Abstract
Background
On March 11, 2011, a massive undersea earthquake and tsunami struck East Japan. Few studies have investigated the impact of exposure to a natural disaster on preschool children. We investigated the association of trauma experiences during the Great East Japan Earthquake on clinically significant behavior problems among preschool children 2 years after the earthquake.
Method
Participants were children who were exposed to the 2011 disaster at preschool age (affected area, n = 178; unaffected area, n = 82). Data were collected from September 2012 to June 2013 (around 2 years after the earthquake), thus participants were aged 5 to 8 years when assessed. Severe trauma exposures related to the earthquake (e.g., loss of family members) were assessed by interview, and trauma events in the physical environment related to the earthquake (e.g. housing damage), and other trauma exposure before the earthquake, were assessed by questionnaire. Behavior problems were assessed by caregivers using the Child Behavior Checklist (CBCL), which encompasses internalizing, externalizing, and total problems. Children who exceeded clinical cut-off of the CBCL were defined as having clinically significant behavior problems.
Results
Rates of internalizing, externalizing, and total problems in the affected area were 27.7%, 21.2%, and 25.9%, respectively. The rate ratio suggests that children who lost distant relatives or friends were 2.36 times more likely to have internalizing behavior problems (47.6% vs. 20.2%, 95% CI: 1.10–5.07). Other trauma experiences before the earthquake also showed significant positive association with internalizing, externalizing, and total behavior problems, which were not observed in the unaffected area.
Conclusions
One in four children still had behavior problems even 2 years after the Great East Japan Earthquake. Children who had other trauma experiences before the earthquake were more likely to have behavior problems. These data will be useful for developing future interventions in child mental health after a natural disaster.
Introduction
On March 11, 2011, a massive undersea earthquake and subsequent tsunami struck East Japan. With a Richter-scale magnitude of 9.0, the Great East Japan Earthquake was one of the most powerful earthquakes on record and the largest to hit Japan. As of September 2013, the Fire and Disaster Management Agency reported 18,703 deaths, 2,674 missing, and 6,220 injured as a result of the disaster [1]. The most severely affected area was located on the Pacific Ocean side of northeast Japan, encompassing Iwate, Miyagi, and Fukushima prefectures, with 21,262 casualties (18,592 deaths and 2,670 people missing) [1]. Furthermore, 1,706 children lost a parent in the disaster [2].
Several studies have reported the impact of natural disasters on children's mental health, including studies on the 1995 Hanshin-Awaji earthquake in Japan [3]–[5], the 1999 Marmara earthquake in Turkey [6]–[11], the 2004 Indian Ocean earthquake and tsunami [12]–[17], Hurricane Katrina in the USA in 2005 [18]–[21], and the 2008 Sichuan earthquake in China [22]–[25]. Interestingly, most of these previous studies focused on posttraumatic stress disorder (PTSD) or depression as mental health outcomes among children, and few studies investigated the impact of exposure to natural disasters on behavior problems, especially in the preschool to pre-adolescent age range. When assessing mental health status among young children after a natural disaster, it is difficult to diagnose PTSD or depression because young children's responses might be unreliable during the psychiatric interview. Instead, a caregiver's assessment of behavior using the Child Behavior Checklist (CBCL) is better suited to identify young children who need mental health services after a natural disaster, as the CBCL has valid cut-off scores that identify clinically significant behavior problems. It has been suggested that PTSD symptoms can be estimated by CBCL [26], but the validity is arguable [27].
McLaughlin et al. reported that 2 years after Hurricane Katrina approximately 15% of children aged 4 to 17 years showed serious emotional disturbances using the Strength and Difficulties Questionnaire, that is, emotional and behavioral problems that cause significant impairment in role functioning [21]. Further, 3 years after the disaster Lowe et al. assessed behavior problems using the Behavioral Problems Index, which is based on the CBCL, and reported that hurricane-related stressors were indirectly associated with behavior problems [28]. Chemtob et al. assessed the impact of the World Trade Center attack on the mental health of preschool children using the CBCL, and reported that 15–30% of preschool children who were exposed to high-intensity traumatic events related to the World Trade Center attack, such as witnessing the towers collapse, had behavioral symptoms [29].
Moreover, as young children are exposed to multiple trauma experiences after a natural disaster, such as losing a home, parent or friend; witnessing a tsunami or fire; seeing a dead body, or experiencing restrictions on their lifestyle due to radiation, it remains unclear which exposure is associated with which mental disorder or behavior problem. Thienkrua et al. reported that after the tsunami in Sumatra, extreme panic or fear was associated with PTSD, whereas believing that one's own or a family member's life had been in danger was associated with depression in children aged 7 to 14 years in Thailand [12]. To the best of our knowledge, no study has reported the association between specific trauma experiences in a natural disaster and behavior problems among preschool children. Further, there is a need to investigate whether trauma experiences that occurred before the Great East Japan Earthquake, such as the loss of a family member or separation from a caregiver, are associated with behavior problems among children in the affected area, which may have no association in the unaffected area.
Thus, the purpose of this study is to investigate the association of trauma experiences among preschool children on clinically significant behavior problems 2 years after the Great East Japan Earthquake.
