Abstract
Background: Magnetic resonance imaging (MRI) is widely used in clinical practice, and “abnormal brain MRI” findings often prompt assessment for multiple sclerosis (MS), even when there are no symptoms suggestive of the disease. Despite several studies involving individuals with “radiologically isolated syndrome” (RIS), little is known about what factors might predict future development of MS. The objective of this study was to longitudinally evaluate clinical and MRI characteristics of people who presented to an MS clinic because of incidental abnormal MRI findings but did not have typical symptoms of MS, in order to assess risk factors for developing MS.
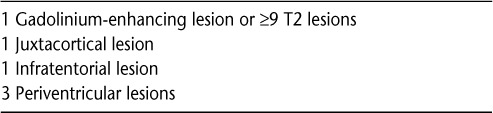
Methods: Thirty consecutive patients presenting to an MS clinic for evaluation of abnormal MRI findings were enrolled in the study. Clinical and paraclinical data, including MRI results, were reviewed. Magnetic resonance imaging findings of T2 hyperintensities measuring more than 3 mm in diameter and fulfilling at least three out of four Barkhof criteria, with or without gadolinium-enhancing lesions, were considered to be suggestive of MS.
Results: The median follow-up time was 5.5 years. No participants without MRI findings suggestive of MS were diagnosed with MS (P = .005). Fifteen participants had MRI findings suggestive of MS. Seven of the 15 (47%) were diagnosed with MS on follow-up. Cerebrospinal fluid (CSF) testing results were available for 15 participants. Abnormal results were found in six participants, of whom five (83%) also had MRI findings suggestive of MS. Only two of the nine (22%) participants with normal CSF results (P = .04) had MRI findings suggestive of MS.
Conclusions: In our cohort, none of the participants without MRI findings suggestive of MS developed MS. The participants with MRI findings suggestive of MS were more likely to develop symptoms and MRI changes typical of MS on follow-up.
Multiple sclerosis (MS) is an inflammatory and neurodegenerative disease affecting more than 2.5 million people worldwide (primarily young adults) that may lead to significant disability.1 Diagnosis of MS requires demonstration of dissemination in time and space of central nervous system lesions with the presence of at least one clinical event and objective clinical findings.2 Over the years the diagnostic criteria have been revised, mostly in relation to magnetic resonance imaging (MRI) findings, in order to reach an earlier diagnosis and enable earlier initiation of specific treatment.3 The dissemination in time and space can now be determined with serial MRI3; however, for the diagnosis to be made, a clinical event is still paramount.
Radiologically isolated syndrome (RIS) is a term used to describe MRI changes typical of MS that occur in asymptomatic individuals.4 Brain lesions typical of MS were described by Phadke and Best5 in 1983 in individuals without diagnoses of MS following brain autopsy. Several case reports followed in which incidental brain MRI findings were suggestive of MS, yet full neurologic evaluations did not reveal symptoms or findings consistent with a diagnosis of MS.6–8 Because of the widespread use of MRI in clinical practice, incidental findings of brain lesions have become increasingly common, often prompting assessment for MS due to “abnormal brain MRI.” The purpose of this study was to longitudinally evaluate individuals who presented to the MS clinic at the Henry Ford Hospital because of an incidental finding of “abnormal brain MRI,” in an effort to assess risk factors for developing MS.
Methods
Participants
Thirty consecutive individuals with “abnormal brain MRI” presenting to the MS clinic for assessment for possible MS were included in the study and followed longitudinally. None of the participants had experienced an episode of neurologic symptoms suggestive of clinical manifestation of MS. All participants had previously undergone MRI because of various symptoms, most frequently headache. Some participants had undergone cerebrospinal fluid (CSF) or evoked potential tests to assess for evidence of MS, or blood tests to assess for different inflammatory/infectious disorders. All participants had undergone a full neurologic examination at presentation in the clinic, and none had abnormal findings. All aspects of the study protocol were reviewed and approved by the Henry Ford Health System institutional review board.
