded every 5 min in each group with an ambulatory monitor worn on the nurses’ waists, ActiMarker (EW4800, Panasonic Inc., Osaka, Japan). An ActiMarker was used to accurately quantify body movements during activities that required low to medium exertion. The ActiMarker is a compact, lightweight, and accurate physical activity monitor that was developed with the use of an algorithm for estimating physical activity from the standard deviation of 3-axis composite acceleration of body movements31).
Subjective measures
Sleepiness and Fatigue were assessed subjectively using the Visual Analog Scale (VAS)32). Participants rated their sleepiness and fatigue on a 100-mm line. The values ranged from 0 mm (not at all sleepy or tired) to 100 mm (extremely sleepy or tired).
Power spectral analysis
The ECG tracings were recorded using the HOLTREC RAC-T102 (Nihon Kohden Inc., Tokyo, Japan) and were analyzed using MemCalc for Windows (Global Medical Solutions, Inc., Sherman Oaks, CA, USA). Data were analyzed offline after analog-to-digital conversion of 250-Hz R-R waves. Irregularities in ECG recordings were excluded from analysis. Variability was measured as an indicator of autonomic nerve activity. For frequency domain analysis of R-R wave intervals, the percentage of low-frequency power (LF) was calculated as the power within the frequency range of 0.04 to 0.15 Hz, and the percent of high-frequency power (HF) was calculated as the power within the frequency range of 0.15 to 0.4 Hz. The LF/HF ratio represents the sympathetic to parasympathetic balance.
The bispectral index (BIS) monitor (A-2000; Covidien Inc., Dublin, Ireland) is a system used to measure sedation levels33). BIS measurement is taken using three to four dedicated electrodes attached to the forehead, and part of the cortical activity associated with level of consciousness is calculated on the basis of the frequency, amplitude, and interference of the electroencephalogram. This is continuously displayed as the BIS value. Some investigators recently analyzed changes in the BIS during natural sleep in adults and found that the BIS diminished considerably as sleep became deeper34, 35). The mean BIS values of coma, semicoma, stupor and drowsiness are 0.14 ± 0.23, 38.9 ± 18.0, 60.3 ± 14.5, and 73.6 ± 16.5, respectively36). BIS is often used as a tool to measure sleep37). Even though the BIS could never replace polysomnography (PSG) when a more precise determination of the stages of sleep is necessary, the BIS is easier to use and interpret, is less time consuming, and allows for continuous monitoring. Information was also collected regarding subjective assessment of sleep quality; all participants were asked immediately after the nap whether they felt they had slept properly.
Procedures
The researcher attached an electrocardiograph and an ActiMarker to subjects while explaining the measurement methods to them before they started to work. In addition, the BIS monitor was attached to the participants in the Nap group prior to the nap. Other measurement methods had been explained in advance, and the researcher confirmed them at the time of measurement. To reduce the stress on the nurses in each group as much as possible, the researcher instructed them to spend break time (including eating and drinking) in the same way as much as possible as they did on other night shift days. Subjects were requested to refrain from eating or drinking for 15 min before each hourly temperature measurement, and at each measurement researchers confirmed that participants had not had any food or drink.
The researcher also noted and recorded the time of awakening and amount of time spent napping the day before the night shift, break time during the night shift, and sleeping time in the daytime following the night shift.
No-nap condition
At hourly intervals, beginning at 0:00 or 0:30 and ending at 9:00, participants were required to complete a brief battery of scales (sleepiness and fatigue VAS). These measurements were taken at the nursing station, and each hourly measurement took 2–3 min. They were asked not to lie down or sleep during break time.
Nap condition
The general procedure for the Nap condition was similar to the No-nap condition, except that participants were allowed to have a nap for 30 min. This time included 5 min to go to the restroom, 5 min for attaching the BIS monitor, 15 min for sleeping, and 5 min for removal of the BIS monitor and checking sleepiness, etc. A nap was taken twice, beginning between 2:30 and 3:00 (first nap), and between 4:30 and 5:45 (second nap) in a resting room. The nap opportunity was set at 30 min for two reasons. First, this duration fits within current employee break restrictions. Second, available data on nap efficacy suggest benefits for greater alertness from naps of 15-min duration25). It was expected that a 30-min break time would allow 15 min of sleep to be achieved, with time for normal sleep onset processes. There were three to four nurses on each ward who took turns to nap or take a break.
To take either their naps or their breaks, participants were able to use a resting room in an isolated section of the hospital, away from patient rooms and staff activity, but less than 10 m from the nurse’s station. Noise levels were minimal and naps were taken on a mattress on the floor of the room, with ample linen for participants’ comfort. During this nap break, participants were connected to a portable BIS monitor to record their sleep activity.
Participants were awakened by the researcher 15 min after the nap started. After the nap, at least 10 min was allowed for a break before the participant returned to work.
Statistical analysis
To ensure validity of the comparisons between the Nap condition and No nap condition, the first step of the analysis compared participants’ age, hours of sleep before the night shift, break time during the night shift, and hours of daytime sleep after the night shift.
Values are shown as mean ± SD or SE of mean unless otherwise noted. In analyses of napping time before work, break time, and sleep time in the daytime, the Mann-Whitney U test was conducted.
