Abstract
We summarized studies describing the prevalence of, trends in, and correlates of nonmedical exemptions from school vaccination mandates and the association of these policies with the incidence of vaccine-preventable disease.
We searched 4 electronic databases for empirical studies published from 1997 to 2013 to capture exemption dynamics and qualitatively abstracted and synthesized the results. Findings from 42 studies suggest that exemption rates are increasing and occur in clusters; most exemptors questioned vaccine safety, although some exempted out of convenience. Easier state-level exemption procedures increase exemption rates and both individual and community disease risk.
State laws influence exemption rates, but policy implementation, exemptors’ vaccination status, and underlying mechanisms of geographical clustering need to be examined further to tailor specific interventions.
Childhood vaccinations are one of the most significant public health interventions of all time. They reduce the risk of contracting dangerous vaccine-preventable childhood diseases on the individual level and, when immunization coverage is high enough, confer herd immunity at the population level for those diseases that are contagious.1,2 Recognizing the public health importance of the childhood immunization schedule, all 50 US states require parents to provide documentation of immunization for admission to school and day care, a mandate that has been crucial for achieving widespread vaccination.1,2 However, all states also allow medical exemptions for those children unable to receive vaccines for medically contraindicated reasons.3 Exemption laws in all but 2 states (Mississippi and West Virginia) also provide for nonmedical exemptions (NMEs) on the basis of parents’ religious, philosophical, or personal beliefs. NMEs are considered an important mechanism to balance child welfare and the protection of public health with parental rights.4,5 Although some have argued that NMEs should not be allowed because parents who choose not to immunize their children put their own children and others at risk,6 others believe that the negative consequences of exemption are not sufficient to justify violating parental autonomy.
As concerns about vaccine safety have increased over the past 15 years, more parents are choosing to refuse or delay vaccines.3,7 This increase in vaccine hesitancy can be seen at the point of school entry in the rising rates of NMEs. Furthermore, NMEs from school-entry immunization mandates are receiving increased policy and public health scrutiny because exemption rates within and across schools have significant epidemiological implications. Where NME rates are high enough to compromise herd immunity at the local level, the risk of vaccine-preventable disease outbreak increases. Understanding the spatial and social patterning of NMEs is therefore critical to infectious disease prevention and control efforts.
Over the past decade, rising attention to vaccine hesitancy and NMEs has prompted several state legislatures to introduce, consider, and in some cases enact new exemption laws. In 2003, Arkansas, which previously only allowed medical and religious exemptions, started allowing philosophical exemptions on the condition that parents provided a notarized statement requesting an exemption, completed a vaccination education component, and signed a statement acknowledging the receipt of vaccination information.8,9 Similarly, in 2003, Texas also started to allow philosophical exemptions, requiring those who wanted to exempt to obtain a form from the Texas Department of Health and declare their objections in an affidavit.10 Conversely, Washington, Oregon, and California, all of which previously had lenient exemption policies and, particularly in the case of Washington and Oregon, very high exemption rates, recently made the process for claiming an exemption harder by requiring a signed statement from a health care practitioner that the parent had been informed of the risks and benefits of immunization. In the 2011–2012 legislative cycle, bills to tighten or eliminate NMEs were introduced in 3 states, whereas bills to expand or allow NMEs were proposed in another 10.11
Continued increases in vaccine refusal and NME rates and the growing attention to NMEs in state legislatures underscore the importance of understanding the determinants of NMEs, the impact of state NME policies, and the epidemiological implications of NMEs for vaccine coverage, herd immunity, and disease outbreak risk. The goal of this systematic review, therefore, is to summarize the recent evidence on NMEs, including the prevalence of, trends in, and correlates of NMEs and the association of these exemptions and exemption policies with the incidence of vaccine-preventable disease.
METHODS
We designed and report this systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.12 The protocol was not registered. We identified search terms, inclusion criteria, and exclusion criteria before the literature search. The search terms were exemption* AND (vaccin* OR immuniz*), and we restricted the results to 1997 to 2013 to capture exemption dynamics in the most recent period of vaccine hesitancy and refusal.13,14 For the study to be included, it had to be an empirical or modeling study that addressed at least 1 of the following topics:
prevalence and trends in exemptions from mandated school-entry vaccines,
predictors or correlates of seeking an exemption (parent level) or granting an exemption (provider, school, or community level),
characteristics and trends in state-level exemption policies and their impact on exemption rates and disease risk, and
epidemiological implications of exemptions.
We excluded studies if they
were not in English;
did not refer to US exemption laws and trends;
did not refer to exemption from school vaccine mandates;
did not refer to personal belief, philosophical, religious, or nonmedical exemptions; or
referred only to the legal or ethical arguments for or against vaccine mandates or exemptions.
We conducted electronic searches in CINAHL, PubMed, and OVID or MEDLINE in consultation with a reference librarian. We found additional studies through citation searches of identified articles and through Table of Contents alerts from Pediatrics, Vaccine, American Journal of Public Health, JAMA Pediatrics, and Health Affairs after our search was conducted. J. C., E. W., and C. D.-H. screened titles and abstracts of articles identified in the initial search for eligibility according to inclusion and exclusion criteria, with no discrepancy in study selection. Studies deemed eligible after the first screen were then assessed in a full-text review using the same inclusion and exclusion criteria. E. W. and J. C. extracted the following elements from included articles: data collection time frame, sample size, study methodology, geographic location, demographics, and key results by topic (prevalence and trends, predictors or correlates of seeking or granting exemptions, characteristics and trends in state-level policies, and epidemiological implications).
After data extraction, we also assessed the articles for quality; because the majority of included articles were observational, we used the Quality Assessment Tool for Systematic Reviews of Observational Studies.15 This tool covers aspects of external validity, reporting, bias, and confounding; it checks for appropriate sampling methods, reliable and valid measurement of the predictor and outcome variables, an adequate response rate, control for any confounding factors, and appropriate statistical methods. E. W. reviewed each eligible article using this tool; all 44 eligible studies met a medium or high quality standard, and therefore all were included in the review.
E. W. analyzed and qualitatively summarized key results according to the 4 key topics of interest, and A. B. verified them. Some studies’ results addressed more than 1 topic and were therefore included in more than 1 category. Within each topic, studies with similar data and results were grouped together and synthesized, and studies with conflicting results were noted.
RESULTS
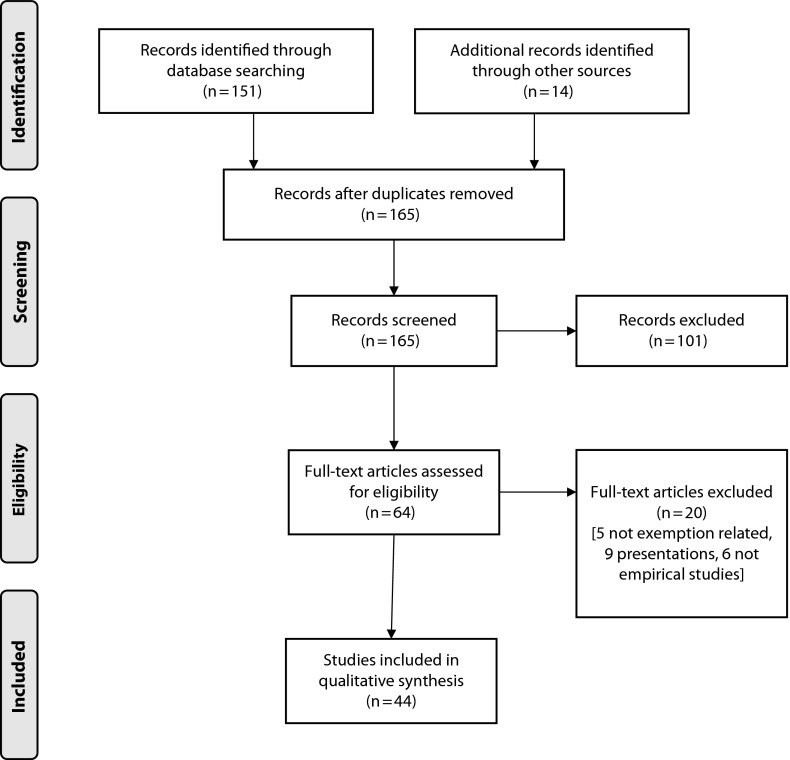
Our initial search yielded 165 articles, with 64 full-text articles assessed for eligibility (see Figure 1 for Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart). Of the full-text articles assessed, 5 were not related to exemptions, 9 were presentations, and 6 were commentaries, historical reviews, or otherwise not empirical studies, for a total of 20 excluded. We therefore included 44 studies in the review: 29 quantitative, 13 mixed, and 2 qualitative. Of the quantitative and mixed studies, most (27) were cross-sectional observational studies, 12 were time-series cohort studies, 1 was a retrospective cohort study, and 2 were case-control studies. Key elements of the 44 included studies are shown in Table 1.
FIGURE 1—
Flow diagram of study selection for systematic review of research on nonmedical exemptions from school immunization requirements.