Methods
Sample
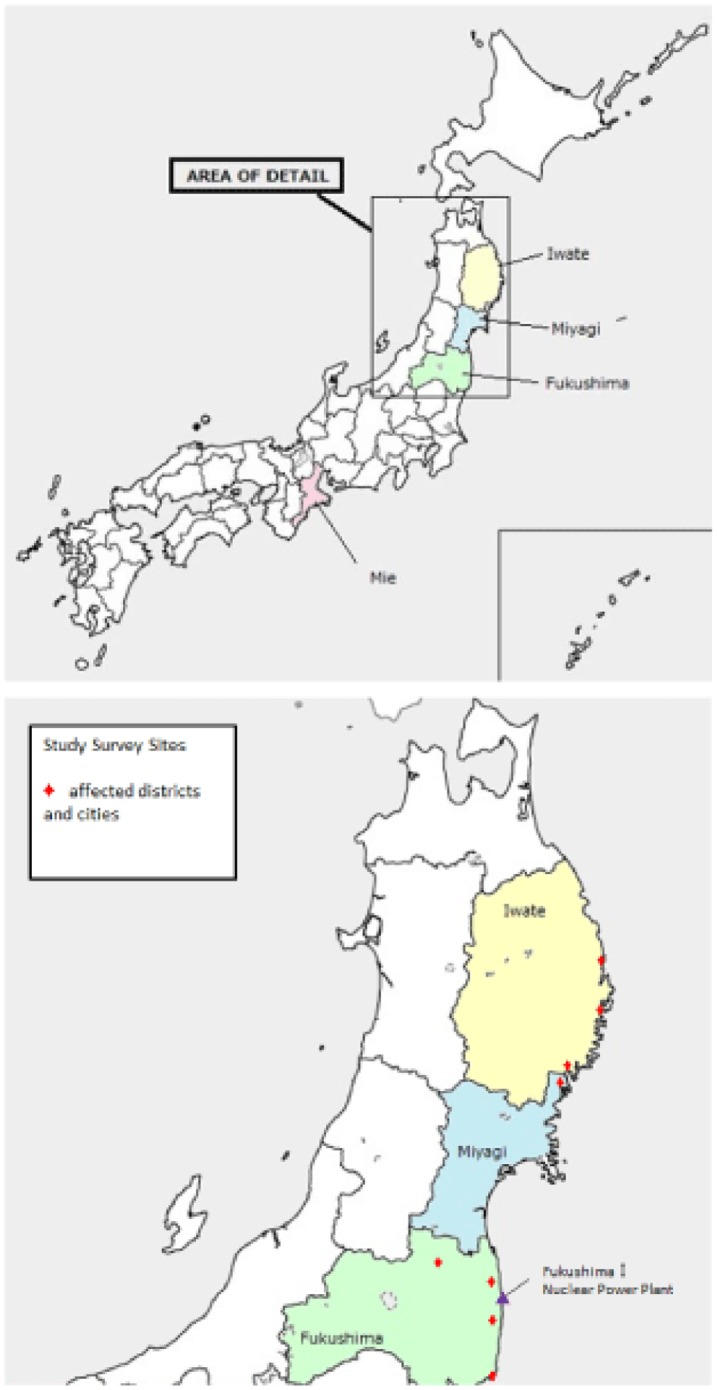
We recruited affected children with a multistage sampling method in Iwate, Miyagi, and Fukushima prefectures, which were closest to the earthquake epicenter and affected by the tsunami (Figure 1). First, we selected municipalities within each prefecture that were severely affected by the tsunami (coastal side) and radiation caused by the nuclear power plant explosion in Fukushima prefecture. Second, we invited preschools in the selected municipalities to participate. In Iwate prefecture, three municipalities were selected, and four of 32 preschools agreed to participate. In Miyagi prefecture, one municipality was selected, and two of 16 preschools agreed to be involved. Further, in Fukushima prefecture, four municipalities were selected and four of 120 preschools agreed to participate. Third, we defined our target sample as children who were enrolled in a class of 3- to 5-year-olds in the fiscal year of 2010, that is, children who experienced the earthquake on March 11, 2011. Then, from September 2012 to June 2013, principals or staff of the preschools asked the caregivers of the targeted children (N = 787) to participate in the study. Finally, the caregivers of 205 children gave informed consent for their child to participate (consent rate: 26.0% of target children) and 178 children (Iwate, 59, Miyagi, 53, Fukushima, 66) completed the questionnaire or interview (participation rate: 87.3% of consented children; 170 completed the questionnaire (95.5%) and 150 completed the interview (84.3%)). Our solicitations to participate were largely refused due to the high transience of residents who had to relocate to other areas after the earthquake, especially in Fukushima. Research coordinators obtained written informed consent from all participants. For children, written informed consent was obtained from the child's parent or legal guardian. The Research Ethics Committee at the National Center for Child Health and Development approved this study, including the informed consent procedure.
Figure 1. Study sites and provinces affected by the Great East Japan Earthquake.
For comparison, we selected Mie prefecture, which is located in West Japan and was unharmed by the earthquake and tsunami on March 11, 2011. Similar to the sampling strategy in the affected area, two municipalities were selected in Mie prefecture, in which one preschool agreed to participate. Children enrolled in the class of 3- to 5-year-olds in the fiscal year of 2010 were selected and recruited, and 30 out of 220 eligible children participated in the study (consent and participation rate: 13.6%). Two additional communities were selected in the municipalities, and caregiver consent to participate was obtained for 52 out of 608 eligible children (consent and participation rate: 8.6%), resulting in a sample of 82 children from unaffected areas (total consent and participation rate: 9.9%).
Measurements
Trauma exposure related to the physical environment was assessed via questionnaires administered from September 2012 to June 2013 (around 2 years after the earthquake). Trauma exposure related to the physical environment included status of the home (lost or completely damaged, partially damaged, or not damaged), experience of staying at a shelter immediately after the earthquake, living in temporary housing, evacuating to a relative's house, and family members living in separate places. We assessed these exposures by asking, for example, “Did you stay at a shelter at the time of the Great East Japan Earthquake?”, for which the response items were “yes” or “no”.
Information on severe trauma exposure was collected through interviews by child psychiatrists or clinical psychologists, who were blinded to the children's psychopathological status. In defining trauma exposure, we referred to a previous study assessing children's mental health [12] and the experiences reported in the affected area of a tsunami. Severe trauma exposure assessed by the semi-structured interview method included separation from caregivers, loss of a close family member, loss of distant relatives or friends, witnessing the tsunami waves, witnessing someone being swept away by the tsunami, witnessing a fire, seeing a dead body, hearing the sound of the nuclear power plant explosion, and experiencing restrictions on their lifestyle due to radiation (e.g. unable to play outside, drink tap water, or eat local food).
Caregivers were also asked questions using the Trauma Events Screening Inventory (TESI-C), modified for use with preschool children [29] and further adapted for use in Japan, inquiring whether the child had experienced a wide range of traumatic events, including the experience of a close friend or family member being involved in a serious accident, suffering from a serious illness or dying; self-injury or serious illness; separation from a caregiver; assault, bullying, or other exposure to violence; and exposure to a natural disaster. Response items included “yes”, “no”, or “unknown”, and only “yes” responses were coded as having the actual experience.