In analyses of body temperature, sense of fatigue, and subjective evaluation of sleepiness (measured using the VAS), the Shapiro-Wilk (normality) test was first conducted to identify differences in the conditions for napping from the start of work (0:00 or 0:30) to 9:00. Differences were noted in body temperature and sleepiness (VAS), and the Friedman test was carried out following determination of the ranges of data with significant differences using the Bonferroni post-hoc test to compare the conditions for napping. For multiple comparisons with the data before work, the Wilcoxon signed-rank test was conducted. The Mann-Whitney U test was used to compare factors at every hour between the two groups. No marked difference was noted between the two groups in the sense of fatigue (VAS); therefore, a two-way repeated-measures analysis of variance (ANOVA) was performed (with taking or not taking a nap and data range as factors). A one-way repeated-measures ANOVA (timing of nap during the shift as the factor) was conducted to examine changes to each of the conditions over time, and the Bonferroni post-hoc test was used for multiple comparisons with the data before work. To compare the two groups hourly, a t-test was used.
The Shapiro-Wilk (normality) test was conducted to compare HF, LF/HF, heart rate (HR), and level of activity at every hour between the two groups. Marked differences were noted and the Mann-Whitney U test was carried out.
Using the Pearson product-moment correlation coefficient, correlations between factors, including the start time, level of activity, sleepiness, sense of fatigue, LF/HF, and HR were examined.
Analyses were carried out using SPSS 16.0 J for Windows (SPSS, Tokyo, Japan), with significance set at 5% (two-sided).
Results
In comparing resting time, no significant difference was identified between the two groups (Table 1). All participants took a nap between the afternoon and the start of the night shift, with six participants in the Nap group and four in the No-nap group having more than 3 h sleep before the night shift. During the night shift, three participants in the Nap group and four in the No-nap group had a meal, consisting of a small amount of bread or rice, during the time after the fifth hourly measurement and 5 h 45 min. Three nurses from each group drank one cup of coffee during the shift. Of the three nurses who drank coffee, two drank it at 2:00 and one drank it at 4:00. One of the nurses who drank coffee at 2:00 and the nurse who drank it at 4:00 did not nap at all. The remaining nurse who drank coffee at 2:00 slept during both nap times. The relationship between coffee and sleep was not investigated in the present study.
Table 1. Age and status of napping before, during, and after work.
| Variable | Group |
p-value | |
|---|---|---|---|
| No nap (n=7) | Nap (n=8) | ||
| Age (yr) | 23.71 (1.88) | 23.00 (0.92) | 0.46 |
| Nap time before night shift (h) | 2.07 (1.17) | 3.71 (2.33) | 0.30 |
| Nap time while on night shift (min) | 61.88 (5.30) | 60.00 (15.00) | 0.88 |
| Sleep time during the day following a night shift (h) | 3.28 (1.21) | 3.13 (1.66) | 0.95 |
Values are expressed as means (SD) in each category. Differences were evaluated by the Mann-Whitney U test.
The sleep stage while napping was determined based on BIS monitor measurements. The mean BIS values at 2:30 and 4:30 were 90.3 ± 4.60, 81.1 ± 13.1, respectively. The mean BIS values from the first and second nap indicated that sleep was deeper during the second nap, but the difference was not significant.
In the nap at 2:00, which was the first nap, five participants had mean BIS value ≥90 and three participants had mean BIS value <90. Of the five people with BIS ≥90, one reported dozing and the other four reported that they could not sleep. Of the three participants with BIS value ≤90, one reported sleeping and the other two reported that they could not sleep. In the second nap starting from 4:30 onward, four participants with BIS ≥90 reported they could not sleep, and of the four participants with BIS <90, two reported they were able to sleep and two responded “I slept well and dreamed.” Seven of the eight nurses felt they could not sleep well and that napping did not reduce sleepiness or fatigue. Their comments after napping included: “I could not have sufficient sleep”, “It did not reduce sleepiness”, and “I felt better by just lying down”. The other nurse felt that the second nap was effective: “Although I had never slept on a break during work, I was able to take a nap for 15 min during this time. Thanks to that, I did not feel sleepy until the end of work”.