TABLE 1—
Selected Information From Studies in the Review
| Citation | Time Frame | Method and Study Design | Sample and Demographics | Geographic Location | Study Contained Key Results Related to | Key Results |
| Atwell et al.16 | 2005–2010 | Quantitative, time-series cohort | All kindergarten students with nonmedical exemptions in CA and all cases of pertussis from 2005 to 2010 | CA | C, E | Census tracts within a NME cluster were more likely to be in a pertussis cluster than those outside an NME cluster. Both NME and pertussis clusters were associated with high SES characteristics. |
| Birnbaum et al.17 | 2010–2011 | Quantitative, cross-sectional | 1018 private and public schools; kindergarteners | AZ | T, C | Rates of PBE are highly spatially aggregated in AZ and within Phoenix. Schools with highest proportion of White students had the highest PBE rates. Charter schools and those with low prevalence of free and reduced lunches had significantly higher rates of PBE. |
| Blank et al.11 | 2011–2013 | Mixed, descriptive, and cross-sectional | 50 states | US | S | Fourteen, 15, and 15 states were found to have easy, medium, and difficult exemption policies, respectively. States that granted philosophical exemptions and states with simpler exemption procedures had higher rates of exemption. No association was found between strictness of religious exemption policy language and percentage of children exempted for religious reasons. From 2011 to 2012, bills were introduced in 4 states restricting scope of NMEs and in 10 states broadening it. However, only bills that tightened exemption policies passed. |
| Britten18 | 2008–2009 | Quantitative, cross-sectional, mathematical model | 5 communities; kindergarteners | CA | T, E | Using a hypothetical population, each percentage decrease in exemption coverage was found to lead to a significant increase in severity of the outbreak and duration of the outbreak. The most significant increase in severity happened between 93% and 90% coverage, dependent on population size. |
| Buttenheim et al.19 | 2008–2010 | Quantitative, cross-sectional | > 7000 private and public schools; around 500 000 kindergartners | CA | T | Crude PBE rates in CA increased 25% from 2008 to 2010, and PBE rate per 100 kindergartners increased from 1.9 to 2.3. The percentage of schools with a high PBE rate also increased from 2.2% to 2.6%. The interaction index increased from 1.6 to 2.0, and the aggregation index increased from 14.7 to 15.6, indicating increased interactions of exempted kindergarteners with other exempted kindergartners. Aggregation indexes varied widely among counties. |
| Centers for Disease Control and Prevention20 | May–June 2005 | Mixed, descriptive, cross-sectional | 34 measles patients | Cincinnati, OH | E | A 17-year-old girl not vaccinated for measles contracted measles in Bucharest, Romania, during an outbreak and returned to Indiana. 34 people were later identified with measles, only 2 of whom were partially or fully vaccinated. |
| Centers for Disease Control and Prevention21 | March 2004 | Mixed, descriptive, cross-sectional | 1 case of measles | Cedar Rapids, IA | E | 28 students from a college with a high exemption rate went to India, and 6 measles cases occurred among the students. It was recommended they not return to the US until after the period of infectivity, but 1 student went against these precautions, alerting public health officials about the potential risk of outbreak. |
| Centers for Disease Control and Prevention22 | March–June 2011 | Mixed, descriptive, cross-sectional | 2 measles outbreaks, 13 cases of measles | UT | E | Two outbreaks occurred in Utah in April and May 2011. Thirteen people were confirmed to have measles; 9 (69%) were unvaccinated and had PBEs. The infection was acquired during international travel (1 case), in households (8 cases), and schools (3 cases). Source of infection was unknown in 1 case. |
| Centers for Disease Control and Prevention23 | April 9–July 7, 1996 | Mixed, descriptive, cross-sectional | 107 measles reports | Washington County, UT | E | Of the 99 measles cases who were vaccine-eligible, 64 (64%) had not been vaccinated. At the high school at which the outbreak was initially reported, 27 (3%) of 879 students were unvaccinated, and 780 (89%) had received only 1 dose of the MMR vaccine. Seventeen of the unvaccinated students had philosophic exemptions, and the other 10 had no record of measles vaccination. |
| Centers for Disease Control and Prevention24 | January 1–April 25, 2008 | Mixed, descriptive, cross-sectional | 64 measles reports | NY, AZ, CA, MI, WI, HI, IL, NY, PA, VA | E | Of the 64 patients with measles 63 were unvaccinated or had unknown or undocumented vaccination status. Of these, 14 were not vaccinated because of religious or personal beliefs. 5 who had traveled abroad were unvaccinated, 2 because of personal beliefs. |
| Centers for Disease Control and Prevention25 | January–July 2008 | Mixed, descriptive, cross-sectional | 131 measles reports | IL, NY, WA, AZ, CA, WI, HI, MI, AR, DC, GA, LA, MO, NM, PA, VA | E | Among the 131 measles patients, 123 were US residents, of whom 112 (91%) were unvaccinated or had unknown vaccination status. Among these 112 patients, 95 (85%) were eligible for vaccination, and 63 (66%) of those were unvaccinated because of philosophical or religious beliefs. |
| Centers for Disease Control and Prevention26 | 2009–2010 | Quantitative, descriptive, cross-sectional | 47 states and DC | US | T | From 2009 to 2010, total kindergarten exemption rates ranged from < 1% to 6.2% across states; 15 states had a total exemption rate ≥ 3.0%, and 15 states had exemption rates < 1%. Nonmedical exemptions ranged from 0.2% (Rhode Island) to 5.8% (Washington) among the states that allow NMEs. |
| Centers for Disease Control and Prevention27 | 2011–2012 | Quantitative, descriptive, cross-sectional | 49 states and DC | US | T | From 2011 to 2012, total kindergarten exemption rates ranged from < 0.1% in Mississippi to 7.0% in Alaska, with 10 reporting rates < 1%, and 9 reporting > 4% total exemption rates. The median total exemption level was 1.5%, a median increase of 0.2 percentage points compared with the 2009–2010 school year. Arkansas reported the largest increase in exemptions with an increase of 3.4 percentage points, and Nebraska reported the largest decrease, with a decrease of 2.3 percentage points. The median NME level was 1.2%, where allowed, with a range from 0.04% in Delaware and Kentucky to 5.8% in Oregon. |
| Centers for Disease Control and Prevention28 | 2012–2013 | Quantitative, descriptive, cross-sectional | 49 states and DC | US | T | From 2012 to 2013, the percentage of kindergarteners with an exemption was < 1% for 9 states and > 4% for 11 states, ranging from < 0.1% in Mississippi to 6.5% in Oregon, with a median of 1.8%. Georgia and West Virginia had the largest increases in total exemptions, each with an increase of 1.0 percentage point; 4 states reported decreases of > 1.0 percentage points. The median NME level was 1.5%, ranging from 0.2% in New Mexico to 6.4% in Oregon. |
| Ernst & Jacobs29 | 2009–2011 | Quantitative, cross-sectional, descriptive | Vaccine coverage levels in 18 states; county-level PBE rates in 8 states | US | S, E | A significant trend of increasing vaccine coverage was found with increasing difficulty of obtaining PBE for DTP–DTaP–DT and poliovirus vaccines (P < .05) and a modest association for MMR and HepB vaccines (P < .01). Although mean vaccination coverage remains > 90% even in states in which exemptions are easy to obtain, geographic heterogeneity exists in vaccine exemptions; in Arizona, PBE rates ranged from 0.6% to 8.5% among counties, and in Washington, rates ranged from 1% to 25.3%. |
| Fair et al.30 | 1992–2000 | Mixed, descriptive, cross-sectional | 15 cases of tetanus in children aged < 15 y | TN, MT, MO, IN, FL, MI, CA, OH, PA, TX, WV | T, E | Fifteen cases of tetanus in children aged < 15 y were reported in 11 states. 12 (80%) children were unprotected because of lack of vaccination. Among all unvaccinated cases, objection to vaccination, either religious (n = 9) or philosophic (n = 3), was the reported reason for choosing not to vaccinate. |
| Feikin et al.31 | 1987–1998 | Quantitative, time-series cohort | All children aged 3–18 y in CO | CO | S, E | The percentage of philosophical exemptions among school-aged children in Colorado increased from 1.02% to 1.87%. Exemptors were 22.2 times more likely to acquire measles and 5.9 times more likely to acquire pertussis than vaccinated children. The frequency of exemptors in a county was associated with the incidence rate of measles and pertussis in vaccinated children. Schools with pertussis outbreaks had more exemptors than schools without outbreaks. At least 11% of vaccinated children in measles outbreaks acquired infection through contact with an exemptor. |
| Fiebelkorn et al.32 | 2001–2008 | Quantitative, time-series cohort | 557 cases, 38 outbreaks | US | E | In the US, 557 confirmed cases of measles and 38 outbreaks were reported, 232 (42%) of which were imported from other countries. A total of 285 US-resident case-patients (65%) were considered to have preventable measles. From 2004 to 2008, a total of 68% of vaccine-eligible US-resident case-patients claimed exemptions for personal beliefs. |
| Gaudino & Robison33 | 2004–2005 | Quantitative, retrospective cohort | 1588 parents of OR elementary school students | OR | T, C | Exempting parents reported more markers of lower SES than nonexemptors. Exemptors were significantly more likely to have: strong vaccine concerns, > 1 childbirths at a nonhospital, distrust of local doctors, chiropractic health care, and knowledge of someone with a vaccine-hurt child, although this varied by specific communities. Exemptors were less likely to have pro-vaccine beliefs and less likely to report relying on print materials. |
| Gullion et al.34 | Not mentioned | Qualitative, semistructured interviews | 25 nonvaccinating parents | TX | C | Most (88%) of the interviewees mentioned aspects of their lifestyle that could be categorized as ‘‘alternative living.” Participants engaged in sophisticated data collection and analysis in formulating their stance on vaccinations and were skeptical of the medical community, although they placed a high value on scientific knowledge. |
| Gust et al.35 | July and August 2003 | Quantitative, cross-sectional | 642 parents with at least 1 child aged < 6 y | US | C | Parents who disagreed that they had enough immunization information were more likely to report that they would not have their child immunized if it were not required by law; to believe states should grant exemptions; to mistrust the government to establish immunization policy; and to believe that they should be allowed to obtain exemptions for their child even if it raised the risk of disease for everyone else. |
| Gust et al.36 | May 2004–February 2006 | Mixed: interviews, focus groups, cross-sectional | 100 cases of parents who would not immunize children if not required or who had considered filing or filed a NME and 100 controls | US | C | Parents who had filed exemptions or considered it did not differ demographically from those who did not file exemptions but were significantly more likely to have negative attitudes about immunizations, including safety, number of immunizations, and trust. A brochure intervention was found not to have improved parents’ immunizations attitudes compared with controls. |
| Imdad et al.37 | 2000–2011 | Quantitative, time-series cohort | All schools in NY; all pertussis cases among children aged < 19 y | NY | T, S, E | Religious exemptions in NY increased from 0.23% to 0.45% in the past 10 y, although not uniformly among counties. Counties with religious exemption prevalence rates > 1% had a higher incidence of pertussis, and a 0.1% increase in exemption rate corresponded with an increased pertussis incidence of 5 in 100 000. The mean incidence of pertussis among exempted children was 14 times that among vaccinated children. High exemption rates in a county increased pertussis risk for both vaccinated and exempted children. |
