Summary
Cocaine-induced leukoencephalopathy is a rare neurological complication. It is most likely related to the substances used to adulterate the cocaine. Levamisole is one of the most common adulterants of cocaine and causes reversible leukoencephalopathy. Patients display severe neurological symptoms that resolve at termination of the exposure. MRI shows diffuse white matter involvement with sparing of the U fibers, without brain stem or cerebellar involvement. We describe the case of a woman with three neurologic episodes and remitting and recurrent brain white matter lesions.
Keywords: anterior reversible leukoencephalopathy, cocaine
Case Report
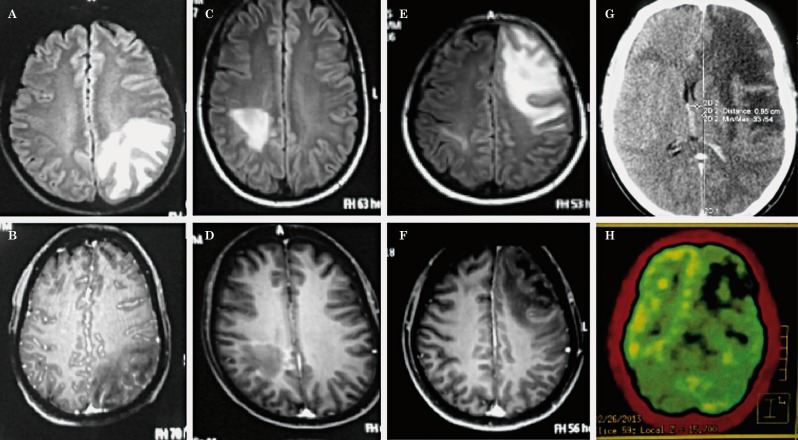
A 40-year old woman with chronic daily use of cocaine was admitted to the ER for acute onset of confusion, altered language and mild fever. At entry, her blood pressure was 110/70 mmHg, temperature was 38.5°C and she exhibited motor aphasia. The rest of the examination was normal. Laboratory tests were within normal limits and HIV was negative. A lumbar puncture showed leucocytes of 200 cells/mm3 (75% PMN, 25% MN), glucose of 85 mg/dl, proteins of 35 mg/dl, negative gram and fungal stains, and negative PCR for HSV-1 and 2 and Mycobacterium tuberculosis. Serum HIV and skin tuberculin tests were negative. T2 and FLAIR sequences of the brain MRI displayed areas of hyperintense signal in the white matter of the left parietal lobe (Figure 1A,B). The DWI/ADC sequences and resonance angiography were normal. Presumptive treatment for an incipient brain abscess was initiated with ceftriaxone, metronidazole and dexamethasone. A transesophageal echocardiogram was normal. ENT and dental evaluations did not reveal any focus of infection. The blood and CSF cultures taken at entry were negative. The patient recovered completely after two days. A follow-up lumbar puncture after ten days showed leucocytes of 10 cells/mm3 , glucose of 72 mg/dl and proteins of 17 mg/dl, but the MRI indicated only mild improvement of the lesion. Because she was asymptomatic, she was discharged after 14 days of IV antibiotics.
Ten days later she began experiencing sudden visual changes and weakness of the left arm. MRI showed resolution of the previous lesion but displayed a new one in the right frontal lobe (Figure 1C,D). She was readmitted and IV imipenem, linezolid and dexamethasone were begun. The patient recovered completely after a few days. Serum antibodies against Borrelia and Hystoplasma, anti-phospholipid and antinuclear antibodies were negative. A lung biopsy of a small nodule was negative for granulomas, stains and cultures. After one week she was discharged with the same IV treatment administered by a nurse at her home.
Seven days later she had a new episode consisting of motor aphasia. The patient was unable to talk, read or write. The MRI showed a third lesion in the left frontal lobe with resolution of the previous lesions (Figure 1E,F). The patient and her family refused a brain biopsy. A spinal MRI did not show spinal lesions consistent with autoimmune demyelinating disease. PET-CT (Figure 1G,H) failed to show lesions suggestive of lymphoma. Complete clinical recovery was achieved within two weeks. After the last episode she admitted she had consumed cocaine at home. After a year of follow-up she has not presented new episodes.
Figure 1.
Brain images per timeline. Fluid attenuated inversion recovery (FLAIR) and T1 with gadolinium MRI at entry (A,B), one week after the first discharge (C,D), ten days after the second discharge (E,F). G,H) CT and PET-CT at the same time as E (see text for description).
Discussion
Although cocaine use is often associated with stroke, white matter lesions similar to toxic or metabolic injury may also occur 1,3-5. Brain changes are best appreciated on FLAIR-MRI, and DWI restriction lesions are not observed 1. Unlike "chasing the dragon" or leukoencephalopathy associated with inhaled heroin, the frontal lobes are most affected, and the brainstem and cerebellum are spared 1,3.