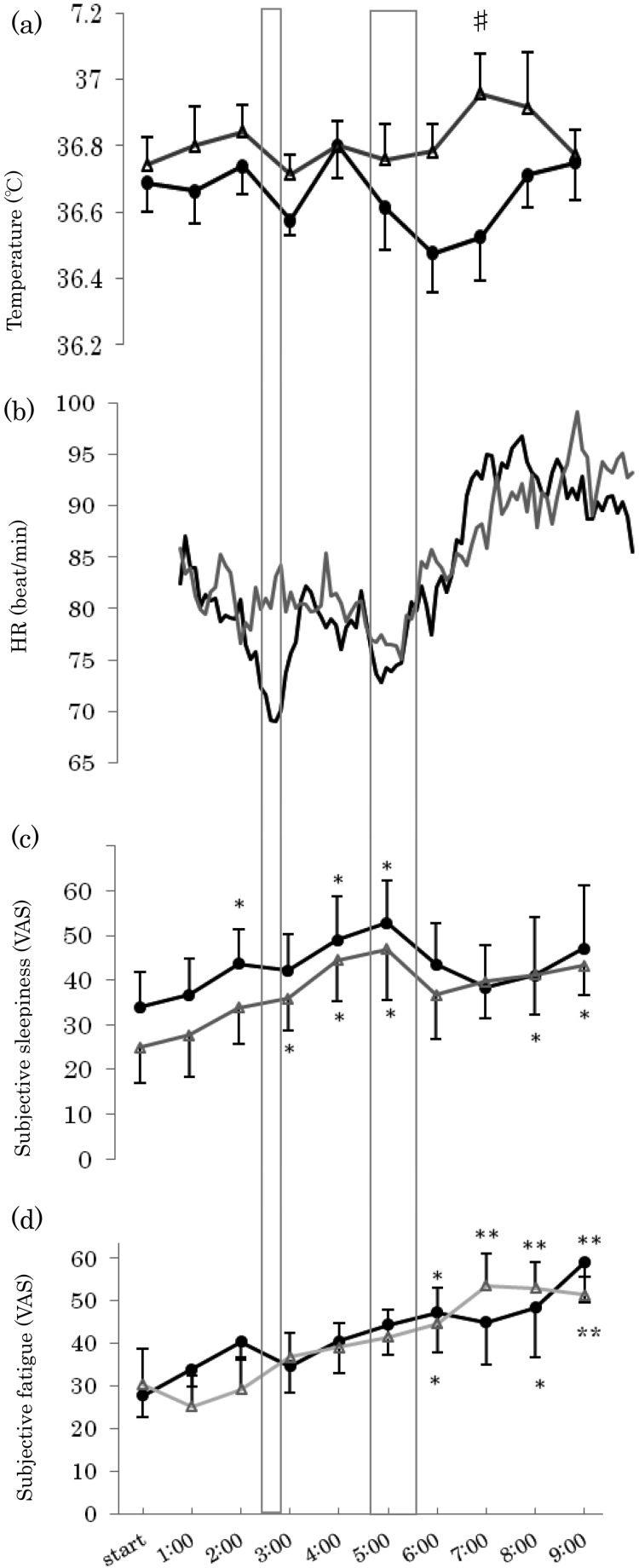
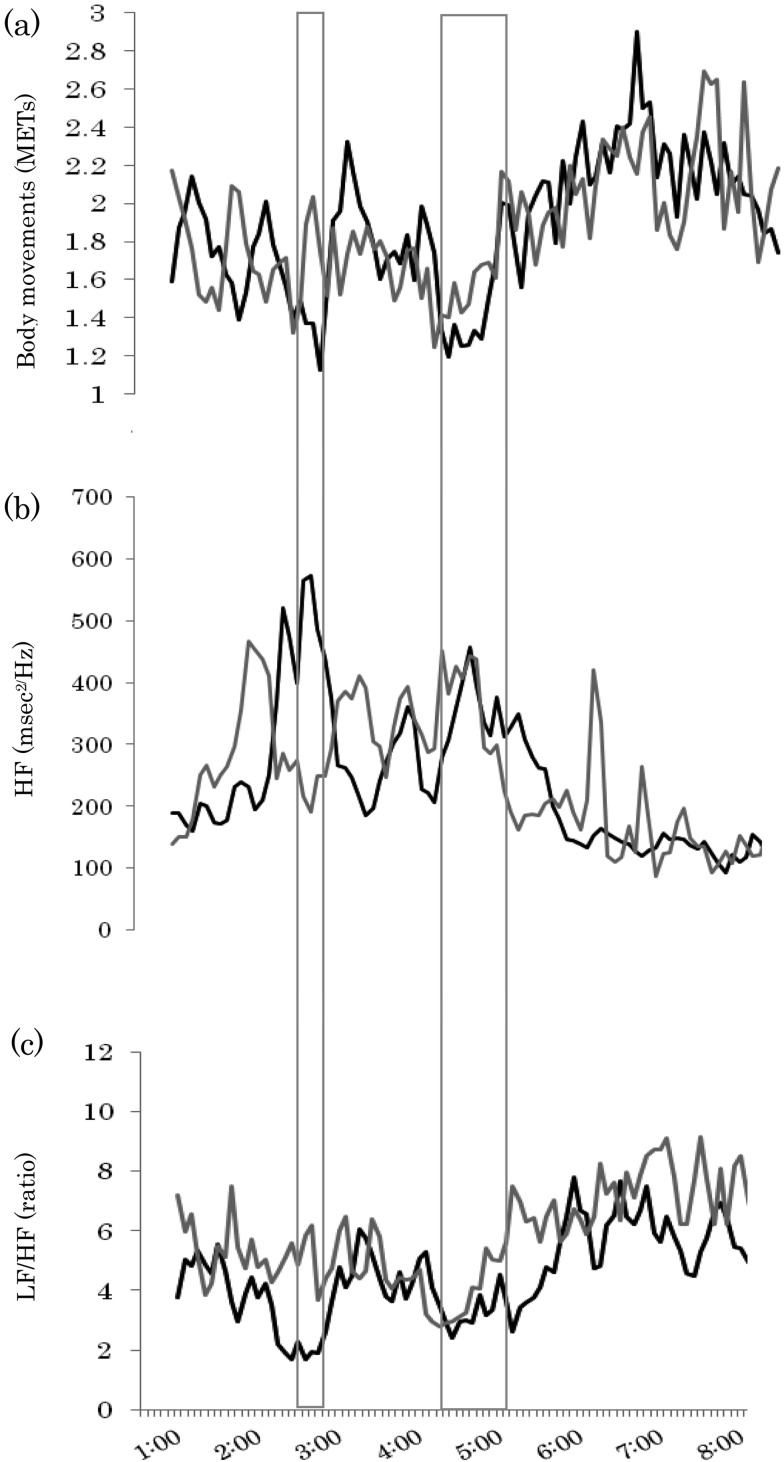
Regarding subjective sleepiness, fatigue, and physical activity (Fig. 1), no significant differences were observed; in both groups, sleepiness increased most markedly at 4:00 to 5:00, and fatigue after 6:00. Furthermore, as a measure of cardiac autonomic function, changes in the HF occasionally increased to 200 m sec2/Hz after 6:00 in the No-nap condition group, while remaining almost stable in the range from 100 to 150 m sec2/Hz in the Nap condition group (Fig. 2).