| Kennedy et al.38 | 2002 | Quantitative, cross-sectional | 1527 parents with at least one child aged ≤ 18 y | US | T, C, S | A parent’s belief regarding compulsory vaccination for school entry is significantly associated with beliefs in the safety and utility of vaccines and the intention to have the youngest child fully vaccinated. Supportive parents were more likely to be White, to have a higher household income, and to have a smaller household size. Residence in a state that permits philosophical exemptions was also associated with a parent’s opposition to compulsory vaccination. |
| Kennedy & Gust39 | Sometime between 2005 and 2008 | Mixed, focus group, interview, cross-sectional | 6 church members for focus group; 12 study households involved in the outbreak for interview | IN | C | Outbreak households recognized the importance of vaccines, yet had concerns or doubts about their safety and necessity, believing that childhood vaccinations may cause serious side effects or learning disabilities. All believed in the right to refuse vaccines but were open to alternatives such as quarantine during an outbreak, and all reported that they had access to enough information on vaccination. Most said that the outbreak experience did not make their opinion of vaccines more positive. |
| Luthy et al.40 | Not mentioned | Qualitative, cross-sectional questionnaire | 287 parents | UT | C | Five overarching themes were identified regarding PBEs: parental perceptions of vaccine harm (such as the belief that vaccines caused autism), health care systems issues (insofar as filing for a PBE was more convenient), chronic disease concerns, immune system concerns, and adverse reaction concerns. |
| Luthy et al.41 | Not mentioned | Quantitative, cross-sectional questionnaire | 801 parents who have an exempted child | UT | C | The most commonly reported reason for seeking a personal exemption was vaccination conflicting with philosophical beliefs. Most parents communicated their vaccine concerns with their health care provider before seeking exemption. The majority of exempting parents did not use the Internet when researching vaccines even though they had Internet access. |
| Mergler et al.42 | 2002–2003, 2005 | Quantitative, cross-sectional | 1367 parents and 551 providers | CO, MA, MO, WA | C | Parents who agreed that a child’s immune system could be weakened by too many immunizations or, conversely, who the community benefits from having children fully vaccinated; that the child benefited from vaccination; and that vaccines were very safe had greater odds of having a provider who shared those beliefs. |
| Omer et al.43 | 1993–2004 | Quantitative, time-series cohort | 4495 schools, 1111 cases | MI | S, E | A total of 23 significant clusters of high exemption rates and 6 clusters of pertussis cases were identified. There was a statistically significant geographic overlap between exemptions and pertussis case clusters. Census tracts in exemptions clusters were 3 times more likely to also be in a pertussis cluster than census tracts outside any exemptions cluster. |
| Omer et al.44 | 1991–2004; 1986–2004 | Quantitative, time-series cohort | 48 states, kindergarten or first-grade data | US, except MS and WV | S, E | States that easily granted exemptions had higher NME rates than states with medium and difficult exemption processes, as well as increased pertussis incidence. Although the mean exemption rate increased an average of 5% for easy-exemption-process states, there was no significant change in states with only religious exemptions or with medium or difficult exemption processes. |
| Omer et al.45 | 2005–2011 | Quantitative, time-series cohort | 50 states | US | S | Unadjusted rates of NME in states with easy exemption policies were 2.31 times as high as those of states with difficult exemption policies. By 2011, exemption rates in states with easy, medium, and hard exemption policies increased to 3.3%, 2.0%, and 1.3%, with annual rates of 13%, 18%, and 8%, respectively. |
| Peterson et al.46 | February–May 2010 | Quantitative, cross-sectional | 2052 students in elementary, middle, and high schools in rural school district | WA | T | A total of 5.4% of children in kindergarten and 4.74% of children in kindergarten through 12th grade were exempted from immunizations, with higher exemptions in rural districts. Correcting school immunization records resulted in an increase in the number of students classified as fully immunized. After conducting school-based immunization clinics, the number of fully immunized students also increased. |
| Richards et al.47 | 1994–2009 | Quantitative, time-series cohort | 6392 schools | CA | T, C | The average school PBE rate increased from 0.6% in 1994 to 2.3% in 2009, an average of 9.2% per year. The average PBE rate among private schools was 1.77 times that among public schools, and its annual rate of increase was higher. Schools located in rural census tracts had 1.66 times higher PBE rates than those in urban census tracts. Exemption rates were also found to be associated with race, population density, education, and income. |
| Rota et al.48 | January 1998 | Mixed, cross-sectional survey | 48 states, distributed to state health department immunization program managers | US, except MS and WV | S | Sixteen states delegated sole authority for processing exemptions to school officials, and 9 states had written policies informing parents who seek an exemption of the risks of not immunizing. The complexity of the exemption process was inversely associated with the proportion of exemptions filed. |
| Safi et al.8 | 2001–2010 | Quantitative, time-series cohort | All students with exemptions in AR | AR | T, S | Exemptions increased steadily from 2003 after philosophical exemptions became allowed. Kindergarten had the steepest increase in exemptions. Medical exemptions declined by 55%, and religious exemptions declined and then increased. In the 2009–2010 school year, 70.8% of exemptions were requested for all vaccines, 9.2% were requested for ≥ 2 vaccines, and 20% were requested for a single vaccine. Of the single-vaccine exemptions, 93% were for the MMR and 4.6% were for HepB and varicella. |
| Salmon et al.49 | 1985–1992 | Quantitative, time-series cohort | Mapping of exemptors by county in CA; individuals aged 5–19 y | US | E | On average, exemptors were 35 times more likely to contract measles; relative risk varied by age and year. When mapping exemptors by county in CA, exempt populations tended to be clustered in certain geographic regions. If the number of exemptors doubled, incidence of measles in nonexempt populations would increase by 5.5%, 18.6%, and 30.8%, respectively, for intergroup mixing ratios of 20%, 40%, and 60%. |
| Salmon et al.50 | 1998–2004 | Quantitative, case-control | 1367 parents, 391 of exempt children and 976 of fully vaccinated children | CO, MA, MO, WA | T, C, S | Most children (75%) with NMEs received at least some vaccines. Parents of exempt children were significantly more likely to report low perceived vaccine safety and efficacy, a low level of trust in the government, low perceived susceptibility to and severity of vaccine-prevented diseases, lower confidence in government sources for information, and higher confidence in alternative medicine professionals. |
| Salmon et al.51 | May 2001– June 2002 | Quantitative, cross-sectional | 695 schools, surveys mailed to elementary school personnel who had completed state immunization report | CO, MA, MO, WA | C | Greater perceived disease susceptibility and severity of vaccines were associated with a decreased likelihood of a child in the school having an exemption. Children in schools at which the respondents were nurses or who had confidence in health departments were significantly less likely to be given an exemption. Use of professional organizations, government resources, and vaccine companies and pharmacists for vaccine information were associated with decreased likelihood of a child having an exemption. |
| Salmon et al.52 | 2001–2002 | Quantitative, cross-sectional | 1000 school immunization personnel in CO, MA, MO, and WA | CO, MA, MO, WA | S | School policies associated with an increased likelihood of children having exemptions included lack of provision of written instructions for completing the immunization requirement before enrollment, administrative procedures making it easier to claim an exemption, and granting of philosophical exemptions. A correlation was found between the number of procedures that make administration of exemptions difficult and a lower odds of actual exemptions. |
| Salmon et al.53 | Not mentioned | Quantitative, case-control | 780 parents | WI | T, C | Varicella vaccine and HepB vaccine were the top vaccines often not received by exempt children. The top reasons for seeking exemptions included the belief that vaccines might cause harm, that it was better to get natural disease, that the child was not at risk for disease, and that the child might develop autism. Exempt parents were also less likely to believe in disease susceptibility, severity, and vaccine efficacy and safety. |
| Smith et al.54 | 1995–2001 | Quantitative, time-series cohort | 151 720 children aged 19–35 mo, 795 of whom were unvaccinated | US | T, C, S | Undervaccinated children tended to be Black; have a younger mother who was not married and did not have a college degree; live in a poorer household; and live in a central city. Unvaccinated children tended to be White; have a mother who was married and had a college degree; live in a wealthier household; and have parents who expressed concerns regarding safety of vaccines. States that allowed philosophical exemptions also had significantly higher estimated rates of unvaccinated children. |
| Sugerman et al.55 | 2008 | Mixed, discussion groups, survey, cross-sectional | 839 patients | CA | T, C, E | PBE rates increased, and higher PBE rates in public schools were associated with higher median income. There was no significant effect of income in public charter and private schools. On the parent level, nearly all parents who reported declining or delaying vaccination were White and college educated. Most reported substantial skepticism of the government, pharmaceutical industry, and medical community; believed vaccination was unnecessary; and felt vaccines can produce a number of adverse health effects. |
| Thompson et al.56 | 2001–2002, 2002–2003, 2003–2004 school years | Quantitative, time-series cohort | Immunization exemptions granted for all AR school attendees, K–12 | AR | T, S | Philosophical exemptions were found to be clustered geographically. After AR started allowing philosophical exemptions, the total number of exemptions granted increased by 23% from year 1 to year 2, by 17% from year 2 to year 3, and by 50% from year 3 to year 4. NMEs accounted for 79% of exemptions granted in years 1 and 2, 92% in year 3, and 95% in year 4. |
| Wenger et al.57 | 007 | Mixed, cross-sectional | 359 Amish parents | OH | T, C | A total of 68% stated that all of their children had received ≥ 1 immunization, and 17% reported that some of their children had received ≥ 1 immunization. Only 14% of the parents reported that none of their children had received immunizations. Reasons Amish parents resisted immunizations include concerns about adverse effects such as side effects, dangerous chemicals, and injection of a disease. |
Note. C = predictors or correlates; DT = diphtheria and tetanus; DTaP = diphtheria, tetanus, and pertussis; DTP = diphtheria, pertussis, and tetanus; E = epidemiological implications; HepB = hepatitis B; MMR = measles–mumps–rubella; NME = nonmedical exemption; PBE = personal beliefs exemption; S = characteristics and impact of state-level exemption policies; SES = socioeconomic status; T = prevalence and trends.