We describe a patient with three consecutive episodes of white matter lesions associated with cocaine use. Despite displaying severe neurological symptoms at the onset of each episode, the patient's recovery was remarkably complete after a few days. PRES was excluded because there was no history of hypertensive crisis, and blood pressure was within normal values all of the time. The patient did not suffer from immune suppression, or present relevant risk factors to investigate a JC virus infection. Other forms of immune leukoencephalopathy such as multiple sclerosis, ADEM or Baló, systemic lupus erythematosus, Sjogën syndrome or antiphospholipid syndrome were considered, but the lack of periventricular or spinal lesions, and the absence of systemic data ruled them out.
Leukoencephalopathy in this case seems to be related to the adulterants obtained from the cocaine. In particular, levamisole has been implicated since its use is recent and it can be found in up to 65% of cocaine samples 3,6 and in urine of patients positive for cocaine 7. In addition, the medication has been directly associated with leukoencephalopathy 8-11. The pathology is believed to be similar to other spongiform encephalopathies, where fluid entrapment is found in small vacuoles within the myelin lamellae 1. The apparent progression of the brain images despite the steady clinical improvement is due to the expansion of such vacuoles 1. There is no general consensus on the treatment of toxic leukoencephalopathy. In our case, dexamethasone proved to be helpful. Extensive work-up may be deferred in patients with an unclear cause of leukoencephalopathy with a confirmation of the use of cocaine.
References
- 1.Bianco F, Iacovelli E, Tinelli E, et al. Recurrent leukoencephalopathy in a cocaine abuser. Neurotoxicology. 2011;32(4):410–412. doi: 10.1016/j.neuro.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Neiman J, Haapeniemi HM, Hillbom M. Neurological complications of drug abuse: pathophysiological mechanisms. Eur J Neurol. 2000;7(6):595–606. doi: 10.1046/j.1468-1331.2000.00045.x. [DOI] [PubMed] [Google Scholar]
- 3.Blanc PD, Chin C, Lynch KL. Multifocal inflammatory leukoencephalopathy associated with cocaine abuse: is levamisole responsible? Clin Toxicol (Phila) 2012;50(6):534–535. doi: 10.3109/15563650.2012.692794. [DOI] [PubMed] [Google Scholar]
- 4.Bartlett E, Mikulis D. Chasing “chasing the dragon” with MRI: leukoencephalopathy in drug abuse. Br J Radiol. 2005;78(935):997–1004. doi: 10.1259/bjr/61535842. [DOI] [PubMed] [Google Scholar]
- 5.Pericot-Niera I, Lopez-Pousa S, Lozano-Gallego M, et al. Acute disseminated encephalomyelitis associated to overdose cocaine. Med clin (Barc) 2007;128(3):119. doi: 10.1016/s0025-7753(07)72507-1. [DOI] [PubMed] [Google Scholar]
- 6.Larocque A, Hoffman RS. Levamisole in cocaine: unexpected news from an old acquaintance. Clin Toxicol (Phila) 2012;50(4):231–241. doi: 10.3109/15563650.2012.665455. [DOI] [PubMed] [Google Scholar]
- 7.Buchanan J, Heard K, Burbach C, et al. Prevalence of levamisole in urine toxicology screens positive for cocaine in an inner-city hospital. JAMA. 2011;305(16):1657–1658. doi: 10.1001/jama.2011.531. [DOI] [PubMed] [Google Scholar]
- 8.Buchanan JA, Lavonas EJ. Agranulocytosis and other consequences due to use of illicit cocaine contaminated with levamisole. Curr Opin Hematol. 2012;19(1):27–31. doi: 10.1097/MOH.0b013e32834da9ef. [DOI] [PubMed] [Google Scholar]
- 9.Anbarasan D, Campion P, Howard J. Drug-induced leukoencephalopathy presenting as catatonia. Gen Hosp Psychiatry. 2011;33(1):85.e1–3. doi: 10.1016/j.genhosppsych.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 10.Savarese DM, Gordon J, Smith TW, et al. Cerebral demyelination syndrome in a patient treated with 5-flourouracil and levamisole. The use of thallium SPECT imaging to assist in noninvasive diagnosis - A case report. Cancer. 1996;77(2):387–394. doi: 10.1002/(SICI)1097-0142(19960115)77:2<387::AID-CNCR23>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 11.Ryan A, Molloy FM, Farrell MA, et al. Fatal toxic leukoencephalopathy: clinical, radiological and necropsy findings in two patients. J Neurol Neurosurg Psychiatry. 2005;76(7):1014–1016. doi: 10.1136/jnnp.2004.047134. [DOI] [PMC free article] [PubMed] [Google Scholar]