Abstract
Mixed adenoneuroendocrine carcinoma (MANEC) is exceedingly rare with a poor outcome. In this article, we reported a MANEC in a 68-year-old woman with a symptom of abdominal pain and distension. MANEC derived from the ascending colon with highly aggressive behavior. The diagnosis and distinguish of MANEC must base on histological findings and immunohistochemical findings. In this case, microscopic observation showed tumor cells were arranged in conglobate and nested by fibrous tissue with a visible cell atypia and mitotic. NEC-like and exocrine glandular cells were also been seen in a single neoplasm. MANEC tissues were immunopositive for CK, CK20, P53, CK7, CDX-2, Ki-67 (70%+), E-cad, CD56, CEA, Syn, villin and CgA, and immunonegative for CA125, NSE, ER and PR. Here, the patient was treated by surgical operation and was followed-up near 3 months, no local recurrence and distant metastasis.
Keywords: Mixed adenoneuroendocrine carcinoma, ascending colon, immunohistochemistry
Introduction
Neuroendocrine neoplasms (NENs) arise from endodermal cells, ranging from well-differentiated carcinoids to poorly differentiated neuroendocrine carcinomas (NECs) [1-3]. NEC is a very rare, highly aggressive and poorly prognostic carcinoma and squamous cell carcinoma (SqCC), in which included an additional significant proportion of malignant exocrine glandular cells termed as mixed adenoneuroendocrine carcinoma (MANEC) [2-6]. MANEC is thought to derive from multi-potential stem cells, which have differentiated bidirectionally. According to biclonal transformation of two separate but adjacent neoplasms and multi-directional differentiation of a single neoplasm, MANEC are further classified into collision and composite types [1,6]. Here, we report a composite MANEC in ascending colon with clinical serosal invasion, and the patient was treated by surgical operation and was followed-up near 3 months, no local recurrence and distant metastasis.
Case report
A 68-year-old woman with a symptom of unexplained abdominal pain and paroxysmal aggravation with nausea and vomiting last for 3 days visited Taiping People’s Hospital of Dongguan. Specialist examination showed no chills, no fever, no diarrhea, no jaundice and without frequent micturition, besides a symptoms of decreased appetite. There is no past history of hepatitis, tuberculosis, typhoid fever and other infectious disease, as well as coronary heart disease, hypertension and diabetes. Laboratory tests revealed an obviously rising carcinoembryonic antigen (CEA) level (6.59 ng/ml) and alpha fetoprotein(AFP) level (16.94 IU/ml), but carbohydrate antigen (CA) 15-3 level (6.96 U/ml), CA 125 level (7.90 U/ml), CA 19-9 level (< 0.6 U/ml) and CA 72-4 level (4.68 U/ml) were within normal limits. The patient was diagnosed as ascending colon tumor. An intestinal tube measured 30 cm×13 cm×4.5 cm in diameter, and an appendix measured 7.5 cm×0.8 cm×0.5 cm in diameter on ileocecal valve were taken out (Figure 1A). And a hump shaped mass measured 6 cm×6 cm×6 cm in volume on the ascending colon with clinical serosal invasion was obvious, 7.5 cm in distance away from ileocecal valve. The tumor tissues were stained with hematoxylin and eosin (Figure 1B and 1C). Microscopic observation showed tumor cells were arranged in conglobate and nested by fibrous tissue. A visible cell atypia and mitotic was easy to see on the tumor cells. NEC-like cells in a typical mass comprised infiltrative nests of small uniform tumor cells, and exocrine glandular cells with NEC-like cells were been seen in a single neoplasm. Tumor tissues were immunopositive for CK (+++), CK20 (++), P53 (+++), CK7 (+++), CDX-2 (+), Ki-67 (70%+), E-cad (+++), CD56 (partly+), CEA (++), Syn (partly+), villin (+++) and CgA (partly++), and immunonegative for CA125 (-), NSE (-), ER (-) and PR (-) (Figure 2). According to histopathological and immunohistochemical findings, this patient was diagnosed as an ascending colon mixed adenoneuroendocrine carcinoma with clinical serosal invasion.
Figure 1.
