Abstract
The objectives of this study were to understand how different types of barriers to adherence to antiretroviral therapy (ART) were related and their differential impact on objectively measured adherence over time. Data from 151 patients taking ART were used to describe four sub-types of self-reported adherence barriers: medication and health concerns (MHC), stigma (S), family responsibilities (FR), and problems with schedule and routine (PSR). Generalized linear models with generalized estimating equations (GEE) were used to examine the impact of barriers on adherence over time. The sample was 25% female, mean age 42 years, with 26% African-American and 20% Hispanic. The overall average adherence was 73%. Patients reported at least one PSR barrier in 66% of study visits, MHC in 40%, S in 17%, and FR in 6%. In 40% of visits, patients reported two or more barrier sub-types. There were statistically significant (p<0.05) decreases of 3.9, 2.5, and 2.4 in percent adherence, for MHC, PSR, and S, respectively, per unit increase in barrier score. Interventions to address different types of patient-identified barriers to ART adherence using targeted approaches are needed.
Keywords: Barriers, Adherence, Medication, HIV/AIDS, Antiretroviral Therapy (ART)
INTRODUCTION
Adherence to antiretroviral therapy (ART) is critical to viral suppression and maintaining health status and quality of life among patients living with HIV (1). Research has repeatedly shown, however, that many patients struggle with achieving and/or maintaining optimal adherence (2). Given that treatment with ART is long term and lifelong for most patients, it is critical to understand what barriers patients face in adhering to ART over time in order to design interventions that best promote and maintain adherence.
There is a large body of research examining the correlates and predictors of adherence among patients in the US, detailed in several reviews (3-5). However, although a number of mostly cross-sectional studies have examined patient-identified barriers to adherence (2), results have been primarily descriptive in nature and there has been less research to understand how different types of adherence barriers are related to one another. Several qualitative studies have addressed this gap by describing broad categories of barriers including patient characteristics and health beliefs, the healthcare provider-patient relationship, the healthcare system, and issues related to the medication regimen (6-11,11-13). Also frequently cited by patients and researchers are stigma and the social environment within which the patient lives (14).
There is limited quantitative research, however, on how self-reported barriers relate to one another, how they may change over time, and how they differentially predict objectively measured adherence. This additional information about patient-identified barriers is critical for clinicians to understand if they are to provide effective and efficient counseling to their patients using ART. Understanding how barriers relate to each other is important because patients who report one kind of adherence barrier may also report other seemingly unrelated barriers. Knowing if and how barriers change over time helps to determine how often assessment of barriers is needed and whether it is necessary to fully explore all potential barriers at each patient visit. If certain barriers are more strongly related to adherence, it may be worth prioritizing these concerns during adherence counseling.
The objective of this study, therefore, was to examine self-reported barriers to adherence among patients currently taking ART. The four main goals of this analysis were to: 1) determine the frequency of different types of barriers identified by patients, 2) examine how different types of barriers were correlated and how often patients reported multiple types of barriers, 3) determine whether barriers changed over time, and 4) estimate the impact of barriers on adherence. Related to this final goal, we examined the impact of both the type and frequency of different self-reported barriers on objectively measured adherence to ART.
METHODS
Study sample
Data for the current study were from a randomized controlled trial of an intervention that provided short adherence reports at routine visits to clinicians in order to increase patient adherence through improved dialogue with providers about adherence behaviors. Details about the study are provided elsewhere (15). Briefly, patients were recruited from two academic medical centers, a community health center, a general medicine practice, and a private infectious disease practice in the New England area. Eligibility requirements included current use of ART, detectable HIV-RNA at the most recent clinical visit, willingness to use an electronic pill bottle cap for monitoring ART use, and fluency in English. Enrollment occurred between November 2002 and January 2005. Participation in the trial included a baseline visit and five additional visits, with randomization occurring at the third visit. The intervention was found to have no impact on adherence (15). Assessment of adherence barriers occurred at the randomization visit and each subsequent study visit.
Study measures and data collection
Data presented here includes socio-demographic and other patient characteristics, self-reported barriers, and adherence data from randomization through the final study visit. Socio-demographic information was collected by interviewer-administered survey and included sex, age, race/ethnicity, education, employment (prior 30 days), and sexual identity. Additional information was collected regarding risk behaviors including frequency of alcohol in the prior 30 days, history of drug use (i.e., ever used cocaine, heroin, amphetamines, Ecstasy, G, K, or methadone), HIV transmission risk factors (i.e., sex with a man, sex with a woman, injection drug use, other), and current homelessness. Depression in the prior 30 days was assessed using the Primary Care Screener for Affective Disorder (PC-SAD) (16). Time on ART was assessed by self-reported length of time on the current ART regimen.