Behavior problems were assessed with the CBCL, which targets children aged 4 to 18 years. Ratings were completed by caregivers [30]. The T score of the CBCL internalizing, externalizing, and total problem scores were calculated using standardized distribution among Japanese children, and a T score over 63 was defined as having clinically significant behavior problems [31].
Covariates, including the child's age, sex, number of siblings, parental age, education, and father's occupation were collected via questionnaire.
Analysis
First, the associations between trauma exposure and behavior problems were analyzed using a bivariate poisson regression model because of the high prevalence of the outcome [32], [33]. Further, multivariate poisson regression using significant variables in bivariate regression was used to examine the independent associations between trauma exposure variables and behavior problems. Moreover, we analyzed the interaction effects between exposure to other trauma before the earthquake and disaster exposure for behavior problems. These analyses were implemented primarily among children in the affected area, and for comparison, the association between other trauma exposure before the earthquake and behavior problems was conducted separately among children in the unaffected area. Stata MP 12 was used for analysis.
Results
Table 1 shows the demographic characteristics of children and their caregivers in the affected area and the rate of clinically significant behavior problems determined by the CBCL. Children's mean age was around 7 years, sex distribution was equal, and approximately 22% had no siblings. In the unaffected area, caregivers who responded (mostly mothers) were older and more highly educated compared to the affected area. Overall, in the affected area the clinical cut-off was exceeded for internalizing, externalizing, and total behavior problems in 27.7% (95% confidence interval [CI]: 20.9–34.4), 21.2% (95% CI: 15.0–27.4), and 25.9% (95% CI: 19.2–32.5) of participants, respectively. The rate of clinically significant behavior problems did not significantly differ by prefecture, although children in Fukushima showed lower rates.
Table 1. Demographic characteristics, trauma exposure related to the Great East Japan Earthquake, other trauma events before the earthquake, and clinically significant behavior problems among young children in the affected area 2 years after the earthquake (N = 170).
| Characteristics | n or Mean | % or SD | |
| Mean child age in years | 7.1 | 1.0 | |
| Child age group | 5 years | 23 | 13.5 |
| 6 years | 64 | 37.7 | |
| 7 years | 38 | 22.4 | |
| 8 years | 45 | 26.5 | |
| Child sex | Boys | 84 | 49.4 |
| Girls | 86 | 50.6 | |
| Number of siblings | No sibling | 37 | 21.8 |
| 1 sibling | 83 | 48.8 | |
| 2+ siblings | 48 | 28.2 | |
| Missing | 2 | 1.2 | |
| Mean caregiver age in years | 36.3 | 6.2 | |
| Caregiver's education | High school or less | 79 | 46.5 |
| Some college | 69 | 40.6 | |
| College+ | 20 | 11.8 | |
| Missing | 2 | 1.2 | |
| Father's occupation before earthquake | Manual/Other/Unemployed | 88 | 51.8 |
| Non-manual | 38 | 22.4 | |
| No response | 44 | 25.9 | |
| Exposure to trauma events related to the Great East Japan Earthquake | Home lost or completely damaged | 45 | 26.5 |
| Home partially damaged | 43 | 25.3 | |
| Stayed at shelter | 50 | 29.4 | |
| Lived in temporary housing | 34 | 20.0 | |
| Evacuated to relative's house | 96 | 56.5 | |
| Family members lived in separate places | 53 | 31.2 | |
| Separation from caregiver | 54 | 31.8 | |
| Lost close family member or relative | 11 | 6.5 | |
| Lost distant relative or friend | 21 | 12.4 | |
| Witnessed tsunami waves | 63 | 37.1 | |
| Witnessed someone being swept away by tsunami | 11 | 6.5 | |
| Witnessed a fire | 30 | 17.7 | |
| Saw a dead body | 3 | 1.8 | |
| Heard the sound of nuclear power plant explosion | 3 | 1.8 | |
| Experienced restrictions on lifestyle due to radiation | 32 | 18.8 | |
| Any of these events | 157 | 92.4 | |
| Number of these events | 3.23 | 1.94 | |
| Exposure to other trauma events before the Great East Japan Earthquake | Involvement in a serious accident | 5 | 2.9 |
| Witnessed a serious accident | 0 | 0 | |
| Attacked by a dog or other animals | 0 | 0 | |
| Had a close friend or family member who had a serious illness | 28 | 16.5 | |
| Death of a close friend or family member | 33 | 19.4 | |
| Visited hospital due to serious disease or injury, or underwent a serious medical procedure, or admitted to hospital | 15 | 8.8 | |
| Separated from a caregiver | 27 | 15.9 | |
| Experienced sexual assault | 0 | 0 | |
| Experienced other criminal assault | 3 | 1.8 | |
| Bullied by peers at preschool or in the neighborhood | 3 | 1.8 | |
| Experienced violence from a close friend or family member | 2 | 1.2 | |
| Witnessed a violent incident involving a close friend or family member | 5 | 2.9 | |
| Had a close friend or family member who attempted suicide | 2 | 1.2 | |
| Experienced a previous natural disaster | 1 | 0.6 | |
| Other stressful events | 5 | 2.9 | |
| Any of these events | 78 | 45.9 | |
| Number of these events | 0.74 | 0.98 | |
| CBCL clinically significant behavior problems | Internalizing problems | 47 | 27.7 |
| Externalizing problems | 36 | 21.2 | |
| Total problems | 44 | 25.9 |
CBCL: Child Behavior Checklist.
Regarding the distribution of trauma experience, 157 children (92.4%) experienced trauma events related to the Great East Japan Earthquake, in which the mean number of trauma events was 3.23 (SD = 1.94, range 0–9). More specifically, the homes of about half of the participants in the affected area were lost, completely damaged, or partially damaged. In terms of traumatic events revealed in the interviews, witnessing tsunami waves was the most frequent (44%), followed by separation from caregivers (39%), restrictions on their lifestyle due to radiation (28%), witnessing a fire (21%), losing distant relatives or friends (18%), and losing a close family member or relative (10%). Further, 45.9% experienced a traumatic event before the earthquake, in which the mean number of other trauma events before the earthquake was 0.74 (SD = 0.98, range 0–4), mostly the death of a close friend or family member (19.4%), a close friend or family member having a serious illness (16.5%), and being separated from their caregiver (15.9%).