Procedure
Magnetic resonance imaging scans of all participants were evaluated by the same staff neurologist to determine whether the lesions present were suggestive of MS. Routine MRI scans were obtained at 1.5 or 3 T, and conventional images were reviewed with neuroradiologists to eliminate potential differences in technical quality. Images were considered to be suggestive of MS if they showed T2-hyperintense lesions greater than 3 mm in diameter and fulfilled the Barkhof criteria (Table 1).9,10 Cerebrospinal fluid analysis was offered to all participants, and 15 of them agreed to have a spinal tap 1 to 2 weeks following the initial visit. The CSF findings were considered abnormal if there were two or more oligoclonal bands that were not present in corresponding serum or an elevated IgG index. Participants were evaluated clinically every 6 to 12 months and at the end of the study follow-up period; they were categorized as not having MS or as having MS based on the 2005 and/or the 2010 McDonald diagnostic criteria.3,11
Table 1.
Data Analysis
Descriptive characteristics including sex, race, age, symptoms at presentation, and duration of follow-up were recorded. Based on MRI findings at presentation, patients were categorized into those with and without lesions suggestive of MS according to the Barkhof criteria. For those participants who had undergone CSF testing, results were characterized as normal or abnormal, based on the definition given previously. Kaplan-Meier curves and log-rank tests were performed to assess the association between MRI lesions suggestive of MS and time to MS diagnosis (using the 2010 McDonald criteria). Time to MS diagnosis was defined as number of years between initial presentation and MS diagnosis or last follow-up for participants with no MS diagnosis. Given the small sample size of participants with CSF analysis, the association between CSF testing results and time to MS diagnosis was not assessed. However, the association between CSF testing results and the presence of MRI lesions suggestive of MS was assessed using the Fisher exact test. Log-rank and Fisher exact tests were also performed to assess the association of the initial symptoms that prompted the first MRI study with MS diagnosis and the presence of MRI lesions suggestive of MS. Associations were considered to be statistically significant at P < .05. All analyses were conducted using SAS version 9.2. Among participants who were not diagnosed with MS during follow-up, the numbers of individuals with certain presenting symptoms were recorded.
Results
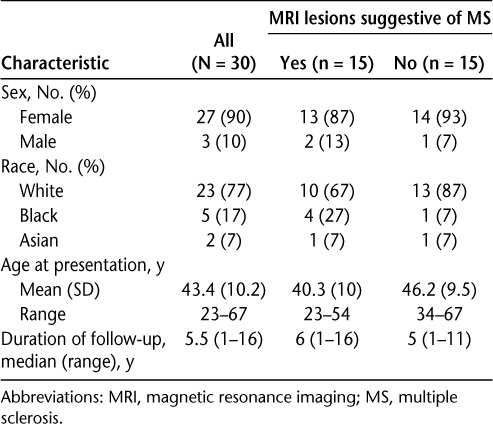
Of the 30 study participants, 90% were female and 77% were white. The mean age at presentation was 43.4 years (range, 23–67 years). The median duration of follow-up was 5.5 years (Table 2).
Table 2.
Sociodemographic characteristics and duration of follow-up
Of the 30 participants, 15 (50%) had presenting MRI scans that met the Barkhof criteria and were considered to be suggestive of MS. Of these 15 participants, 7 (47%) were diagnosed with MS using the 2010 McDonald criteria (4 of whom also met the 2005 criteria), and 8 (53%) were not given the diagnosis of MS during follow-up. All participants who received a diagnosis of MS did so within 4 years. The participants who developed clinical manifestations of MS during follow-up had symptoms of partial myelitis (4), brain stem syndrome (1), and optic neuritis (2). None of the participants whose initial MRI studies did not suggest MS developed clinical manifestations of MS (P = .005) (Figure 1).
Figure 1.
