Abstract
Bacillus anthracis is the etiologic agent of anthrax, an acute fatal disease among mammals. It was thought to differ from Bacillus cereus, an opportunistic pathogen and cause of food poisoning, by the presence of plasmids pXO1 and pXO2, which encode the lethal toxin complex and the poly-γ-d-glutamic acid capsule, respectively. This work describes a non-B. anthracis isolate that possesses the anthrax toxin genes and is capable of causing a severe inhalation anthrax-like illness. Although initial phenotypic and 16S rRNA analysis identified this isolate as B. cereus, the rapid generation and analysis of a high-coverage draft genome sequence revealed the presence of a circular plasmid, named pBCXO1, with 99.6% similarity with the B. anthracis toxin-encoding plasmid, pXO1. Although homologues of the pXO2 encoded capsule genes were not found, a polysaccharide capsule cluster is encoded on a second, previously unidentified plasmid, pBC218. A/J mice challenged with B. cereus G9241 confirmed the virulence of this strain. These findings represent an example of how genomics could rapidly assist public health experts responding not only to clearly identified select agents but also to novel agents with similar pathogenic potentials. In this study, we combined a public health approach with genome analysis to provide insight into the correlation of phenotypic characteristics and their genetic basis.
Bacillus cereus and Bacillus anthracis are members of a closely related phylogenetic cluster referred to as the B. cereus group. Although classification of B. anthracis and B. cereus as separate species based on molecular analysis has been questioned, they differ in phenotype and in the diseases they cause (1-4). B. cereus is ubiquitous in nature and is an opportunistic pathogen. In individuals with underlying conditions, immuno-compromised individuals, or patients recovering from surgery, B. cereus has been known to cause a variety of infections, including: endophthalmitis, bacteremia, septicemia, endocarditis, salpingitis, cutaneous infections, pneumonia, and meningitis (5). In contrast, B. anthracis is the etiologic agent of anthrax, an acute fatal disease among mammals, which in recent years has become known for its use as a biological weapon (6). The genes encoding the major anthrax toxins and the poly-γ-d-glutamic acid capsule are located on two virulence plasmids, pXO1 (182 kb) and pXO2 (96 kb), respectively, and are required for full virulence (7-9).
Materials and Methods
Genome Sequencing. Genomic DNA extraction of B. cereus G9241 was performed at the Centers for Disease Control and Prevention. Random shotgun sequencing was undertaken by using a strategy similar to previous projects (10). Random insert libraries of 2.5-4.5 kb and 4.5-9.0 kb were constructed, and 93,562 high-quality sequences were obtained (817-bp average read length). A 13.5× coverage draft genome sequence was obtained and assembled by using the Celera assembler (11). The assembly consisted of 131 contigs that were ordered and concatenated with our prior knowledge of the B. anthracis and B. cereus genome sequences (10, 12). The resulting 5,286,464-bp sequence was annotated through the Institute for Genomic Research Bioinformatics pipeline as reported (13). The genomic features of this molecule are described in Table 2, which is published as supporting information on the PNAS web site.
Capsule Visualization. B. cereus was streaked onto trypticase soy agar containing 5% sheep blood (Becton Dickinson Microbiology Systems) and incubated in ambient atmosphere overnight at 37°C. B. anthracis was streaked onto trypticase soy agar containing 0.8% sodium bicarbonate and incubated in 5% CO2 at 37°C. Cells from a single colony were dispersed into 5 μl of water on a microscope slide and covered with a coverslip. A single drop of india ink (Remel, Lenexa, KS) was applied to the edge of the coverslip and allowed to diffuse into the sample. The cells were visualized with a ×100 oil-immersion objective (14).
Biochemical and Microbiological Phenotypic Characterization. Motility was observed by wet mount of cells grown in heart infusion broth and by using Motility Test medium with triphenyltetrazolium chloride (Remel). Susceptibility to γ-phage (15) was performed by adding 5 μl of γ-phage to the first and second quadrants of a 5% sheep blood plate streaked for isolation and incubated at 37°C overnight. The B. anthracis specific two-component direct fluorescent Ab (DFA) assay was performed as described by De et al. (16). Sequencing of the 16S rRNA gene was performed as described by Sacchi et al. (17).
Comparative Genomic Hybridization (CGH). CGH was performed as described for other B. cereus isolates by Read et al. (10).