Associations of demographics and traumatic experience with clinically significant internalizing behavior problems are shown in Table 2. In our bivariate model, we found that the deaths of distant relatives or friends and other trauma experienced before the earthquake showed significant association with clinically significant internalizing behavior problems (47.6% vs. 20.2%, rate ratio [RR]: 2.36, 95% CI: 1.10–5.07), and they remained significant even in the multivariate model, which were mutually adjusted. That is, the rate ratio suggests that children who lost distant relatives or friends were 2.22 times (95% CI: 1.03–4.78) more likely to show clinically significant internalizing problems, independent of other trauma experiences before the earthquake. Similarly, children in the affected area who experienced other trauma before the earthquake were 2.22 times (95% CI: 1.22–4.07) more likely to show clinically significant internalizing problems, regardless of trauma exposure related to the earthquake, at 2 years after the earthquake. The interaction effect between experience of other trauma before the earthquake and disaster exposure was not observed (p for interaction term = 0.502) for internalizing problems, although 28 out of 73 (38.4%) children who experienced both other trauma before the earthquake and trauma related to the earthquake had internalizing problems. This is a higher proportion compared to children who experienced trauma related to the earthquake only and had no prior trauma exposure (15 out of 84, 17.9%, p for chi-square = 0.004). The association between other trauma experiences and internalizing problems was not found in the unaffected area (RR: 0.64, 95% CI: 0.07–5.73, data not shown).
Table 2. Bivariate and multivariate analyses of CBCL clinically significant internalizing behavior problems among young children 2 years after the Great East Japan Earthquake (N = 170).
| CBCL clinically significant internalizing behavior problems | ||||||||||
| n | % | Bivariate RR | 95% CI | Multivariate RR | 95% CI | |||||
| Demographics | Child age group | 5–6 y | 19 | 21.8 | reference | |||||
| 7–8 y | 28 | 33.7 | 1.54 | (0.86–2.77) | ||||||
| Child sex | Boy | 28 | 33.3 | reference | ||||||
| Girl | 19 | 22.1 | 0.66 | (0.37–1.19) | ||||||
| Number of siblings | No sibling | 8 | 21.6 | reference | ||||||
| 1 sibling | 26 | 31.3 | 1.45 | (0.66–3.20) | ||||||
| 2+ siblings | 12 | 25.0 | 1.16 | (0.47–2.83) | ||||||
| Caregiver age group | 36 or less | 28 | 28.6 | reference | ||||||
| 37+ | 19 | 26.4 | 0.92 | (0.52–1.65) | ||||||
| Education | High school or less | 18 | 22.8 | reference | ||||||
| Some college+ | 29 | 32.6 | 1.43 | (0.79–2.58) | ||||||
| Father's occupation before earthquake | Manual/Other/Unemployed | 19 | 21.6 | reference | ||||||
| Non-manual | 12 | 31.6 | 1.46 | (0.71–3.01) | ||||||
| No response | 16 | 36.4 | 1.68 | (0.87–3.28) | ||||||
| Traumatic experience | Status of home | Lost or completely damaged | 13 | 28.9 | 0.99 | (0.50–1.94) | ||||
| Partially damaged | 10 | 23.3 | 0.79 | (0.38–1.66) | ||||||
| Not damaged | 24 | 29.3 | reference | |||||||
| Stayed at shelter | Yes | 17 | 34.0 | 1.50 | (0.81–2.77) | |||||
| No | 25 | 22.7 | reference | |||||||
| Lived in temporary housing | Yes | 10 | 29.4 | 1.15 | (0.57–2.33) | |||||
| No | 33 | 25.6 | reference | |||||||
| Evacuated to relative's house | Yes | 22 | 22.9 | 0.70 | (0.39–1.26) | |||||
| No | 22 | 32.8 | reference | |||||||
| Family members living in separate places | Yes | 14 | 26.4 | 1.41 | (0.76–2.62) | |||||
| No | 30 | 27.5 | reference | |||||||
| Separation from caregiver | Yes | 17 | 31.5 | 1.24 | (0.65–2.37) | |||||
| No | 20 | 25.3 | reference | |||||||
| Lost close family member or relative | Yes | 2 | 18.2 | 0.63 | (0.15–2.62) | |||||
| No | 31 | 29.0 | reference | |||||||
| Lost distant relative or friend | Yes | 10 | 47.6 | 2.36 | (1.10–5.07) | 2.22 | (1.03–4.78) | |||
| No | 19 | 20.2 | reference | reference | ||||||
| Witnessed tsunami waves | Yes | 17 | 27.0 | 0.97 | (0.51–1.82) | |||||
| No | 22 | 27.9 | reference | |||||||
| Witnessed someone being swept away by tsunami | Yes | 4 | 36.4 | 1.36 | (0.48–3.83) | |||||
| No | 35 | 26.7 | reference | |||||||
| Witnessed a fire | Yes | 9 | 30.0 | 1.10 | (0.52–2.32) | |||||
| No | 30 | 27.3 | reference | |||||||
| Saw a dead body | Yes | 2 | 66.7 | 2.41 | (0.58–10.02) | |||||
| No | 37 | 27.6 | reference | |||||||
| Heard the sound of nuclear power plant explosion | Yes | 0 | 0.0 | NA | ||||||
| No | 31 | 25.6 | ||||||||
| Experienced restrictions on lifestyle due to radiation | Yes | 8 | 25.0 | 0.99 | (0.44–2.23) | |||||
| No | 21 | 25.3 | reference | |||||||
| Exposure to any trauma events or other trauma before the earthquake | Yes | 31 | 39.7 | 2.29 | (1.25–4.18) | 2.22 | (1.22–4.07) | |||
| No | 16 | 17.4 | reference | |||||||
CBCL: Child Behavior Checklist.
RR: rate ratio.
In our bivariate model, no traumatic experiences related to the earthquake were associated with externalizing problems, while other trauma experiences before the earthquake were significantly associated (Table 3). In the multivariate model adjusted for father's occupation, which showed significant association with externalizing problems in the bivariate model, children in the affected area who experienced other trauma before the earthquake were 2.41 times (95% CI: 1.16–4.99) more likely to show externalizing behavior problems. The interaction effect between experience of other trauma before the earthquake and disaster exposure was not observed (p for interaction term = 0.296) for externalizing problems, although 24 out of 73 (32.9%) children who experienced both other trauma before the earthquake and trauma related to the earthquake had externalizing problems. This is a higher proportion compared to children exposed to disaster trauma only (9 out of 84 (10.7%), p for chi-square = 0.001). This association was not found in the unaffected area (RR: 1.28, 95% CI: 0.32–5.12, data not shown).