Nonmedical Exemptions Prevalence and Trends
Nineteen studies summarized NME prevalence. Data from the Centers for Disease Control and Prevention’s annual school immunization assessment showed a general increase in state-level NME rates over time, from 1.6% in 2009–201026 to 2.0% in 2011–201227 to 1.9% in 2012–2013,28 an overall 19% increase (data for 2009–2010 and 2012–2013 are shown in Table 2). For 2012–2013, state exemption rates ranged from a low of 0.0% in Delaware to a high of 6.4% in Oregon (note that Mississippi and West Virginia do not permit NMEs). Thirteen state and metropolitan grantees had NME rates exceeding 3%, and 16 grantees had exemption rates below 1%. Since 2009–2010, 32 states have shown an increase in state-level exemption rates, 4 states and the District of Columbia have remained the same, 9 states have decreased their exemption rates, and 5 states did not have data for a longitudinal comparison. Since 2005–2006 (not shown in Table 2),58 many states have seen a rough doubling of exemption rates, regardless of the initial rates. For example, between 2005–2006 and 2012–2013, Arkansas’s exemption rate increased from 0.3% to 0.7%, California’s rate from 1.3% to 2.8%, and Oregon’s rate from 3.4% to 6.4%.
TABLE 2—
Kindergarten NME from School-Entry Immunization Mandates by State: United States, 2009–2010 and 2012–2013
| 2009–201026 |
2012–201328 |
||||||||||
| State or District (No Cities) | Total Kindergarten Population, No. | Religious Exemptions, No. | Philosophical Exemptions, No. | Total NMEs, No. | % | Total Kindergarten Population, No. | Religious Exemptions, No. | Philosophical Exemptions, No. | Total NMEs, No. | % | % Point Change, 2009–2012 |
| Alabama | 75 358 | 282 | . . . | 282 | 0.4 | 72 929 | 414 | . . . | 414 | 0.6 | 0.2 |
| Alaska | 9641 | 369 | . . . | 369 | 3.8 | 10 319 | 415 | . . . | 415 | 4.0 | 0.2 |
| Arizonaa | 89 287 | . . . | 2479 | 2479 | 2.8 | 90 054 | 3790 | 4.2 | 1.4 | ||
| Arkansas | 34 733 | 33 | 132 | 165 | 0.5 | 43 212 | 99 | 342 | 458 | 1.1 | 0.6 |
| California | 507 191 | . . . | 10 280 | 10 280 | 2.0 | 535 523 | . . . | 14 921 | 14 921 | 2.8 | 0.8 |
| Colorado | NA | NA | NA | NA | NA | 70 657 | 0 | 2678 | 2678 | 3.8 | NA |
| Connecticut | 46 158 | 387 | . . . | 387 | 0.8 | 41 604 | 601 | . . . | 601 | 1.4 | 0.6 |
| Delaware | 11 327 | 65 | . . . | 65 | 0.6 | 11 997 | 5 | . . . | 5 | 0.0 | −0.6 |
| District of Columbia | 6092 | 20 | . . . | 20 | 0.3 | 7842 | 27 | . . . | 27 | 0.3 | 0.0 |
| Florida | 218 630 | 2100 | . . . | 2100 | 1.0 | 234 628 | 3281 | . . . | 3281 | 1.4 | 0.4 |
| Georgia | 141 949 | 1478 | . . . | 1478 | 1.0 | 142 732 | 73 | . . . | 73 | 0.1 | −0.9 |
| Hawaii | 18 427 | 645 | . . . | 645 | 3.5 | 20 104 | 138 | . . . | 138 | 0.7 | −2.8 |
| Idaho | 22 624 | 68 | 726 | 794 | 3.5 | 23 888 | 171 | 1138 | 1309 | 5.5 | 2.0 |
| Illinois | 165 845 | 5629 | . . . | 5629 | 3.4 | 166 884 | 8082 | . . . | 8082 | 4.8 | 1.4 |
| Indiana | 84 390 | 674 | . . . | 674 | 0.8 | 86 983 | 804 | . . . | 804 | 0.9 | 0.1 |
| Iowa | 42 698 | 359 | . . . | 359 | 0.8 | 41 701 | 500 | . . . | 500 | 1.2 | 0.4 |
| Kansas | 39 073 | 304 | . . . | 304 | 0.8 | 40 738 | 363 | . . . | 363 | 0.9 | 0.1 |
| Kentucky | 56 526 | 193 | . . . | 193 | 0.3 | 58 466 | 286 | . . . | 286 | 0.5 | 0.2 |
| Louisiana | 53 846 | 32 | 228 | 260 | 0.5 | 68 874 | 27 | 322 | 349 | 0.5 | 0.0 |
| Maine | 14 162 | 11 | 412 | 423 | 3.0 | 14 313 | 17 | 541 | 559 | 3.9 | 0.9 |
| Maryland | 75 061 | 393 | . . . | 393 | 0.5 | 75 007 | 494 | . . . | 494 | 0.7 | 0.2 |
| Massachusetts | 74 476 | 538 | . . . | 538 | 0.7 | 79 661 | 843 | . . . | 843 | 1.1 | 0.4 |
| Michigan | 129 810 | 751 | 4121 | 4872 | 3.8 | 124 662 | 1086 | 5540 | 6626 | 5.3 | 1.5 |
| Minnesotaa | 70 653 | NA | NA | NA | NA | 73 310 | 1149 | 1.6 | NA | ||
| Mississippi | 46 922 | . . . | . . . | 0 | 0.0 | 46 595 | . . . | . . . | . . . | 0.0 | |
| Missouri | 75 958 | 626 | . . . | 626 | 0.8 | 78 416 | 1665 | . . . | 1665 | 2.1 | 1.3 |
| Montana | 12 335 | 262 | . . . | 262 | 2.2 | 12 516 | 380 | . . . | 380 | 3.0 | 0.8 |
| Nebraska | 29 607 | 802 | . . . | 802 | 2.8 | 24 999 | 269 | . . . | 269 | 1.1 | −1.7 |
| Nevada | 35 209 | 357 | . . . | 357 | 1.0 | 36 070 | 224 | . . . | 224 | 0.6 | −0.4 |
| New Hampshire | NA | NA | NA | NA | NA | 12 943 | 298 | . . . | 298 | 2.3 | NA |
| New Jersey | 118 347 | 905 | . . . | 905 | 0.8 | 122 516 | 1458 | . . . | 1458 | 1.2 | 0.4 |
| New Mexico | 26 318 | 183 | . . . | 183 | 0.7 | 29 279 | 27 | . . . | 27 | 0.1 | −0.6 |
| New York | 229 273 | 1117 | . . . | 1117 | 0.5 | 239 484 | 1335 | . . . | 1335 | 0.6 | 0.1 |
| North Carolina | 116 087 | 756 | . . . | 756 | 0.7 | 130 612 | 871 | . . . | 871 | 0.7 | 0.0 |
| North Dakota | 8323 | 17 | 50 | 67 | 0.8 | 9503 | 6 | 123 | 130 | 1.4 | 0.6 |
| Ohioa | N/R | 1515 | 1.2 | 163 687 | 2665 | 1.6 | 0.4 | ||||
| Oklahoma | 51 128 | 137 | 319 | 456 | 0.9 | 56 943 | 179 | 493 | 672 | 1.2 | 0.3 |
| Oregon | 44 674 | 2330 | . . . | 2330 | 5.2 | 47 102 | 3010 | . . . | 3010 | 6.4 | 1.2 |
| Pennsylvaniaa | 149 656 | 2924 | 2.0 | 151 364 | 2339 | 1.5 | −0.5 | ||||
| Rhode Island | 11 818 | 26 | . . . | 26 | 0.2 | 12 552 | 94 | . . . | 94 | 0.7 | 0.5 |
| South Carolina | 53 725 | 303 | . . . | 303 | 0.6 | 61 799 | NA | NA | NA | NA | NA |
| South Dakota | 11 499 | 83 | . . . | 83 | 0.7 | 12 468 | 182 | . . . | 182 | 1.5 | 0.8 |
| Tennessee | 90 811 | 421 | . . . | 421 | 0.5 | 85 801 | 905 | . . . | 905 | 1.1 | 0.6 |
| Texasa | 381 425 | 2904 | 0.8 | 414 688 | 4936 | 1.2 | 0.4 | ||||
| Utah | 49 957 | 22 | 1793 | 1815 | 3.6 | 54 605 | 6 | 2010 | 2016 | 3.7 | 0.1 |
| Vermont | 6713 | 13 | 341 | 354 | 5.3 | 6792 | 14 | 371 | 385 | 5.7 | 0.4 |
| Virginia | 100 891 | 751 | . . . | 751 | 0.7 | 104 826 | 427 | . . . | 427 | 0.4 | −0.3 |
| Washington | 81 511 | 168 | 4515 | 4684 | 5.7 | 87 773 | 274 | 2774 | 3048 | 3.5 | −2.2 |
| West Virginia | 22 730 | . . . | . . . | 0 | 0.0 | 22 588 | . . . | . . . | . . . | 0.0 | |
| Wisconsin | 61 095 | 87 | 1782 | 1868 | 3.1 | 72 416 | 275 | 3631 | 3907 | 5.4 | 2.3 |
| Wyoming | NA | NA | NA | NA | NA | 8133 | 155 | . . . | 155 | 1.9 | NA |
| Total | 3 803 969 | 58 218 | 1.6 | 4 234 425 | 79 408 | 1.9 | 0.3 | ||||
Note. NA = not available; NME = nonmedical exemption. Ellipses indicate that the state does not offer that particular exemption.