Multiple Locus Sequence Typing. Phylogenetic tree of members of the B. cereus sensu lato group was generated based on partial nucleotide sequences of seven housekeeping genes, totaling 2,977 nucleotides and was built by using the neighbor-joining method (18) applied to a matrix of pairwise differences among sequences. Detailed multiple locus sequence typing methods are available online at http://pubmlst.org/bcereus.
blast Score Ratio Analysis. The blast score ratio analysis is a modification of the technique described by Read et al. (19). For each of the predicted proteins of B. cereus G9241, we obtained a blastp raw score for the alignment against itself (REF_SCORE) and the most similar protein (QUE_SCORE) in each of the genomes of B. cereus ATCC10987 (12), B. cereus ATCC14579 (20), and B. anthracis Ames (10). These scores were normalized by dividing the QUE_SCORE obtained for each query genome protein by the REF_SCORE. Proteins with a normalized ratio of <0.4 were considered to be nonhomologous. The normalized blast score ratio of 0.4 is generally similar to two proteins being ≈30% identical over their entire length.
blast score ratios were plotted as x,y coordinates as shown in Fig. 5, which is published as supporting information on the PNAS web site. Each protein in the reference genome (B. cereus G9241) was grouped according to its scores in each of the query genomes and colored as follows: yellow, unique to the reference; red, common to all three; cyan, common between query 1 and the reference but absent in query 2; blue, common between query 2 and the reference but absent in query 1.
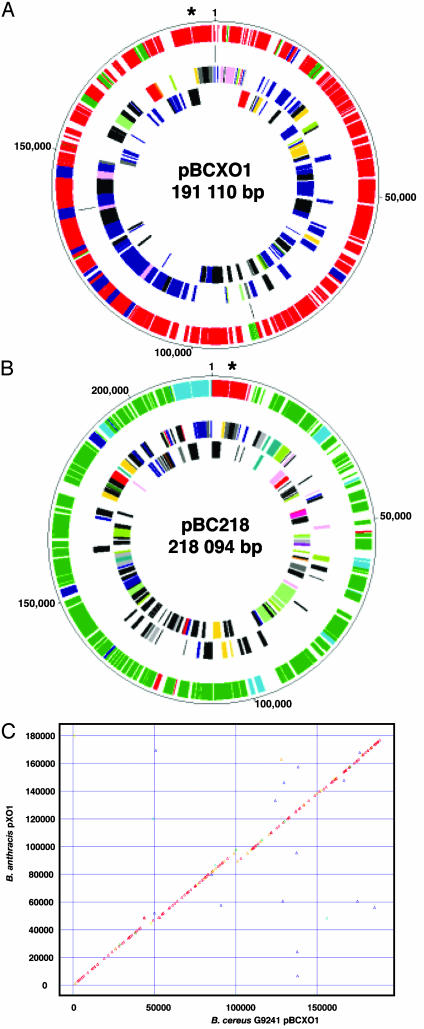
Fig. 1C shows a synteny plot in which each triangle indicates a single protein plotted on the 5′ end of the coding region in the reference genome and the best match in the query organism.
Fig. 1.
(A-B) Circular representations of the plasmids of B. cereus G9241. The plasmids were compared by using blastp to the B. anthracis pXO1 and pXO2 plasmids and B. cereus ATCC10987 pBC10987 and Bacillus thuringiensis israeliensis pBtoxis. The inner two rings represent the plasmid coding regions in forward and reverse orientation; color scheme is as described (13). The outer-ring color scheme is as follows: red, B. anthracis plasmids; blue, B. cereus ATCC10987 plasmid pBC10987; cyan, proteins equally similar in both species; and green, proteins unique to that plasmid. The third ring represents the remaining physical gaps of the plasmids. (C) Synteny plots of the plasmids of B. cereus G9241 pBCXO1 versus B. anthracis Ames pXO1. Each triangle represents a single protein of G9241. They are color coded as follows: red, normalized score ≥0.95; orange, normalized scores ≥0.80 and <0.95; yellow, normalized scores ≥0.60 and <0.80; green, normalized scores ≥0.40 and <0.60; cyan, normalized scores ≥0.20 and <0.40; and blue, normalized scores≥0.0 and <0.20.
Protective Antigen (PA) ELISA. Rows of an ELISA plate were coated overnight in PBS with B. anthracis PA-specific mAb (Biological Defense Research Directorate) or normal mouse IgG (Sigma) (negative capture). Plates were blocked for 1 h with 5% skim milk at 37°C. After washing three times with wash buffer (1× PBS with 0.1% Tween 20), the antigen (i.e., supernatant of cells grown in horse serum) was added to well 1 and titered across the plate from wells 1-9 with 1:2 serial dilution in 5% skim milk with 0.1% Tween (dilution buffer). Plates were incubated for 1 h at 37°C and then washed three times with wash buffer. The biotinylated detector Ab was then applied in the dilution buffer. The detector for this assay is the same mAb as the capture, only biotinylated. The plate was again incubated for 1 h at 37°C, then washed three times. A streptavidin/horseradish peroxidase conjugate in dilution buffer was applied, and, after incubation for 1 h, the plate was washed three times. Substrate [2,2′-azinobis(3-ethylbenzthiazoline-6-sulfonic acid)] was added, and the plate was incubated for 30 min at 37°C, at which point it was read in an Ultra Evolution ELISA plate reader (Tecan, Durham, NC). The positive cutoff was calculated to be three times the standard deviation of the mean of the negative capture plus 0.150. Purified B. anthracis PA protein (2-500 ng/ml; Biological Defense Research Directorate) was used as a positive control and to generate the standard curve for quantitation.