Fig. 1.
Mean ± SE hourly values for (a) Changes in temperature, (b) Changes in heart rate, (c) Subjective sleepiness, and (d) Subjective fatigue. (·), Nap condition; (△), No-nap condition. Significance was plotted compared with baseline values for nap and no-nap in all 4 graphs. (**: p<0.01;*: p<0.05). Significance was plotted compared with the No-nap condition in all graphs. (#: p<0.05). The Nap condition was between 2:30 and 3:00 (first nap), and between 4:30 and 5:45 (second nap).
Fig. 2.
Mean hourly values for (a) body movements, (b) Changes in HF, (c) Changes in LF/HF, (−), Nap condition; (−), No-nap condition. The Nap condition was between 2:30 and 3:00 (first nap), and between 4:30 and 5:45 (second nap).
On correlation analysis, no correlation was observed between the time and sleepiness and fatigue after 6:00 in either group. In contrast, the LF/HF, HR, and activity level significantly decreased in the Nap condition group, while the HR increased, and the activity level decreased in the No-nap condition group. The activity level decreased with time in both groups, and showed a positive correlation with the LF/HF and HR in the Nap condition group after 6:00.
In short, with a decrease in the activity level in the morning, the LF/HF and HR similarly decreased in the Nap condition group. On the other hand, the LF/HF showed a negative correlation with the activity level in the No-nap condition group, without being correlated with the HR; in other words, while the activity level gradually decreased after 6:00, the LF/HF increased, and HR was not affected by the activity level (Table 2).
Table 2. Correlations among the time (6:00 to 9:00), level of activity, sleepiness, and fatigue.
| Sleepiness | Sense of fatigue | LF/HF | HR | Level of activity | ||
|---|---|---|---|---|---|---|
| Time (6:00 to 9:00) | Nap | r=0.049 n.s. | r=0.157 n.s | r=–0.565** | r=–0.759*** | r=–0.696*** |
| No nap | r=0.112 n.s. | r=0.129 n.s. | r=0.007 n.s. | r=0.537** | r=–0.209 n.s. | |
| Level of activity | Nap | r=–0.155 n.s | r=–0.039 n.s. | r=0.589*** | r=0.594** | – |
| No nap | r=–0.063 n.s. | r=0.069 n.s. | r=–0.560*** | r=0.315 n.s. | – | |
*: p<0.05, **: p<0.01, ***: p<0.001. n.s.: not significant, r: correlation coefficient.
Furthermore, the body temperature and LF/HF were lower in the Nap group than in the No-nap condition group after 6:00 (Table 3).
Table 3. Comparison of sleepiness, fatigue, and autonomic nervous activity between the two groups (6:00 to 9:00).
| Variable | Group |
p-value | |
|---|---|---|---|
| Nap | No nap | ||
| Temperature (°C) | 36.62 (0.34) | 36.86 (0.30) | 0.02 |
| HR (beat/min) | 92.01 (9.83) | 92.18 (9.12) | 0.28 |
| Sleepiness (VAS) | 42.53 (31.64) | 40.21 (21.42) | 0.68 |
| Fatigue (VAS) | 49.91 (27.87) | 50.68 (17.26) | 0.9 |
| HF (msec2/Hz) | 135.76 (102.70) | 157.84 (262.48) | 0.07 |
| LF/HF (ratio) | 5.83 (3.21) | 7.44 (3.37) | <0.001 |
| Physical activity (mets) | 2.21 (0.55) | 2.16 (0.56) | 0.13 |
Mean (SD), Fatigue (VAS) was examined by performing a t-test, and the other items by conducting a Mann-Whitney U test.
Discussion
The purpose of the present study was to clarify the effects of taking two short naps during the night shift. Although napping for 15 min at 2:30 and during the period from 4:30 to 5:45 during the night shift was not shown to decrease subjective sleepiness or fatigue, HF/LF in the Nap condition group was significantly lower than in the No-nap condition group. Furthermore, a sudden, brief increase in HF values was observed in the No-nap condition group in the morning.
Most participants did not recognize sleep, although the BIS monitor showed data indicating deeper sleep during the second nap compared with the first one. Sleepiness fluctuates during the course of a day, and the main causes of this fluctuation are circadian rhythms and continued prolongation of the waking time until sleep38).