A literature search was conducted to identify existing measures of barriers to adherence to ART. Questions regarding barriers to ART adherence were taken primarily from the AIDS Clinical Trials Group assessments. Items consisted of statements that participants were asked to score how often a given barrier had prevented them from taking their ART in the prior 30 days according to a 4-point scale where 0 indicated “never,” 1 indicated “rarely,” 2 indicated “sometimes,” and 3 indicated “often.” We performed cognitive testing on all survey items prior to their first administration in the study.
Items were organized and categorized into four broad types of barriers a priori: medication-specific concerns, health and well-being concerns, social environment, and problems with schedule and routine. In order to examine the hypothesized sub-types of barriers and determine how to group them for comparative analysis, factor analysis with orthogonal (varimax) rotation was conducted on 23 items. From this initial factor analysis, four factors were identified with eigenvalues greater than 1. Factor analysis was repeated specifying four factors. We specified a priori that items with factor loadings of 0.40 or higher and uniqueness values of 0.80 or below would be included as items in the sub-scale. Two items did not load on any factor and were therefore excluded from future analysis, leaving 21 items. The four factors confirmed the hypothesized categories with the following exceptions: the medication-specific and health and well-being categories were combined into one factor and the social environment items were split into two factors separately representing stigma and family responsibilities. In addition, one item hypothesized to be in the problems with schedule and routine group (problems taking pills at specified time, with meals, on empty stomach, etc.) loaded onto the medication and health concerns factor. The results of this analysis left us with the following four factors: medication and health concerns, stigma, family responsibilities and problems with schedule/routine.
Table 1 presents the individual items within each sub-scale and the reliability measures for each of the four identified factors. The internal consistency of three of the measures ranged from good to acceptable, with Cronbach’s alpha scores of 0.86 for problems with schedule and routine, 0.86 for medication and health concerns, and 0.75 for stigma. The alpha for family responsibilities was borderline acceptable at 0.62. It is important to note, however, that many patients without partners or children responded “not applicable” to these items since the statements referred specifically to these types of family members. In addition this factor contained only 2 items, decreasing the reliability rating. Therefore, we retained the family responsibility sub-scale in the analysis for exploratory purposes only. We created summary scores by totaling each item score within each sub-scale. Since the sub-scales had different numbers of items, scores were rescaled to correspond to a 0-10 scale in order to increase comparability across sub-scales.
Table 1.
Percents of visitsa with responses to items from four sub-scales of barriers to ART adherence, Cronbach’s alpha for reliability of sub-scales, and mean and standard deviation (SD)b of total sub-scale scores.
| Item | Never | Rarely | Sometimes | Often | Cronbach’s alpha |
Mean sub- scale score b (SD) |
|---|---|---|---|---|---|---|
| Medication and health concerns | 0.86 | 0.9 (1.7) | ||||
|
| ||||||
| Had too many pills to take | 86 | 4 | 3 | 1 | ||
| Wanted to avoid side effects | 82 | 4 | 5 | 3 | ||
| Felt like the drug was toxic/harmful | 85 | 4 | 5 | 2 | ||
| Felt sick or ill | 78 | 6 | 10 | 2 | ||
| Felt depressed/overwhelmed | 78 | 5 | 9 | 4 | ||
| Stopped because felt good | 85 | 4 | 6 | 2 | ||
| Problems taking pill at specified times (with meals, on empty stomach, etc.) |
73 | 9 | 10 | 4 | ||
|
| ||||||
| Stigma | 0.75 | 0.5 (1.5) | ||||
|
| ||||||
| Did not want others to notice you taking medication | 81 | 6 | 4 | 3 | ||
| Don’t want people live with to know you have HIV | 74 | 2 | 2 | 1 | ||
| Don’t want people work with to know you have HIV | 62 | 1 | 2 | 3 | ||
|
| ||||||
| Family responsibilities | 0.62 | 0.2 (1.1) | ||||
|
| ||||||
| Taking care of children | 70 | 1 | 1 | 0.4 | ||
| Taking care of partner, spouse, parent | 78 | 1 | 2 | 1 | ||
|
| ||||||
| Problems with schedule and routine | 0.86 | 1.4 (1.6) | ||||
|
| ||||||
| Away from home | 60 | 18 | 14 | 2 | ||
| Simply forgot | 50 | 23 | 21 | 3 | ||
| Busy doing other things | 60 | 19 | 16 | 3 | ||
| Change in daily routine | 70 | 12 | 12 | 2 | ||
| Fell asleep/slept through dose | 65 | 17 | 13 | 2 | ||
| On vacation | 63 | 5 | 3 | 0.4 | ||
| Having a good time | 78 | 8 | 8 | 0.4 | ||
| Out late | 69 | 14 | 11 | 1 | ||
| Intoxicated by drugs/alcohol | 75 | 7 | 7 | 0 | ||
Percents do not add to 100 because of missing and N/A responses
Average total scores were calculated and transformed to 0-10 scale as follows: total score of items in sub-scale (where never = 0, rarely = 1, sometimes = 2, often = 3)/3 × number of items in the sub-scale × 10)