Mice i.p. Challenge. Spores of B. anthracis Sterne strain, B. cereus ATCC10987, and B. cereus G9421 were prepared by the outgrowth on sporulation medium (per liter, 23 g of nutrient agar/0.025 g MNSO4·H2O/0.25 g KH2PO4). Spore titer (and percentage of spores to vegetative cells) was determined by direct counting under a phase-contrast microscope. Spore suspensions were washed and diluted appropriately in PBS. Employing the method outlined by Beedham et al. (21), six groups of 10, 6- to 8-week-old, female, A/J mice weighing 20-24 g received i.p. injections either a low (range 1.1 × 104 to 2.7 × 104 colony-forming units) or high (range 1.1 × 106 to 5.3 × 106 colony-forming units) dose of spores of either the Sterne strain of B. anthracis, B. cereus G9421, or B. cereus ATCC10987. The A/J strain was selected because it was found to be sensitive to the vaccine strain B. anthracis Sterne (21). Spores for injection were suspended in 100 μl of PBS. The control group was injected with sterile PBS. Animals were monitored four times daily for 14 days for signs of morbidity/mortality. Mice found unresponsive, paralyzed/unresponsive, or moribund were killed with CO2, and blood and tissue (heart, lung, liver, and spleen) samples were obtained. For mice found dead, only tissue samples were obtained. At day 14, all remaining mice were killed with CO2 and processed as described for sick mice above. Either blood films or touch preparations from heart tissue were performed for staining. Heart tissue and the blood removed from the animals postmortem was plated on 5% (vol/vol) sheep blood agar and incubated at 37°C for 24 h to confirm bacterial infection as cause of death. Student's t test was applied to determine the significance of the average survival between two groups. This study was carried out in strict accordance with the Animals (Scientific Procedures) Act of 1986.
Results
Isolation of B. cereus G9241. During a retrospective analysis of Bacillus isolates that caused unusually severe disease, we identified an isolate (G9241) that contained a homologue of the B. anthracis pXO1-encoded PA gene, pagA, but not the pXO2-encoded poly-γ-d-glutamic acid capsule biosynthetic genes. G9241 was isolated from the sputum and blood of a patient with life-threatening pneumonia, whose history, clinical features, and laboratory findings resemble those reported for 10 bioterrorism-associated inhalation anthrax patients in 2001 (23). The patient, like the 10 inhalation anthrax patients from 2001 (23), was not immunocompromised, did not take drugs, was a nonsmoker, and had no predominant underlying disease. In addition to fever, chills, and hemoptysis, the patient sought care only 2 days from onset of symptoms (3.5 days for 2001 patients), reported nausea and vomiting (80% of 2001 patients), and had an abnormal chest x-ray (multiple abnormalities in all 2001 patients). His initial white blood cell count (WBC) was 12,000 per mm3 (median WBC 9,900 per mm3 for 2001 patients), and peak WBC was 22,400 per mm3 (median peak WBC 26,400 per mm3 for 2001 patients). The patient received intensive care, mechanical ventilation for 44 days, treatment with numerous antimicrobial drugs (timentin, erythromycin, rifampin, isoniazid, and bactrim) and corticosteroids, and a partial lobectomy before he was discharged and subsequently recovered (Table 3, which is published as supporting information on the PNAS web site).
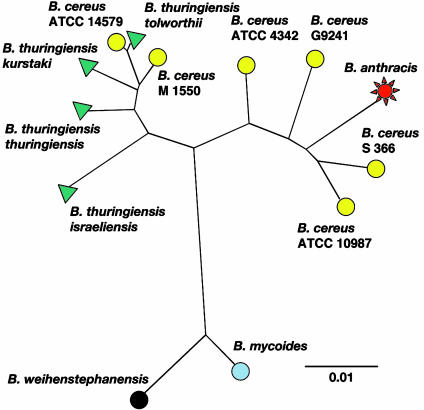
Typing of B. cereus G9241. This anthrax-like clinical presentation was attributed to an isolate (G9241) identified as B. cereus by using traditional phenotypic characteristics and biochemical reactions at the Centers for Disease Control and Prevention Special Bacteriology Reference Laboratory (Table 1). By using the 16S rRNA typing scheme of Sacchi et al. (17), it was determined that G9241 was type 7 (GenBank accession no. AY425946), one of six 16S types exclusively associated with B. cereus isolates. Additionally, strain G9241 was included in a multilocus sequence typing scheme that used seven housekeeping genes and has been developed for the B. cereus group (http://pubmlst.org/bcereus). This analysis showed that strain G9241 is closely related to but distinct from B. anthracis (Fig. 2).