The body temperature decreased after each nap. In general, one sleep cycle lasts 90 to 120 min39), and it has been reported that the body temperature decreases with sleep40, 41). With regard to the relationship between changes in body temperature and sleepiness, there is a positive correlation between the time of most intense sleepiness and the time when deep body temperature shows its maximum reduction10, 42). As body temperature was low at 3:00 in both the Nap and No-nap groups, this reduction could not have been the result of taking a nap and so was likely to have reflected circadian rhythms and be due to reduced body movement. However, while body temperature in the No-nap group increased toward morning, in the Nap group it was at its lowest between 6:00 and 7:00, and at 7:00 the difference between the two groups was significant. Thus, during the first nap, the body temperature decreased and the nurses were readily able to sleep due to the effects of circadian rhythm and reduced body movement43). During the second nap, body temperature was probably lower due to the effect of the first nap. It may be conjectured that in both the first and the second naps, the reduced body temperature resulted in increased sleepiness, thus facilitating sleep. Sleepiness increases with prolongation of the waking time44), and subjects’ inability to sleep during the first nap may have been due to the effects of taking a nap before the shift. Furthermore, a likely reason for deeper sleep during the second nap than the first was that subjects chose by themselves the time for the nap that suited them18).
While previous studies recommended taking a 120-min nap, the present study found that similar effects were obtained by taking short, 15-min naps. Because the night shift nurses remained awake for a longer period of time to work during the night-time, sleep latency might be shortened45), and the condition during a 15-min nap may have become similar to that during sleep despite its shortness, leading to a decrease in body temperature. Generally, the level of arousal falls when body temperature decreases, but in the present study the increased level of activity in the morning from 6:00 onward was not accompanied by increased sleepiness. When seen from changes in HF as well, no decrease was found in the level of arousal. It therefore appears that while the second nap contributed to the noticeable decrease in body temperature, it did not have any effect on the increase in sleepiness.
Influences on subjective sleepiness and fatigue
In both the Nap and No-nap condition groups, fatigue increased after 6:00. A previous study reported that in a 16-h night shift, there was no difference between the level of fatigue at the end of the shift as a result of a nap of 120 min or less and a nap of 120 min or more during the shift46). Similarly, it has also been reported that with naps, a difference in fatigue was found as a result of the timing of when the nap was taken rather than the length of the nap, and that a later nap may be expected to reduce fatigue47). It has also been reported that napping for 40 min at 3:00 in a 12-h night shift reduced fatigue20). In the present study, no differences in fatigue were found after multiple naps, suggesting that it may be difficult to reduce fatigue by increasing the number of naps during a night shift. In order to reduce fatigue, it is probably necessary to ensure that the nap starts in the second half of the night shift, and that the nap is at least 40 min rather than 15 min.
Regarding subjective sleepiness, this increased most markedly between 4:00 to 5:00, and decreased after 6:00, when the activity level increased in both groups. While no differences in subjective sleepiness were observed between the groups, the HF, an objective index of sleepiness or parasympathetic activity, was stable in the morning in the Nap condition group, suggesting that the waking level was maintained. On the other hand, in the No-nap condition group, the parasympathetic activity level occasionally increased after 6:00, indicating an increase in HF values. In previous studies, subjective and objective sleepiness were empirically differentiated, and subjects were electroencephalographically shown to be sleepy when working without taking a nap48). Similar results were also obtained in the present study, suggesting occasional brief increase in HF values in participants who did not have a nap during a night shift. Nurses are often at their busiest after 6:00, when they tend to patients who are waking up, and they need to be able to accurately judge their own condition at this time. As shown in this study, The HF occasionally increases with such a rise in the activity level (Fig. 2). The increase in patient care in the early morning may be accompanied by an increase in sleepiness that goes unnoticed, which is a potential cause of occupational injuries or errors49,50,51).
Although the level of activity could not be strictly controlled for the Nap condition group or the No-nap condition group in the present study, the results of the present study show that taking a 15-min nap twice—at 2:30 and between 4:30 and 5:45, when the levels of sleepiness and fatigue would usually increase—may prevent the sense of fatigue until 9:00 or the end of the shift.
Previous studies have reported that nurses who took a nap on a night shift can spend more time for other activities the following day because they would not have to sleep long in the daytime40, 52,53,54). However, in the present study, no marked differences were noted in sleep times in the daytime or in the perceptions of fatigue between the Nap and No-nap condition groups. Taking a 15-min nap twice during the night shift did not increase waking hours during the day following a night shift or reduce the sense of fatigue, and there was no increase in the time that could be spent for other domestic activities.
Stress-reducing effects
The LF/HF values were significantly lower in the Nap than in the No-nap condition group at 6:00 to 9:00. Because the LF/HF has been reported to represent changes in the sympathetic nerve activity of the autonomic nervous system as a stress index55), the stress level may have been lower in the former than in the latter. Taking a nap can be effective in reducing stress56), and the results of the present study appear to be consistent with this. In night shift nurses who remain awake for a long period of time to work, sleepiness and fatigue increase, and their stress levels also gradually rise with an increase in the amount of work around the end of their shifts57). If such a stressful situation is prolonged, chronic fatigue may develop. The results of the present study suggest that it may also be effective to take two short-term naps to reduce such stress in the morning. The main reason for reduction in stress would be the effect of the nap itself, but also being away from the tense workplace, even for just a short while, would be relaxing. Also, it may be conjectured that stress levels decrease because napping provides an opportunity to reduce sleep pressure58).
