Burns are one of the most devastating conditions encountered in medicine. The injury represents an assault on all aspects of the patient, from the physical to the psychological. It affects all ages, from babies to elderly people, and is a problem in both the developed and developing world. All of us have experienced the severe pain that even a small burn can bring. However the pain and distress caused by a large burn are not limited to the immediate event. The visible physical and the invisible psychological scars are long lasting and often lead to chronic disability. Burn injuries represent a diverse and varied challenge to medical and paramedical staff. Correct management requires a skilled multidisciplinary approach that addresses all the problems facing a burn patient.
This series provides an overview of the most important aspects of burn injuries for hospital and non-hospital healthcare workers.
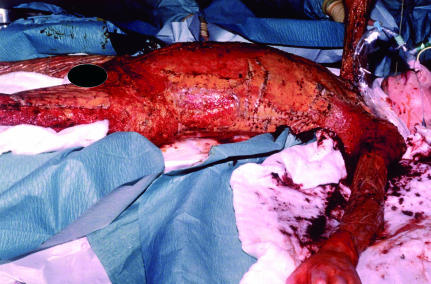
Figure 1.
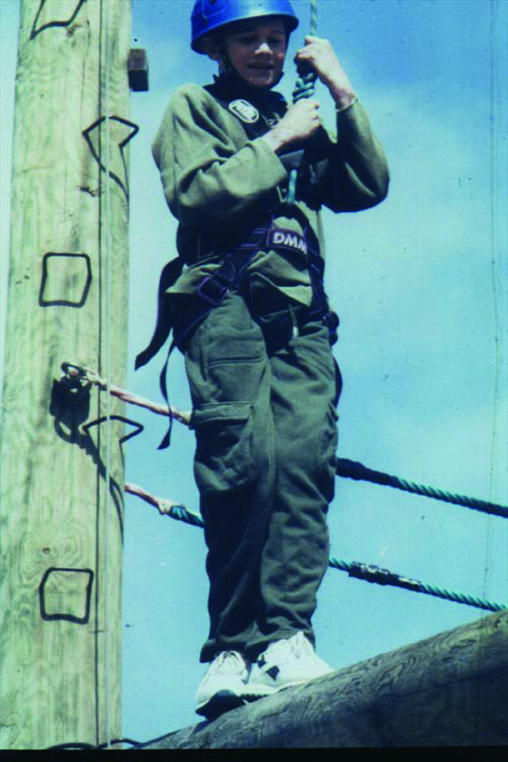
Top: Child with 70% full thickness burns, which required resuscitation, intensive care support, and extensive debridement and skin grafting. Left: The same child one year later at a burns camp, having made a good recovery. A reasonable outcome is possible even with severe burn injuries
How common are burns?
In the United Kingdom about 250 000 people are burnt each year. Of these, 175 000 attend accident and emergency departments, and 13 000 of these are admitted to hospital. Some 1000 patients have severe enough burns to warrant formal fluid resuscitation; half of these are children aged under 12 years. In an average year 300 burn deaths occur. These UK figures are representative of most of the developed world countries, although some, such as the United States, have a higher incidence.
Burns are also a major problem in the developing world. Over two million burn injuries are thought to occur each year in India (population 500 million), but this may be a substantial underestimate. Mortality in the developing world is much higher than in the developed world. For example, Nepal has about 1700 burn deaths a year for a population of 20 million, giving a death rate 17 times that of Britain.
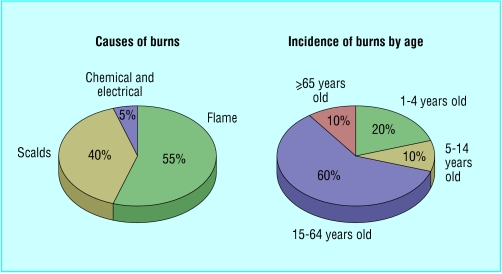
Figure 3.
Causes of burns (left) and incidence of burns by age (right)
What are the causes of burns?
Most burns are due to flame injuries. Burns due to scalds are the next most common. The most infrequent burns are those caused by electrocution and chemical injuries. The type of burns suffered is related to the type of patient injured. It is therefore useful to break down burn aetiology by patient groups as this reveals the varying causes of injury. In most groups there is a male predominance. The only exception is in elderly people, among whom more women are injured because of the preponderance of women in that population.
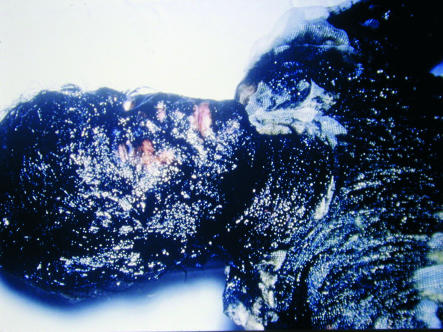
Figure 4.