Table 1. Biochemical and microbiological characteristics of B. anthracis, B. cereus spp., and B. cereus G9241.
| B. anthracis | B. cereus spp. | B. cereus G9241 | |
|---|---|---|---|
| Hemolytic | — | + | + |
| Motile | — | + | + |
| γ-Phage* | S | R | R |
| Penicillin† | S | R | R |
| Cell-wall DFA | + | +/—‡ | + |
| Capsule DFA | + | — | — |
| 16S rRNA type | 6§ | V§ | 7§ |
| Capsule | +¶ | —¶ | +¶ |
+, positive. —, negative. S, sensitive/susceptible. R, resistant. V, variable.
γ-Phage sensitivity is measured by the capacity of the γ-phage to lyse the culture
Penicillin susceptibility and resistance is measured by standard culture techniques
B. cereus species have a variable reaction to the B. anthracis cell-wall DFA test
Typing for 16S rRNA is based on the system of Sacchi et al. (17). To note, B. cereus spp. have a variety of types; however, type 6 has never been identified in any group other than B. anthracis
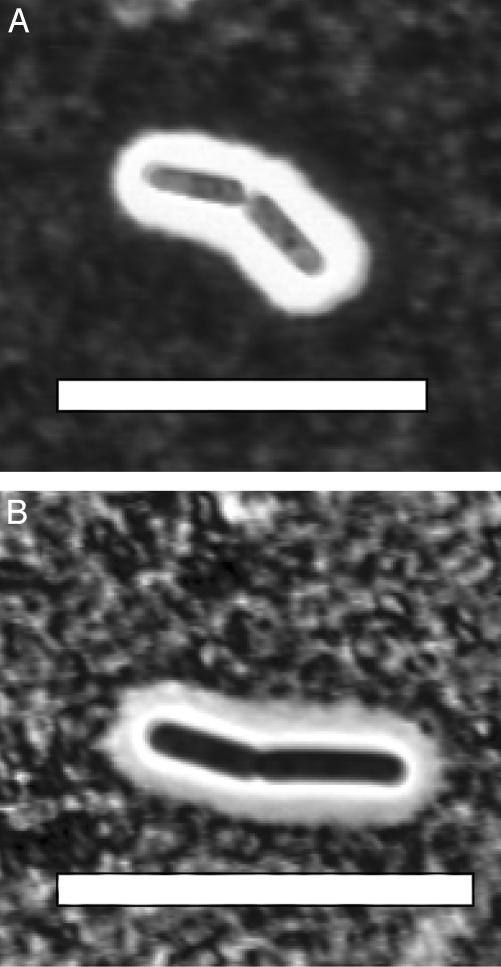
B. anthracis produces a poly-γ-d-glutamic acid capsule, and a putative capsule operon has been identified in B. cereus ATCC10987 (12) and B. cereus ATCC14579 (20). However, under the experimental conditions employed in this study, no capsule has been observed in association with either strain. B. cereus G9241 expresses a capsule (Fig. 3) that is not a poly-γ-d-glutamic acid capsule
Fig. 2.
Unrooted, neighbor-joining tree derived from multiple-locus sequence typing of B. cereus G9241 and other Bacillus spp. (http://pubmlst.org/bcereus).
This conclusion was also supported by the CGH, which also revealed a high degree of hybridization to pXO1 genes, including all three anthrax toxin genes (Fig. 6, which is published as supporting information on the PNAS web site).
Taken collectively, these data provided multiple lines of evidence to suggest that the G9241 isolate, responsible for an anthrax-like clinical presentation, is indeed a B. cereus isolate containing pXO1 genes, including the genes encoding the anthrax toxins.
Genome Sequence Analysis. To obtain a more in-depth understanding of this unusual B. cereus clinical isolate, whole-genome shotgun sequencing was performed. One feature of the B. cereus G9241 genome is its mosaic structure. This structure could be explained by the presence of a great number of known and novel putative mobile genetic elements (insertion sequence elements, phages, transposases, integrases, and recombinases). Fig. 5A shows the degree of homology of each of the B. cereus G9241 predicted proteins to either B. anthracis Ames, B. cereus ATCC10987, or B. cereus ATCC14579. The proteome of B. cereus G9241 shows a greater degree of similarity to the core proteome of the complete genome of B. cereus ATCC10987 than to B. cereus ATCC14579 and, to a lesser extent, B. anthracis Ames, also shown by blast score ratio analysis (Fig. 5B). Overall, 60% of the G9241 proteome is more similar to B. cereus strains than to B. anthracis, in full agreement with the initial classification of G9241 as a B. cereus strain.
Comparative analysis of the chromosome of B. cereus G9241 with those of B. cereus ATCC10987, B. cereus ATCC14579, and B. anthracis Ames revealed a set of specific characteristics that can be linked to phenotypic observations. PlcR is a positive regulator of many secreted and virulence-associated genes in B. cereus strains, including protease, phospholipases, hemolysins, and motility genes (24). In common with other B. cereus stains, G9241 does not have the nonsense frameshift found in the plcR gene of B. anthracis; hence, it could produce a fully functional PlcR regulator, which may explain many of its phenotypic characteristics (Fig. 7, which is published as supporting information on the PNAS web site).