Source. Centers for Disease Control and Prevention.26,28
The philosophical and religious exemption rates were reported together for this state.
Although exemption rates varied considerably across states, several studies found even greater within-state variation, identifying both spatial and social clustering of exemptions.8,33,37,55 For example, county-level NME rates in California ranged from 0% to 17% in 2010.19 In Arizona, school-level exemption rates ranged from 0% to 68% in the 2010–2011 school year; 21% of schools had exemption rates higher than 5%, 8% had rates higher than 10%, and 3% had rates higher than 20%.17 The phenomenon of clustered exemptions is important both to understand the determinants of spatial and social patterning of vaccine hesitancy and refusal and to identify the epidemiological implications of increased disease outbreak risk associated with the clustering of unvaccinated children. In addition, 1 study in Arkansas showed that although exemption rates, both nonmedical and medical, were increasing in general, the proportion of philosophical exemptions was increasing relative to other exemptions.8 That same study also showed that exemption rates were increasing faster among kindergarten children than among any other age group requiring vaccination documentation.8
Sociodemographic, Attitudinal, and Behavioral Correlates
Eighteen studies reviewed included results related to correlates of NMEs. Two studies that surveyed parents who exempted, delayed, or refused vaccines found that they tended to be White and college educated and to have relatively high incomes compared with parents who did not seek exemptions or who did not delay or refuse vaccines.18,19 Similarly, another study found that high exemption clusters were associated with higher socioeconomic status characteristics.50 However, 2 studies showed a slightly contradictory trend. In 1 survey of Oregon parents, those who exempted were more likely to have a lower socioeconomic status than nonexemptors.58 In another study, parents with lower household incomes were more likely to oppose compulsory vaccination than those with higher incomes.17 Parents who exempted from school vaccine mandates were also more likely to have a lifestyle categorized as “alternative living,” which includes veganism or vegetarianism, organic gardening, and use of natural healing remedies.34,50
The sociodemographic composition of the school and surrounding community also predicted exemption rates. Higher exemption rates were associated with higher proportion of Whites, higher percentage of college graduates, higher median household income, and lower percentage of families in poverty at the census tract, zip code, or school district level.16,17,47 Studies found more exemptions in rural than in urban school districts,46,47 and exemption rates were higher, and increased faster, among private than public schools.47
Perceptions of information provision and sufficiency were correlated with exemption preferences. Parents who did not believe they had enough immunization information were more likely to believe that states should grant exemptions on the basis of religious and personal beliefs and that parents should be allowed to obtain exemptions for their child even if it raised the risk of disease for everyone else.35 However, a majority of parents in an Indiana measles outbreak who exempted their children believed they had access to enough information on vaccination.33 Trust was also a consistent correlate of seeking exemptions: parents who filed exemptions were more likely to be skeptical of the government, pharmaceutical industry, and medical community and to distrust information, or not rely on material, coming from those sources.7,33,34,50,55 The evidence was inconsistent on the sources of information most commonly consulted by parents who exempt. Although some read peer-reviewed medical journals,34 others cited media reports questioning vaccine safety.39 Internet research was frequently reported by providers as a source of parental information; however, 1 study showed that a majority of exemptors did not use the Internet when researching vaccines even though they had Internet access.41
Not surprisingly, negative attitudes and beliefs about vaccines predict exemption. Exemptors and parents who have considered exempting are significantly more likely than nonexemptors to have strong vaccine concerns and negative attitudes about immunizations and immunization safety.33,36,39,41,50 A common and persistent concern is the belief that vaccines harm the health of the child and cause adverse reactions or developmental problems such as autism.38–41,53,55,57 Other concerns identified in the literature included fear of acquiring the disease from the vaccine, dangerous chemicals or preservatives in vaccines, the child’s receiving too many shots at 1 time, and overloading the immune system.36,39–41,57 Another common belief associated with exemption is that vaccination is unnecessary because of low perceived susceptibility to and severity of vaccine-preventable diseases.17,34,50
There also appears to be a strong association between parental and provider immunization beliefs. In 1 study that surveyed parents of exempted or nonexempted children, parents had a 12 times greater odds of believing healthy children do not need immunizations if their provider also held this belief than parents whose provider did not hold this belief.42 Parental beliefs in vaccine safety and in vaccine mandates impeding parental choice were also correlated with provider beliefs.42 This study was not able to determine whether parental views are shaped by interactions with health care providers or whether parents choose health care providers with similar vaccine beliefs; both dynamics are likely operating.
Exemptions are sometimes sought for some vaccinations but not others. In the 2009–2010 school year in Arkansas, although most (71%) exemptions were requested for all vaccines, 9% were requested for 2 or more vaccines and 20% for a single vaccine.8 Another multistate study showed that 75% of children with NMEs had received at least some vaccines (based on parent report), and 22% of the parents who filed exemptions responded that their children were fully vaccinated.50 The measles–mumps–rubella, varicella, and hepatitis B vaccines were also reported as the most frequently exempted vaccines.8,53
Although many parents seek exemptions for philosophical reasons, some parents also exempt out of convenience or because of poor access to immunization services. Parents who cannot locate child immunization records may find that filing a NME is more convenient than tracking down lost records.40,52 School personnel may therefore also affect exemption rates. Children attending schools at which nurses (vs other professional staff) are responsible for tracking immunizations were less likely to have an exemption.51 School-based immunization clinics increased the number of fully immunized students (and decreased exemptions), which supports the idea that at least some exemptions are obtained for reasons of convenience rather than conviction.46
State Exemption Policies
Fourteen studies focused on state exemption policies. States have the authority to mandate specific immunizations for day care and school attendees. All states allowed exemptions to immunization mandates for medical contraindications; 30 states and the District of Columbia allowed religious exemptions but no philosophical exemptions; 18 states allowed both religious and philosophical exemptions; and 2 (Mississippi and West Virginia) did not allow either.59 Studies have consistently found that allowing philosophical and religious exemptions increases exemption rates and decreases vaccination rates.8,11,31,43,44,56 For example, after Arkansas introduced philosophical exemptions in 2003, the total number of exemptions granted increased from 651 in 2002–2003 to 764 in 2003–2004 and 1145 in 2004–2005.8,56 Furthermore, in states with philosophical exemptions, such exemptions have increasingly encompassed an overwhelming majority of all exemptions.8,31,56 Allowing philosophical exemptions affected not only exemptions for school-aged children but also the rates of unvaccinated children too young for school-entry mandates.54 Residence in a state that offers philosophical exemptions was also associated with parents’ opposition to compulsory vaccination for school entry, although the direction of causality was not clear.38
State exemption rates also appeared to be correlated with the ease with which NMEs can be obtained. Studies have consistently found that states with easier exemption requirements (in terms of paperwork or the effort required) have higher exemption rates and vice versa.11,29,44,45,48,52 Again, causal inference is challenging here: Although stricter exemption policies may lead to lower exemption rates, legislators with constituents who have vocal vaccine-refusing parents may also be more likely to enact lenient exemption policies.11 For example, the 2003 Arkansas law that allowed philosophical exemptions but that required an educational module and an annual application process neither increased nor retarded the increase in exemptions compared with other states in the region that did not require such rigorous requirements.8 In terms of long-term trends, exemption rates in states with easy exemption regimes increased significantly over time, whereas states with medium to difficult exemption regimes showed no significant increase, although rates have been increasing in recent years across all states, regardless of exemption regime.44,45 Even in states that do not grant philosophical exemptions, such as New York, religious exemption rates are increasing and are now comparable to rates in those states that permit philosophical exemptions,37 with easier religious exemption procedures associated with higher exemption rates.11 This likely indicates that parents seek religious exemptions for philosophical or personal beliefs, and religious exemption processes should be scrutinized as well.11,37
Crucially, easier exemption regimes were associated not only with higher exemption rates but also with higher disease outbreak risk. For example, pertussis incidence from 1986 to 2004 was 41% higher in the 6 states that accepted parental signature as sufficient proof of immunization than in the 45 states and the District of Columbia that required medical records, suggesting that exemption policies affect vaccination rates and therefore disease incidence.44 Despite this strong association, even in states in which exemptions were easiest to obtain, mean vaccination coverage rate remained higher than 90%. Easy exemption regimes clearly do not produce universally high exemption rates across an entire state. The spatial and social patterning of parental preferences can interact with the variations in school-level administration and implementation of immunization and exemption laws to produce substantial heterogeneity in exemption rates both within and across counties independent of exemption regimes.29,43,47,52
Epidemiological Implications of Nonmedical Exemptions