Adherence was measured using electronic monitoring. For one chosen medication for each patient, the Medication Event Monitoring System (MEMS) system recorded the date and the time of each bottle opening. We limited monitoring to daily or twice daily regimens. The medication within the regimen was selected for monitoring according to the following prioritization: protease-inhibitors (PI), non-nucleoside reverse transcriptase inhibitors (NNRTIs) nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs). Adherence was summarized as covered time, calculated as the percent of the time in an interval that was covered by medication. Uncovered time began accumulating in the interval 3 hours following the expected next dose (i.e., 27 hours for once a day medication and 15 hours for twice a day). Adherence was expressed as a percentage and calculated as the total minutes in the 30 days prior to a study visit minus the number of uncovered minutes in the same interval, divided by the total minutes in the interval × 100.
Statistical Analysis
The unit of analysis was the study visit. Standard descriptive statistics were used to characterize the sample, examine the frequencies of the items in each sub-scale, the mean barrier scores overall and at each visit. We examined the frequency of each reported barrier by creating dichotomous variables to indicate whether any barrier within the sub-scale had been reported at the study visit. We examined the frequency of reporting any barriers using stacked bar charts. To examine overlap in reporting of each type of barrier, we then generated a variable to determine whether the individual had reported any barrier on any other sub-scale. We plotted the number of reported types of barriers (ranging from 0-4) using bar charts. The correlations between average sub-scale scores were examined using Pearson’s correlation coefficients to further determine how types of barriers were related to each other. To determine whether there were changes in barriers over time, we examined visit-to-visit changes in whether or not individuals reported any of the barriers in each sub-scale using logistic regression with generalized estimating equations (GEE) to account for correlation of repeated measures over time.
We fit generalized linear models with GEE to examine the effect of each barrier type on adherence. Adherence was modeled as a continuous variable from 0 to 100. Each barrier was included in models as a continuous variable representing the total sub-scale score, with scores transformed to 0 to 10. Age in years and duration on ART in months were included as continuous variables. Depression was also included as a continuous variable ranging from 0 to 9, representing the number of depressive symptoms reported on the PC-SAD. Race was included as a dummy variable with the following categories: Asian, Black (non-Hispanic), Hispanic, Other, and White was the referent group. Highest educational attainment was included as a dummy variable with the following categories: grade school, college, graduate/professional school, and completion of high school as the referent group (this group was the largest). Sex (female vs. male), alcohol use (daily/nearly daily/3-4 times per week vs. less frequent), drug use (any vs. none), and intervention group assignment (treatment vs. control) per visit were included in the model as dichotomous variables. Time was included as a fixed factor representing four study visits with the last visit as the reference group.
We first fit a base model including study visits and intervention group to account for the study design and potential confounders including socio-demographic characteristics (i.e., age, sex, race/ethnicity, educational attainment, employment), risk behaviors (i.e., alcohol and drug use), mental health status (i.e., depression), and time on ART. Type-3 P-values were used, with values less than or equal to 0.05 indicating statistical significance. In final adjusted models, we retained any variable that was found to be statistically significant (p<0.05) in the base model. We then conducted unadjusted and adjusted models for each barrier sub-scale separately.
RESULTS
Sample characteristics
The study sample included 151 patients with 503 study visits. Although 156 patients were randomized in the trial at the third study visit, 5 patients were excluded from this analysis because they did not have adherence data available. Twenty-three percent of the sample was female with a mean age of 42 years (standard deviation (SD) = 7.6 years). Nearly half of the sample was white, with 26% African-American, 20% Hispanic and the remaining another race. Fifty-one percent had a high-school education, with 43% having college level education or beyond, and 6% a grade school education. Fifty-six percent reported sex with a man as an HIV transmission risk factor, while 13% reported sex with a woman, 15% reported injecting drugs, and 16% reported other risk factors. Six percent were homeless and nearly one-third of the patients were employed. Twenty-four percent of the sample had five or more depressive symptoms out of 9 items. The average duration of time from randomization to the final study visit was 228 days (SD= 104 days). The average time on ART was 18.8 months (SD = 20.7 months) at randomization. The average adherence summarized across all study visits was 73% (SD=30).