B. cereus G9241 is motile (Table 1), a phenotype that could be explained by the presence of a complete flagella biosynthetic cluster. Although B. anthracis is not motile, it is common for B. cereus and other motile Bacillus species to be flagellated. Even though B. anthracis contains most of this system, four essential proteins are truncated by frameshifts (10), all of which are full-length in G9241. Two PlcR palindromic binding sites are located 124 bp in front of a flagella component subunit (flgB) and a conserved hypothetical protein that is part of the same cluster. Interestingly, this isolate contains five flagellin subunits (only two are found in B. cereus ATCC10987, four in B. cereus ATCC14579, and one in B. anthracis Ames), four of which are clustered and have low similarity to either B. anthracis or B. cereus flagellins. However, the fifth is most similar to a flagellin subunit that appears to be only found in B. cereus (Fig. 8, which is published as supporting information on the PNAS web site).
The genome of G9241 encodes for four putative hemolysins (hemolysin A, BL, II, and III). Hemolysin BL appears to be PlcR-regulated as in other B. cereus strains, which could explain the observed hemolytic activity of the G9241 isolate (Table 1). In addition, G9241 phospholipase C, which is responsible for lecithin degradation, has all its components under the control of PlcR as do other B. cereus strains.
An unexpected finding in the G9241 genome was the presence of a 191,110-bp circular plasmid with high similarity and synteny to B. anthracis pXO1 (Fig. 1). This plasmid was responsible for the high level of hybridization to pXO1 genes observed by CGH. We will refer to this plasmid as pBCXO1 to differentiate it from B. anthracis pXO1. pBCXO1 encodes for the entire anthrax toxin biosynthetic complex, PA (99.7% amino acid identity), lethal toxin (99% amino acid identity), and edema factor (96% amino acid identity) and its associated regulatory proteins AtxA (100% amino acid identity) and PagR (98.6% amino acid identity), confirming the CGH and PCR results. The presence of AtxA and a full PlcR regulon raises some interesting questions, because it was suggested previously that in B. anthracis these two regulators were incompatible (25) and may have led to the selection for the plcR nonsense mutation in B. anthracis. The B. cereus G9241 pBCXO1-encoded pagA gene represents a distinctive PA sequence type by using the typing scheme of Price et al. (26). Two point mutations are found at positions 1,999 and 2,672, resulting in serine to proline and isoleucine to serine amino acid changes, respectively (Table 4, which is published as supporting information on the PNAS web site). With these two mutations, the identified sequence is most similar to PA genotype V, which has been primarily associated with the western North America diversity group of B. anthracis (26, 27). Expression of the PA by B. cereus G9241 was confirmed in the supernatant of a stationary phase culture (109 cells per ml) by ELISA (see Materials and Methods). The amount of PA expressed (4.3 μg/ml) was found to be equivalent to that seen in B. anthracis Ames (3.4 μg/ml) and B. anthracis Sterne (2.7 μg/ml). Importantly, the negative controls B. anthracis Pasteur and B. cereus ATCC10987 did not express any detectable amount of PA.
By using a two-component DFA assay (16), B. cereus G9241 was tested (Table 1) for cell envelope similarities to B. anthracis. G9241 produced a positive reaction with mAb specific to the B. anthracis cell-wall antigen but not with Ab against the B. anthracis capsule. Because it is not uncommon for some clinical isolates of B. cereus to react with the cell-wall-specific Ab, the positive reaction with this Ab was not unusual (16). Although the isolate did not react with the B. anthracis-specific capsule Ab, it did produce a capsule that was expressed during growth on sheep blood agar plates or in horse serum (Fig. 3) but did not require CO2 induction, as is the case for B. anthracis. However, a thicker capsule was observed during growth with elevated CO2 (M. Chute, personal communication). A novel polysaccharide capsule biosynthetic gene cluster has been found on a unique and previously unidentified 218,094-bp circular plasmid in the genome of G9241. pBC218 encodes 188 putative ORFs, among which we identified gene products with similarities to B. anthracis pXO1-encoded toxin regulator AtxA (78% amino acid identity), PA (60% amino acid identity), and the lethal factor (36% amino acid identity) but not the edema factor or the B. anthracis pXO2-encoded poly-γ-d-glutamic acid capsule biosynthetic genes. The pBC218-encoded PA peptide is identical to B. anthracis at all 10 dominant negative amino acid residues identified by Mourez et al. (28). Another 33 residues were identified that resulted in decreased activity when substituted by cysteine, of which 27 are identical in pBC218-encoded PA. The remaining six residues are conservative substitutions (28). This evidence suggests that the pBC218-encoded PA could be functional; however, this must be verified experimentally. Because no pXO2-like plasmid was identified in the genome, the encapsulation of G9241 observed in the laboratory (Table 1) may be encoded by the pBC218 capsule biosynthetic cluster. Analysis of this cluster indicates that it encodes for a polysaccharide capsule (Fig. 9, which is published as supporting information on the PNAS web site). In addition, our detailed genomic examination has not revealed any other capsule biosynthetic clusters on either the chromosome or plasmids.