Findings regarding nursing care work
In the present study, only one of the eight nurses subjectively reported benefits for greater alertness from napping. This was presumably because most of the subjects did not have the habit of napping, let alone taking a 15-min nap twice per night. By continuing the habit of taking a short nap, the effects of napping could be further increased. For night shift nurses to take turns taking a nap twice per night or more, it is necessary to address the issue of the workplace as a whole, in addition to the effort by individual nurses. As some of the nurses who could not sleep well while napping commented: “Just lying down for a while, I felt better”, simply lying on a bed during break time on a night shift to stretch the arms and legs and relax the muscles is expected to reduce fatigue59). Although 120 min of napping is recommended, taking a 15-min nap twice should be effective as well if break time is 60 min at a time. If this is established as a way of spending break time, it will help prevent medical malpractice and chronic fatigue, and help nurses to maintain their health and improve medical safety.
The present study had several limitations. First, the study included only a small number of participants. It is necessary to conduct further studies involving a larger number of subjects in order to validate the results. Second, measurements of brain waves using polysomnography were not conducted in this study, and the sleep stage of the subjects during their naps was not clearly determined. Third, the start time of napping varied widely between 4:30 and 5:45 (more than 1 h). It is almost impossible for all nurses to take a nap at the same time in clinical practice. Fourth, the start time and the length of naps taken before the night shift affect sleepiness and fatigue during the shift, but this could not be standardized. Finally, although the level of activity was measured, the sense of mental fatigue that nurses must have felt while performing handover and other tasks during busy hours in the morning was not determined. Further studies using a combination of critical flicker fusion frequency (CFF) and questionnaires to measure fatigue subjectively and objectively are needed in order to clarify the relationship of fatigue to sleepiness.
Acknowledgments
This work was supported by Grants-in-Aid for Scientific Research (20890140 and 22390409) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
References
- 1.McVicar A. (2003) Workplace stress in nursing-a literature review. J Adv Nurs 44, 633–42. [DOI] [PubMed] [Google Scholar]
- 2.Josten EJ, Ng-A-Tham JE, Thierry H. (2003) The effects of extended workdays on fatigue, health, performance and satisfaction in nursing. J Adv Nurs 44, 643–52. [DOI] [PubMed] [Google Scholar]
- 3.Ruggerio JS. (2003) Correlates of fatigue in critical care nurses. Res Nurs Health 44, 1003–11. [DOI] [PubMed] [Google Scholar]
- 4.Fukuda H, Takahashi M, Airto H. (1999) Nurses’ workload associated with 16-h night shifts on the 2-shift system-Comparison with the 3-shift system. Psychiatry Clin Neurosci 53, 219–21. [DOI] [PubMed] [Google Scholar]
- 5.Oriyama S, Miyakoshi Y, Kobayashi T. (2011) Influence of night-shift work on nurses: changes in activity, sleepiness, fatigue and physiological indices during night shifts. J Jpn Soc Healthc Adm 48, 147–56 (in Japanese with English abstract). [Google Scholar]
- 6.Åkerstedt T, Kecklund G. (2011) Shift work, severe sleepiness and safety. Ind Health 49, 141–2. [DOI] [PubMed] [Google Scholar]
- 7.Scott LD, Hwang WT, Rogers AE, Nysse T, Dean GE, Dinges DF. (2007) The relationship between nurse work schedules, sleep duration, and drowsy driving. Sleep 30, 1801–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wever RA. (1979) The circadian system of man: Results of experiments under temporal isolation, Springer-Verlag, New York. [Google Scholar]
- 9.Gil EA, Aubert XL, Most EL, Beersma DG. (2013) Human circadian phase estimation from signals collected in ambulatory conditions using an autoregressive model. J Biol Rhythms 28, 152–63. [DOI] [PubMed] [Google Scholar]
- 10.Gilbert SS, Van den Heuvel CJ, Dawson D. (1999) Daytime melatonin and temazepam in young adult humans: equivalent effects on sleep latency and body temperatures. J Physiol 514, 905–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harrington J. (2001) Health effects of shift work and extended hours of work. Occup Environ Med 58, 68–72. [Google Scholar]
- 12.Kim HI, Jung SA, Choi JY, Kim SE, Jung HK, Shim KN, Yoo K. (2013) Impact of shiftwork on irritable bowel syndrome and functional dyspepsia. J Korean Med Sci 28, 431–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fuller TP, Brain EI. (2010) Shift workers give sleep short shrift. Am J Nurs 110, 28–30. [DOI] [PubMed] [Google Scholar]
- 14.Takeyama H, Kubo T, Itani T. (2005) The nighttime nap strategies for improving night shift work in workplace. Ind Health 43, 24–9. [DOI] [PubMed] [Google Scholar]
- 15.Fushimi A, Hayashi M. (2008) Pattern of slow-wave sleep in afternoon naps. Sleep Biol Rhythms 6, 187–9. [Google Scholar]
- 16.Hayashi M, Motoyoshi N, Hori T. (2005) Recupetative power of a short daytime nap with or without stage 2 sleep. Sleep 28, 829–36. [PubMed] [Google Scholar]
- 17.Minors DS, Waterhouse JM. (1981) Anchor sleep as a synchronizer of rhythms on abnormal routines. Int J Chronobiol 7, 165–88. [PubMed] [Google Scholar]
- 18.Davy J, Göbel M. (2013) The effects of a self-selected nap opportunity on the psychophysiological, performance and subjective measures during a simulated industrial night shift regimen. Ergonomics 56, 220–34. [DOI] [PubMed] [Google Scholar]
- 19.Japanese Nursing Association (2010) Survey on the Demand and supply of hospital nurses, http://www.nurse.or.jp/nursing/practice/shuroanzen/jikan/pdf/02_05_09.pdf. Accessed January 28, 2013 (in Japanese).