Frequency of self-reported barriers
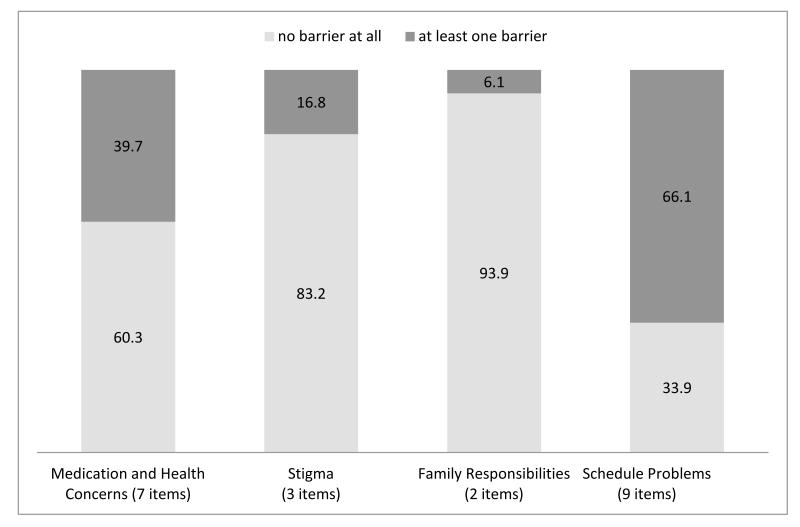
Table 1 presents the frequency of each response (i.e., never, rarely, sometimes, often) for each item within each barrier sub-scale type. When considering each item separately, at the majority of visits, most patients reported not having experienced barriers in the prior 30 days. The items in the problems with schedule and routine sub-scale were the most frequently reported, followed by medication and health concerns, stigma, and family responsibilities. Figure 1 displays the frequency of reporting any barrier within sub-scales summarized over all four study visits. For the medication and health concerns sub-scale, at least one of the barriers in this sub-scale were reported in nearly 40% of study visits. The stigma and family responsibilities barriers were least frequently reported, at 17% and 6% of visits, respectively. In 66% of study visits, at least one schedule and routine barrier was reported.
Figure 1.
Proportion of study visits with at least one barrier item reported on each of four sub-scales
The average total scores for each sub-scale, transformed to a 0 to 10 scale, are also presented in Table 1. Overall the mean medication and health concerns score was 0.9 (SD = 1.7). The means of the stigma and family responsibilities scores were lower, 0.5 (SD = 1.5) and 0.2 (SD = 1.0), respectively. The mean problems with schedule and routine score was 1.4 (SD = 1.6). The average scores by study visit were similar to the overall mean scores (data not shown).
Relationship between barrier types
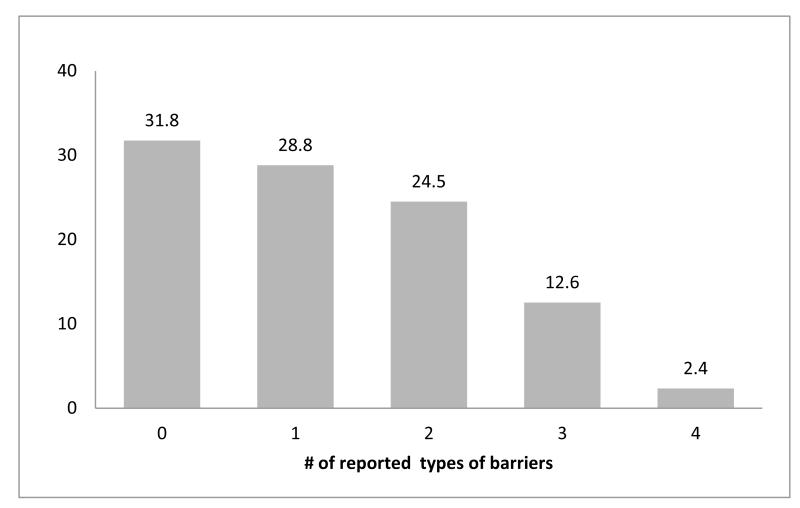
Figure 2 shows the frequency of concurrent reporting of each barrier type. Individuals who responded with any response other than “never” to any item within each sub-scale were considered to have experienced that type of barrier in the prior 30 days. In approximately one-third of the study visits, none of the barriers in any sub-scale were reported. During another third of the visits, at least one type of barrier was reported. During nearly 25% of visits, patients reported at least two types of barriers, while three types of barriers were reported in 13% of study visits, and four types in 2.4% of visits.