Fig. 3.
B. cereus G9241 capsule. India ink stain of B. cereus G9241 grown in ambient atmosphere (A) and B. anthracis grown in 5% CO2 (B). (Scale bar, ≈10 μm.)
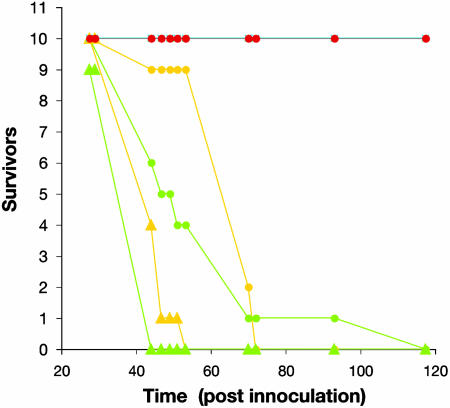
Lethality of B. cereus G9241 in Mice. These genotypic characteristics of the G9241 B. cereus strain supported by the severe clinical presentation are consistent with its properties as a B. anthracis-like pathogen. To assess the mammalian virulence of B. cereus G9241, A/J mice were challenged by i.p. injection (21) with mature spores of B. anthracis Sterne, B. cereus G9241, and B. cereus ATCC10987 (12). In these preliminary studies, G9241 produced 100% lethality, consistent with the positive control B. anthracis Sterne, although lethality was achieved faster when the high-spore dose was inoculated (t test, P = 0.081) (Fig. 4). B. cereus G9241 colonies were recovered from the heart tissue, and the blood was removed from the animals postmortem and plated on sheep blood agar incubated at 37°C for 24 h. Bacterial colonies were not recovered from any of the negative control mice injected with either PBS or with the nonpathogenic B. cereus ATCC10987.
Fig. 4.
Survival of A/J mice i.p. challenged with B. cereus G9241 (green), B. anthracis Sterne (yellow), and B. cereus ATCC10987 (red). High-spore dose (1 × 106) and low-spore dose (1 × 104) are represented by triangles and circles, respectively. The experiment was monitored for 14 days, after which the mice inoculated with B. cereus ATCC10987 were still alive.
Additional Genome Features. Several other interesting features of this strain included a cryptic phage of 29,886 bp (pBClin29, Table 2) that encodes phage-like proteins and a plasmid replicon similar to B. anthracis pXO2. In addition and particularly relevant to public health and patient treatment, G9241 contains genes that, if functional, should provide the isolate with resistance to β-lactam, chloramphenicol, and macrolide antimicrobial agents (Table 4). A PlcR palindromic binding site is located 48 bp in front of a metallo-β-lactamase (ORF04823), which could explain the penicillin-resistant phenotype observed in the laboratory. This binding site is also present in the other B. cereus genome and in B. anthracis Ames. However, the truncated PlcR is proposed to explain the penicillin-susceptible phenotype observed in the latter.
Discussion
This article describes the detection of naturally occurring anthrax toxin genes in a species other than B. anthracis and associated with an inhalation anthrax-like illness. Although identification of B. cereus as the etiologic agent of pneumonia is not common, it has been reported and is generally, but not exclusively, associated with significant risk factors. Miller et al. (22) reported on two fatal cases of fulminating bacteremia and pneumonia that occurred in 1995 and 1996 with similarity in their clinical presentation to the present study, but those B. cereus strains did not contain pagA-like genes. Recently, two cases of fatal respiratory illness in the United States were also attributed to B. cereus isolates, and preliminary tests indicated the presence of a B. anthracis-like pagA gene in these isolates (A.R.H. and T.P., unpublished data). Further characterization of these and other B. cereus isolates from cases of severe pneumonia, for which the Centers for Disease Control and Prevention is in the process of setting up a prospective surveillance, could potentially reveal the true burden of disease caused by isolates harboring what are traditionally considered B. anthracis virulence plasmids and/or their genes. The presence of the pXO1 and pXO2 plasmid-associated genes, however, is not normally investigated in an isolate unless it is suspected to be B. anthracis. In addition, the isolation of B. cereus in a clinical laboratory is frequently considered contamination, resulting in it being discarded rather than to follow up with further characterization and reporting (5). Consequently, clinical isolates of species other than B. anthracis containing pXO1 or its genes may have been missed.
The rapidity with which whole-genome sequencing data can currently be obtained provides a new approach to the public health challenges associated with emerging diseases (29). The high-coverage draft genome data on G9241 not only clarified the relationship of this isolate to other members of the B. cereus group but also provided direct insight into the correlation of phenotypic characteristics and the genetic basis for their presentation. Recent studies have shown that genes that have traditionally been considered restricted to B. cereus or B. anthracis are actually more widespread (10, 30-32). Although genomic sequences with homology to B. anthracis pXO1 and pXO2 sequences have been detected in other Bacillus spp. (12), this work reports on the toxin genes and an entire pXO1-like plasmid found outside of a B. anthracis isolate.
