Abstract
We report the identification of Kaposiform hemangioendothelioma of the cecum presenting as colocolic intussusception in a 4-month-old boy without Kasabach–Merrit syndrome. To our knowledge this is the first reported case in the literature of such a presentation.
Keywords: KHE-Kaposiform hemangioendothelioma, KMS-Kasabach Merrit syndrome, Colo colic intussusception
INTRODUCTION
Kaposiform hemangioendothelioma (KHE) is a rare locally aggressive vascular neoplasm. It occurs mainly in infants, children and adolescents with adult presentations constituting a minority of the cases.[1] These lesions are often associated with Kasabach-Merrit syndrome (KMS) and lymphangiomatosis. They can be solitary or multiple and cutaneous lesions are the most common. Visceral involvement is very rare with retroperitoneal and mediastinal lesions being reported. Here we report a case of KHE that occurred in the cecum resulting in colocolic intussusception. There were no other lesions and no KMS.
CASE REPORT
A 4-month-old exclusively breast fed male infant presented to the emergency room of our institution with history of abdominal distention and loose stools for 3 days and bilious vomiting for 1 day. The child was severely dehydrated with abdominal examination revealing generalized tenderness and palpable dilated bowel loops. He was resuscitated with fluid boluses and investigated. Blood investigations were normal, X-ray of the abdomen showed multiple air fluid levels suggestive of intestinal obstruction and ultrasound of the abdomen showed an intussusception that required emergent surgery.
Via a supraumbilical right transverse skin incision, the intussusception was reduced. Further palpation and subsequent enterotomy revealed a 2 × 2 cm firm irregular mass in the cecum [Figure 1]. Limited resection of the ileo cecum with end to end ileocolic anastomosis was done. A biopsy showed the cecum to be transmurally infiltrated by a tumor constituted by bundles of spindle cells and proliferated blood vessels which included ectatic and thrombosed vessels [Figure 2]. Resected margins and lymph nodes were found to be negative for the tumor. Immunohistochemical analysis revealed the spindle cells to be immunopositive for CD 31, FLI-1 and CD 34 supporting a diagnosis of KHE. He made an uneventful recovery and is well with a normal weight gain at a 6-month follow up.
Figure 1.

Cut-open specimen showing the lesion
Figure 2.
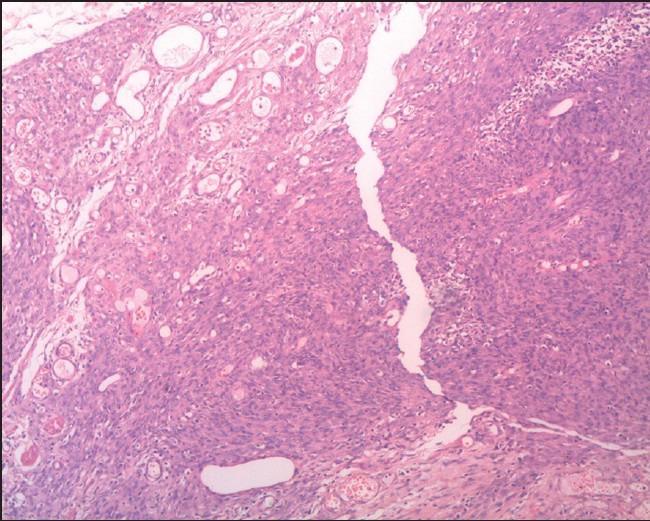
Tumor with areas looking like hemangioma (upper left) and kaposiæs sarcoma (lower right)
DISCUSSION
KHE is a rare locally aggressive endothelium-derived spindle cell neoplasm seen predominantly in infants and children. It was first described in 1993 by Zuckerberg et al.,[2] The name originated from the fact that this lesion showed features common to both capillary hemangioma and Kaposi sarcoma. Cutaneous lesions are common with visceral involvement (mediastinum[3] and retroperitoneum) being extremely rare. Extremity, retroperitoneal and mediastinal lesions are usually associated with KMS[4] and lymphangiomatosis.