Figure 2.
Proportion of study visits with reported number of types of barriers
Table 2 presents the correlation coefficients between each of the four sub-scales. Each sub-scale was moderately correlated with the other sub-scales. The correlation between the medication and health concerns and stigma, family responsibilities, and schedule and routine were 0.49, 0.32 and 0.55, respectively. The correlation between stigma and family responsibilities and schedule and routine were 0.28 and 0.47, respectively. The correlation between family responsibilities and schedule and routine was 0.36. All p-values for the correlation coefficients presented were p<0.0001.
Table 2.
Pearson correlation coefficients of four adherence barriers sub-scales
| Sub-scale | Medication and health concerns |
Stigma | Family responsibilities |
Problems with schedule and routine |
|---|---|---|---|---|
| Medication and health concerns | 1 | 0.49 | 0.32 | 0.55 |
| Stigma | 1 | 0.28 | 0.47 | |
| Family responsibilities | 1 | 0.36 |
All p-values for correlation coefficients were p<0.0001
Change in barriers over time
The results of the analysis comparing changes in barriers from each sub-scale from one visit to the next using logistic regression with GEE demonstrated no statistically significant differences (p< 0.05) in scores over the four study visits (data not shown).
Impact of barriers on ART adherence
In the base adjusted model (data not shown), only depression was statistically significant (p<0.05), therefore all subsequent models included only the barrier sub-scale score, depression, the indicator variable for study visits, and intervention group assignment. Table 3 presents the results from the unadjusted and adjusted repeated measures models examining the impact of each barrier type on adherence. Coefficients represent the change in adherence, measured as percent covered time, per one unit increase in the total sub-scale score (scaled to 0-10). For each of the sub-scales, an increase of one unit in the summary sub-scale score was associated with statistically significant reductions in medication adherence, however this difference was not statistically significant (p=0.26) for the family responsibilities sub-scale. Each point increase on the medication and health concerns sub-scale was associated with an almost four percent decline (y = −3.93, 95% CI: −6.10, −1.76) in adherence in adjusted models. Increasing scores on the stigma (y = −2.35, 95% CI: −4.12, −0.59) and problems with schedule and routine (y = −2.45, 95% CI: −4.49, −0.41) sub-scales were both associated with more than a two percent decline in adherence.
Table 3.
Estimated coefficients from unadjusted and adjusteda models examining the change in adherence to ART associated with four adherence barrier sub-scales among 151 patients across 503 study visitsb.
| Barrier sub-scales | Medication and health concerns |
Stigma | Family responsibilities |
Problems with schedule and routine |
|---|---|---|---|---|
| Unadjusted coefficient (95% CI) | −4.40 (−6.45. −2.36) | −2.74 (−4.43, −1.06) | −0.26 (−2.36, 1.84) | −2.73 (−4.76, −0.69) |
| Adjusteda coefficient (95% CI) | −3.93 (−6.10, −1.76) | −2.35 (−4.12, −0.59) | −0.07 (−1.54, 5.78) | −2.45 (−4.49, −0.41) |
Unadjusted models included barrier sub-scale, time (study visit) and intervention assignment; Adjusted models included barrier sub-scale, time (study visit) and depression (score of 0-9 on PC-SAD).
Model 4 sample size is smaller (N=421) since there were N/A responses for questions related to family members.
DISCUSSION
There were several important findings in this study. First, the reporting of individual items was infrequent and patients had low barrier scores overall. This suggests that most patients currently taking ART have limited self-perceived and self-reported barriers to adhering to ART medication regimens. However, it is important to understand even limited barriers to ART adherence, as patients who disrupt treatment for even short timeframes due to occasional barriers face the possibility of reducing viral suppression over time as well as introducing the potential for viral resistance (17,18). By quantifying and categorizing the frequency of different types of barriers, this study builds on the existing qualitative literature which has described broad categories of barriers including patient characteristics and health beliefs, issues related to the medication regimen, and the social environment and fear of stigma (6-11,11-14).