Identification of Bacillus spp. containing the B. anthracis virulence genes and able to cause severe respiratory illness that could potentially be confused with inhalation anthrax adds substantially to the complexity of clinical and laboratory diagnosis in general and particularly during a potential bioterrorism event. Given that pXO1- and pXO2-based genes and/or their encoded products are the most frequently used targets to detect and identify B. anthracis, false positive results could occur and result in unnecessary alarm. On the other hand, it may not be appropriate to consider B. anthracis, as currently defined, as the only species capable of causing inhalation anthrax-like disease. Although this isolate caused a respiratory illness, it will also be interesting to study the potential of this isolate to cause gastrointestinal or cutaneous infections similar to B. anthracis. Limiting screening for B. anthracis-specific phenotypes rules out isolates that are hemolytic and/or motile, such as the B. cereus described in this study. A more sophisticated system to prospectively monitor for the presence of B. anthracis-specific virulence plasmids and plasmid-associated genes in Bacillus spp. other than B. anthracis may have to be developed. Vigilance and close communication between clinicians treating patients and laboratory scientists is needed to assure that the true causative agents are rapidly isolated and identified.
The discovery of a pathogen such as B. cereus G9241 also emphasizes the challenges of creating lists of potential biothreat agents. Although it is not practical to include every pathogenic species on such lists, it should be noted that depending on the extent of lateral gene transfer, nature could produce an unlimited number of variations and combinations. We must not only be able to quickly recognize the clearly identified select agents but be flexible enough to rapidly identify and respond to other agents. However, premature conclusions about origins of novel pathogens (whether natural or the result of bioterrorism events) with properties similar to species on the select agent list must be avoided.
Supplementary Material
Acknowledgments
We thank Dr. Roland J. Degeyter, Dr. Mickey Viator, and Penny Cuneo for their contributions and Captain Alfred Mateczun, Robert Bull, Linwood Johnson, Les Baillie, and Peter Turnbull for their assistance. Funding for the mouse challenge studies was provided by the Defense Threat Reduction Agency. This work was supported by the National Institute of Allergy and Infectious Diseases, National Institutes of Health, under contract no. N01-AI15447.
Abbreviations: CGH, comparative genomic hybridization; PA, protective antigen; DFA, direct fluorescent Ab.
Data deposition: The Whole Genome Shotgun project reported in this work has been deposited in the GenBank database (accession no. AAEK00000000). The version described in this paper is the first version, AAEK01000000.
References
- 1.Helgason, E., Økstad, O. A., Caugant, D. A., Johansen, H. A., Fouet, A., Mock, M., Hegna, I. & Kolstø, A. B. (2000) Appl. Environ. Microbiol. 66, 2627-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ticknor, L. O., Kolstø, A. B., Hill, K. K., Keim, P., Laker, M. T., Tonks, M. & Jackson, P. J. (2001) Appl. Environ. Microbiol. 67, 4863-4873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daffonchio, D., Cherif, A. & Borin, S. (2000) Appl. Environ. Microbiol. 66, 5460-5468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cherif, A., Brusetti, L., Borin, S., Rizzi, A., Boudabous, A., Khyami-Horani, H. & Daffonchio, D. (2003) J. Appl. Microbiol. 94, 1108-1119. [DOI] [PubMed] [Google Scholar]
- 5.Logan, N. A. & Turnbull, P. C. (1999) in Manual of Clinical Microbiology, ed. Murray, P. R. (Am. Soc. Microbiol., Washington, DC), pp. 357-369.
- 6.Jernigan, D. B., Raghunathan, P. L., Bell, B. P., Brechner, R., Bresnitz, E. A., Butler, J. C., Cetron, M., Cohen, M., Doyle, T., Fischer, M., et al. (2002) Emerg. Infect. Dis. 8, 1019-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okinaka, R. T., Cloud, K., Hampton, O., Hoffmaster, A. R., Hill, K. K., Keim, P., Koehler, T. M., Lamke, G., Kumano, S., Mahillon, J., et al. (1999) J. Bacteriol. 181, 6509-6515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okinaka, R., Cloud, K., Hampton, O., Hoffmaster, A., Hill, K., Keim, P., Koehler, T., Lamke, G., Kumano, S., Manter, D., et al. (1999) J. Appl. Microbiol. 87, 261-262. [DOI] [PubMed] [Google Scholar]
- 9.Green, B. D., Battisti, L., Koehler, T. M., Thorne, C. B. & Ivins, B. E. (1985) Infect. Immun. 49, 291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Read, T. D., Peterson, S. N., Tourasse, N., Baillie, L. W., Paulsen, I. T., Nelson, K. E., Tettelin, H., Fouts, D. E., Eisen, J. A., Gill, S. R., et al. (2003) Nature 423, 81-86. [DOI] [PubMed] [Google Scholar]
- 11.Myers, E. W., Sutton, G. G., Delcher, A. L., Dew, I. M., Fasulo, D. P., Flanigan, M. J., Kravitz, S. A., Mobarry, C. M., Reinert, K. H., Remington, K. A., et al. (2000) Science 287, 2196-2204. [DOI] [PubMed] [Google Scholar]
- 12.Rasko, D. A., Ravel, J., Økstad, O. A., Helgason, E., Cer, R. Z., Jiang, L., Shores, K. A., Fouts, D. E., Tourasse, N. J., Angiuoli, S. V., et al. (2004) Nucleic Acids Res. 32, 977-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peterson, J. D., Umayam, L. A., Dickinson, T., Hickey, E. K. & White, O. (2001) Nucleic Acids Res. 29, 123-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chapin, K. C. & Murray, P. R. (2003) in Manual of Clinical Microbiology, eds. Murray, P. R., Baron, E. J., Jorgensen, J. H., Pfaller, M. A. & Yolken, R. H. (Am. Soc. Microbiol., Washington, DC), pp. 257-267.