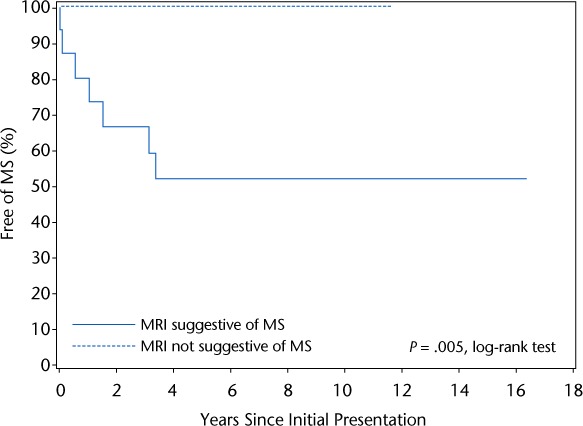
Kaplan-Meier survival analysis of 15 participants with magnetic resonance imaging (MRI) suggestive of multiple sclerosis (MS) and 15 participants with MRI not suggestive of MS and no evidence of clinical manifestations of MS
Of the 15 participants for whom CSF analysis was performed, 6 (40%) had abnormal findings (presence of oligoclonal bands and/or increase in IgG index). Of the six participants with abnormal CSF findings, four were eventually diagnosed with MS, while only one of the nine participants with normal CSF test results eventually developed clinical manifestations of MS meeting the 2010 McDonald criteria. This comparison was not tested because of the small sample size. Of the nine participants who had normal CSF findings, 22% had MRI lesions suggestive of MS, compared with 83% of the participants with abnormal CSF findings (Fisher exact test; P = .04).
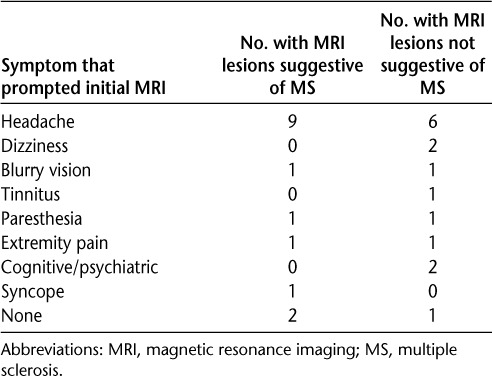
As for symptoms that prompted the first MRI study, headache was the most common (50%). Less common symptoms were dizziness (7%), blurry vision (7%), and paresthesia (7%) (Table 3). The association between presence of headache as an initial symptom prompting the first MRI study and MS diagnosis was not significant (20% with headache vs. 26% without headache; P = .648). The same was true for the association between headache as a symptom and the presence of MRI lesions suggestive of MS (40% with headache vs. 60% without headache; P = .466). For the other symptoms that prompted the first MRI study, the sample size was too small to test the association with MS diagnosis and presence of MRI lesions suggestive of MS.
Table 3.
Symptoms in relation to presenting MRI characteristics
Discussion
The purpose of this study was to evaluate the risk of developing MS among individuals who presented to an MS clinic because of abnormalities seen on brain MRI, but who did not have clinical manifestations of MS. In practice, misdiagnosis of MS is common; in addition to having significant health and social consequences, this may lead to unnecessary health-care costs.12
The results of our study showed that none of the participants without symptoms and MRI findings suggestive of MS developed MS during follow-up. This finding may help physicians to decide whether to order follow-up brain MRI scans for individuals who lack symptoms and MRI findings suggestive of MS. Particularly in the United States, brain MRI is frequently performed because of a variety of symptoms, leading to potential overuse of this diagnostic procedure.
Headache was the presenting symptom for the majority of our study participants with abnormal MRI findings not suggestive of MS. A Dutch population-based study found that patients with migraine, with and without aura, are at increased risk of having deep white matter lesions.13 Also, subclinical vascular changes and white matter lesions are common in the general population, and their prevalence increases with age.14–16 A recent MRI study of patients with headaches found white matter hyperintensities in approximately 51%, with modified Barkhof criteria met in 2.4% to 7.1%.17 The study did not include clinical and laboratory information on those patients or follow-up.
In the present study, participants who had MRI findings meeting the Barkhof criteria were more likely to develop MS. Participants who had MRI lesions suggestive of MS were also more likely to have abnormal CSF study results. This suggests that in some people, RIS consists of an asymptomatic period before the clinical presentation of MS4,18,19; however, it is unclear why some people with RIS progress to MS while others do not. In previous studies, attempts were made to assess the association of abnormal CSF testing results in RIS with progression to clinically isolated syndrome (CIS) or MS. One study involving 41 patients found no increased risk of radiologic or clinical progression with the presence of oligoclonal bands or elevated IgG index in CSF.4 Another study involving 70 patients found that CSF abnormalities were predictive when associated with nine or more T2-hyperintense lesions on initial MRI.18 The same study found that abnormal visual evoked potential (VEP) at baseline was a predictive factor for developing CIS.18 In our study, only ten participants had evoked potential studies performed, and the data could not be analyzed because of the small number (data not shown). Of four participants who were subsequently diagnosed with MS, one had abnormal VEP at presentation; another one had abnormal somatosensory evoked potential (SSEP). Seven participants whose initial MRI studies did not suggest MS had normal evoked potential studies (VEP and SSEP). Further studies are needed to clarify the predictive value of CSF and VEP testing in progression to clinically definitive MS.