Table 3. Bivariate and multivariate analysis of CBCL clinically significant externalizing behavior problems among young children 2 years after the Great East Japan Earthquake (N = 170).
| CBCL clinically significant externalizing behavior problems | ||||||||||
| n | % | Bivariate RR | 95% CI | Multivariate RR | 95% CI | |||||
| Demographics | Child age group | 5–6 y | 14 | 16.1 | reference | |||||
| 7–8 y | 22 | 26.5 | 1.65 | (0.84–3.22) | ||||||
| Child sex | Boy | 19 | 22.6 | reference | ||||||
| Girl | 17 | 19.8 | 0.87 | (0.45–1.68) | ||||||
| Number of siblings | No sibling | 8 | 21.6 | reference | ||||||
| 1 sibling | 16 | 19.3 | 0.89 | (0.38–2.08) | ||||||
| 2+ siblings | 11 | 22.9 | 1.06 | (0.43–2.64) | ||||||
| Caregiver age group | 36 or less | 16 | 16.3 | reference | ||||||
| 37+ | 20 | 27.8 | 1.70 | (0.88–3.28) | ||||||
| Education | High school or less | 18 | 22.8 | reference | ||||||
| Some college+ | 18 | 20.2 | 0.89 | (0.46–1.71) | ||||||
| Father's occupation before earthquake | Manual/Other/Unemployed | 14 | 15.9 | reference | reference | |||||
| Non-manual | 7 | 18.4 | 1.16 | (0.47–2.87) | 1.02 | (0.41–2.53) | ||||
| No response | 15 | 34.1 | 2.14 | (1.03–4.44) | 1.69 | (0.80–3.58) | ||||
| Traumatic experience | Status of home | Lost or completely damaged | 10 | 22.2 | 1.30 | (0.58–2.93) | ||||
| Partially damaged | 12 | 27.9 | 1.63 | (0.76–3.53) | ||||||
| Not damaged | 14 | 17.1 | reference | |||||||
| Stayed at shelter | Yes | 12 | 24.0 | 1.39 | (0.67–2.86) | |||||
| No | 19 | 17.3 | reference | |||||||
| Lived in temporary housing | Yes | 7 | 20.6 | 0.98 | (0.43–2.26) | |||||
| No | 27 | 20.9 | reference | |||||||
| Evacuated to relative's house | Yes | 16 | 16.7 | 0.62 | (0.32–1.22) | |||||
| No | 18 | 26.9 | reference | |||||||
| Family members living in separate places | Yes | 10 | 18.9 | 0.82 | (0.40–1.71) | |||||
| No | 25 | 22.9 | reference | |||||||
| Separation from caregiver | Yes | 12 | 22.2 | 1.17 | (0.55–2.50) | |||||
| No | 15 | 19.0 | reference | |||||||
| Lost close family member or relative | Yes | 0 | 0 | NA | ||||||
| No | 26 | 24.3 | ||||||||
| Lost distant relative or friend | Yes | 4 | 19.1 | 0.99 | (0.34–2.94) | |||||
| No | 18 | 19.2 | reference | |||||||
| Witnessed tsunami waves | Yes | 16 | 25.4 | 1.67 | (0.79–3.53) | |||||
| No | 12 | 15.2 | reference | |||||||
| Witnessed someone being swept away by tsunami | Yes | 3 | 27.3 | 1.43 | (0.43–4.73) | |||||
| No | 25 | 19.1 | reference | |||||||
| Witnessed a fire | Yes | 7 | 23.3 | 1.28 | (0.54–3.03) | |||||
| No | 20 | 18.2 | reference | |||||||
| Saw a dead body | Yes | 0 | 0 | NA | ||||||
| No | 28 | 20.9 | ||||||||
| Heard the sound of nuclear power plant explosion | Yes | 0 | 0.0 | NA | ||||||
| No | 23 | 19.0 | ||||||||
| Experienced restrictions on lifestyle due to radiation | Yes | 4 | 12.5 | 0.61 | (0.21–1.81) | |||||
| No | 17 | 20.5 | reference | |||||||
| Exposure to any trauma events or other trauma before the earthquake | Yes | 25 | 32.1 | 2.68 | (1.32–5.45) | 2.41 | (1.16–4.99) | |||
| No | 11 | 12.0 | reference | reference | ||||||
CBCL: Child Behavior Checklist.
RR: rate ratio.
Finally, the associations of CBCL clinically significant total behavior problems with demographics and traumatic experiences are shown in Table 4. As with the results regarding externalizing problems, no traumatic experiences related to the earthquake were associated with total behavior problems, while other trauma experiences before the earthquake were significantly associated. In the multivariate model adjusted for child age, which showed a marginal association with total behavior problems in the bivariate model, children in the affected area who experienced other trauma before the earthquake were 2.98 times (95% CI: 1.53–5.81) more likely to show total behavior problems. The interaction effect between experience of other trauma before the earthquake and disaster exposure was not observed (p for interaction term = 0.242) for total behavior problems, although 31 out of 73 (42.5%) children who experienced both other trauma before the earthquake and trauma related to the earthquake had total behavior problems. This is a higher proportion compared to children exposed to disaster trauma only (10 out of 84 (11.9%), p for chi-square <0.001). This association was not found in the unaffected area (RR: 1.03, 95% CI: 0.20–5.28, data not shown).