Second, although patients had low barrier scores overall, we also found that patients reported all types of barriers and commonly reported more than one type of barrier. During approximately 70% of study visits patients reported at least one barrier, while they reported two or more types of barriers in 40% of visits. These results suggest that future research on patient-identified barriers to adherence should examine barriers within several different categories. The observed correlations between the sub-scales suggested that they measured related but distinct challenges to adherence among patients. Clinicians should consider more exhaustive assessments of barriers to ART adherence. Patient-identified challenges in one area do not preclude problems in other domains.
Third, self-reported barriers did not change over time in this study. While we acknowledge that challenges patients face in adhering to ART are fluid and dynamic in nature (12), this study did not demonstrate marked changes over time. However, it is important to note that while this study is one of the first to examine patient barriers longitudinally, the duration of the study interval may not have been long enough to capture the changes in barriers we would expect to see among patients currently taking ART. In addition while this study examined barriers among patients taking ART for an average of 18 months, it is possible that the experience of barriers and different types of barriers changes with the duration of time on treatment. Additional research examining different types of barriers over longer timeframes is needed to fully characterize how patient barriers evolve over the course of treatment.
Finally, we found that different types of self-reported barriers to adherence were associated with statistically significant reductions in objectively measured adherence among patients currently taking ART. With each increasing point on each barrier sub-scale except for family responsibilities, there were corresponding decreases of 2-4 adherence percentage points. Medication and health concerns were associated with an almost two-fold greater decrease in adherence compared to stigma.
Previous research has examined “intentional” and “unintentional” barriers to patient adherence. Intentional barriers have been characterized as deliberate decisions on the part of patients not to adhere to medications, whether altering the schedule of doses or to stop taking medications altogether, while unintentional barriers are considered “mistakes” that are not purposely made (19). Although this classification system may assist researchers in parsing out patients who accept their HIV diagnosis and are committed to their regimens from those who are not engaged with treatment (20), in our opinion this dichotomy may oversimplify patients’ psychosocial processes related to medication adherence. Patients who may be defined as having “unintentional” barriers to adherence may also have other important issues that would be overlooked should concerns about forgetfulness and intentionality be placed at the forefront. At the same time, patients with “intentional” barriers may be interacting with social forces that constrain their behaviors. Still, we characterized the barriers that would be considered “unintentional” largely as interruptions to schedule or routine.
In fact the barriers in the schedule and routine sub-scale were the most commonly reported by patients, a finding that confirms other research on patient-identified barriers to adherence (2,8,21,22). However, despite their relative common occurrence in this sample, barriers related to schedule and routine did not lead to the largest reductions in adherence. Barriers related to concerns about medications and health had a larger overall impact on adherence in this study. Again, interventions designed to improve adherence among patients currently taking ART should focus on assisting with issues specifically identified by patients as barriers to achieving optimal adherence.
The main implication of this study is that patient-identified barriers should be addressed with different types of interventions and counseling (23). Recently reminders and cues via mobile text messages were shown to promote adherence (24). It is possible that the largest improvements were among those with interruptions in schedules or routines and it is unknown how this type of intervention may be perceived by participants with concerns about their medications or fears related to stigma. Additional research is needed to examine how different types of interventions may be targeted to the specific needs and barriers of patients during the course of their engagement with ART.
Because barriers to ART adherence are multi-dimensional, providers who assess one or two given items will overlook many other types of patient concerns, which may be reported less frequently, but have a greater impact on adherence. Because comprehensively assessing barriers during medical visits is time consuming, pre-visit assessment tools for barriers to adherence may be useful. Patient self-reported assessments have been used successfully by HIV care providers to identify patients with non-adherence to HIV medications, as well as other issues such as depression, risk behaviors and substance use (25,25,26). However we know of no studies that have examined pre-visit assessments of barriers to adherence. A pre-visit assessment is a low-cost, easily implemented, and quick strategy that can be used by providers to help frame conversations with patients and focus counseling and intervention on issues that are most relevant to the patient. Ideally this type of tool would also allow for interventions to ameliorate barriers to adherence prior to viral failure or other clinical events. Additional research is needed to evaluate the utility and impact of pre-visit screening tools for barriers to adherence among patients taking ART.
The adherence barrier items successfully measured four types of patient barriers to ART. The factor analysis results presented here should be considered exploratory. Additional work is needed to confirm these assessments, as well as to further establish the reliability and validity of the measures through additional testing with different samples and the examination of the barrier types with respect to other factors known to be related to patient medication adherence. Still, administering these items to patients may be a useful and efficient strategy for clinicians to guide their counseling and referrals for support services.