A number of studies have been conducted to determine other factors that predict the evolution of RIS into MS. Some studies have suggested that the presence of infratentorial, spinal cord, or cortical lesions increases the risk of progression to MS.20–22 A recent study found that although macroscopic brain damage was similar in RIS and relapsing-remitting MS (RRMS), magnetization transfer ratio (MTr), which reveals subtle tissue damage, was milder in RIS than in RRMS. This new approach could be useful for differentiating cases of RIS with a high likelihood of progression from those that will remain asymptomatic.23 Other studies have focused on family history of MS and found that individuals who have first-degree relatives with MS are more likely to have asymptomatic brain lesions on MRI.24 In addition, although MRI has helped in understanding MS pathology and in management of disease, it captures only a small fraction of MS-related changes that may be detectable by other techniques or by pathological assessment.25 For example, a recent study has suggested that people with RIS have a similar cognitive deficit profile as those with MS and that such individuals may have an undiagnosed CIS presenting as cognitive dysfunction.26
The natural course of RIS is still unknown. Yielding findings similar to ours, a few cohort studies have indicated that one-third of cases of RIS will convert to MS during a 5-year follow-up and two-thirds will show radiologic progression.4,18 There are no guidelines concerning treatment of RIS.27 Although an increasing number of studies have highlighted the role of early pharmacologic therapy in CIS,28,29 early treatment with disease-modifying therapies is still debatable even in CIS. One-third of individuals with RIS develop neurologic symptoms during follow-up.30 In our study, the likelihood of developing clinical manifestations of MS in these individuals was 47%. The literature indicates a risk of clinical conversion of between 15% and 50% in patients with RIS.30 The prevalence of conversion to MS among patients with CIS in 12 to 24 months' follow-up has been reported as between 31% and 45%.9,10 A patient-specific approach to follow these individuals with RIS has been proposed.31 Our study may provide guidance in identifying patients who may need close follow-up.
Limitations
The present study has several limitations. First, the sample size is not large enough for risk stratification according to the number of Barkhof criteria met. The number of participants undergoing CSF analysis was also small. Obtaining CSF studies for all participants could be useful for further assessing the combined risk of having both abnormal MRI and abnormal CSF findings. Second, the specificity of the Barkhof criteria has been debated.32 These results, however, provide additional evidence for the utility of these criteria. In addition, our study was conducted using conventional MRI; thus the results apply only to conventional imaging.
Conclusion
This study found that patients lacking symptoms and MRI findings suggestive of MS were not at risk of developing clinically definitive MS during follow-up. However, the presence of MRI lesions suggestive of MS at presentation, described in the literature as RIS, increased the risk of developing MS later in life. Larger-scale studies of RIS are needed to determine additional specific characteristics that increase the risk of developing clinical manifestations of MS in the future. Such data will be valuable in helping to counsel patients, plan imaging follow-up, and identify treatment options.
PracticePoints.
Individuals with symptoms and magnetic resonance imaging (MRI) findings not suggestive of MS and with normal cerebrospinal fluid (CSF) testing results are unlikely to develop definitive MS on follow-up.
Individuals with MRI lesions suggestive of MS but without symptoms suggestive of MS (radiologically isolated syndrome) are at some risk of developing MS. Abnormal CSF results may add to this risk.