- 20.Smith-Coggins R, Howard SK, Mac DT, Wang C, Kwan S, Rosekind MR, Sowb Y, Balise R, Levis J, Gaba DM. (2006) Improving alertness and performance in emergency department physicians and nurses-the use of planned naps. Ann Emerg Med 48, 596–604. [DOI] [PubMed] [Google Scholar]
- 21.Smith S, Kilby S, Jorgensen G, Douglas J. (2007) Napping and nightshift work-Effects of a short nap on psychomotor vigilance and subjective sleepiness in health workers. Sleep Biol Rhythms 5, 117–25. [Google Scholar]
- 22.Tremaine R, Dorrian J, Lack L, Lovato N, Ferguson S, Zhou X, Roach G. (2010) The relationship between subjective and objective sleepiness and performance during a simulated night-shift with a nap countermeasure. Appl Ergon 42, 52–61. [DOI] [PubMed] [Google Scholar]
- 23.Naitoh P, Kelly T, Babkoff H. (1993) Sleep inertia-best time not to wake up? Chronobiol Int 10, 109–18. [DOI] [PubMed] [Google Scholar]
- 24.Fushimi A, Hayashi M. (2008) Length of nap and appearance pattern of slow wave sleep. Sleep Biol Rhythms 6, 187–89. [Google Scholar]
- 25.Purnell MT, Feyer AM, Herbison GP. (2002) The impact of a nap opportunity during the night shift on the performance and alertness of 12-h shift workers. J Sleep Res 11, 219–27. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi M, Kawamoto N, Hori T. (2006) The effects of a 20-min nocturnal nap on performance and sleepiness during the night. J Sleep Res 15 (Suppl 1), 131. [Google Scholar]
- 27.Oriyama S, Miyakoshi Y, Kobayashi T. (2008) Effective brief nap during the late-night shift by nurses working the 3-shift system. Journal of the Japan society for Healthcare Administration 45, 7–15 (in Japanese with English abstract). [Google Scholar]
- 28.Härmä M, Waterhouse J, Minors D, Knauth P. (1994) Effect of masking on circadian adjustment and interindividual differences on a rapidly rotating shift schedule. Scand J Work Environ Health 20, 55–61. [DOI] [PubMed] [Google Scholar]
- 29.Yamaguchi H, Mitani H, Wakabayashi N, Ohta M, Hirata M. (2002) A basic study on body temperature measurement(4): Influence on oral temperature by change of the mouth condition after drinking water. Bull Kobe C Jr Col Of Nursing 21, 65–72 (in Japanese). [Google Scholar]
- 30.Wehrens SM, Hampton SM, Skene DJ. (2012) Heart rate variability and endothelial function after sleep deprivation and recovery sleep among male shift and non-shift workers. Scand J Work Environ Health 38, 171–81. [DOI] [PubMed] [Google Scholar]
- 31.Mastumura Y, Yamamoto M, Kitado T, Nakamura H, Kidera K, Fujimoto S. (2008) High-accuracy physical activity monitor utilizing three-axis accelerometer. Panasonic Tech J 56, 60–6 (in Japanese with English abstract). [Google Scholar]
- 32.Monk TH. (1989) A visual analog scale technique to measure global vigor and affect. Psychol Res 27, 89–99. [DOI] [PubMed] [Google Scholar]
- 33.Jang SY, Park HG, Jung MK, Cho CM, Park SY, Jeon SW, Tak WY, Kweon YO, Kim SK, Jeon YH. (2012) Bispectral index monitoring as an adjunct to nurse-administered combined sedation during endoscopic retrograde cholangiopancreatography. World J Gastroenterol 18, 6284–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carozzi C, Rampil IJ. (2011) Bispectral Index for sleep screening-it is time to move on. Minerva Anestesiol 77, 485–7. [PubMed] [Google Scholar]
- 35.Benini F, Trapanotto M, Sartori S, Capretta A, Gobber D, Boniver C, Zacchello F. (2005) Analysis of the bispectral index during natural sleep in children. Anesth Analg 101, 641–4. [DOI] [PubMed] [Google Scholar]
- 36.Jung JY, Cho CB, Min BM. (2013) Bispectral index monitoring correlates with the level of consciousness in brain injured patients. Korean J Anesthesiol 64, 246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tung A, Lynch JP, Roizen MF. (2002) Use of the BIS monitor to detect onset of naturally occurring sleep. J Clin Monit Comput 17, 37–42. [DOI] [PubMed] [Google Scholar]
- 38.Richardson GS. (2005) The human circadian system in normal and disordered sleep. J Clin Psychiatry 66 (Suppl 9), 3–9. [PubMed] [Google Scholar]