Table 4. Bivariate and multivariate analysis of Child Behavior Checklist (CBCL) clinically significant total behavior problems among young children 2 years after the Great East Japan Earthquake (N = 170).
| CBCL clinically significant total behavior problems | ||||||||||
| n | % | Bivariate PR | 95% CI | Multivariate PR | 95% CI | |||||
| Demographics | Child age group | 5–6 y | 16 | 18.4 | reference | reference | ||||
| 7–8 y | 28 | 33.7 | 1.83 | (0.99–3.39) | 1.25 | (0.93–1.67) | ||||
| Child sex | Boy | 27 | 32.1 | reference | ||||||
| Girl | 17 | 19.8 | 0.61 | (0.34–1.13) | ||||||
| Number of siblings | No sibling | 13 | 35.1 | reference | ||||||
| 1 sibling | 22 | 26.5 | 0.75 | (0.38–1.50) | ||||||
| 2+ siblings | 8 | 16.7 | 0.47 | (0.20–1.14) | ||||||
| Caregiver age group | 36 or less | 23 | 23.5 | reference | ||||||
| 37+ | 21 | 29.2 | 1.24 | (0.69–2.25) | ||||||
| Education | High school or less | 21 | 26.6 | reference | ||||||
| Some college+ | 23 | 25.8 | 0.97 | (0.54–1.76) | ||||||
| Father's occupation before earthquake | Manual/Other/Unemployed | 18 | 20.5 | reference | ||||||
| Non-manual | 11 | 29.0 | 1.42 | (0.67–3.00) | ||||||
| No response | 15 | 34.1 | 1.67 | (0.84–3.31) | ||||||
| Traumatic experience | Status of home | Lost or completely damaged | 12 | 26.7 | 1.21 | (0.59–2.52) | ||||
| Partially damaged | 14 | 32.6 | 1.48 | (0.74–2.98) | ||||||
| Not damaged | 18 | 22.0 | reference | |||||||
| Stayed at shelter | Yes | 14 | 28.0 | 1.28 | (0.66–2.48) | |||||
| No | 24 | 21.8 | reference | |||||||
| Lived in temporary housing | Yes | 9 | 26.5 | 1.03 | (0.50–2.16) | |||||
| No | 33 | 25.6 | reference | |||||||
| Evacuated to relative's house | Yes | 22 | 22.9 | 0.81 | (0.44–1.49) | |||||
| No | 19 | 28.4 | reference | |||||||
| Family members living in separate places | Yes | 15 | 28.3 | 1.14 | (0.61–2.15) | |||||
| No | 27 | 24.8 | reference | |||||||
| Separation from caregiver | Yes | 17 | 31.5 | 1.38 | (0.71–2.68) | |||||
| No | 18 | 22.8 | reference | |||||||
| Lost close family member or relative | Yes | 1 | 9.1 | 0.31 | (0.04–2.30) | |||||
| No | 31 | 29.0 | reference | |||||||
| Lost distant relative or friend | Yes | 8 | 38.1 | 1.71 | (0.76–3.85) | |||||
| No | 21 | 22.3 | reference | |||||||
| Witnessed tsunami waves | Yes | 19 | 30.2 | 1.40 | (0.73–2.70) | |||||
| No | 17 | 21.5 | reference | |||||||
| Witnessed someone being swept away by tsunami | Yes | 4 | 36.4 | 1.49 | (0.53–4.21) | |||||
| No | 32 | 24.4 | reference | |||||||
| Witnessed a fire | Yes | 10 | 33.3 | 1.47 | (0.70–3.05) | |||||
| No | 25 | 22.7 | reference | |||||||
| Saw a dead body | Yes | 1 | 33.3 | 1.28 | (0.17–9.32) | |||||
| No | 35 | 26.1 | reference | |||||||
| Heard the sound of nuclear power plant explosion | Yes | 0 | 0.0 | NA | ||||||
| No | 28 | 23.1 | ||||||||
| Experienced restrictions on lifestyle due to radiation | Yes | 6 | 18.8 | 0.78 | (0.31–1.94) | |||||
| No | 20 | 24.1 | reference | |||||||
| Exposure to any trauma events or other trauma before the earthquake | Yes | 32 | 41.0 | 3.15 | (1.62–6.11) | 2.98 | (1.53–5.81) | |||
| No | 12 | 13.0 | reference | reference | ||||||
CBCL: Child Behavior Checklist.
RR: rate ratio.
Discussion
We found that clinically significant behavior problems were reported in 26% of young children 2 years after the Great East Japan Earthquake. Interestingly, we observed that the rate of internalizing problems (28%) was higher than the rate of externalizing problems (21%) in the affected area. As internalized problems are less likely to be recognized compared to externalized problems in this age group, these behavior problems may have been underestimated during the 2 years following the earthquake.
To the best of our knowledge, this is the first study to show the rate of behavior problems using the CBCL among 5- to 8-year-old children 2 years after the Great East Japan Earthquake. The rate of clinically significant behavior problems using the CBCL was equivalent to findings from the study of preschool children exposed to the World Trade Center attack, for which the rate was 15–30% for each subscale of the CBCL [29]. McLaughlin et al. reported that 2 years after Hurricane Katrina, 15% of children aged 4 to 17 years had serious emotional disturbances (defined by a combination of scores for conduct problems, hyperactivity-inattention, emotional symptoms, peer problems, and symptom-related impairment measured by the Strengths and Difficulties Questionnaire) [21]. Furthermore, depression, which can be considered an internalizing problem, was reported in 12% of children aged 7 to 14 years who had been living for 9 months in displacement camps after the 2004 Indian Ocean earthquake and tsunami [12]. Although a simple comparison is not plausible because of differences in age, ethnicity, type of disaster, and timing of the assessment after the disaster, it is noteworthy that the rate of children aged 5 to 8 years with behavior problems after the Great East Japan Earthquake was higher than the rate after Hurricane Katrina or after the 2004 Indian Ocean disaster in affected parts of southern Thailand, which illustrates the severity of the trauma experienced by children residing in the affected area of Japan as a result of the earthquake, tsunami, and subsequent radiation crisis.
We found that losing distant relatives or friends was associated with clinically significant internalizing problems, but not externalizing or total behavior problems. This is consistent with previous research, which shows that depression among children after the 2004 Indian Ocean tsunami in devastated areas of southern Thailand was associated with the experience of a close family member or friend being injured [12]. The experience of losing a relative or friend may cause children to feel sadness, fear, or regret because they were unable to help during the tsunami, which leads to internalizing behavior. In our study, the lack of association of depression with losing a close family member or relative might have been due to selection bias and lack of power; that is, caregivers who lost a family member were less likely to participate in this study. In our study, only two children lost a close family member or relative. A previous study also reported that a natural disaster's long-term repercussions on children's mental health is influenced by various determinants including being separated from caregivers, experiencing traumatic events, and feeling that one's life or that of a close friend or family member is under threat [34].