Further studies are needed on radiologically isolated syndrome in order to determine the best way to follow these individuals clinically and radiologically and to make decisions regarding therapeutic management.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Confavreux C, Vukusic S. The clinical epidemiology of multiple sclerosis. Neuroimaging Clin N Am. 2008;18:589–622. doi: 10.1016/j.nic.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 2.McDonald WI, Compston A, Edan G et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on Diagnosis of Multiple Sclerosis. Ann Neurol. 2001;50:121–127. doi: 10.1002/ana.1032. [DOI] [PubMed] [Google Scholar]
- 3.Polman CH, Reingold SC, Banwell B et al. Diagnostic criteria for multiple sclerosis: 2010 revision to the McDonald criteria. Ann Neurol. 2011;69:292–302. doi: 10.1002/ana.22366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okuda DT, Mowry EM, Beheshtian A et al. Incidental MRI abnormalities suggestive of multiple sclerosis. Neurology. 2009;72:800–805. doi: 10.1212/01.wnl.0000335764.14513.1a. [DOI] [PubMed] [Google Scholar]
- 5.Phadke JG, Best PV. Atypical and clinically silent multiple sclerosis: a report of 12 cases discovered unexpectedly at autopsy. J Neurol Neurosurg Psychiatry. 1983;46:414–420. doi: 10.1136/jnnp.46.5.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McDonnell GV, Cabrera-Gomez J, Calne DB et al. Clinical presentation of primary progressive multiple sclerosis 10 years after the incidental finding of typical magnetic resonance imaging brain lesions—the subclinical stage of primary progressive multiple sclerosis may last 10 years. Mult Scler. 2003;9:204–209. doi: 10.1191/1352458503ms890cr. [DOI] [PubMed] [Google Scholar]
- 7.de Seze J, Vermersch P. Sequential magnetic resonance imaging follow-up of multiple sclerosis before the clinical phase. Mult Scler. 2005;11:395–397. doi: 10.1191/1352458505ms1179oa. [DOI] [PubMed] [Google Scholar]
- 8.Hakiki B, Goretti B, Portaccio E et al. ‘Subclinical MS’: follow-up of four cases. Eur J Neurol. 2008;18:858–861. doi: 10.1111/j.1468-1331.2008.02155.x. [DOI] [PubMed] [Google Scholar]
- 9.Barkhof F, Filippi M, Miller DH et al. Comparison of MRI criteria at first presentation to predict conversion to clinically definite multiple sclerosis. Brain. 1997;120:2059–2069. doi: 10.1093/brain/120.11.2059. [DOI] [PubMed] [Google Scholar]
- 10.Tintore M, Rovira A, Martinez MJ et al. Isolated demyelinating syndrome: comparison of different MR imaging criteria to predict conversion to clinically definite multiple sclerosis. Am J Neuroradiol. 2000;21:702–706. [PMC free article] [PubMed] [Google Scholar]
- 11.Polman CH, Reingold ST, Edan G et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria.”. Ann Neurol. 2005;58:840–846. doi: 10.1002/ana.20703. [DOI] [PubMed] [Google Scholar]
- 12.Solomon AJ, Klein EP, Bourdette D. “Undiagnosing” multiple sclerosis: the challenge of misdiagnosis in MS. Neurology. 2012;78:1986–1991. doi: 10.1212/WNL.0b013e318259e1b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kruit MC, van Buchem MA, Hofman PAM et al. Migraine as a risk factor for subclinical brain lesions. JAMA. 2004;291:427–434. doi: 10.1001/jama.291.4.427. [DOI] [PubMed] [Google Scholar]
- 14.Howard G, Wagenknecht LE, Cai J et al. Cigarette smoking and other risk factors for silent cerebral infarction in the general population. Stroke. 1998;29:913–917. doi: 10.1161/01.str.29.5.913. [DOI] [PubMed] [Google Scholar]
- 15.de Leeuw FE, de Groot JC, Achten E et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. J Neurol Neurosurg Psychiatry. 2001;70:9–14. doi: 10.1136/jnnp.70.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vernooji MW, Ikram A, Tanghe HL et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007;357:1821–1828. doi: 10.1056/NEJMoa070972. [DOI] [PubMed] [Google Scholar]