- 15.Brown, E. R. & Cherry, W. B. (1955) J. Infect. Dis. 96, 34-39. [DOI] [PubMed] [Google Scholar]
- 16.De, B. K., Bragg, S. L., Sanden, G. N., Wilson, K. E., Diem, L. A., Marston, C. K., Hoffmaster, A. R., Barnett, G. A., Weyant, R. S., Abshire, T. G., et al. (2002) Emerg. Infect. Dis. 8, 1060-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sacchi, C. T., Whitney, A. M., Mayer, L. W., Morey, R., Steigerwalt, A., Boras, A., Weyant, R. S. & Popovic, T. (2002) Emerg. Infect. Dis. 8, 1117-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saitou, N. & Nei, M. (1987) Mol. Biol. Evol. 4, 406-425. [DOI] [PubMed] [Google Scholar]
- 19.Read, T. D., Myers, G. S., Brunham, R. C., Nelson, W. C., Paulsen, I. T., Heidelberg, J., Holtzapple, E., Khouri, H., Federova, N. B., Carty, H. A., et al. (2003) Nucleic Acids Res. 31, 2134-2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ivanova, N., Sorokin, A., Anderson, I., Galleron, N., Candelon, B., Kapatral, V., Bhattacharyya, A., Reznik, G., Mikhailova, N., Lapidus, A., et al. (2003) Nature 423, 87-91. [DOI] [PubMed] [Google Scholar]
- 21.Beedham, R. J., Turnbull, P. C. & Williamson, E. D. (2001) Vaccine 19, 4409-4416. [DOI] [PubMed] [Google Scholar]
- 22.Miller, J. M., Hair, J. G., Hebert, M., Hebert, L., Roberts, F. J., Jr., & Weyant, R. S. (1997) J. Clin. Microbiol. 35, 504-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jernigan, J. A., Stephens, D. S., Ashford, D. A., Omenaca, C., Topiel, M. S., Galbraith, M., Tapper, M., Fisk, T. L., Zaki, S., Popovic, T., et al. (2001) Emerg. Infect. Dis. 7, 933-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agaisse, H., Gominet, M., Økstad, O. A., Kolstø, A. B. & Lereclus, D. (1999) Mol. Microbiol. 32, 1043-1053. [DOI] [PubMed] [Google Scholar]
- 25.Mignot, T., Mock, M., Robichon, D., Landier, A., Lereclus, D. & Fouet, A. (2001) Mol. Microbiol. 42, 1189-1198. [DOI] [PubMed] [Google Scholar]
- 26.Price, L. B., Hugh-Jones, M., Jackson, P. J. & Keim, P. (1999) J. Bacteriol. 181, 2358-2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keim, P., Kalif, A., Schupp, J., Hill, K., Travis, S. E., Richmond, K., Adair, D. M., Hugh-Jones, M., Kuske, C. R. & Jackson, P. (1997) J. Bacteriol. 179, 818-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mourez, M., Yan, M., Lacy, D. B., Dillon, L., Bentsen, L., Marpoe, A., Maurin, C., Hotze, E., Wigelsworth, D., Pimental, R. A., et al. (2003) Proc. Natl. Acad. Sci. USA 100, 13803-13808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marra, M. A., Jones, S. J., Astell, C. R., Holt, R. A., Brooks-Wilson, A., Butterfield, Y. S., Khattra, J., Asano, J. K., Barber, S. A., Chan, S. Y., et al. (2003) Science 300, 1399-1404. [DOI] [PubMed] [Google Scholar]
- 30.Rowan, N. J., Caldow, G., Gemmell, C. G. & Hunter, I. S. (2003) Appl. Environ. Microbiol. 69, 2372-2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pannucci, J., Okinaka, R. T., Williams, E., Sabin, R., Ticknor, L. O. & Kuske, C. R. (2002) BMC Genomics 3, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pannucci, J., Okinaka, R. T., Sabin, R. & Kuske, C. R. (2002) J. Bacteriol. 184, 134-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.