There is a well-documented relationship between depression and adherence to ART (27,28). This study confirmed that a higher number of depressive symptoms were associated with statistically significant decreases in objectively measured adherence. The results presented here add to the literature by demonstrating that four types of self-reported barriers did not confound the relationship between depression and adherence. Specifically, depression remained associated with adherence after accounting for four different types of self-reported barriers to adherence. This suggests that depressive symptoms may impact adherence to ART via different mechanisms than concerns regarding medication and health, stigma, family responsibilities, and problems with routines and scheduling.
This study had a number of limitations. There may have been some measurement bias in the assessment of barriers due to social desirability. Patients may have been reluctant to share their difficulties with the study interviewers, leading to underestimates of the reported barriers. We have no reason, however, to think that this bias would be differential with respect to the different types of barriers under study. The family responsibilities sub-scale was limited and considered exploratory in this study due to the small number of items and substantial number of respondents who considered the questions “not applicable” to their lives. Measurement error may also have been an issue for the assessment of adherence. Electronic monitoring of medication taking is not a perfect measurement tool (29). For example, there is no guarantee that a patient opening the cap actually took the medication as directed. If patients systematically open their medication bottles without taking the drug, adherence may be overestimated. This paper also presents data collected between 2002-2005. Since then there has been significant development of ART regimens and medication-specific barriers may be different now from what is presented here. Future research on newer ART regimens is needed to determine the lasting impact of medication-specific barriers. Finally there were also concerns regarding the external validity of our results. Our findings may not be generalizable beyond the greater New England area, however sampling from patients currently in care across a wide variety of clinical practices potentially increased the external validity of the current study. In addition the sample included patients with varying risk factors for HIV acquisition including both sexual and drug-related behaviors, potentially also increasing the generalizability of the results.
This study demonstrated that patient-identified barriers to ART adherence are varied and independently impact adherence behaviors. Future quantitative research is needed to confirm the types of barriers presented here among different patient samples outside the context of a randomized trial. Additional research is also needed to design and evaluate interventions to address the different types of barriers presented here, including the use of patient self-report assessments of adherence barriers in clinical practice.
Acknowledgments
This work was supported by grants from the National Institute on Drug Abuse (R01DA015679, R21MH073420), the National Institute for Mental Health (R21MH073420; K24MH092242), and the Lifespan/Tufts/Brown Centers for AIDS Research (P30AI042853).
REFERENCES
- (1).Bangsberg DR, Perry S, Charlebois ED, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15(9):1181–1183. doi: 10.1097/00002030-200106150-00015. [DOI] [PubMed] [Google Scholar]
- (2).Mills EJ, Nachega JB, Bangsberg DR, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PLoS Med. 2006;3(11):e438. doi: 10.1371/journal.pmed.0030438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Ammassari A, Trotta MP, Murri R, et al. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–7. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- (4).Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17(4):169–177. doi: 10.1089/108729103321619773. [DOI] [PubMed] [Google Scholar]
- (5).Fogarty L, Roter D, Larson S, Burke J, Gillespie J, Levy R. Patient adherence to HIV medication regimens: a review of published and abstract reports. Patient Educ Couns. 2002;46(2):93–108. doi: 10.1016/s0738-3991(01)00219-1. [DOI] [PubMed] [Google Scholar]
- (6).Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a southern minority population with HIV disease. J Assoc Nurses AIDS Care. 2008;19(2):98–104. doi: 10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Konkle-Parker D. Medication adherence: what are the barriers and facilitators? HIV Clin. 2007;19(4):8–9. [PubMed] [Google Scholar]
- (8).Roberts KJ. Barriers to and facilitators of HIV-positive patients’ adherence to antiretroviral treatment regimens. AIDS Patient Care STDS. 2000;14(3):155–168. doi: 10.1089/108729100317948. [DOI] [PubMed] [Google Scholar]