- 39.Carskadon MA, Dement WC. (1980) Distribution of REM sleep on a 90 minute sleep-wake schedule. Sleep 2, 309–17. [PubMed] [Google Scholar]
- 40.Okamoto-Mizuno K, Yamashiro Y, Tanaka H, Komada Y, Mizuno K, Tamaki M, Kitado M, Inoue Y, Shirakawa S. (2008) Heart rate variability and body temperature during the sleep onset period. Sleep Biol Rhythms 6, 42–9. [Google Scholar]
- 41.Aschoff J. (1983) Circadian control of body temperature. J Therm Biol 8, 143–7. [Google Scholar]
- 42.Campbell SS, Broughton RJ. (1994) Rapid decline in body temperature before sleep: Fluffing the physiological pillow? Chronobiol Int 11, 126–31. [DOI] [PubMed] [Google Scholar]
- 43.Youngstedt SD. (2005) Effects of exercise on sleep. Clin Sports Med 24, 355–65. [DOI] [PubMed] [Google Scholar]
- 44.Goel N, Basner M, Rao H, Dinges DF. (2013) Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci 119, 155–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Signal TL, Gander PH, Anderson H, Brash S. (2009) Scheduled napping as a countermeasure to sleepiness in air traffic controllers. J Sleep Res 18, 11–9. [DOI] [PubMed] [Google Scholar]
- 46.Matsumoto S, Sasaki T, Sakita M, Naito K, Aoyagi N, Takahashi E, Sakai K. (2008) The effect of naps taken by hospital nurses during 16-hour nightshifts on their subjective fatigue feelings and subsequent sleeps. J Sci Labour 84, 25–9 (in Japanese with English abstract). [Google Scholar]
- 47.Kubo T, Takeyama H, Matsumoto S, Ebara T, Murata K, Tachi N, Itani T. (2007) Impact of nap length, map timing and sleep quality on sustaining early morning performance. Ind Health 45, 552–63. [DOI] [PubMed] [Google Scholar]
- 48.Chervin RD, Aldrich MS, Picket R, Guilleminault C. (1997) Comparison of the result of the Epworth sleepiness scale and the multiple sleep latency test. J Psychosom Res 42, 145–55. [DOI] [PubMed] [Google Scholar]
- 49.Lombardi DA, Folkard S, Willetts JL, Smith GS. (2010) Daily sleep, weekly working hours, and risk of work-related injury: US national health interview survey (2004–2008). Chronobiol Int 27, 1013–30. [DOI] [PubMed] [Google Scholar]
- 50.Swaen GM, Van Amelsvoort LG, Bultmann U, Kant IJ. (2003) Fatigue as a risk factor for being injured in an occupational accident: results from the Maastricht Cohort Study. Occup Environ Med 60 (Suppl 1), i88–i92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Trinkoff AM, Le R, Geiger-Brown J, Lipscomb J. (2007) Work schedule, needle use, and needlestick injures among registered nurses. Infect Control Hosp Epidemiol 28, 156–64. [DOI] [PubMed] [Google Scholar]
- 52.Ribeiro-Silva F, Rotenberg L, Soares RE, Pessanha J, Ferreira FL, Oliveira P, Silva-Costa A, Benedito-Siva AA. (2006) Sleep on the job partially compensates for sleep loss in night-shift nurses. Chronobiol Int 23, 1389–99. [DOI] [PubMed] [Google Scholar]
- 53.Matsumoto K, Harada M. (1994) The effect of nighttime naps on recovery from fatigue following night work. Ergonomics 37, 899–907. [DOI] [PubMed] [Google Scholar]
- 54.Rogers AS, Spencer MB, Stone BM, Nicholson AN. (1989) The influence of a 1h nap on performance overnight. Ergonomics 32, 1193–205. [DOI] [PubMed] [Google Scholar]
- 55.Collins SM, Karasek RA, Costas K. (2005) Job strain and autonomic indices of cardiovascular disease risk. Am J Ind Med 48, 182–93. [DOI] [PubMed] [Google Scholar]
- 56.Motohashi Y, Takano T. (1993) Effects of 24-hour shift work with nighttime napping on circadian rhythm characteristics in ambulance personnel. Chronobiol Int 10, 461–70. [DOI] [PubMed] [Google Scholar]
- 57.Ohashi Y, Tachi N, Niwa S, Sakuragi Y, Kouyama U, Suzumura H. (2010) Investigation of factors influencing fatigue in hospital nurses. J Jpn Soc Nurs Health Care 12, 20–9 (in Japanese with English abstract). [Google Scholar]
- 58.Sasaki T, Matsumoto S. (2001) A preliminary attempt on the evaluation of a nocturnal nap viewed from the sws-srem balance and progressive stage changes during daytime sleep. J Sci Labour 77, 131–46 (in Japanese with English abstract). [Google Scholar]
- 59.Ohashi Y. (2002) Encyclopedia Dictionary of Nursing, 2nd Ed., Gakken, Tokyo, 796–99 (in Japanese). [Google Scholar]