The most common mode of presentation is that of a progressively enlarging, irregular, superficial (violaceous plaque) or deep soft tissue mass in the extremities or the upper trunk. Symptoms of retroperitoneal and mediastinal KHE are mainly related to tumor growth and associated KMS. Tumor growth can cause extensive soft tissue involvement and bone destruction. Bone involvement in KHE is virtually indistinguishable radiographically from the bone involvement that occurs in rhabdomyosarcoma or aggressive fibromatosis. KHE has an unpredictable clinical course in that some can undergo spontaneous regression and some, particularly those in the mediastinum and retroperitoneum, can form extensive unresectable lesions. Because of this, lesions in the retroperitoneum and the mediastinum reportedly have a high morbidity and mortality. These lesions tend to be locally invasive but do not produce distant metastasis.
Definitive diagnosis is obtained by histological analysis. Histologically, KHE consists of irregular tumor nodules that infiltrate soft tissue and produce a dense hyaline stromal response. These tumors are intimately associated with thin-walled lymphatic vessels. The irregular tumor nodule is composed of spindle-shaped endothelial cells with abundant eosinophilic cytoplasm that form cresenteric vascular spaces and fragmented red cells. The cytoplasm contains hemosiderin, hyaline globules and cytoplasmic vacuoles [Figure 2].[5] Immunohistochemical analysis shows the nodules to be positive for CD 31, CD 34 and Friend leukemia virus integration-1 (FLI-1) but negative for GLUT-1 and Lewis Y antigen (LeY).
The most important prognostic factors are the size of the tumor, the location of the tumor and the presence of consumptive coagulopathy. Small cutaneous lesions without coagulopathy are the ones with the best prognosis. Treatment mainly depends on the location and the extent of the tumor. Although the definitive treatment is complete surgical excision, medical measures are indicated in incompletely excised lesions or those lesions with associated KMS. The most commonly used medical measures are steroids and interferon with anti-cancer drugs like cyclophosphamide, actinomycin D and vincristine being used rarely.
In our case the child presented to us with features of intestinal obstruction. Ultrasound of the abdomen showed intussusception. As he presented 72 hours after the onset of symptoms a decision was made not to try pneumatic reduction and proceed directly with surgery. Also the fact that the child was exclusively breast fed pointed to a pathological lead point being the cause for intussusception. This is the first instance where KHE of the cecum presenting as colocolic intussusception without KMS is being described. A wide local excision in the form of a limited ileocaecal resection with end to end ileocolic anastomosis is indicated in such cases.
CONCLUSION
KHE is a locally aggressive vascular neoplasm. KHE involving a visceral location is extremely rare with only few cases being reported in the literature. As far as we know, this is the first reported case of KHE of the cecum presenting as colocolic intussusception without KMS. As with any case of KHE amenable to surgical excision, the treatment of caecal KHE is limited resection of the section of intestine containing the tumor.[1]
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
REFERENCES
- 1.Drolet BA, Trenor CC, 3rd, Brandao LR, Chiu YE, Chun RH, Dasgupta R, et al. Consensus-derived practice standards plan for complicated Kaposiform hemangioendothelioma. J Pediatr. 2013;163:285–91. doi: 10.1016/j.jpeds.2013.03.080. [DOI] [PubMed] [Google Scholar]
- 2.Zukerberg LR, Nickoloff BJ, Weiss SW. Kaposiform hemangioendothelioma of infancy and childhood. An aggressive neoplasm associated with Kasabach-Merritt syndrome and lymphangiomatosis. Am J Surg Pathol. 1993;17:321–8. doi: 10.1097/00000478-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Iwami D, Shimaoka S, Mochizuki I, Sakuma T. Kaposiform hemangioendothelioma of the mediastinum in a 7-month-old boy: A case report. J Pediatr Surg. 2006;41:1486–8. doi: 10.1016/j.jpedsurg.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Jahnel J, Lackner H, Reiterer F, Urlesberger B, Urban C. Kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon: From vincristine to sirolimus. Klin Padiatr. 2012;224:395–7. doi: 10.1055/s-0032-1323823. [DOI] [PubMed] [Google Scholar]
- 5.DeFatta RJ, Verret DJ, Adelson RT, Gomez A, Myers LL. Kaposiform Hemangioendothelioma: Case report and literature review. Laryngoscope. 2005;115:1789–92. doi: 10.1097/01.mlg.0000176539.94515.75. [DOI] [PubMed] [Google Scholar]