Seventeen studies assessed the epidemiological implications of NMEs. Exemptions from mandated immunizations increased individual risk for contracting a disease and population risk for disease outbreak. Exemptors were more likely to acquire measles and pertussis than vaccinated children,21,37 with a 22- to 35-times higher risk for measles49 and a 6-times higher risk for pertussis.31 In outbreaks of vaccine-preventable childhood diseases in the United States, many affected children had exemptions or were otherwise unvaccinated because of parental philosophical or religious beliefs.20,21,23–25,55 The evidence was most striking in the case of measles.23,29,32 For example, in 1997 when a total of 138 cases were reported in the entire United States, 1 county in Utah had an exemption rate nearly 6 times the national average and experienced a measles outbreak with 107 cases. Half of these cases were people who had been vaccinated, showing that high exemption rates can put nonexemptors at risk, too.23 Of 131 confirmed measles cases in the United States in 2008, 112 were not vaccinated and of those, 63 (66%) had not been vaccinated because of religious or philosophical beliefs.25 In 2 measles outbreaks in Washington State and Illinois in 2008, 100% of 16 children and 25 of 29 children, respectively, had not received the measles vaccine because of their parents’ beliefs.25 In 2 measles outbreaks in Utah in 2011, 9 of 13 people who contracted measles were unvaccinated because of personal belief exemptions.22 The evidence is not limited to measles: from 1992 to 2000, of the 15 cases of tetanus in children, 12 were not vaccinated for nonmedical reasons.30 Furthermore, of the school-based outbreaks in Colorado examined from 1987 to 1998, schools with pertussis outbreaks had more exemptors (mean = 4.3%) than schools without pertussis outbreaks (mean = 1.5%, P = .001).31
At the community level, studies have found that geographic clusters of vaccine exemptors are associated with outbreak risk and with higher incidence of vaccine-preventable disease.21 In California, census tracts within a cluster of NMEs were more likely to also be in a pertussis cluster than those outside a cluster of NMEs; the incidence of pertussis was also higher in NME clusters than outside of those clusters.16 Local-area exemption rates have been shown to be positively associated with the incidence of measles and pertussis even in vaccinated children, and epidemiological models based on outbreak data have shown that an increase in exemptions will lead to higher incidence of measles in nonexempt populations.18,31,37,43,49 Decreased vaccination coverage as a result of exemptions could also lead to a significant increase in the severity and duration of an outbreak, depending on the population size.18
DISCUSSION
Our review of the evidence on NMEs from mandated school-entry vaccines shows increasing NME rates in the United States, with substantial variation in rates across schools, regions, and states. Parents seeking exemptions are more likely to be White and of higher socioeconomic status and to be skeptical of the government and of the pharmaceutical medical industry. Parents who exempt are more likely to have concerns about vaccine safety and adverse effects, particularly if their health care provider shared these concerns. Exemption rates are also associated with state laws and school administrative policies: states in which it is easier to file an exemption have higher exemption rates than states in which it is harder to do so, and this, in turn, is associated with higher disease risk. Epidemiologically, higher exemption rates are associated with lower vaccination rates and therefore higher individual risk of contracting disease and higher community outbreak risk.
Although overall vaccine coverage generally remains high in the United States, our review shows both higher prevalence and more intensive geographic clustering of NMEs over time. Clustering is particularly associated with disease outbreaks because herd immunity is compromised in areas with higher proportions of undervaccinated children.60 Clustering of exemptions can result from both selection effects—like-minded people tend to live near and socialize with each other—and social influence or diffusion effects, through which parents learn about social norms and about variations in the implementation of state and school immunization requirements and in provider responses to requests for exemptions.33 Further research should disentangle these effects to better inform interventions to preserve herd immunity at the local level.
The determinants and epidemiological implications of NMEs are varied and multifactorial, suggesting that multiple intervention strategies are needed. An important underlying factor is the true immunization status of exempted children. If exempted children are completely unvaccinated, the disease outbreak risk may be higher than that estimated using exemption rates. For example, a study that used child medical records showed a 23-fold higher risk of pertussis infection among children whose parents refused pertussis vaccination than among vaccinated children,61 compared with the 6-fold higher risk found in a study that used exemptions to proxy this effect.31 Although additional studies that directly used data of unvaccinated children rather than those of exempted children have shown that the individual risk for contracting disease is increased,62,63 further research is needed to ascertain the validity of NMEs as a proxy for vaccination status in determining population-wide, epidemiological risk. This would have implications for administrative and implementation purposes—if high exemption rates are driven by parents not having complete vaccine records accessible, then reducing exemptions through better record keeping is not likely to reduce disease outbreak risk, because these children are probably fully or near-fully vaccinated.40
Previous studies have demonstrated that parental exemption decisions are shaped in part by state exemption policies. State-level policy changes that make exemption more difficult or burdensome for parents, such as have been implemented in Vermont, Washington State, and recently in California, can therefore both decrease exemption rates and increase vaccination coverage.64 However, as states look to legislative action either to reduce exemptions or to accommodate parent preferences for greater freedom to exempt, the distinctions among religious, philosophical, and personal belief exemptions will warrant further attention. When philosophical exemptions in Arkansas were introduced, religious exemptions decreased, implying substitution of religious with philosophical exemptions.8 States with a relatively easy religious exemption option but no philosophical exemption option have been shown to have higher overall rates of exemption than those with more burdensome religious exemptions and no philosophical exemptions, suggesting that vaccine-hesitant parents with philosophical but not religious objections to vaccination may be willing to use a religious exemption when the process is simple.11 The experience of California, whose new exemption law makes attaining a personal beliefs exemption harder but adds a religious option for parents who claim that they cannot seek medical advice or attention, will be important to monitor in the coming years.65,66
Furthermore, regulations related to vaccine mandates and exemptions are implemented by school and district officials, and both school culture and administrative procedures will affect implementation. For example, California’s new exemption law allows credentialed school nurses to sign the health provider attestation of vaccine counseling. Not all schools have school nurses on site, and school districts vary in their recommendations to school nurses about providing signatures for exemption requests. There is also considerable within- and across-state variation in, for example, the kindergarten registration process (when and where it occurs and what forms and documentation are required at the time of registration) and the publication of exemption data.18 Evaluation of the impact of exemption legislation should acknowledge and exploit this variation. Finally, careful evaluations of the impact of new state policies on parent preferences, school-level procedures, and exemption rates will be needed to inform future legislative initiatives and to identify the extent to which convenience, rather than conviction, is driving current exemption rates. For parents whose decision to refuse vaccines is rooted in deep-seated beliefs, however, stricter state policies for obtaining exemptions are not likely to change attitudes or behaviors; as such, these parents may nevertheless decide to exempt their child despite any stipulations the government places on obtaining exemptions.67 Because previous studies are inconsistent about the best way to address persistent vaccine hesitancy and refusal in the pre-school years, further innovation is needed in this area.68
As exemption rates climb, state health and education officials are eager to prevent further increases. Prevention strategies can be implemented at 2 time points. The first is during the prenatal period and throughout early infancy, when health care providers and public health messaging can encourage adherence to the recommended immunization schedule—a method that the United Kingdom uses without compulsory vaccination laws.69 To do this counseling effectively, health care providers need clear, evidence-based, tailored counseling messages that can be delivered in the span of a brief well-child visit; although some resources exist, they are not widely used and tend to rely on conventional health education and promotion frameworks.7 There is also variation in provider approaches to vaccine hesitancy, and certain providers may choose to dismiss parents who refuse vaccines, thereby driving them to a specific group of other providers. Conversely, parents may simply choose providers who have similar vaccine beliefs or who will accommodate requests for alternative schedules.42 However, if vaccine-hesitant parents cluster in a smaller number of provider practices that will accommodate alternative schedules, the risk of exposure to vaccine-preventable diseases increases for this population.70 Finally, financial incentives for both parents and providers have also been used in countries such as the United Kingdom and Australia.69
A second prevention strategy uses legislation and regulation to reduce requests for exemptions at the time of school entry by making the exemption process more difficult or burdensome—for example, by requiring parents to provide evidence of vaccine counseling from a health care provider.11 Several states including Washington, California, and Vermont have recently implemented such legislation.71–73 However, again, this strategy is more likely to be effective for parents with mild vaccine hesitancy or for those for whom exemption is a matter of convenience; for parents with strong antivaccine views, mandating risk–benefit counseling long after they have decided to delay or opt out of some vaccinations may actually backfire and cause protests or more mistrust if they feel the government has overstepped its boundaries in both mandating vaccinations and adding restrictions to the exemption process.67,69
We note some important limitations to this review. Many included studies were cross-sectional, and therefore we cannot ascertain the direction of causation nor completely rule out confounding. Several studies also relied on survey data, with the potential for selection or nonresponse bias. Population-level data from epidemiological studies may be susceptible to misclassification or measurement error, leading to information biases. Retrospective studies of parental beliefs are subject to recall bias. Many studies were specific to 1 or a few states, limiting generalizability. In addition to individual study limitations, the heterogeneity of study designs and outcomes precluded a quantitative meta-analysis from this systematic review, which would have been useful for analyzing quantitative trends. Many studies were also descriptive and were easily designated as high quality by the Quality Assessment Tool for Systematic Reviews of Observational Studies. As a result, quality assessment may not have been as rigorous for descriptive qualitative studies. We also excluded any studies without the mention of exemptions, even if they stated that the parents refused vaccinations for their child. This therefore could have left out other articles that are highly related to this topic but did not specifically discuss exemptions.