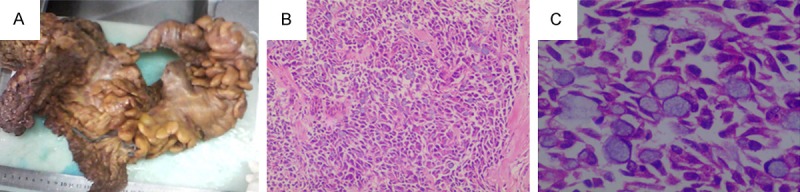
The MANEC tissues were stained with hematoxylin and eosin. A. An intestinal tube and an appendix on ileocecal valve were taken out from patient after surgical operation; B. Tumor cells were arranged in conglobate and nested by fibrous tissue. NEC-like and exocrine glandular cells were also been seen in a single neoplasm (40×); C. A visible cell atypia and mitotic was easy to see on the tumor cells (100×).
Figure 2.
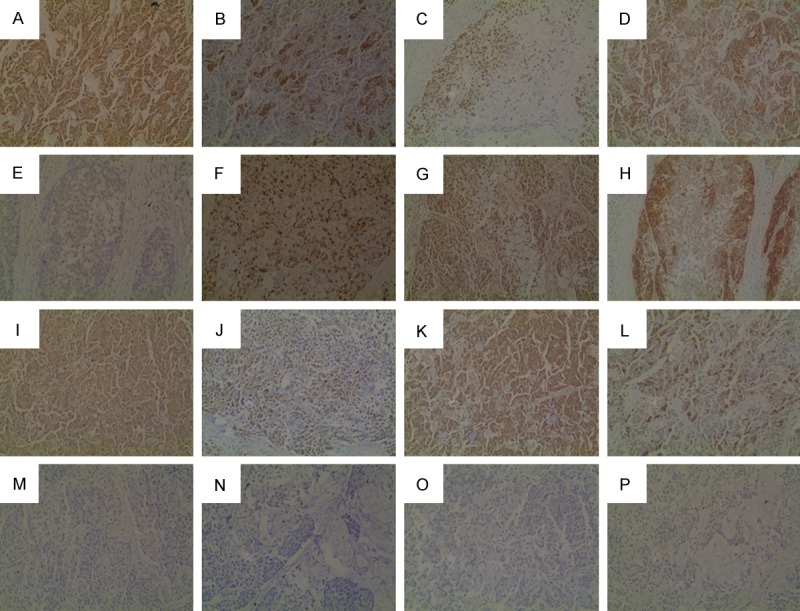
MANEC tissues were stained with immunohistochemistry. The tissues were immunopositive for CK (A), CK20 (B), P53 (C), CK7 (D), CDX-2 (E), Ki-67 (F), E-cad (G), CD56 (H), CEA (I), Syn (J), villin (K), CgA (L) and immunonegative for CA125 (M), NSE (N), ER (O), PR (P) in MANEC tissues (100×).
Discussion
Neuroendocrine carcinomas (NECs) arising in the ascending colon are rare neoplasms with highly aggressive behavior [2-5]. Here, we report a case of NEC mixed with adenocarcinoma, named mixed adenoneuroendocrine carcinoma (MANEC), in the ascending colon. MANEC was first described by the Cardier in 1924. However, until in 2011, a new WHO classification of digestive neuroendocrine tumors classified it as five main digestive neuroendocrine neoplasms categories along with neuroendocrine tumor G1, neuroendocrine tumor G2, small cell type neuroendocrine carcinoma and large cell type neuroendocrine carcinoma [1]. MANEC is exceedingly rare, and the location of MANEC influences the treatment and outcome. Most of them arise in the gastro-intestinal tract like stomach, colon, esophagogastric junction and cecum, also arise in the gallbladder, bile duct, ampulla, appendix and uterine cervix [7-14]. MANEC is thought to derive from multi-potential stem cells, which have differentiated bidirectionally. So the diagnosis and distinguish of MANEC must base on histological findings and immunohistochemical findings. In this case, microscopic observation showed tumor cells were arranged in conglobate and nested by fibrous tissue with a visible cell atypia and mitotic. NEC-like and exocrine glandular cells were also been seen in a single neoplasm. MANEC tissues were immunopositive for CK (+++), CK20 (++), P53 (+++), CK7 (+++), CDX-2 (+), Ki-67 (70%+), E-cad (+++), CD56 (partly+), CEA (++), Syn (partly+), villin (+++) and CgA (partly++), and immunonegative for CA125 (-), NSE (-), ER (-) and PR (-). According to histopathological and immunohistochemical findings, this case was diagnosed as an ascending colon mixed adenoneuroendocrine carcinoma with clinical serosal invasion.