- 17.Liu S, Kullnat J, Bourdette D et al. Prevalence of brain magnetic resonance imaging meeting Barkhof and McDonald criteria for dissemination in space among headache patients. Mult Scler J. 2013;19:1101–1105. doi: 10.1177/1352458512471874. [DOI] [PubMed] [Google Scholar]
- 18.Lebrun C, Bensa C, Debouverie M et al. Association between clinical conversion to multiple sclerosis in radiologically isolated syndrome and magnetic resonance imaging, cerebrospinal fluid and visual evoked potential. Arch Neurol. 2009;66:841–846. doi: 10.1001/archneurol.2009.119. [DOI] [PubMed] [Google Scholar]
- 19.Siva A, Saip S, Altintas A et al. Multiple sclerosis risk in radiologically uncovered asymptomatic possible inflammatory-demyelinating disease. Mult Scler. 2009;15:918–927. doi: 10.1177/1352458509106214. [DOI] [PubMed] [Google Scholar]
- 20.Maia ACM, da Rocha AJ, Borros BR, Tilbery CP. Incidental demyelinating inflammatory lesions in asymptomatic patients: a Brazilian cohort with radiologically isolated syndrome and a critical review of current literature. Arq Neuropsiquiatr. 2012;70:5–11. doi: 10.1590/s0004-282x2012000100003. [DOI] [PubMed] [Google Scholar]
- 21.Okuda DT, Mowry EM, Cree BA et al. Asymptomatic spinal cord lesions predict disease progression in radiologically isolated syndrome. Neurology. 2011;76:686–692. doi: 10.1212/WNL.0b013e31820d8b1d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giorgio A, Stromillo ML, Rossi F et al. Cortical lesions in radiologically isolated syndrome. Neurology. 2011;77:1896–1899. doi: 10.1212/WNL.0b013e318238ee9b. [DOI] [PubMed] [Google Scholar]
- 23.De Stefano N, Stromillo ML, Rossi F et al. Improving the characterization of radiologically isolated syndrome suggestive of multiple sclerosis. PloS One. 2011;6:e19452. doi: 10.1371/journal.pone.0019452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tienari PJ, Salonen O, Wikstrom J et al. Familial multiple sclerosis: MRI findings in clinically affected and unaffected siblings. J Neurol Neurosurg Psychiatry. 1992;55:883–886. doi: 10.1136/jnnp.55.10.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sicotte NL. Imaging in multiple sclerosis: the role of conventional imaging. Neurol Clin. 2011;29:343–356. doi: 10.1016/j.ncl.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 26.Lebrun C, Blanc F, Brassat D et al. Cognitive function in radiologically isolated syndrome. Mult Scler. 2010;16:919–925. doi: 10.1177/1352458510375707. [DOI] [PubMed] [Google Scholar]
- 27.Brassat D, Lebrun-Frenay C. Treat patients with radiologically isolated syndrome when MRI brain scan shows dissemination in time: yes. Mult Scler. 2012;18:1531–1532. doi: 10.1177/1352458512462268. [DOI] [PubMed] [Google Scholar]
- 28.Kappos L, Polman C, Freedman M et al. Treatment with interferon beta 1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes. Neurology. 2006;67:1242–1249. doi: 10.1212/01.wnl.0000237641.33768.8d. [DOI] [PubMed] [Google Scholar]
- 29.Comi G, Martinelli V, Rodegher M et al. Effects of early treatment with glatiramer acetate in patients with clinically isolated syndrome. Mult Scler. 2013;19:1074–1083. doi: 10.1177/1352458512469695. [DOI] [PubMed] [Google Scholar]
- 30.Granberg T, Martola J, Kristoffersen-Wiberg M et al. Radiologically isolated syndrome—incidental magnetic resonance imaging findings suggestive of multiple sclerosis, a systematic review. Mult Scler. 2012;19:271–280. doi: 10.1177/1352458512451943. [DOI] [PubMed] [Google Scholar]
- 31.Sellner J, Schirmer L, Hemmer B, Muhlau M. The radiologically isolated syndrome: take action when the unexpected is uncovered? J Neurol. 2010;257:1602–1611. doi: 10.1007/s00415-010-5601-9. [DOI] [PubMed] [Google Scholar]
- 32.Sastre-Garriga J, Tintoré M, Rovira A et al. Specificity of Barkhof criteria in predicting conversion to multiple sclerosis when applied to clinically isolated brainstem syndromes. Arch Neurol. 2004;61:222–224. doi: 10.1001/archneur.61.2.222. [DOI] [PubMed] [Google Scholar]