Scald in young child caused by spilling hot liquid. Most of the burn is superficial, except for the patch on the shoulder, which required a skin graft and which healed well
Who gets burnt?
Young children—Children aged up to 4 years comprise 20% of all patients with burn injuries. Most injuries (70%) are scalds due to children spilling hot liquids or being exposed to hot bathing water. These mechanisms can lead to large area burns. Because of changes in the design and material of night clothing, flame burns are less common than they were. Boys are more likely to be injured, a reflection of the behavioural differences between boys and girls.
Older children and adolescents—10% of burns happen to children between the ages of 5 and 14. Teenagers are often injured from illicit activities involving accelerants, such as petrol, or electrocution.
Figure 5.
Burn incurred by an adolescent boy while inhaling butane gas. There was full thickness damage to the lower lip, which required debridement and extensive reconstruction
Working age—Most burns (> 60%) occur in patients aged 15-64. These are mainly due to flame burns, and up to a third are due to work related incidents.
Elderly people—Some 10% of burns occur in people aged over 65. Various effects of ageing (such as immobility, slowed reactions, and decreased dexterity) mean elderly people are at risk from scalds, contact burns, and flame burns.
Compromising factors—Burn victims' health is often compromised by some other factor, such as alcoholism, epilepsy, or chronic psychiatric or medical illness. All such problems need to be addressed when managing patients in order to speed recovery and prevent repetition of injury.
Care of a major burn injury
The main aims of burn care are to restore form, function, and feeling, and burn management can be divided up into seven phases—rescue, resuscitate, retrieve, resurface, rehabilitate, reconstruct, and review.
Table 1.
Aims of burn care
| Restore form—Return the damaged area to as close to normality as is possible |
| Restore function—Maximise patient's ability to perform pre-injury activities |
| Restore feeling—Enable psychological and emotional recovery |
Rescue—The aim is to get the individual away from the source of the injury and provide first aid. This is often done by non-professionals—friends, relatives, bystanders, etc.
Resuscitate—Immediate support must be provided for any failing organ system. This usually involves administering fluid to maintain the circulatory system but may also involve supporting the cardiac, renal, and respiratory systems.
Figure 6.
Bitumen burns to face in work related incident
Retrieve—After initial evacuation to an accident and emergency department, patients with serious burns may need transfer to a specialist burns unit for further care.
Resurface—The skin and tissues that have been damaged by the burn must be repaired. This can be achieved by various means, from simple dressings to aggressive surgical debridement and skin grafting.
Rehabilitate—This begins on the day a patient enters hospital and continues for years after he or she has left. The aim is to return patients, as far as is possible, to their pre-injury level of physical, emotional, and psychological wellbeing.
Reconstruct—The scarring that results from burns often leads to functional impairment that must be addressed. The operations needed to do this are often complex and may need repeating as a patient grows or the scars re-form.
Review—Burn patients, especially children, require regular review for many years so that problems can be identified early and solutions provided.
The complexity of the injury and the chronic nature of the sequelae of burns require an integrated multidisciplinary approach with long follow up. Only such management can lead to the best outcomes for burn patients.
Figure 7.
Contact burns in an elderly patient after a collapse and prolonged contact with a radiator. Treatment required excision and split skin grafting as well as investigation into the cause of the collapse
Prognostication in major burns
Determining whether someone will survive a severe burn injury is not simple but is important. Aggressive treatment for someone with a non-survivable injury is inhumane, and it is inappropriate not to treat a patient who has a severe but potentially survivable injury. Unfortunately, there is no exact way to predict who will survive a burn injury. Several formulae have been devised to estimate the risk of death after burn injury. None has been evaluated prospectively in large trials, however, and so they should be used only for audit purposes. It is also inappropriate to apply generic formulae to individuals. Each patient should be considered individually.
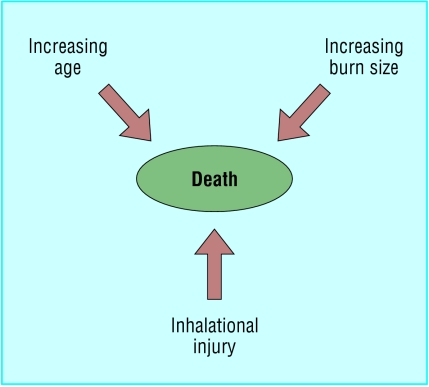
Certain factors increase the risk of death. The most important are increasing age, increasing burn size, and the presence of an inhalational injury. Exactly how these factors interrelate is not clear. Evidence suggests that a patient aged over 60 with a burn covering more than 40% of body surface area and an inhalational injury has a > 90% chance of dying.