We also found that other trauma experiences that occurred before the earthquake were significant risk factors for behavior problems among young children who were exposed to the earthquake, regardless of internalizing or externalizing behavior problems. This is consistent with findings of behavior problems in children after the World Trade Center attacks that showed a combined effect of other trauma exposure before the attacks, and traumatic events related to the attacks showed synergistic effects on behavior problems. High-risk approaches targeting young children who have been exposed to other trauma before the earthquake might be an efficient strategy to provide mental healthcare resources, which are limited after the earthquake.
Several limitations of this study must be addressed. First, the participants were not a representative sample of the municipalities affected by the earthquake; that is, we selected municipalities where one of the authors had enough personal connections to conduct this study. Furthermore, children with severe mental disorders in the target population may have been reluctant to join this study because they had already received psychiatric services. Alternatively, caregivers who were concerned about their children's mental health might have been more likely to participate in this study. Nonetheless, the significance of this study is that it reveals the rate of children with behavior problems in a community sample. Second, the CBCL was filled out by caregivers only; thus, behavior problems in school were not included. Further research should combine teacher and caregiver CBCL ratings. Third, severe traumatic experiences related to the earthquake were assessed through interviews with children, but some children might not describe their true experiences to an interviewer. We double-checked the reported experiences by interviewing caregivers and preschool teachers, but we considered the trauma described by child participants themselves as being the most authentically representative of the children's trauma. Fourth, our sample size was relatively small; thus, there may have been too few participants to properly assess the significance of the associations between specific traumatic experiences and behavior problems. However, even with this small sample size, we demonstrated that some specific traumatic experiences were associated with behavior problems, which informs suggestions for future prevention of behavior problems after a natural disaster. Fifth, the response rate is not very high, especially in Fukushima. This is because most children were evacuated from the original community as a result of the radiation crisis, thus it was extremely difficult to obtain consent.
In conclusion, clinically significant behavior problems were found in one of four young children living in the area affected by the Great East Japan Earthquake, even 2 years after the disaster. Specific trauma experience, i.e., loss of distant relatives or friends, was associated with internalizing problems, but not externalizing or total behavior problems. Moreover, children who experienced other trauma events before the earthquake were more likely to have behavior problems. Based on these findings, we make a call for further interventions for young children exposed to the disaster, such as psychoeducation programs to provide information on traumatic symptoms, coping strategies and recovery, in collaboration with school and preschool principals, teachers, and school counselors. Moreover, larger studies using representative samples are essential to further address the mental health needs of young children exposed to the 2011 disaster.
Acknowledgments
We thank all the participants who contributed to this study. We also thank the child psychiatrists and psychologists who provided extra mental health support to participants when requested during interviews. In addition, we thank the research coordinators, especially Ms Maiko Osawa and Ms Hisayo Saeki, who coordinated the logistics for this study, and Ms. Emma Barber for her editorial assistance. The Great East Japan Earthquake Follow-up for Children Study Team is composed of Dr Takehito Yambe and Ms Mitsuko Miura, Iwate Medical University, Dr Hirokazu Yoshida, Miyagi Prefectural Comprehensive Children's Center, Dr Yoshiko Yamamoto, Iwaki Meisei University, Ms Noriko Ohshima, Fukushima Gakuin University, Dr Keiichi Funahashi and Ms Mai Kuroda, Saitama Children's Hospital, Dr Takahiro Hoshino, Musashino Gakuin School, Ms Rie Mizuki, Dr Lena Akai, and Dr Yoshiyuki Tachibana, National Center for Child Health and Development, lead by Dr Makiko Okuyama (okuyama-m@ncchd.go.jp).
Data Availability
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Due to the ethical restriction by Institutional Review Board, the data cannot be made available in the manuscript, the supplemental files, or a public repository. Please contact corresponding author, Takeo Fujiwara, with any data requests.
Funding Statement
This study is supported by a grant from the Ministry of Health, Labour and Welfare (H24-jisedai-shitei-007). The role of funders is implementation of this study.
References
- 1. Fire and Disaster Management Agency (2013) Higai-hou. Fire and Disaster Management Agency [Google Scholar]
- 2.Japan Child and Family Research Institute (2013) Almanac of data on Japanese children 2013. Tokyo: KTC Chuoh Publishing. [Google Scholar]
- 3. Uemoto M, Shioyama A, Koide K, Honda M, Takamiya S, et al. (2000) [The mental health of school children after the Great Hanshin-Awaji Earthquake: I. Epidemiological study and risk factors for mental distress]. Seishin Shinkeigaku Zasshi 102: 459–480. [PubMed] [Google Scholar]
- 4. Shioyama A, Uemoto M, Shinfuku N, Ide H, Seki W, et al. (2000) [The mental health of school children after the Great Hanshin-Awaji Earthquake: II. Longitudinal analysis]. Seishin Shinkeigaku Zasshi 102: 481–497. [PubMed] [Google Scholar]
- 5. Kitayama S, Okada Y, Takumi T, Takada S, Inagaki Y, et al. (2000) Psychological and physical reactions on children after the Hanshin-Awaji earthquake disaster. Kobe J Med Sci 46: 189–200. [PubMed] [Google Scholar]
- 6. Laor N, Wolmer L, Kora M, Yucel D, Spirman S, et al. (2002) Posttraumatic, dissociative and grief symptoms in Turkish children exposed to the 1999 earthquakes. J Nerv Ment Dis 190: 824–832. [DOI] [PubMed] [Google Scholar]