Vaccine mandates for school entry have been instrumental in sustaining herd immunity. Herd immunity against vaccine-preventable diseases is a valuable public good and a societal asset worth protecting. We found consistent evidence of rising rates of NMEs from school-entry vaccine mandates and of the association of exemption rates with outbreak risk. We have also found that stricter exemption laws can decrease or restrict the growth of these rates and thereby reduce outbreak risk. Interventions such as these, in addition to other strategies that address vaccine hesitancy and refusal before children reach school age, are therefore important to implement to maintain vaccination coverage across the United States and prevent outbreaks of disease.
Acknowledgments
This research was supported by funding from the National Cancer Institute (KM1CA156715).
Human Participant Protection
No protocol approval was necessary for this study because no human participants were involved.
References
- 1.Centers for Disease Control and Prevention. Childcare and school vaccination requirements 2007–2008. 2008. Available at: http://www2a.cdc.gov/nip/schoolsurv/CombinedLaws2007.pdf. Accessed August 4, 2014.
- 2.Malone K, Hinman A. Vaccination mandates: the public health imperative and individual rights. Available at: http://www.cdc.gov/vaccines/imz-managers/guides-pubs/downloads/vacc_mandates_chptr13.pdf. Accessed August 4, 2014.
- 3.Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med. 2009;360(19):1981–1988. doi: 10.1056/NEJMsa0806477. [DOI] [PubMed] [Google Scholar]
- 4.Salmon DA, Siegel AW. Religious and philosophical exemptions from vaccination requirements and lessons learned from conscientious objectors from conscription. Public Health Rep. 2001;116(4):289–295. doi: 10.1093/phr/116.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silverman RD. No more kidding around: restructuring non-medical childhood immunization exemptions to ensure public health protection. Ann Health Law. 2003;12(2):277–294. [PubMed] [Google Scholar]
- 6.Lantos JD, Jackson MA, Harrison CJ. Why we should eliminate personal belief exemptions to vaccine mandates. J Health Polit Policy Law. 2012;37(1):131–140. doi: 10.1215/03616878-1496038. [DOI] [PubMed] [Google Scholar]
- 7.Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization attitudes and beliefs among parents: beyond a dichotomous perspective. Am J Health Behav. 2005;29(1):81–92. doi: 10.5993/ajhb.29.1.7. [DOI] [PubMed] [Google Scholar]
- 8.Safi H, Wheeler JG, Reeve GR et al. Vaccine policy and Arkansas childhood immunization exemptions: a multi-year review. Am J Prev Med. 2012;42(6):602–605. doi: 10.1016/j.amepre.2012.02.022. [DOI] [PubMed] [Google Scholar]
- 9.Salmon DA, Sapsin JW, Teret S et al. Public health and the politics of school immunization requirements. Am J Public Health. 2005;95(5):778–783. doi: 10.2105/AJPH.2004.046193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonn D. Texas law allows conscientious immunisation exemptions. Lancet Infect Dis. 2003;3(9):525. doi: 10.1016/S1473-3099(03)00752-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blank NR, Caplan AL, Constable C. Exempting schoolchildren from immunizations: states with few barriers had highest rates of nonmedical exemptions. Health Aff (Millwood) 2013;32(7):1282–1290. doi: 10.1377/hlthaff.2013.0239. [DOI] [PubMed] [Google Scholar]
- 12.PRISMA. PRISMA. Available at: http://prisma-statement.org. Accessed August 4, 2014.
- 13.Mnookin S. The Panic Virus: The True Story Behind the Vaccine-Autism Controversy. New York, NY: Simon & Schuster; 2012. [Google Scholar]
- 14.Offit P. Deadly Choices: How the Anti-Vaccine Movement Threatens Us All. New York, NY: Basic Books; 2012. [Google Scholar]
- 15.Wong WC, Cheung CS, Hart GJ. Development of a quality assessment tool for systematic reviews of observational studies (QATSO) of HIV prevalence in men having sex with men and associated risk behaviours. Emerg Themes Epidemiol. 2008;5:23. doi: 10.1186/1742-7622-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atwell JE, Otterloo JV, Zipprich J et al. Nonmedical vaccine exemptions and pertussis in California, 2010. Pediatrics. 2013 doi: 10.1542/peds.2013-0878. Epub ahead of print September 30, 2013. [DOI] [PubMed] [Google Scholar]
- 17.Birnbaum MS, Jacobs ET, Ralston-King J, Ernst KC. Correlates of high vaccination exemption rates among kindergartens. Vaccine. 2013;31(5):750–756. doi: 10.1016/j.vaccine.2012.11.092. [DOI] [PubMed] [Google Scholar]
- 18.Britten N. Measles outbreaks in the face of decreasing herd immunity: the impact of vaccine exemptions. 2009. Available at: http://search.proquest.com/docview/305040041/abstract?accountid=14707. Accessed October 14, 2012.
- 19.Buttenheim A, Jones M, Baras Y. Exposure of California kindergartners to students with personal belief exemptions from mandated school entry vaccinations. Am J Public Health. 2012;102(8):e59–e67. doi: 10.2105/AJPH.2012.300821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Import-associated measles outbreak—Indiana, May–June 2005. MMWR Morb Mortal Wkly Rep. 2005;54(42):1073–1075. [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Brief report: imported measles case associated with nonmedical vaccine exemption—Iowa, March 2004. MMWR Morb Mortal Wkly Rep. 2004;53(11):244–246. [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Two measles outbreaks after importation—Utah, March–June 2011. MMWR Morb Mortal Wkly Rep. 2013;62(12):222–225. [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Measles outbreak—Southwestern Utah, 1996. MMWR Morb Mortal Wkly Rep. 1997;46(33):766–769. [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Measles—United States, January 1–April 25, 2008. MMWR Morb Mortal Wkly Rep. 2008;57(18):494–498. [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention. Update: measles—United States, January–July 2008. MMWR Morb Mortal Wkly Rep. 2008;57(33):893–896. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Vaccination coverage among children in kindergarten—United States, 2009–10 school year. MMWR Morb Mortal Wkly Rep. 2011;60(21):700–704. [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Vaccination coverage among children in kindergarten—United States, 2011–12 school year. MMWR Morb Mortal Wkly Rep. 2012;61(33):647–652. [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. Vaccination coverage among children in kindergarten—United States, 2012–13 school year. MMWR Morb Mortal Wkly Rep. 2013;62(30):607–612. [PMC free article] [PubMed] [Google Scholar]
- 29.Ernst KC, Jacobs ET. Implications of philosophical and personal belief exemptions on re-emergence of vaccine-preventable disease: the role of spatial clustering in under-vaccination. Hum Vaccin Immunother. 2012;8(6):838–841. doi: 10.4161/hv.19743. [DOI] [PubMed] [Google Scholar]
- 30.Fair E, Murphy TV, Golaz A, Wharton M. Philosophic objection to vaccination as a risk for tetanus among children younger than 15 years. Pediatrics. 2002;109(1):E2. doi: 10.1542/peds.109.1.e2. [DOI] [PubMed] [Google Scholar]
- 31.Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE. Individual and community risks of measles and pertussis associated with personal exemptions to immunization. JAMA. 2000;284(24):3145–3150. doi: 10.1001/jama.284.24.3145. [DOI] [PubMed] [Google Scholar]
- 32.Parker Fiebelkorn A, Redd SB, Gallagher K et al. Measles in the United States during the postelimination era. J Infect Dis. 2010;202(10):1520–1528. doi: 10.1086/656914. [DOI] [PubMed] [Google Scholar]
- 33.Gaudino JA, Robison S. Risk factors associated with parents claiming personal-belief exemptions to school immunization requirements: community and other influences on more skeptical parents in Oregon, 2006. Vaccine. 2012;30(6):1132–1142. doi: 10.1016/j.vaccine.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Gullion JS, Henry L, Gullion G. Deciding to opt out of childhood vaccination mandates. Public Health Nurs. 2008;25(5):401–408. doi: 10.1111/j.1525-1446.2008.00724.x. [DOI] [PubMed] [Google Scholar]
- 35.Gust DA, Kennedy A, Shui I, Smith PJ, Nowak G, Pickering LK. Parent attitudes toward immunizations and healthcare providers: the role of information. Am J Prev Med. 2005;29(2):105–112. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 36.Gust DA, Kennedy A, Weber D, Evans G, Kong Y, Salmon D. Parents questioning immunization: evaluation of an intervention. Am J Health Behav. 2009;33(3):287–298. doi: 10.5993/ajhb.33.3.7. [DOI] [PubMed] [Google Scholar]