MANEC along with neuroendocrine tumor G1 (G1 NET), G2 NET, small cell type NEC and large cell type NEC are five main digestive neuroendocrine neoplasms categories [1]. So, it is important to distinguish MANEC from them. Neuroendocrine neoplasms (NENs) including NET and NEC arise from endodermal cells. These cells have monomorphous endocrine cells, sharing common features such as looking similar, producing biogenic amines and polypeptide hormones [15]. NENs range from well-differentiated carcinoids to poorly differentiated NECs, which included an additional significant proportion of malignant exocrine glandular cells termed as MANEC. The monomorphous endocrine cells of MANEC have a characteristic of bidirectional differentiation. So, exocrine glandular cells are the key points of MANEC distinguish from other NENs. MANEC are further classified into collision and composite types. Collision tumors have two different histologic patterns from endocrine cells and exocrine cells in close contact, resulting from biclonal transformation of two separate but adjacent neoplasms. However, composite tumors, the endocrine and exocrine cells are intermixed within the same tumor, arising through multi-directional differentiation of a single neoplasm [6]. Our case was a composite tumor.
NCCN clinical practice guideline indicated patients with the neuroendocrine tumor could treat by palliative operation, adjuvant chemotherapy and somatostatin analogue [2]. And, location of the MANEC influences the treatment and outcome. Ito et al. [16] reported a 39-year-old woman with colonic MANEC died on postoperative day 110, even if the combined use of chemotherapy. Marando et al. [17] also reported a 65-year-old male with colonic MANEC died on postoperative 1 month. Ascending colon MANEC is an uncommon tumor with a strong malignant potential and an extremely poor prognosis. Here, the patient was treated by surgical operation and was followed-up near 3 months, no local recurrence and distant metastasis.
Acknowledgements
This work was supported by the Science and Technology Project of Dongguan (20131051010006) and the Science and Technology Fund of Guangdong Medical College (XK1454).
Disclosure of conflict of interest
None.
References
- 1.Scoazec JY, Couvelard A pour le réseau TENpath (réseau national d’expertise pour le diagnostic anatomopathologique des tumeurs neuroendocrines malignes de l’adulte, sporadiques et familiales) [The new WHO classification of digestive neuroendocrine tumors] Ann Pathol. 2011;31:88–92. doi: 10.1016/j.annpat.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Clark OH, Benson AR, Berlin JD, Choti MA, Doherty GM, Engstrom PF, Gibbs JF, Heslin MJ, Kessinger A, Kulke MH Kvols L, Salem R, Saltz L, Shah MH, Shibata S, Strosberg JR, Yao JC NCCN Neuroendocrine Tumos Panel Members. NCCN Clinical Practice Guidelines in Oncology: neuroendocrine tumors. J Natl Compr Canc Netw. 2009;7:712–747. doi: 10.6004/jnccn.2009.0050. [DOI] [PubMed] [Google Scholar]
- 3.Wang HY, Zou J, Zhou GY, Yan JQ, Liu SX. Primary small cell neuroendocrine carcinoma of the tonsil: a case report and review of the literature. Int J Clin Exp Pathol. 2014;7:2678–82. [PMC free article] [PubMed] [Google Scholar]