- (9).Roberts KJ, Mann T. Barriers to antiretroviral medication adherence in HIV-infected women. AIDS Care. 2000;12(4):377–386. doi: 10.1080/09540120050123774. [DOI] [PubMed] [Google Scholar]
- (10).Proctor VE, Tesfa A, Tompkins DC. Barriers to adherence to highly active antiretroviral therapy as expressed by people living with HIV/AIDS. AIDS Patient Care STDS. 1999;13(9):535–544. doi: 10.1089/apc.1999.13.535. [DOI] [PubMed] [Google Scholar]
- (11).Murphy DA, Roberts KJ, Martin DJ, Marelich W, Hoffman D. Barriers to antiretroviral adherence among HIV-infected adults. AIDS Patient Care STDS. 2000;14(1):47–58. doi: 10.1089/108729100318127. [DOI] [PubMed] [Google Scholar]
- (12).Remien RH, Hirky AE, Johnson MO, Weinhardt LS, Whittier D, Le GM. Adherence to medication treatment: a qualitative study of facilitators and barriers among a diverse sample of HIV+ men and women in four US cities. AIDS Behav. 2003;7(1):61–72. doi: 10.1023/a:1022513507669. [DOI] [PubMed] [Google Scholar]
- (13).Vervoort SC, Borleffs JC, Hoepelman AI, Grypdonck MH. Adherence in antiretroviral therapy: a review of qualitative studies. AIDS. 2007;21(3):271–281. doi: 10.1097/QAD.0b013e328011cb20. [DOI] [PubMed] [Google Scholar]
- (14).Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- (15).Wilson IB, Laws MB, Safren SA, et al. Provider-focused intervention increases adherence-related dialogue but does not improve antiretroviral therapy adherence in persons with HIV. J Acquir Immune Defic Syndr. 2010;53(3):338–347. doi: 10.1097/QAI.0b013e3181c7a245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Rogers WH, Wilson IB, Bungay KM, Cynn DJ, Adler DA. Assessing the performance of a new depression screener for primary care (PC-SAD) J Clin Epidemiol. 2002;55(2):164–175. doi: 10.1016/s0895-4356(01)00430-9. [DOI] [PubMed] [Google Scholar]
- (17).Genberg BL, Wilson IB, Bangsberg DR, et al. Patterns of antiretroviral therapy adherence and impact on HIV RNA among patients in North America. AIDS. 2012;26(11):1415–1423. doi: 10.1097/QAD.0b013e328354bed6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4(2):65–72. doi: 10.1007/s11904-007-0010-0. [DOI] [PubMed] [Google Scholar]
- (19).Norton WE, Amico KR, Fisher WA, et al. Information-motivation-behavioral skills barriers associated with intentional versus unintentional ARV non-adherence behavior among HIV+ patients in clinical care. AIDS Care. 2010;22(8):979–987. doi: 10.1080/09540121003758630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (20).Vervoort SC, Grypdonck MH, de Grauwe A, Hoepelman AI, Borleffs JC. Adherence to HAART: processes explaining adherence behavior in acceptors and non-acceptors. AIDS Care. 2009;21(4):431–438. doi: 10.1080/09540120802290381. [DOI] [PubMed] [Google Scholar]
- (21).MacDonell K, Naar-King S, Huszti H, Belzer M. Barriers to medication adherence in behaviorally and perinatally infected youth living with HIV. AIDS Behav. 2013;17(1):86–93. doi: 10.1007/s10461-012-0364-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Murphy DA, Sarr M, Durako SJ, et al. Barriers to HAART adherence among human immunodeficiency virus-infected adolescents. Arch Pediatr Adolesc Med. 2003;157(3):249–255. doi: 10.1001/archpedi.157.3.249. [DOI] [PubMed] [Google Scholar]
- (23).Simoni JM, Amico KR, Pearson CR, Malow R. Strategies for promoting adherence to antiretroviral therapy: a review of the literature. Curr Infect Dis Rep. 2008;10(6):515–521. doi: 10.1007/s11908-008-0083-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Mbuagbaw L, van der Kop ML, Lester RT, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ Open. 2013;3(12):e003950-2013-003950. doi: 10.1136/bmjopen-2013-003950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–318. doi: 10.1007/s10461-012-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (26).Schackman BR, Dastur Z, Rubin DS, et al. Feasibility of using audio computer-assisted self-interview (ACASI) screening in routine HIV care. AIDS Care. 2009;21(8):992–999. doi: 10.1080/09540120802657506. [DOI] [PubMed] [Google Scholar]
- (27).Gonzalez JS, Batchelder AW, Psaros C, Safren SA. Depression and HIV/AIDS treatment nonadherence: a review and meta-analysis. J Acquir Immune Defic Syndr. 2011;58(2):181–187. doi: 10.1097/QAI.0b013e31822d490a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (28).Starace F, Ammassari A, Trotta MP, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S136–9. doi: 10.1097/00126334-200212153-00010. [DOI] [PubMed] [Google Scholar]
- (29).Wendel CS, Mohler MJ, Kroesen K, Ampel NM, Gifford AL, Coons SJ. Barriers to use of electronic adherence monitoring in an HIV clinic. Ann Pharmacother. 2001;35(9):1010–1015. doi: 10.1345/aph.10349. [DOI] [PubMed] [Google Scholar]