- 37.Imdad A, Tserenpuntsag B, Blog DS, Halsey NA, Easton DE, Shaw J. Religious exemptions for immunization and risk of pertussis in New York State, 2000–2011. Pediatrics. 2013;132(1):37–43. doi: 10.1542/peds.2012-3449. [DOI] [PubMed] [Google Scholar]
- 38.Kennedy AM, Brown CJ, Gust DA. Vaccine beliefs of parents who oppose compulsory vaccination. Public Health Rep. 2005;120(3):252–258. doi: 10.1177/003335490512000306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kennedy AM, Gust DA. Measles outbreak associated with a church congregation: a study of immunization attitudes of congregation members. Public Health Rep. 2008;123(2):126–134. doi: 10.1177/003335490812300205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Luthy KE, Beckstrand RL, Callister LC, Cahoon S. Reasons parents exempt children from receiving immunizations. J Sch Nurs. 2012;28(2):153–160. doi: 10.1177/1059840511426578. [DOI] [PubMed] [Google Scholar]
- 41.Luthy KE, Beckstrand RL, Meyers CJH. Common perceptions of parents requesting personal exemption from vaccination. J Sch Nurs. 2013;29(2):95–103. doi: 10.1177/1059840512455365. [DOI] [PubMed] [Google Scholar]
- 42.Mergler MJ, Omer SB, Pan WKY et al. Association of vaccine-related attitudes and beliefs between parents and health care providers. Vaccine. 2013;31(41):4591–4595. doi: 10.1016/j.vaccine.2013.07.039. [DOI] [PubMed] [Google Scholar]
- 43.Omer SB, Enger KS, Moulton LH, Halsey NA, Stokley S, Salmon DA. Geographic clustering of nonmedical exemptions to school immunization requirements and associations with geographic clustering of pertussis. Am J Epidemiol. 2008;168(12):1389–1396. doi: 10.1093/aje/kwn263. [DOI] [PubMed] [Google Scholar]
- 44.Omer SB, Pan WK, Halsey NA et al. Nonmedical exemptions to school immunization requirements: secular trends and association of state policies with pertussis incidence. JAMA. 2006;296(14):1757–1763. doi: 10.1001/jama.296.14.1757. [DOI] [PubMed] [Google Scholar]
- 45.Omer SB, Richards JL, Ward M, Bednarczyk RA. Vaccination policies and rates of exemption from immunization, 2005–2011. N Engl J Med. 2012;367(12):1170–1171. doi: 10.1056/NEJMc1209037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Peterson RM, Cook C, Yerxa ME, Marshall JH, Pulos E, Rollosson MP. Improving immunization coverage in a rural school district in Pierce County, Washington. J Sch Nurs. 2012;28(5):352–357. doi: 10.1177/1059840512446069. [DOI] [PubMed] [Google Scholar]
- 47.Richards JL, Wagenaar BH, Van Otterloo J et al. Nonmedical exemptions to immunization requirements in California: a 16-year longitudinal analysis of trends and associated community factors. Vaccine. 2013;31(29):3009–3013. doi: 10.1016/j.vaccine.2013.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rota JS, Salmon DA, Rodewald LE, Chen RT, Hibbs BF, Gangarosa EJ. Processes for obtaining nonmedical exemptions to state immunization laws. Am J Public Health. 2001;91(4):645–648. doi: 10.2105/ajph.91.4.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salmon DA, Haber M, Gangarosa EJ, Phillips L, Smith NJ, Chen RT. Health consequences of religious and philosophical exemptions from immunization laws: individual and societal risk of measles. JAMA. 1999;282(1):47–53. doi: 10.1001/jama.282.1.47. [DOI] [PubMed] [Google Scholar]
- 50.Salmon DA, Moulton LH, Omer SB, deHart M, Stokley S, Halsey NA. Factors associated with refusal of childhood vaccines among parents of school-aged children: a case-control study. Arch Pediatr Adolesc Med. 2005;159(5):470–476. doi: 10.1001/archpedi.159.5.470. [DOI] [PubMed] [Google Scholar]
- 51.Salmon DA, Moulton LH, Omer SB et al. Knowledge, attitudes, and beliefs of school nurses and personnel and associations with nonmedical immunization exemptions. Pediatrics. 2004;113(6):e552–e559. doi: 10.1542/peds.113.6.e552. [DOI] [PubMed] [Google Scholar]
- 52.Salmon DA, Omer SB, Moulton LH et al. Exemptions to school immunization requirements: the role of school-level requirements, policies, and procedures. Am J Public Health. 2005;95(3):436–440. doi: 10.2105/AJPH.2004.046201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Salmon DA, Sotir MJ, Pan WK et al. Parental vaccine refusal in Wisconsin: a case-control study. WMJ. 2009;108(1):17–23. [PMC free article] [PubMed] [Google Scholar]
- 54.Smith PJ, Chu SY, Barker LE. Children who have received no vaccines: who are they and where do they live? Pediatrics. 2004;114(1):187–195. doi: 10.1542/peds.114.1.187. [DOI] [PubMed] [Google Scholar]
- 55.Sugerman DE, Barskey AE, Delea MG et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally undervaccinated. Pediatrics. 2010;125(4):747–755. doi: 10.1542/peds.2009-1653. [DOI] [PubMed] [Google Scholar]
- 56.Thompson JW, Tyson S, Card-Higginson P et al. Impact of addition of philosophical exemptions on childhood immunization rates. Am J Prev Med. 2007;32(3):194–201. doi: 10.1016/j.amepre.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 57.Wenger OK, McManus MD, Bower JR, Langkamp DL. Underimmunization in Ohio’s Amish: parental fears are a greater obstacle than access to care. Pediatrics. 2011;128(1):79–85. doi: 10.1542/peds.2009-2599. [DOI] [PubMed] [Google Scholar]
- 58.Centers for Disease Control and Prevention. The School Entry Immunization Assessment Report. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Immunization and Respiratory Diseases; 2005. [Google Scholar]
- 59.National Conference of State Legislatures. States with religious and philosophical exemptions from school immunization requirements. 2012. Available at: http://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx. Accessed August 4, 2014.
- 60.May T, Silverman RD. “Clustering of exemptions” as a collective action threat to herd immunity. Vaccine. 2003;21(11–12):1048–1051. doi: 10.1016/s0264-410x(02)00627-8. [DOI] [PubMed] [Google Scholar]
- 61.Glanz JM, McClure DL, Magid DJ et al. Parental refusal of pertussis vaccination is associated with an increased risk of pertussis infection in children. Pediatrics. 2009;123(6):1446–1451. doi: 10.1542/peds.2008-2150. [DOI] [PubMed] [Google Scholar]
- 62.Glanz JM, McClure DL, Magid DJ, Daley MF, France EK, Hambidge SJ. Parental refusal of varicella vaccination and the associated risk of varicella infection in children. Arch Pediatr Adolesc Med. 2010;164(1):66–70. doi: 10.1001/archpediatrics.2009.244. [DOI] [PubMed] [Google Scholar]
- 63.Glanz JM, McClure DL, O’Leary ST et al. Parental decline of pneumococcal vaccination and risk of pneumococcal related disease in children. Vaccine. 2011;29(5):994–999. doi: 10.1016/j.vaccine.2010.11.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Washington State Department of Health. Vaccine exemption rates for school entry drop due to new state requirements. 2012. Available at: http://www.doh.wa.gov/Newsroom/2012NewsReleases/12061VaccineExemptionDecrease.aspx. Accessed August 4, 2014.
- 65.AB-2109 communicable disease: immunization exemption. 2012. Available at: http://leginfo.legislature.ca.gov/faces/billNavClient.xhtml?bill_id=201120120AB2109. Accessed August 4, 2014.
- 66.Brown E. AB 2109 signing message. 2012. Available at: http://gov.ca.gov/docs/AB_2109_Signing_Message.pdf. Accessed January 10, 2013.
- 67.Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011;378(9790):526–535. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
- 68.Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB. A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine. 2013;31(40):4293–4304. doi: 10.1016/j.vaccine.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 69.Salmon DA, Teret SP, MacIntyre CR, Salisbury D, Burgess MA, Halsey NA. Compulsory vaccination and conscientious or philosophical exemptions: past, present, and future. Lancet. 2006;367(9508):436–442. doi: 10.1016/S0140-6736(06)68144-0. [DOI] [PubMed] [Google Scholar]
- 70.Buttenheim AM, Cherng ST, Asch DA. Provider dismissal policies and clustering of vaccine-hesitant families: an agent-based modeling approach. Hum Vaccin Immunother. 2013;9(8):1819–1824. doi: 10.4161/hv.25635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pan R, Wolk L, Fuentes F. Communicable disease: immunization exemption. 2012. Available at: http://www.leginfo.ca.gov/pub/11-12/bill/asm/ab_2101-2150/ab_2109_bill_20120223_introduced.pdf. Accessed August 4, 2014.
- 72.Keiser K, Honeyford J, Becker R. Certification of enrollment. 2011. Available at: http://apps.leg.wa.gov/documents/billdocs/2011-12/Pdf/Bills/Senate%20Passed%20Legislature/5005.PL.pdf. Accessed August 4, 2014.
- 73.Mullin K. An act relating to immunization exemptions and the immunization pilot program. 2012. Available at: http://www.leg.state.vt.us/docs/2012/Acts/ACT157.PDF. Accessed August 4, 2014.