- 7. Tural U, Coskun B, Onder E, Corapcioglu A, Yildiz M, et al. (2004) Psychological consequences of the 1999 earthquake in Turkey. J Trauma Stress 17: 451–459. [DOI] [PubMed] [Google Scholar]
- 8. Sahin NH, Batigun AD, Yilmaz B (2007) Psychological symptoms of Turkish children and adolescents after the 1999 earthquake: exposure, gender, location, and time duration. J Trauma Stress 20: 335–345. [DOI] [PubMed] [Google Scholar]
- 9. Bal A, Jensen B (2007) Post-traumatic stress disorder symptom clusters in Turkish child and adolescent trauma survivors. Eur Child Adolesc Psychiatry 16: 449–457. [DOI] [PubMed] [Google Scholar]
- 10. Eksi A, Braun KL (2009) Over-time changes in PTSD and depression among children surviving the 1999 Istanbul earthquake. Eur Child Adolesc Psychiatry 18: 384–391. [DOI] [PubMed] [Google Scholar]
- 11. Celebi Oncu E, Wise AM (2010) The effects of the 1999 Turkish earthquake on young children: analyzing traumatized children's completion of short stories. Child Dev 81: 1161–1175. [DOI] [PubMed] [Google Scholar]
- 12. Thienkrua W, Cardozo BL, Chakkraband ML, Guadamuz TE, Pengjuntr W, et al. (2006) Symptoms of posttraumatic stress disorder and depression among children in tsunami-affected areas in southern Thailand. JAMA 296: 549–559. [DOI] [PubMed] [Google Scholar]
- 13. Agustini EN, Asniar I, Matsuo H (2011) The prevalence of long-term post-traumatic stress symptoms among adolescents after the tsunami in Aceh. J Psychiatr Ment Health Nurs 18: 543–549. [DOI] [PubMed] [Google Scholar]
- 14. Piyasil V, Ketuman P, Plubrukarn R, Jotipanut V, Tanprasert S, et al. (2007) Post traumatic stress disorder in children after tsunami disaster in Thailand: 2 years follow-up. J Med Assoc Thai 90: 2370–2376. [PubMed] [Google Scholar]
- 15. Piyasil V, Ketumarn P, Prubrukarn R, Pacharakaew S, Dumrongphol H, et al. (2008) Psychiatric disorders in children at one year after the tsunami disaster in Thailand. J Med Assoc Thai 91 Suppl 3: S15–20. [PubMed] [Google Scholar]
- 16. Ularntinon S, Piyasil V, Ketumarn P, Sitdhiraksa N, Pityaratstian N, et al. (2008) Assessment of psychopathological consequences in children at 3 years after tsunami disaster. J Med Assoc Thai 91 Suppl 3: S69–75. [PubMed] [Google Scholar]
- 17. Piyasil V, Ketumarn P, Prubrukarn R, Ularntinon S, Sitdhiraksa N, et al. (2011) Post-traumatic stress disorder in children after the tsunami disaster in Thailand: a 5-year follow-up. J Med Assoc Thai 94 Suppl 3: S138–144. [PubMed] [Google Scholar]
- 18. Scheeringa MS, Zeanah CH (2008) Reconsideration of harm's way: onsets and comorbidity patterns of disorders in preschool children and their caregivers following Hurricane Katrina. J Clin Child Adolesc Psychol 37: 508–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marsee MA (2008) Reactive aggression and posttraumatic stress in adolescents affected by Hurricane Katrina. J Clin Child Adolesc Psychol 37: 519–529. [DOI] [PubMed] [Google Scholar]
- 20. Osofsky HJ, Osofsky JD, Kronenberg M, Brennan A, Hansel TC (2009) Posttraumatic stress symptoms in children after Hurricane Katrina: predicting the need for mental health services. Am J Orthopsychiatry 79: 212–220. [DOI] [PubMed] [Google Scholar]
- 21. McLaughlin KA, Fairbank JA, Gruber MJ, Jones RT, Lakoma MD, et al. (2009) Serious emotional disturbance among youths exposed to Hurricane Katrina 2 years postdisaster. J Am Acad Child Adolesc Psychiatry 48: 1069–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu M, Wang L, Shi Z, Zhang Z, Zhang K, et al. (2011) Mental health problems among children one-year after Sichuan earthquake in China: a follow-up study. PLoS One 6: e14706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang Z, Ran MS, Li YH, Ou GJ, Gong RR, et al. (2012) Prevalence of post-traumatic stress disorder among adolescents after the Wenchuan earthquake in China. Psychol Med 42: 1687–1693. [DOI] [PubMed] [Google Scholar]
- 24. Jia Z, Shi L, Duan G, Liu W, Pan X, et al. (2013) Traumatic experiences and mental health consequences among child survivors of the 2008 Sichuan earthquake: a community-based follow-up study. BMC Public Health 13: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Yang R, Xiang YT, Shuai L, Qian Y, Lai KY, et al. (2013) Executive function in children and adolescents with posttraumatic stress disorder 4 and 12 months after the Sichuan earthquake in China. J Child Psychol Psychiatry [DOI] [PubMed] [Google Scholar]
- 26. Dehon C, Scheeringa MS (2006) Screening for preschool posttraumatic stress disorder with the Child Behavior Checklist. J Pediatr Psychol 31: 431–435. [DOI] [PubMed] [Google Scholar]
- 27. Loeb J, Stettler EM, Gavila T, Stein A, Chinitz S (2011) The child behavior checklist PTSD scale: screening for PTSD in young children with high exposure to trauma. J Trauma Stress 24: 430–434. [DOI] [PubMed] [Google Scholar]
- 28. Lowe SR, Godoy L, Rhodes JE, Carter AS (2013) Predicting mothers' reports of children's mental health three years after Hurricane Katrina. J Appl Dev Psychol 34: 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chemtob CM, Nomura Y, Abramovitz RA (2008) Impact of conjoined exposure to the World Trade Center attacks and to other traumatic events on the behavioral problems of preschool children. Arch Pediatr Adolesc Med 162: 126–133. [DOI] [PubMed] [Google Scholar]
- 30. Achenbach TM (1991) Manual for Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry [Google Scholar]
- 31. Itani T, Kanbayashi Y, Nakata Y, Kita M, Fujii H, et al. (2001) Standardization of the Japanese version of the Child Behavior Checklist/4–18. Psychiatr Neurol Pediatr Jpn 41: 243–252 (in Japanese with English abstract).. [Google Scholar]
- 32. Zhang J, Yu KF (1998) What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280: 1690–1691. [DOI] [PubMed] [Google Scholar]
- 33. Barros AJ, Hirakata VN (2003) Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC Med Res Methodol 3: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lubit R, Rovine D, DeFrancisci L, Eth S (2003) Impact of trauma on children. J Psychiatr Pract 9: 128–138. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that, for approved reasons, some access restrictions apply to the data underlying the findings. Due to the ethical restriction by Institutional Review Board, the data cannot be made available in the manuscript, the supplemental files, or a public repository. Please contact corresponding author, Takeo Fujiwara, with any data requests.