- 4.Ishida M, Iwai M, Kagotani A, Iwamoto N, Okabe H. Cutaneous metastasis from pulmonary large cell neuroendocrine carcinoma in the scalp. Int J Clin Exp Pathol. 2014;7:2701–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Yang L, Sun X, Zou Y, Meng X. Small cell type neuroendocrine carcinoma colliding with squamous cell carcinoma at esophagus. Int J Clin Exp Pathol. 2014;7:1792–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Jain A, Singla S, Jagdeesh KS, Vishnumurthy HY. Mixed adenoneuroendocrine carcinoma of cecum: a rare entity. J Clin Imaging Sci. 2013;3:10. doi: 10.4103/2156-7514.107995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nemoto H, Tate G, Yokomizo K, Umemoto T, Matsubara T, Mizukami H, Kigawa G, Matsumiya A, Tanaka J. Gastric mixed adenoneuroendocrine carcinoma occurring 50 years after a gastroenterostomy with braun anastomosis. Case Rep Oncol. 2014;7:330–6. doi: 10.1159/000363222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levi Sandri GB, Carboni F, Valle M, Visca P, Garofalo A. Mixed adenoneuroendocrine gastric carcinoma: a case report and review of the literature. J Gastric Cancer. 2014;14:63–6. doi: 10.5230/jgc.2014.14.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L, Demay RM. Cytological features of mixed adenoneuroendocrine carcinoma of the ampulla: Two case reports with review of literature. Diagn Cytopathol. 2014 Feb 19; doi: 10.1002/dc.23107. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Veits L, Lang-Schwarz C, Volkholz H, Falkeis C, Vieth M, Schulz H. Mixed adenoneuroendocrine carcinoma (MANEC) of the esophagogastric junction predominantly consisting of poorly differentiated neuroendocrine carcinoma. Endoscopy. 2013;45(Suppl 2 UCTN):E16–7. doi: 10.1055/s-0032-1326113. [DOI] [PubMed] [Google Scholar]
- 11.Nishimura C, Naoe H, Hashigo S, Tsutsumi H, Ishii S, Konoe T, Watanabe T, Shono T, Sakurai K, Takaishi K, Ikuta Y, Chikamoto A, Tanaka M, Iyama K, Baba H, Katabuchi H, Sasaki Y. Pancreatic metastasis from mixed adenoneuroendocrine carcinoma of the uterine cervix: a case report. Case Rep Oncol. 2013;6:256–62. doi: 10.1159/000351308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onishi I, Kitagawa H, Harada K, Maruzen S, Sakai S, Makino I, Hayashi H, Nakagawara H, Tajima H, Takamura H, Tani T, Kayahara M, Ikeda H, Ohta T, Nakanuma Y. Intraductal papillary neoplasm of the bile duct accompanying biliary mixed adenoneuroendocrine carcinoma. World J Gastroenterol. 2013;19:3161–4. doi: 10.3748/wjg.v19.i20.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain A, Singla S, Jagdeesh KS, Vishnumurthy HY. Mixed adenoneuroendocrine carcinoma of cecum: a rare entity. J Clin Imaging Sci. 2013;3:10. doi: 10.4103/2156-7514.107995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shintaku M, Kataoka K, Kawabata K. Mixed adenoneuroendocrine carcinoma of the gallbladder with squamous cell carcinomatous and osteosarcomatous differentiation: report of a case. Pathol Int. 2013;63:113–9. doi: 10.1111/pin.12029. [DOI] [PubMed] [Google Scholar]
- 15.Klimstra DS, Modlin IR, Coppola D, Lloyd RV, Suster S. The pathologic classification of neuroendocrine tumors: a review of nomenclature, grading, and staging systems. Pancreas. 2010;39:707–12. doi: 10.1097/MPA.0b013e3181ec124e. [DOI] [PubMed] [Google Scholar]
- 16.Ito H, Kudo A, Matsumura S, Ban D, Irie T, Ochiai T, Nakamura N, Tanaka S, Tanabe M. Mixed adenoneuroendocrine carcinoma of the colon progressed rapidly after hepatic rupture: report of a case. Int Surg. 2014;99:40–4. doi: 10.9738/INTSURG-D-13-00161.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marando A, Dainese E, La Rosa S, Capella C. Images in endocrine pathology: oncocytic differentiation in a mixed adenoneuroendocrine carcinoma of the colon. Endocr Pathol. 2013;24:54–6. doi: 10.1007/s12022-012-9201-3. [DOI] [PubMed] [Google Scholar]