Figure 8.
Factors that increase the risk of death after a major burn
As well as assessing the injury, it is also important to make some estimation of the patient's quality of life before the burn. This can be obtained from relatives, carers, or the patient. Deciding not to resuscitate a patient is difficult. It is often useful to get a consensus opinion from the whole burn team.
Figure 9.

UK government's “Fire kills” campaign started in 2002
Burn prevention and fire safety
The fact that 90% of burn injuries are preventable has led to many attempts to decrease their incidence. These attempts fall into two main categories—education and legislation. Education is an “active” process that requires a change in an individual's behaviour. Legislation is “passive” and is independent of a person's actions. Both have advantages and disadvantages.
Education—The most successful campaigns have targeted specific burn aetiologies or populations. A good example of this is the campaign to reduce chip pan fires in Britain during the late 1970s. This led to a 30% reduction in the incidence of burns due to chip pan fires. The main problem with educational prevention is that it relies on changing the way individuals behave. This means the message must be repeated regularly, as shown by the UK government launching a second chip pan fire campaign in 1999. However, a successful educational campaign has an instantaneous and widespread impact.
Table 2.
Information in UK government's “Fire kills” campaign “Top 10 safety tips”
| How to make your house a safe home |
| • Fit a smoke alarm and check it regularly |
| • Make a fire action plan so that everyone in your house knows how to escape in the event of fire |
| • Take care when cooking with hot oil and think about using thermostatically controlled deep fat fryers |
| • Never leave lit candles unattended |
| • Ensure cigarettes are stubbed out and disposed of carefully |
| • Never smoke in bed |
| • Keep matches and lighters away from children |
| • Keep clothing away from heating appliances |
| • Take care in the kitchen. Accidents while cooking account for 59% of fires in the home |
| • Take special care when you are tired or when you've been drinking. Half of all deaths in domestic fires occur between 10 pm and 8 am |
| On finding a fire in the home |
|---|
| • Get out |
| • Stay out |
| • Call 999 (telephone number for UK emergency services) |
Legislation—Legislation (such as the compulsory fitting of sprinklers in commercial buildings) has led to substantial decreases in burn injury. The main problem with legislation is that it takes time to pass and to have an effect. Compliance must also be obtained and maintained. However, as it does not rely on a change in individuals' actions, legislation can be effective.
Effective prevention requires both passive and active elements. The basis for all prevention is good epidemiological data to reveal specific causes of burns and at risk populations, both of which can be targeted. The UK government is currently running the “Fire kills” campaign, which covers all aspects of domestic fire prevention and safety. The related website, www.firekills.gov.uk, is an excellent source of information.
Table 3.
Key points
| • Burns are a major cause of injury and death worldwide |
| • Flame burns are the most common type |
| • Young children, elderly people, and those who are mentally or physically compromised are at particular risk |
| • Death is more likely with increasing age, increasing burn size, and presence of inhalational injury |
| • 90% of burns are preventable |
Some risk factors for burns are not easy to change. Overcrowding, poor housing, and the other attributes of poverty are major contributors to the risk of burn injuries.
Shehan Hettiaratchy is specialist registrar in plastic and reconstructive surgery, Pan-Thames Training Scheme, London; Peter Dziewulski is consultant burns and plastic surgeon, St Andrews Centre for Plastic Surgery and Burns, Broomfield Hospital, Chelmsford.
The ABC of burns is edited by Shehan Hettiaratchy; Remo Papini, consultant and clinical lead in burns, West Midlands Regional Burns Unit, Selly Oak University Hospital, Birmingham; and Peter Dziewulski. The series will be published as a book in the autumn.
Competing interests: RP has been reimbursed by Johnson & Johnson, manufacturer of Integra, and Smith & Nephew, manufacturer of Acticoat and TransCyte, for attending symposiums on burn care.
Further reading and resources
- • Wilkinson E. The epidemiology of burns in secondary care, in a population of 2.6 million people. Burns 1998;24: 139-43 [DOI] [PubMed] [Google Scholar]
- • Ryan CM, Schoenfeld DA, Thorpe WP, Sheridan RL, Cassem EH, Tompkins RG. Objective estimates of the probability of death from burn injuries. N Engl J Med 1998;338: 362-6 [DOI] [PubMed] [Google Scholar]
- • Fire kills. You can prevent it. www.firekills.gov.uk
- • Herndon D. Total burn care. 2nd ed. London: WB Saunders, 2002
- • National Community Fire Safety Centre Toolbox. www.firesafetytoolbox.org.uk
- • Liao C-C, Rossignol AM. Landmarks in burn prevention. Burns 2000;26: 422-34 [DOI] [PubMed] [Google Scholar]